Abstract
Objective
Burnout negatively affects the wellness and performance of emergency physicians (EPs). This study aimed to clarify the actual prevalence of burnout and its associated factors among Japanese EPs.
Methods
We conducted a cross‐sectional questionnaire study of selected 27 Japanese emergency departments (EDs). We examined the Maslach Burnout Inventory‐Human Services Survey score and its associations with ED‐level‐ and EP‐level factors in a multivariable analysis.
Results
A total of 267 EPs (81.9%) completed survey. Of these, 43 EPs (16.1%) scored severe emotional exhaustion (EE), 53 (19.8%) scored severe depersonalization (DP), and 179 (67.0%) scored severe personal accomplishment (PA), and 24 (8.9%) scored severely in all three domains. In our multivariable analysis, emergency medical service centers were associated with severe PA scores (odds ratio [OR], 10.56; 95% confidence interval [CI], 1.78–62.66; p = 0.009). A 3 to 6 hour‐sleep period was associated with severe EE scores (OR, 2.04; 95% CI, 1.04–3.98; p = 0.036), and EPs in their 20s were associated with severe DP scores (OR, 7.37; 95% CI, 1.41–38.38; p = 0.018).
Conclusion
Our results suggest that 8.9% of Japanese EPs are in higher degrees of burnout. In particular, Japanese EPs scored more severely on PA. To avoid burnout in Japanese EPs, it is important to improve the working environment by ensuring more than 6 h of sleep, providing more support for young EPs, and taking effective action to combat low EP self‐esteem.
Keywords: burnout, emergency medicine, physician, professional
We assessed the risk of burnout of Japanese emergency physicians (EPs). We distributed questionnaires to the EPs of 27 emergency departments (EDs); these questionnaires were used to analyze the ED‐ and EP‐level factors and correlate to the Maslach Burnout Inventory‐Human Services Survey scores. We found severe degrees of burnout in EPs working in emergency medical service centers, receiving only a 3 to 6 hour‐sleep period and those in their twenties.
INTRODUCTION
Burnout is a state of emotional, physical, and mental exhaustion caused by excessive and prolonged stress. 1 It is a three‐dimensional syndrome involving occupation‐related feelings of emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA). 1 It is usually seen in people working in the service industry, doctors, nurses, and teachers are at particularly high risk for burnout. 1 Burnout has serious consequences for physicians and patients, including lapses in professionalism, medical errors, decreased patient satisfaction, depression, and suicidal ideation. 2
Emergency physicians (EPs) have particularly high risks of burnout caused by heavy workloads, handling multiple sick patients, frequent task‐switching, and patient and colleague rudeness. 3 In 2018, Japan had a total of 3590 EPs, which constitutes only 1.2% of total number of Japanese physicians. 4 However, EPs are required to be on front‐line duty in Japanese society, such as during the coronavirus disease 2019 (COVID‐19) pandemic and to serve the aging population. 5 Therefore, Japanese EPs may be at high risks of burnout, similar to other countries. 6 Therefore, prevention of burnout in EPs warrants attention in the Japanese medical system. However, data to assess the current circumstances of mental health of Japanese EPs, such as burnout, was limited.
Therefore, we aimed to assess burnout among EPs working in emergency departments (EDs) in Japan and the factors associated with it.
METHODS
Study design and setting
A multicentric questionnaire study was conducted in 27 Japanese EDs in June 2021 from academic and community medical institutions in different geographic regions across Japan. We prepared an invitation stating the explanation of this study and request for cooperation.
Participants
In June 2021, we invited 326 physicians who worked at the 27 EDs to participate in this questionnaire study. We excluded transitional interns.
Questionnaire
Data collection
We distributed an invitation and survey questionnaires to the site investigators of the EDs, who distributed them to the participants. Site investigators set up a pickup area during the study period, and participants answered the survey anonymously and personally returned it to the pickup area. After the study period, the site investigators returned the surveys to us. We outsourced read the questionnaires to IID.
ED‐level factors
Site investigators filled out an ED‐level questionnaire assessing the rural–urban distinction, type of institute, practice style, management, shift type, overtime work, and the number of hospital beds, ED beds, daily walk‐in ED visits, daily ambulance ED visits, full‐time EPs, and full‐time female EPs. Rural and urban distinctions were made according to the criteria of the Japanese Ministry of Land, Infrastructure, Transport, and Tourism. 7
The Japanese emergency medical system is based on a unique three‐level system. 8 , 9 In brief, the primary system includes institutions providing medical care at night and on holidays for mildly ill patients who can be safely discharged. The secondary system includes emergency medical care institutions for moderately ill patients requiring hospitalization. The tertiary system includes emergency medical service centers for severely ill patients who require intensive care and emergency surgery. Of the secondary and tertiary emergency medical system institutions, some hospitals accept only walk‐in patients, some accept ambulances, and some accept both. Therefore, some EPs work only at the ED, and some manage both the intensive care unit and general wards along with the ED.
EP‐level factors
Participants were asked to provide their age, sex, years of working after transitional internship, years of working in the ED, specialty, working hours per week, night shift, marital status, childcare, caregiving, and sleep period.
Maslach Burnout Inventory‐Human Services Survey
We added responses to the Maslach Burnout Inventory‐Human Services Survey (MBI‐HSS) items translated into Japanese by Mind Garden. The MBI‐HSS is a 22‐item questionnaire that evaluates the frequency with which human service employees experience feelings or attitudes across three domains: (1) EE, nine items; (2) DP, five items; and (3) PA, eight items. 10 All items are scored on a Likert scale from 0 to 6 (never to every day, respectively). For ease of comparison with previous studies, we summed the scores in each domain. 10 Based on previous studies, 11 , 12 we defined the degree (severe, moderate, mild) of each dimension of burnout using cutoff scores: EE: severe ≥27, moderate: 17–26, mild ≤16; DP: severe ≥10, moderate: 6–9, mild ≤5; and PA: severe ≤33, moderate: 34–39, mild ≥40. The principal investigator of this study procured a license from Mind Garden to administer the copyrighted survey.
Data analysis
The analysis was performed using the Stata/MP17 software (StataCorp LLC). Summary statistics for both EDs and EPs characteristics are presented as proportions and medians with interquartile ranges (IQR), as appropriate. We examined the associations of EDs‐level and EPs‐level factors with the MBI‐HSS scores. Multivariable logistic regression was used to control potential confounders among ED‐level (type of institute, practice style, shift type) and EP‐level (age, sex, working hours, night shift, childcare, sleep period) factors. Factors with high collinearity using Pearson's correlation coefficient were excluded. Missing data were also excluded. All p values were two‐tailed, and statistical significance was set at p < 0.05.
RESULTS
Participant characteristics
Of 326 physicians, 270 EPs (82.8%) responded to the questionnaire. Of these, 267 (81.9%) who completed the survey were enrolled in the study. The characteristics of the EDs are presented in Table 1. Of the EDs, 25.9% were located in urban areas, 62.9% were emergency medical service centers. The characteristics of the EPs are presented in Table 2. Approximately half of the EPs were 30 to 39 years old.
TABLE 1.
Emergency department characteristics.
| EDs (n = 27) | |
|---|---|
| Urban location | 7 (25.9) |
| Type of institute | |
| Emergency medical care institutions | 8 (29.6) |
| Emergency medical service centers | 17 (62.9) |
| Others a | 2 (7.4) |
| Practice style | |
| Ambulance only | 2 (7.4) |
| Walk‐in patients only | 0 |
| Both | 25 (92.5) |
| Management | |
| ED only (no bed management) | 5 (18.5) |
| ICU only | 3 (11.1) |
| General wards only | 2 (7.4) |
| All | 17 (62.9) |
| Shift type | |
| 2‐shift | 13 (48.1) |
| 3‐shift | 6 (22.2) |
| Overnight | 8 (29.6) |
| Overtime work | |
| None | 2 (7.4) |
| <1 h | 7 (25.9) |
| 1–3 h | 17 (62.9) |
| >3 h | 1 (3.7) |
| No. of hospital beds | |
| <500 | 10 (37.0) |
| 500–1000 | 16 (59.2) |
| 1000< | 1 (3.7) |
| No. of ED beds | |
| <5 | 0 |
| 5–10 | 17 (62.9) |
| 10< | 10 (37.0) |
| No. of daily walk‐in ED visits, average | |
| <20 | 8 (29.6) |
| 20–50 | 10 (37.0) |
| >50 | 9 (33.3) |
| No. of daily ambulance ED visits, average | |
| <10 | 8 (29.6) |
| 10–30 | 16 (59.2) |
| >30 | 3 (11.1) |
| No. of full‐time EPs, median [IQR] | 11 [6–16] |
| No. of full‐time female EPs, median [IQR] | 2 [1–3] |
Note: Data are expressed as n (%) unless otherwise specified.
Abbreviations: ED, emergency department; EP, emergency physician; ICU, intensive care unit; IQR, interquartile range.
A general hospital and a pediatric medical center provided ED.
TABLE 2.
Emergency physician characteristics.
| Emergency physicians (n = 267) | |
|---|---|
| Age | |
| 25–29 | 46 (17.2) |
| 30–39 | 134 (50.1) |
| 40–49 | 58 (21.7) |
| ≥50 | 29 (10.8) |
| Male | 214 (80.1) |
| Years of working after transitional internship | |
| 3–4 | 44 (16.4) |
| 5–9 | 81 (30.3) |
| ≥10 | 141 (52.8) |
| Missing | 1 (0.3) |
| Years of working in the emergency department | |
| <3 | 80 (29.9) |
| 3–4 | 38 (14.2) |
| 5–9 | 53 (19.8) |
| ≥10 | 94 (35.2) |
| Missing | 2 (0.7) |
| Specialty | |
| Emergency medicine | 238 (89.1) |
| Others | 28 (10.4) |
| Missing | 1 (0.3) |
| Working hours per week, median [IQR] | 45 [40–55] |
| Night shift | |
| Yes | 236 (88.3) |
| Times per month, median [IQR] | 5 [3–7] |
| No | 30 (11.2) |
| Missing | 1 (0.3) |
| Marital status | |
| Married | 211 (79.0) |
| Single | 52 (19.4) |
| Missing | 4 (1.49) |
| Childcare | |
| Yes | 149 (55.8) |
| No | 118 (44.1) |
| Caregiving | |
| Yes | 8 (3.0) |
| No | 259 (97.0) |
| Sleep period | |
| ≥6 | 131 (49.0) |
| 3–6 | 136 (50.9) |
| <3 | 0 |
Note: Data are expressed as n (%) unless otherwise specified.
Abbreviation: IQR, interquartile range.
MBI‐HSS
Among the 267 respondents, 43 (16.1%), 53 (19.8%), and 179 (67.0%) EPs scored severe EE, DP, and PA, respectively; and 24 EPs (8.9%) scored severe in all three domains. Table 3 shows a comparison of this study with studies conducted in other countries. 13 , 14
TABLE 3.
Comparison this study with other studies in other countries.
| This study | Takayesu et al. 13 | Legassie et al. 14 | |
|---|---|---|---|
| (n = 267) | (n = 218) | (n = 48) | |
| Emotional exhaustion | |||
| Severe | 43 (16.1%) | 72 (33.0%) | 14 (29.2%) |
| Moderate | 81 (30.3%) | 82 (37.6%) | 15 (31.3%) |
| Mild | 143 (53.5%) | 64 (29.3%) | 19 (39.6%) |
| Depersonalization | |||
| Severe | 53 (19.8%) | 128 (58.7%) | 26 (54.2%) |
| Moderate | 44 (16.4%) | 51 (23.3%) | 9 (18.8%) |
| Mild | 170 (63.6%) | 38 (17.4%) | 13 (27.1%) |
| Personal accomplishment | |||
| Severe | 179 (67.0%) | 129 (59.1%) | 15 (31.3%) |
| Moderate | 32 (11.9%) | 56 (25.6%) | 20 (41.7%) |
| Mild | 56 (20.9%) | 30 (13.7%) | 13 (27.1%) |
Factors associated with MBI‐HSS scores
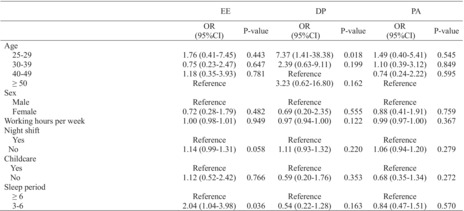
Table 4 shows ED‐level factors associated with MBI‐HSS scores. ED‐level factors compared between institutions showed that emergency medical service centers were significantly associated with severe PA scores (odds ratio [OR], 10.56; 95% confidence interval [CI], 1.78–62.66; p = 0.009). Table 5 shows the EP‐level factors associated with MBI‐HSS scores. In terms of EPs‐level factors, compared to more than 6 h, 3 to 6 hour‐sleep period was associated with more severe EE scores (OR, 2.04; 95% CI, 1.04–3.98; p = 0.036). Compared to EPs in their forties, EPs in their twenties were associated with severe DP scores (OR, 7.37; 95% CI, 1.41–38.38; p = 0.018).
TABLE 4.
Emergency departments‐level factors associated with the Maslach Burnout Inventory‐Human Services Survey scores.
| EE | DP | PA | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | |
| Type of institute | ||||||
| Others (included emergency medical care institutions) | Reference | Reference | Reference | |||
| Emergency medical service centers | 0.57 (0.08–4.11) | 0.582 | 2.41 (0.75–7.67) | 0.135 | 10.56 (1.78–62.66) | 0.009 |
| Practice style | ||||||
| Ambulance only | Reference | Reference | Reference | |||
| Ambulance and walk‐in patients | 0.98 (0.11–8.30) | 0.992 | 0.47 (0.10–2.15) | 0.334 | 0.63 (0.11–3.49) | 0.601 |
| Shift type | ||||||
| 2‐shift | Reference | Reference | Reference | |||
| 3‐shift | 0.80 (0.17–3.70) | 0.776 | 0.76 (0.24–2.40) | 0.644 | 2.83 (0.63–12.54) | 0.170 |
| Overnight | 0.28 (0.04–1.94) | 0.199 | 0.75 (0.22–2.46) | 0.640 | 0.61 (0.11–3.24) | 0.562 |
Abbreviations: CI, confidence interval; DP, depersonalization; EE, emotional exhaustion; OR, odds ratio; PA, personal accomplishment.
TABLE 5.
Emergency physicians‐level factors associated with the Maslach Burnout Inventory‐Human Services Survey scores.
| EE | DP | PA | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | OR (95% CI) | p‐Value | |
| Age, years | ||||||
| 25–29 | 1.76 (0.41–7.45) | 0.443 | 7.37 (1.41–38.38) | 0.018 | 1.49 (0.40–5.41) | 0.545 |
| 30–39 | 0.75 (0.23–2.47) | 0.647 | 2.39 (0.63–9.11) | 0.199 | 1.10 (0.39–3.12) | 0.849 |
| 40–49 | 1.18 (0.35–3.93) | 0.781 | Reference | 0.74 (0.24–2.22) | 0.595 | |
| ≥50 | Reference | 3.23 (0.62–16.80) | 0.162 | Reference | ||
| Sex | ||||||
| Male | Reference | Reference | Reference | |||
| Female | 0.72 (0.28–1.79) | 0.482 | 0.69 (0.20–2.35) | 0.555 | 0.88 (0.41–1.91) | 0.759 |
| Working hours per week | 1.00 (0.98–1.01) | 0.949 | 0.97 (0.94–1.00) | 0.122 | 0.99 (0.97–1.00) | 0.367 |
| Night shift | ||||||
| Yes | Reference | Reference | Reference | |||
| No | 1.14 (0.99–1.31) | 0.058 | 1.11 (0.93–1.32) | 0.220 | 1.06 (0.94–1.20) | 0.279 |
| Childcare | ||||||
| Yes | Reference | Reference | Reference | |||
| No | 1.12 (0.52–2.42) | 0.766 | 0.59 (0.20–1.76) | 0.353 | 0.68 (0.35–1.34) | 0.272 |
| Sleep period, hours | ||||||
| ≥6 | Reference | Reference | Reference | |||
| 3–6 | 2.04 (1.04–3.98) | 0.036 | 0.54 (0.22–1.28) | 0.163 | 0.84 (0.47–1.51) | 0.570 |
Abbreviations: CI, confidence interval; DP, depersonalization; EE, emotional exhaustion; OR, odds ratio; PA, personal accomplishment.
DISCUSSION
In this survey on burnout among 267 EPs working at 27 Japanese EDs, 8.9% scored severely in all three domains of MBI‐HSS. Multivariate analysis showed that emergency medical service centers were associated with severe PA scores. Additionally, a 3–6 hour‐sleep period was associated with more severe EE scores, and EPs in their twenties were associated with more severe DP scores. To the best of our knowledge, this is the first study to conduct a burnout survey among Japanese EPs.
The prevalence of burnout among EPs varies widely ranging from 25% to 77% in published literature. 6 Although the MBI‐HSS is not an appropriate tool to identify burnout, severe scores in EE, DP, and PA indicate higher degrees of burnout. 10 Another study reported that 28% of Japanese transitional interns were in a state of burnout. 15 As we showed in Table 3, a smaller number of Japanese EPs in our study experienced high degrees of burnout. In particular, EPs in our study had milder scores than that of other studies in terms of EE and DP. In contrast, the findings of this study were more severe than that of other studies in terms of PA. Maslach et al. 10 indicated country‐level differences in response to the MBI. Therefore, some difference in our results may have been caused by modesty, distinct Japanese character, which do not express negative feelings (e.g., anger, disgust) well, 16 or low self‐esteem.
Additionally, we found that EPs who worked at emergency medical service centers tended to score low in PA, and frequently encountered life‐threatening situations and death. Therefore, the nature of their work might make them feel helpless, therefore, leading to low self‐esteem. A previous study showed that PA scores were associated with the Clance Impostor Scale, which indicates impostor syndrome. 14 Impostor syndrome is characterized by feelings of self‐doubt and fear of being discovered as an intellectual fraud. 17 It is associated with negative mental health effects, including but not limited to anxiety, depression, neuroticism, and low self‐esteem. 18 The prevalence of impostor syndrome among medical students and professionals varies widely in published literature, between 22.5% and 46.6%. 18 Medical students and professionals feel shame in several situations, such as at conferences, during reports, rounds, and when receiving feedback. 18 These experiences may affect their mental health, leading to impostor syndrome. The present study did not assess the Clance Impostor Scale, therefore, we cannot conclude that the EPs, scoring severely in PA, may have been experiencing impostor syndrome. Therefore, to more accurately assess the mental health of EPs, future studies should focus on low self‐esteem.
We found that a 3‐ to 6‐h sleep period was associated with severe EE scores. A previous study showed that sleep loss is associated with burnout. 3 Additionally, <6 h of sleep impairs neurobehavioral functions. 19 Therefore, to prevent burnout, it is very important for EPs to ensure more than 6 h of sleep.
We found that EPs in their twenties were associated with severe DP scores, compared to EPs in their forties. We excluded factors, such as years working after transitional internships and years working at the ED that had high collinearity; however, it is suggested that less clinically experienced EPs have increased risks of severe DP scores. This finding is consistent with that of a previous study that showed that residents scored more severe in DP than that in EE. 14 Therefore, DP attitudes may have emerged as an attempted coping strategy during the development of burnout. 14 Residents with anxiety in clinical management had a significantly higher prevalence of burnout. 13 In an attempt to prevent burnout in young EPs, it is very important to improve the workplace environment to reduce undue worries, for example employing additional staffing mentors and supporting clinical practices.
Potential limitations
This study has several key limitations. First, we could not verify whether the participants were actually experiencing burnout. As previously described, MBI‐HSS is not appropriate for identifying burnout. However, MBI‐HSS is the most frequently used assessment tool that can suggest burnout, and therefore, we used it to tentatively assess the burnout situation, similar to other studies. 6 Second, this was an observational study that did not examine the direct causal relationship between burnout and factors. However, as previously described, this is the first study to report a burnout survey among Japanese EPs. This is a meaningful study to clarify factors associated with burnout. Third, we could not determine how the COVID‐19 pandemic affected this survey. The survey period, June 2021, was during COVID‐19 pandemic in Japan. Before the COVID‐19 pandemic, no study had described burnout in EPs in Japan. Therefore, we could not compare this study with other studies before the COVID‐19 pandemic in Japan. The COVID‐19 pandemic may have significantly affected the stress levels of EPs. Finally, we studied only 27 EDs, which suggest selection bias. Of these, 60% were emergency medical service centers, which constitute only 5.9% of emergency medical care institutions in Japan. 20 However, the EDs that were enrolled in this study were selected from every region of Japan, and therefore, we suggest that this study may have accurately reflected the actual situation of Japanese EPs.
CONCLUSIONS
In this multicentric survey of 267 Japanese EPs, 8.9% of Japanese EPs are in higher degrees of burnout. In particular, Japanese EPs scored more in terms of PA. To avoid burnout in Japanese EPs, it is important to improve the working environment, such as ensuring more than 6 h of sleep, and providing more support systems for younger EPs. Furthermore, the system needs to take effective action to prevent the development of low self‐esteem among them. To maintain pride in their work as front‐line physicians, ED supervisors need to do more to address the burnout rates of EPs.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interest for this article.
ETHICS STATEMENT
Approval of the Research Protocol: The Institutional Review Board of Juntendo University Urayasu Hospital approved the study (approval no. 2020–067).
Informed Consent: Informed consent was obtained from all the participants who responded to the questionnaire.
Registry and the Registration no. of the study: Not applicable.
Animal studies: Not applicable.
ACKNOWLEDGMENTS
We thank the site principal investigators and EPs working at following sites: Yusuke Hagiwara, MD, MPH (Tokyo Metropolitan Children's Medical Center, Tokyo); Masako Hata, MD (Hiroshima City Hiroshima Citizens Hospital, Hiroshima); Seiji Hirota, MD (Japanese Red Cross Kochi Hospital, Kochi); Tetsuya Hoshino, MD (University of Tsukuba Hospital, Ibaraki); Jin Irie, MD (Hirosaki University Hospital, Aomori); Kei Jitsuiki, MD, PhD (Juntendo University Shizuoka Hospital, Shizuoka); Yoichi Kato, MD (Japanese Red Cross Kumamoto Hospital, Kumamoto); Yoshimi Kitagawa, MD, PhD (Nagoya Ekisaikai Hospital, Aichi); Kentaro Kobayashi, MD (National Center for Global Health and Medicine, Tokyo); Yusuke Kodama, MD (Kyoritsu General Hospital, Aichi); Satoru Matsushima, MD (Chutoen General Medical Center, Shizuoka); Toshifumi Miki, MD (Chikamori Hospital, Kochi); Kingo Nishiyama, MD, PhD (Kochi Medical School Hospital, Kochi); Nobuhiro Sato, MD, MPH, PhD (Niigata City General Hospital, Niigata); Yasuyuki Sumida, MD (Rakuwakai Otowa Hospital, Kyoto); Hiroki Takami, MD, (Juntendo University Nerima Hospital, Tokyo); Kotaro Takebe, MD (North Medical Center Kyoto Prefectural University of Medicine, Kyoto); Yukitoshi Toyoda, MD, PhD (Saiseikai Yokohamashi Tobu Hospital, Kanagawa); Seiichiro Tsuzuki, MD (Fujita Health University Okazaki Medical Center, Aichi); Naoki Yamada, MD (University of Fukui Hospital, Fukui); Ichita Yamamoto, MD (Okinawa Prefectural Chubu Hospital, Okinawa); Kochi Health Sciences Center, Nagoya University Hospital, and institutions that authors belong to.
Morikawa M, Uechi T, Hanaki N, Goto Y, Funakoshi H, Takeuchi S, et al. Burnout among Japanese emergency medicine physicians: A multicentric questionnaire study. Acute Med Surg. 2023;10:e848. 10.1002/ams2.848
DATA AVAILABILITY STATEMENT
The data are not available due to privacy restrictions.
REFERENCES
- 1. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. [DOI] [PubMed] [Google Scholar]
- 2. Krall EJ. Ten commandments of physician wellness. Clin Med Res. 2014;12:6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stehman CR, Testo Z, Gershaw RS, Kellogg AR. Burnout, drop out, suicide: physician loss in emergency medicine, Part I. West J Emerg Med. 2019;20:485–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ministry of Health, Labour and Welfare . Number of Physicians and Dentists in Healthcare Facilities by Department. Handbook of Health and Welfare Statistics; Part 2. 2021. Table 2–45. Available from: https://www.mhlw.go.jp/english/database/db‐hh/2‐2.html.
- 5. Fire and Disaster Management Agency . Overview of the 2019 white paper on fire service. 2023. [cited 2023 Feb 7]; Available from: https://www.kaigai‐shobo.jp/files/fireserviceinjapan/20210301_White_paper02_eng.pdf.
- 6. Boutou A, Pitsiou G, Sourla E, Kioumis I. Burnout syndrome among emergency medicine physicians: an update on its prevalence and risk factors. Eur Rev Med Pharmacol Sci. 2019;23:9058–65. [DOI] [PubMed] [Google Scholar]
- 7. National spatial strategy (national plan) . Ministry of Land Infrastructure Transport and Tourism. [cited 2023 Feb 7]; Available from: https://www.mlit.go.jp/common/001127196.pdf
- 8. Hori S. Emergency medicine in Japan. Keio J Med. 2010;59:131–9. [DOI] [PubMed] [Google Scholar]
- 9. Ministry of Health Labour and Welfare . Summary of Static/Dynamic Surveys of Medical Institutions and Hospital Report. 2023. [cited 2023 Feb 7]; Available from: https://www.mhlw.go.jp/english/database/db‐hss/dl/Definitions_2017.pdf
- 10. Christina Maslach SEJ, Leiter MP. Maslach burnout inventory manual. 4th ed. California: Mind Garden, Inc.; 2018. [Google Scholar]
- 11. Doulougeri K, Georganta KGA, Montgomery A. “Diagnosing” burnout among healthcare professionals: can we find consensus? Cogent Med. 2016;3:1237605. [Google Scholar]
- 12. Shanafelt TD, West CP, Dyrbye LN, et al. Changes in burnout and satisfaction with work‐life integration in physicians during the first 2 years of the COVID‐19 pandemic. Mayo Clin Proc. 2022;97:2248–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kimo Takayesu J, Ramoska EA, Clark TR, et al. Factors associated with burnout during emergency medicine residency. Acad Emerg Med. 2014;21:1031–5. [DOI] [PubMed] [Google Scholar]
- 14. Legassie J, Zibrowski EM, Goldszmidt MA. Measuring resident well‐being: impostorism and burnout syndrome in residency. J Gen Intern Med. 2008;23:1090–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Matsuo T, Takahashi O, Kitaoka K, Arioka H, Kobayashi D. Resident burnout and work environment. Intern Med. 2021;60:1369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Safdar S, Friedlmeier W, Matsumoto D, et al. Variations of emotional display rules within and across cultures: a comparison between Canada, USA, and Japan. Can J Behav Sci. 2009;41:1–10. [Google Scholar]
- 17. Clance PR, Imes S. The impostor phenomenon in high achieving women: dynamics and therapeutic intervention. Psychotherapy SA I. 1978;15:241–7. [Google Scholar]
- 18. Thomas M, Bigatti S. Perfectionism, impostor phenomenon, and mental health in medicine: a literature review. Int J Med Educ. 2020;11:201–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose‐response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. [DOI] [PubMed] [Google Scholar]
- 20. Ministry of Health Labour and Welfare . Summary of Static/Dynamic Surveys of Medical Institutions and Hospital Report. [cited 2023 Feb 7]; Available from: https://www.mhlw.go.jp/english/database/db‐hss/dl/Survey_of_Medical_Institutions_2017.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are not available due to privacy restrictions.


