Abstract
In the last few years, transcatheter aortic valve replacement (TAVR) has rapidly become the standard of care for severe symptomatic aortic stenosis (AS). If initially it was preferred only for high-risk surgical patients, now even low-risk patients are eligible candidates. There were several factors to consider why patients with bicuspid aortic valves (BAVs) were omitted from these trials. However, it should be noted that bicuspid AS is not unusual among patients who experience transcatheter valve implantation. The TAVR procedure in BAV is a reliable and safe treatment option for surgical aortic valve replacement (SAVR) but it is associated with an elevated incidence of paravalvular regurgitation (PVR) and the likelihood of implanting a permanent pacemaker. Bicuspid valves do not appear to be a contraindication to TAVI according to current data, but further specific clinical trials will be required to confirm this conclusion.
Keywords:aortic stenosis, bicuspid aortic valve, bicuspid aortopathy, transcatheter aortic valve replacement.
INTRODUCTION
Bicuspid aortic valves (BAVs) are usually diagnosed in young adults; however, they may also manifest themselves in older adults. In the case of BAVs, stenosis or regurgitation can occur, which is usually associated with a large aorta (1). There is an increased prevalence of congenital bicuspid valves observed in patients with aortic stenosis (AS) under the age of 60 years. The utilization of transcatheter valves for severe AS symptoms has substantially advanced since 2002. This has led to improvements in transcatheter valve technologies, facilitating vascular access, and providing simpler implantation procedures (2). All of these have resulted in improved clinical outcomes since they were first performed under compassionate- use conditions. The indications of TAVR were formerly limited to patients who were considered an inoperable or high surgical risk (3, 4) but recent studies have established that it was comparable to, or superior to, SAVR in intermediate- risk patients (5, 6), therefore extending its therapeutic application. There are several ongoing clinical trials in low-risk patients that may justify the use of TAVR in AS patients. Transcatheter aortic valve replacement may be a viable option for therapeutic intervention for AS patients based on the results of several recent clinical trials in low-risk patients. Forrest et al suggested that transcatheter aortic valve implantation resulted in promising 30-day results, significant decreases in mortality and stroke rates, and significant success rates among low-surgical risk patients with BAV stenosis (7).
A description of the anatomical structure of the bicuspid valve
The technique for TAVR in BAV continues to be a challenge due to a combination of anatomical and technical aspects. As a starting point, the predominantly elliptical than spherical shape of the aortic annulus usually encountered with BAV, in conjunction with the enlarged dimensions of the ascending aorta and root, makes placement and attachment of a transcatheter valve more difficult (8, 9).
Aortic valvular irregularities and dissymmetrical calcification patterns could contribute to the valve body being misaligned or inadequately expanded and positioned during valve placement. The aortic root and ascending aorta are more likely to be harmed following pre-dilatation valvuloplasty, valve deployment, and post-dilatation (10). High-resolution computed tomography (CT) has a better understanding of bicuspid AS. Computed tomography facilitates the assessment of the condition in numerous patients for whom standard echocardiographic imaging is inappropriate. Sievers and Schmidtke's classification (11) of congenital bicuspid valve features (which is able to be clearly recognized by CT) distinguishes the three main variants of the congenital bicuspid valve (types 0, 1, 2) based on the presence or absence of seam-like raphes that connect the leaflets in the valve (Figure 1) (12). In terms of bicuspid valve morphologies, ethnicity appears to play a significant role. Jilaihawi et al suggested that those who had type 0 morphology were found to be more frequent in China (13), whereas those with type 1 morphology exceeded 50% of patients in most published series from Western countries.
Phillip et al reported that aortic annuli were less elliptical in bicuspid valves relative to tricuspid valves (ellipticity index 1.24 versus 1.29) (14). According to this investigation, the annular area of subjects with bicuspid valves was significantly greater (5.21 cm2 vs. 4.63 cm2), and eccentric calcium accumulation was more prevalent in patients with bicuspid valves. It is important to underline that in a large series of bicuspid patients, the annular dimensions do not exceed those commonly treated with commercially available TAVI devices (15-17).
Procedural approach
Considering the annular characteristics of both lesions, the selection of a TAVI device for bicuspid AS is similar to the selection of a TAVI device for tricuspid AS (18). In contrast, the deployment of the device is more complex due to the irregular and asymmetric appearance of the cusps on angiography, which may result in mispositioning, paravalvular regurgitation, and an increased need for pacemakers following TAVI. Anatomical parameters of the bicuspid valve are likely to impact TAVI device expansion. In a study of 15 patients treated with an expandable device, Himbert et al reported that the annular expansion was not circular (19). In a bicuspid orifice, non-circular expansion may be more common with self-expanding valves (16), perhaps due to the irregular shape and forces exerted. In the latest transcatheter valve devices, exteriorly attached skirts or cuffs are able to prevent PVR by increasing apposition without producing additional damage to the aortic valve architecture. A study investigating the first-generation valves without external skirts (Sapien and CoreValve) with the second-generation valves with external skirts (Sapien 3 and Lotus) reported a significant reduction in PVR from 8.5% to 0.0% (20). A new-generation balloon-expandable valve also exhibits an asymmetric longitudinal expansion, but there is no information regarding the degree of expansion of the annulus in these devices (17).
OUTCOMES
In patients with BAV, a number of case reports have documented a higher PVR, valve misplacement, and permanent pacemaker implantation after TAVR (15, 21, 22).
The Society of Thoracic Surgery/American College of Cardiology (STS/ACC) Transcatheter Valve Therapy (TVT) registry reported a 95% procedure success rate according to a meta-analysis of 13 observational research papers (758 BAV patients) (23, 24).In this study, there was a significantly greater proportion of moderate and severe PVR than that observed for the tricuspid aortic valve (95% CI, 3.2% to 24.7%). A comparable rate of early safety complications was documented in the BAV and tricuspid valves. These complications consisted of all-cause mortality, stroke, life-threatening bleeding, major vascular complications, or valve dysfunction. In addition, there was no variation in the occurrence of annular rupture between the BAV and the tricuspid aortic valve. In opposition, there was an increased requirement for PPM placement compared to those with BAV, recent large series have reported a new pacemaker rate of 17-29% (15, 17, 21, 25, 26). Pacemaker implantation rates may be higher because of difficulty in achieving the exact height of the implantation due to irregular shapes of the leaflets on fluoroscopy. As a consequence, there may be a lower level of implantation, which is known to increase the rates of pacemaker implantation. In patients treated with SAPIEN 3 TAVI, the depth of implantation was assessed. Lower implantations (8 mm below the annulus) were associated with higher pacemaker rates (17).
It has been suggested that the most common type of bicuspid valve (right-left fusion) may exert greater forces on the membranous septum and the conduction system, resulting in a higher requirement for pacemaker implantation (15). As BAV patients are usually young and have fewer comorbid conditions than tricuspid AS patients, there are no long-term outcome data available for BAV subjects following the TAVR procedure. By contrast to patients with tricuspid AS, those with BAV had an increased rate of switching to surgery following TAV [2.0% vs. 0.2%; P=0.006], and moderate or severe paravalvular leak [10.4% vs. 6.8%; P=0.04], and the necessity for second valve implantation [4.8% vs. 1.5%; P=0.002] resulting in reduced device success rate [85.3% vs. 91.4%] (15).After two years, the average mortality rates for the bicuspid and tricuspid AS cohorts were almost identical (17.2% and 19.4%, respectively; P=0.28) (22).
CONCLUSION
Even though AS caused by BAV was formerly seen as a relative contraindication for TAVR, now TAVR is an option, with viable outcomes, and safe in the BAV population. The implementation of more advanced techniques and equipment has led to an improvement in device success rates and decreased complication rates.
The trend in favor of TAVI being recommended to younger, low-risk patients is predicted to culminate in a significant share of patients with bicuspid AS becoming treated with TAVI. There will be a need for more extensive research to evaluate the long-term benefits, feasibility, and reliability of TAVR in comparison with surgical procedures as a first-line treatment approach for patients with BAV.
Conflict of interests: none declared.
Financial support: none declared.
FIGURE 1.
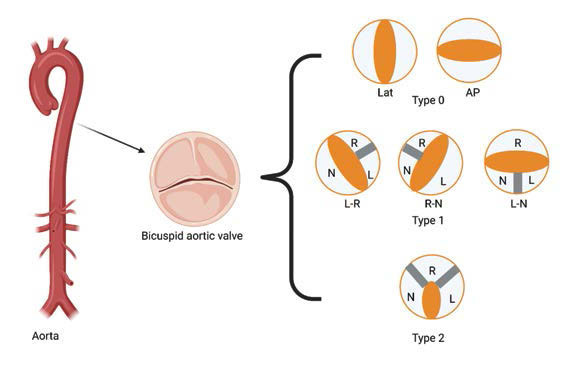
Sievers classification of BAV – figure adapted from (12). AP=anteroposterior; L=left coronary cusp; N=noncoronary cusp; R=right coronary cusp
Contributor Information
Flavius Alexandru GHERASIE, "Carol Davila" University of Medicine and Pharmacy, Bucharest, Romania.
Cristian Alexandru UDROIU, University Emergency Hospital, Bucharest, Romania.
References
- 1.Siu SC, Silversides CK. Bicuspid aortic valve disease. J Am Coll Cardiol. 2010;55:2789–800. doi: 10.1016/j.jacc.2009.12.068. [DOI] [PubMed] [Google Scholar]
- 2.Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: First human case description. Circulation. 2002;106:3006–3008. doi: 10.1161/01.cir.0000047200.36165.b8. [DOI] [PubMed] [Google Scholar]
- 3.Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. New Engl J Med. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 4.Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus Surgical Aortic-Valve Replacement in High-Risk Patients. New Engl J Med. 2011;364:2187–2198. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 5.Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. New Engl J Med. 2016;374:1609–1620. doi: 10.1056/NEJMoa1514616. [DOI] [PubMed] [Google Scholar]
- 6.Thourani VH, Kodali S, Makkar RR, et al. Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: A propensity score analysis. The Lancet. 2016;387:2218–2225. doi: 10.1016/S0140-6736(16)30073-3. [DOI] [PubMed] [Google Scholar]
- 7.Forrest JK, Ramlawi B, Deeb GM, et al. Transcatheter Aortic Valve Replacement in Low-risk Patients With Bicuspid Aortic Valve Stenosis. JAMA Cardiology. 2021;6:50–57. doi: 10.1001/jamacardio.2020.4738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah SY, Higgins A, Desai MY. Bicuspid aortic valve: Basics and beyond. Cleve Clin J Med. 2018;85:779–784. doi: 10.3949/ccjm.85a.17069. [DOI] [PubMed] [Google Scholar]
- 9.Stock S, Mohamed SA, Sievers HH. Bicuspid aortic valve related aortopathy. Gen Thorac Cardiovasc Surg. 2019;67:93–101. doi: 10.1007/s11748-017-0821-x. [DOI] [PubMed] [Google Scholar]
- 10.Praz F, Windecker S, Huber C, et al. Expanding Indications of Transcatheter Heart Valve Interventions. JACC Cardiovasc Interv. 2015;8:1777–1796. doi: 10.1016/j.jcin.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Ridley CH, Vallabhajosyula P, Bavaria JE, et al. The Sievers Classification of the Bicuspid Aortic Valve for the Perioperative Echocardiographer: The Importance of Valve Phenotype for Aortic Valve Repair in the Era of the Functional Aortic Annulus. J Cardiothorac Vasc Anesth. 2016;30:1142–1151. doi: 10.1053/j.jvca.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Sievers HH, Schmidtke C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg. 2007;133:1226–1233. doi: 10.1016/j.jtcvs.2007.01.039. [DOI] [PubMed] [Google Scholar]
- 13.Jilaihawi H, Wu Y, Yang Y, et al. Morphological characteristics of severe aortic stenosis in China: Imaging corelab observations from the first Chinese transcatheter aortic valve trial. Catheter Cardiovasc Interv, 2015. [DOI] [PubMed]
- 14.Philip F, Faza NN, Schoenhagen P, et al. Aortic annulus and root characteristics in severe aortic stenosis due to bicuspid aortic valve and tricuspid aortic valves: Implications for transcatheter aortic valve therapies. Catheter Cardiovasc Interv. 2015;86:E88–E98. doi: 10.1002/ccd.25948. [DOI] [PubMed] [Google Scholar]
- 15.Mylotte D, Lefevre T, Søndergaard L, et al. Transcatheter aortic valve replacement in bicuspid aortic valve disease. J Am Coll Cardiol. 2014;64:2330–2339. doi: 10.1016/j.jacc.2014.09.039. [DOI] [PubMed] [Google Scholar]
- 16.Hayashida K, Bouvier E, Lefèvre T, et al. Transcatheter Aortic Valve Implantation for Patients With Severe Bicuspid Aortic Valve Stenosis. Circ Cardiovasc Interv. 2013;6:284–291. doi: 10.1161/CIRCINTERVENTIONS.112.000084. [DOI] [PubMed] [Google Scholar]
- 17.Perlman GY, Blanke P, Dvir D, et al. Bicuspid Aortic Valve Stenosis: Favorable Early Outcomes With a Next-Generation Transcatheter Heart Valve in a Multicenter Study. JACC Cardiovasc Interv. 2016;9:817–824. doi: 10.1016/j.jcin.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Willson AB, Webb JG, Labounty TM, et al. 3-Dimensional Aortic Annular Assessment by Multidetector Computed Tomography Predicts Moderate or Severe Paravalvular Regurgitation After Transcatheter Aortic Valve Replacement: A Multicenter Retrospective Analysis. J Am Coll Cardiol. 2012;59:1287–1294. doi: 10.1016/j.jacc.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 19.Himbert D, Pontnau F, Messika-Zeitoun D, et al. Feasibility and outcomes of transcatheter aortic valve implantation in high-risk patients with stenotic bicuspid aortic valves. Am J Cardiol. 2012;110:877–883. doi: 10.1016/j.amjcard.2012.04.064. [DOI] [PubMed] [Google Scholar]
- 20.Yoon SH, Lefèvre T, Ahn JM, et al. Transcatheter Aortic Valve Replacement With Early- and New-Generation Devices in Bicuspid Aortic Valve Stenosis. J Am Coll Cardiol. 2016;68:1195–1205. doi: 10.1016/j.jacc.2016.06.041. [DOI] [PubMed] [Google Scholar]
- 21.Yousef A, Simard T, Webb J, et al. Transcatheter aortic valve implantation in patients with bicuspid aortic valve: A patient level multi-center analysis. Int J Cardiol. 2015;189:282–288. doi: 10.1016/j.ijcard.2015.04.066. [DOI] [PubMed] [Google Scholar]
- 22.Perlman GY, Blanke P, Webb JG. Transcatheter aortic valve implantation in bicuspid aortic valve stenosis. EuroIntervention. 2016;12:Y42–Y45. doi: 10.4244/EIJV12SYA10. [DOI] [PubMed] [Google Scholar]
- 23.Reddy G, Wang Z, Nishimura RA, et al. Transcatheter aortic valve replacement for stenotic bicuspid aortic valves: Systematic review and meta analyses of observational studies. Catheter Cardiovasc Interv. 2018;91:975–983. doi: 10.1002/ccd.27340. [DOI] [PubMed] [Google Scholar]
- 24.Grover FL, Vemulapalli S, Carroll JD, et al. 2016 Annual Report of The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol. 2017;69:1215–1230. doi: 10.1016/j.jacc.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 25.Bauer T, Linke A, Sievert H, et al. Comparison of the effectiveness of transcatheter aortic valve implantation in patients with stenotic bicuspid versus tricuspid aortic valves (from the German TAVI Registry). Am J Cardiol. 2014;113:518–521. doi: 10.1016/j.amjcard.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 26.Kochman J, Huczek Z, Ścisło P, et al. Comparison of one- and 12-month outcomes of transcatheter aortic valve replacement in patients with severely stenotic bicuspid versus tricuspid aortic valves (results from a multicenter registry). Am J Cardiol. 2014;114:757–762. doi: 10.1016/j.amjcard.2014.05.063. [DOI] [PubMed] [Google Scholar]


