Abstract
Aim:
The objective of the parent study was to examine attitudes and experiences regarding counselling about preconception care among Black and/or Latina women in the United States with type 2 diabetes (T2DM). Here, we present emergent findings from a secondary analysis of caregiving.
Methods:
In this qualitative descriptive study, we used conventional content analysis to identify themes from semi-structured interviews with 32 Black and/or Latina women ages 18–40 who have T2DM in the United States recruited from online platforms and snowball sampling.
Results:
Caregiving responsibilities both motivate and disrupt diabetes self-management behaviours. Caregiving largely meant taking care of children, but women also had responsibilities to adult family members and romantic partners. Women were motivated to manage their diabetes in order to prevent negative health effects on their children and to stay healthy so they could fulfil caregiving responsibilities. However, caregiving competed for time, energy and money with self-management. Struggling to balance caregiving and self-management caused stress that women felt was intrinsically unhealthy and undermined self-management.
Conclusions:
Young adult women with T2DM identified different ways that the roles and responsibilities in the family could affect their diabetes self-management. Providers and policymakers should develop health-promoting interventions that accommodate caregiving responsibilities.
Keywords: diabetes mellitus, financial stress, minority health, psychological stress, self-management, type 2, women
1 |. INTRODUCTION
Globally, more than 422 million adults have diabetes.1 Reducing the risk of disease progression and complications requires the performance of numerous daily self-management behaviours, which include adherence to a specified diet, exercise routines, blood glucose testing and medication administration.2 For individuals capable of pregnancy, elevated blood glucose threatens to cause obstetrical complications, including fetal malformation and pregnancy loss, which can be prevented by optimising self-management with preconception care (care before conception).2,3 When we conducted a qualitative study about women’s attitudes and experiences with preconception care (paper currently under review), themes about caregiving emerged as important barriers and facilitators to diabetes self-management generally. Here, we present findings from a secondary analysis of being a family caregiver.
Family engagement by spouses of adults with diabetes or parents of children with diabetes can both help and harm diabetes self-management,4 and interventions to encourage more family engagement can enhance engagement in health behaviours.5 In families, being a caregiver, defined conventionally as ‘a person who provides direct care (as for children, elderly people, or the chronically ill)’, is common among women of reproductive age.6 Approximately 35 million women in the United States are caring for children under 18, with a quarter reported being single parents.7 These parenting roles are likely to become an increasingly common experience as type 2 diabetes (T2DM) onset is rapidly increasing in young adulthood.7 Furthermore, caregiving duties may extend beyond parenting; for example, relative to men, women are disproportionally caregivers for ageing parents.8 While previous research has addressed how family members can support an individual with diabetes, a gap in the literature exists concerning the impact of being a family caregiver on the self-management of the individual who has diabetes.4,5 To address this gap, our objective is to present findings about women’s perceptions of the relationship between their diabetes self-management and their experiences of caregiving.
2 |. METHODS
This is a qualitative descriptive study with naturalistic inquiry approaches appropriate for the exploration of the poorly understood phenomena.9 We performed all study procedures remotely due to COVID-19 restrictions. We conducted online recruitment by posting advertisements on the online classified advertisement platform Craigslist in the northeastern United States (New York, New Jersey and Connecticut), Columbia University’s participant recruitment platform and snowball sampling. Women who were interested in the study contacted us, and we assessed eligibility (Figure 1).
FIGURE 1.
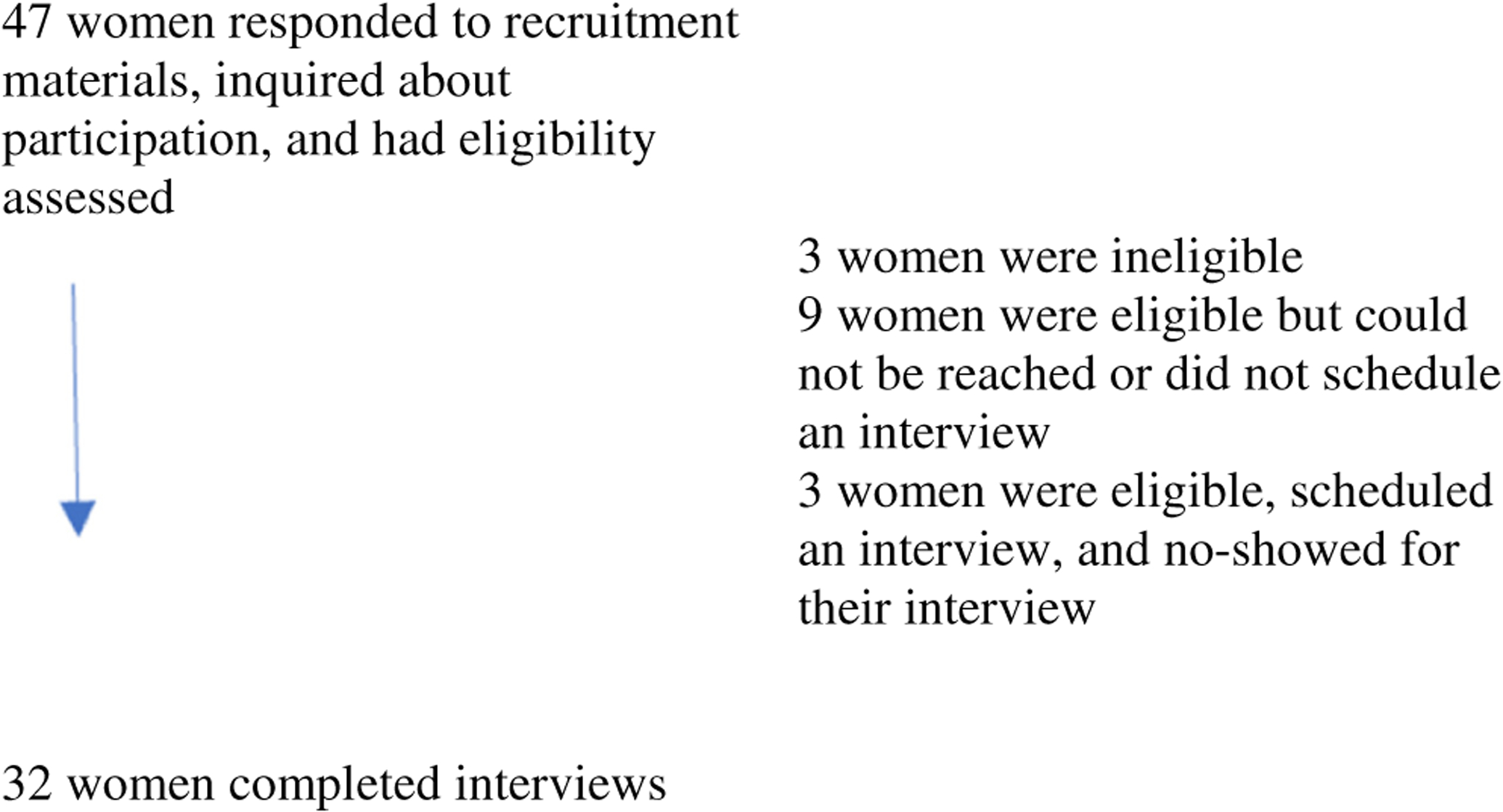
Enrollment flow diagram.
We purposively sampled (1) English-speaking women ages 18–40 years old, (2) with self-reported type 2 diabetes mellitus (T2DM) and (3) who self-identified as Black and/or Latina, because their communities are disproportionately affected by diabetes morbidity and mortality.10 Study personnel responded to interested potential participants by phone to provide a full description of the study, answer questions, assess eligibility, and obtain informed consent. We used a structured questionnaire to collect demographic information and we administered the 17-item Diabetes Distress Scale (α = 0.93) and the 10-item Perceived Stress Scale (α = 0.70) to characterise the levels of psychological distress related to managing diabetes and stress generally among women in our sample.11,12 Participants next completed an audio-recorded semi-structured interview (average length 48 minutes). We used an interview guide that we developed iteratively with expert assessment, internal testing and field-testing to confirm clarity and appropriateness, guided by best practices (sample questions in Table 1).13,14 Audio recordings were professionally transcribed. Concurrent with data collection, we analysed transcripts using a conventional content analysis approach.15 Three analysts (LB, OS and GK) read transcripts and used an iterative codebook to apply codes to the transcripts. All three analysts coded the first 10 interviews, and then alternating pairs completed the remainder. Disagreements in the analysis were reconciled via group discussion. We employed several of Guba’s strategies to enhance the rigour of our findings: peer debriefing and member-checking strengthened credibility, an ongoing debriefing reflexive practice to manage our personal biases to improve confirmability and maintaining an audit trail enhanced confirmability and dependability.16 Data were managed with NVivo 12 (QRS International). All study procedures were approved by the institutional review board of Columbia University.
TABLE 1.
Sample questions from the interview guide
| Question 1: I’d like to hear about your experience with diabetes. |
| Probes for Question 1 |
| * Can you tell me more about your diagnosis? |
| * Can you tell me more about how managing your diabetes is going? |
| * What’s been challenging? |
| * What does ‘being healthy’ mean to you? |
| * What goals do you have? |
| * What motivates you? |
3 |. RESULTS
We performed semi-structured interviews with 32 women (Table 2). Notably, over half of the participants (n = 18, 56.25%) were parenting at least one child. We included women without children in our analysis because they spoke about different types of caregiving responsibilities and community norms around caregiving. We identified two primary themes about how caregiving facilitates women’s diabetes self-management, and three primary themes about how caregiving impedes women’s diabetes self-management.
TABLE 2.
Participant characteristics (n = 32)
| Demographic characteristics of participants | ||
|---|---|---|
| Age, median (interquartile range (IQR)) | 34.5 years (29.75–38 years) | |
| Race and ethnicitya, n (%) | ||
| Latina | 7 | 21.9% |
| Latina and Black | 5 | 15.6% |
| Black | 20 | 62.5% |
| Educational attainment, n (%) | ||
| High school graduate or GEDb | 6 | 18.8% |
| Some college or associate’s degree | 7 | 21.9% |
| Bachelors degree or more | 19 | 59.4% |
| Health insurance, n (%) | ||
| Public | 21 | 65.6% |
| Private | 11 | 34.4% |
| Annual household income, n (%) | ||
| $20,000 or less | 4 | 12.5% |
| $21–50,000 | 13 | 40.6% |
| $50,000 or more | 15 | 46.9% |
| Currently working, n (%) | ||
| Yes | 12 | 37.5% |
| No—maternity leave | 6 | 18.8% |
| No—other reasons | 14 | 43.8% |
| Health characteristics of participants | ||
| Age of diabetes diagnosis, median (IQR) | 21.5 years (14–29.75 years) | |
| Duration of diabetes since diagnosis median (IQR) | 10 years (4.74–20 years) | |
| Most recent HbA1cc | ||
| 5.8%−7.5% | 8 | 25.0% |
| 7.51%−9.01% | 5 | 15.6% |
| 9.0%−15.0% | 14 | 43.8% |
| Do not know | 5 | 15.6% |
| Current management in addition to diet and exercise | ||
| None | 12 | 37.5% |
| Medication (not insulin) | 9 | 28.1% |
| Insulin (with or without other medications) | 11 | 34.4% |
| Diabetes distress scale (DDS)d, median (IQR) | 1.8 (1.1–2.7) | |
| Perceived stress scale (PSS)e, median (IQR) | 16 (10–22.75) | |
| Family characteristics of participants | ||
| Relationship status | ||
| Single or dating casually | 13 | 40.6% |
| Cohabitating | 7 | 21.9% |
| Married | 12 | 37.5% |
| Parenting status | ||
| Not parenting | 14 | 43.7% |
| Parenting one biological child | 10 | 31.3% |
| Parenting more than one biological child | 8 | 25.0% |
Of the Black participants, eight were born outside of the United States in Uganda, England, Ghana or Kenya. Of the Latina participants, one was born outside of the continental United States. Half of the Hispanic participants reported their family originated in Puerto Rico, while the other half reported that their families originated from Brazil, the Dominican Republic, Ecuador, Mexico, or Venezuela.
Tests of General Educational Development (GED) is an alternative to a traditional high school diploma in the United States.
HbA1c values converted to International Federation of Clinical Chemistry IFCC units: 5.8%–7.5% is IFCC 39.9–58.5 mmol/mol; HbA1c 7.51%–9.0% is 58.6–74.9 mmol/mol; 9.01%–15.0% is 75.0–140.0 mmol/mol.
Diabetes Distress Scale (DDS) values 1.9 or below indicate low diabetes distress, between 2.0 and 2.9 indicate moderate diabetes distress and 3.0 or above indicates high diabetes distress.12
Percieved Stress Scale (PSS) values 13 or below indicate low percieved stress, between 14 and 26 indicate moderate perceived stress and 27 and 40 indicate high perceived stress.11
4 |. HOW CAREGIVING FACILITATES SELF-MANAGEMENT
4.1 |. Motivated by the direct impact on fetal health and child health
Regardless of parenting status, women described a desire to have a healthy child as normative motivation for diabetes self-management during pregnancy. Women believed that diabetes self-management in pregnancy could prevent adverse outcomes. Notably, participants believed dutiful self-management could prevent their children from being born with a pediatric diagnosis of diabetes. Following a miscarriage, some women reframed self-management during subsequent pregnancies as a caregiving act, even when there were other children to tend to: ‘I would say, for me taking care of myself, I just planned for this. I realized from the second pregnancy I need to take care of myself despite the fact that the children are here, you have to continue taking care of yourself, but at the same time, be there for your children, take care of them’ (32 years old, Black and Latina, parenting).
After their children were born, women continued to fear that their children would develop diabetes and articulated a sense of responsibility to prevent this outcome. Some women were motivated to self-manage because they believed that they were role-modelling healthy eating and exercise habits for their children. One woman who was not yet a mother but hoped to be soon viewed self-management as cultivating skills and qualities she would need as a parent: ‘I feel like it gives me more patience, and more resilience. I think it would make it better, because if my child is sick, I would know there’s a medical team to call’ (27 years old, Black, not parenting). Viewed in this light, caregiving and self-management aligned and were mutually reinforcing.
4.2 |. Motivated by duty to care for others
Another source of motivation was the belief that women needed to be healthy enough to take care of their children. Some women recognised that hypoglycaemia symptoms, like dizziness or fainting, and hyperglycaemia symptoms, like fatigue and headaches, impeded their performance of caregiving duties. Others feared dying: ‘I’m just taking it more serious now, I’m trying not to die because, who’s going to take care of these kids when I’m gone? I’m trying to live for me and I’m trying to live so they can have a future’ (39 years old, Black, parenting).
Some women saw their self-management improve when they derived a greater sense of self-worth from their role in the family. Prioritizing motherhood was also a strategy for deflecting other social pressures that conflicted with diabetes self-management: ‘You want to have to keep yourself together and that will only start with you taking care of yourself, then taking care of the rest’ (30 years old, Black and Latina, parenting). When women felt guilty about prioritizing self-management, childrearing responsibilities were a justification that let them maintain an identity as a good person: ‘I have decided I put myself, like, always first… Even if you are told that you are selfish, you know you have a good heart. Tell yourself: I have a good heart. I have done so many things for people, … [and] if I don’t take care of myself, the child is not getting the best from me’ (35 years old, Black, parenting).
Caregiving fostered mutually supportive reciprocating relationships as children grew older. One participant had adolescent daughters who encouraged healthy eating and exercised with her. Support from adolescent children was particularly valuable to single mothers who had no other adults in the household. One woman, who was raising her three children alone, felt like her family was safer because she taught her adolescent son how to identify and respond to hypoglycemic episodes.
Although childrearing was the primary form of caregiving, other kinds of caregiving also emerged as motivating for some women, such as responsibility for pets: ‘I need to be healthy for them, you know, because I’ve had them for, since they were, you know, puppies and kittens. So especially since I don’t have children, they’re like my children. I want to be there for them’ (28 years old, Black and Latina, not parenting).
5 |. HOW CAREGIVING IMPEDES SELF-MANAGEMENT
5.1 |. Caregiving requires time, energy and money
Caregiving responsibilities for an infant posed particular challenges to diabetes self-management. ‘For a mum, I think they tend to overwork themselves and they forget to take care of themselves. They don’t have time to take care of their exercising or taking care of their bodies. They take care of other things and forget themselves’ (27 years old, Black, parenting). It was particularly difficult for women to exercise or plan meals if their baby had irregular sleep schedules or colic. All of the mothers in our sample saw themselves as their children’s primary caregivers with varying degrees of involvement from their partners. Some women asserted that they were only able to manage their diabetes in the post-partum period because of their partner’s help, whether that was taking on more childcare responsibilities or financing a childcare worker. For women with financial resources, childcare was conceptualised as a strategy for supporting diabetes self-management, creating time in which women could focus on exercise, meditation or other self-management practices. Other women expressed reluctance to ask their partners to take on more childcare responsibility because ‘you feel like you’re now becoming a burden’ (33 years old, Black and Latina, parenting).
In our sample, 18 of the 32 participants were caring for children under 18 years old. As women had more children, self-management became increasingly difficult. Women with and without children affirmed that caring for children was a widely experienced phenomenon that drew time, energy and money away from self-management. An additional four participants described some degree of responsibility for older family members and adult siblings: ‘Growing up, they say men are strong and they’re able to do all the heavy lifting and take care of the family. In reality, for me, it was always my mother and for me … When it comes to children, relationships, family. … it all comes down to the female taking care of the house, taking care of the family, the parents, making sure everything’s okay’ (39 years old, Latina, parenting). Some women felt pulled in two directions by pressure from their families both to care for family members, including parents and adult siblings and to adhere to a diabetes self-management regimen.
5.2 |. Concurrent self-management and caregiving create stress
Women were stressed when diabetes self-management and caregiving responsibilities competed for resources. The median score on the Perceived Stress Scale was 16 and on the Diabetes Distress Scale was 1.8, indicating moderate stress and low diabetes distress in this sample. Participants largely conceptualised mental health as a cornerstone of diabetes management and were concerned about the negative health impacts of stress. ‘You feel more stressed to try to balance your health, but also give yourself the self-care you need but also care for your children’ (21 years old, Black and Latina, not parenting). One woman emphasised the importance of managing her mental health to protect her child from her own negative emotions: ‘You’ll bring up a very broken child because of self-pity’ (32 years old, Black, parenting). For some women, a cycle emerged: the demands of diabetes self-management and the burden of diabetes symptoms exacerbated the typical stress of childrearing. Some women viewed their stress as detrimental to their children, and they believed that they had a responsibility to manage those feelings and felt guilty when they could not. Struggling with caregiver responsibilities could also impact their self-worth and consequentially, their self-management: ‘Because if you don’t consider yourself important, why are you going to prick your finger? If you know you shouldn’t be eating three slices of chocolate cake, but you’re depressed and you’re worried about bills and life and family or just even yourself?’ (38 years old, Black and Latina, not parenting). While some saw the stress, in itself, as harmful, others experienced stress as bad for their diabetes because those feelings made it harder to resist tempting foods. One woman said that
Stress is the key to basically any health problem. It’s stress. It’s just like you’re overwhelmed with so much stuff. These kids, the job, how do you have money, you have money, the food, just the area you live in, the people, the neighbors, family. Just all the medication you have to pay so much for. It’s just a lot of stuff and all that stuff becomes overwhelming. Sometimes you just sit down and you’re just like, oh, I’m so tired, you give up a little bit. But then you realize that, oh, I got to take care of these kids and make a good life for them. Then you get up and start all over again. But it’s stress, though, it’s stress. Then you start like you know you’re not supposed to eat no cake, no chocolate cake and coffee but you still do it anyway. So you’re failing in that aspect. Then when you feel like it you snap back out of it and then you don’t eat the junk food. It’s stress.
(39 years old, Black, parenting).
COVID-19 put more pressure on the precarious balance between diabetes self-management and caregiving for many women. Work furloughs exacerbated financial stress. Others faced a difficult choice: knowing that diabetes put them at risk for COVID-19 complications, they had to decide whether to stop working or to keep working in professions which involved a greater risk of COVID-19 exposure. If they were to get sick, then they would be unable to work. Working from home was stressful, especially for mothers concurrently caring for children home from daycare or school, and participants linked this stress to poor self-management behaviours. One mother, who was working fulltime remotely without help for her 2-year-old and kindergartener reported, ‘My stress level is through the roof… Whenever I’m stressed, I just don’t put myself first’ (40 years old, Black, parenting).
Women emphasised that balancing childcare and diabetes self-management could be particularly overwhelming in the post-partum period. One woman experiencing post-partum depression felt ‘worthless” and felt that she only existed to take care of her infant (35 years old, Black, parenting). As a result, she neglected her self-management until she began therapy and hired a nanny. Encouragement from peers, providers, and spouses normalised seeing a mental health counsellor. Women were also grateful when their partners helped them overcome logistical barriers to obtaining mental health services, which subsequently helped their diabetes self-management. Those who experienced stigma for seeking mental health treatment felt trapped.
Women identified stressors in both returning to work after maternity leave or extending their time out of the workforce. Women who worked outside the home were busy and stressed. One participant who stopped working to take care of herself and the baby viewed her choice as a sacrifice: ‘[Responsibility for a new baby] can even prevent you from working. Like the way you are doing some work, you will decide, ‘I don’t want [to do it] anymore.’ It’s overwhelming…. Yes. You could sacrifice work for you to manage diabetes and the baby’ (34 years old, Black, parenting). However, without her income, the family experienced more stress around finances, which in turn undermined her diabetes management. Another woman described how her career and the social world gave her a sense of identity; without it she experienced mood disruptions. ‘Every day you up -- the same thing, the same thing and not even recognizing your efforts, you know?’ (35 years old, Black, parenting). She described how her depressed mood led to her the neglect of her diabetes.
5.3 |. Problematic caregiving relationships
Caregiving of adult family members or romantic partners undermined some women’s diabetes self-management. A ‘toxic relationship’ was one in which ‘they don’t even have time to take care of themselves’ (27 years old, Black, parenting). Changing their role in that relationship could be pivotal for improving diabetes self-management and optimising glycaemia. For some, breakups were turning points:
I was also in a pretty toxic relationship almost all throughout college and just had a breakup this time last year, which was when I started to properly manage my health, to take my diet and exercising into my own hands, and try to particularly work on everything that was stopping me from taking care of my own health. … I was putting that energy towards myself for once.
(22 years old, Latina, not parenting)
Some women extracted themselves from relationships with unhealthy caregiving dynamics. Normative transitions, such as leaving the household to go to college, could provide a break but did not necessarily resolve the family dynamic.
In general, just the type of person I am, I have more care about my dad’s health, ultimately than myself. … it’s sometimes good that I live away from home while I’m in college, because then I can truly focus on my health. But when I’m back home, it’s just a lack of control I feel like I have over (1) what I eat, and then (2), just my own self-care. I feel like I can’t upkeep it, really.
(21 years old, Black and Latina, not parenting)
6 |. DISCUSSION
We found that caregiving can motivate women to stay healthy while also impeding the performance of diabetes self-management activities. Our qualitative inquiry provides a rich explanation for the ways that caregiving and self-management exert bidirectional influences on each other. Our findings contribute to a fuller understanding of the literature about how family affects chronic illness management.4,5,17
When caregiving responsibilities were overwhelming, women described stress and mental health symptoms that impeded the performance of self-management behaviours, which places the woman at risk of being labelled ‘non-adherent’, a stigmatising label that is used more in the electronic health records of Black adults compared to White adults.18 Our findings underscore the importance of investigating competing responsibilities rather than blaming the individual. For example, responsibility for feeding a family may both exhaust a woman’s time19 for meal planning, shopping, cooking and cleaning as well as lower the financial threshold for food insecurity which, in turn, can both interfere with adherence to self-management regimen based on a diet.20 Our findings also suggest that adherence to self-management regimens is particularly difficult in the post-partum period, consistent with previous research which has found that after delivery, women with gestational diabetes focus on infant care, forgoing T2DM prevention and screening.21 It is worth noting that our study was conducted during the COVID-19 pandemic when the responsibility for childcare and household management disproportionately fell to women.19 Our participants with small children described their stressful struggles to fulfil their professional, domestic, and self-management responsibilities when they were unable to outsource childcare.
Caregiving responsibilities may partially explain sex and gender differences observed in adherence and responses to adherence interventions.22,23 For example, compared to men with diabetes, women with diabetes have higher relative cardiovascular disease mortality risk which has been linked to lower rates of medication adherence and self-management.22 Our findings show one way that women are experiencing the observation in the philosophy of ethics that the responsibility to the ‘other’ precedes the centrality of the ‘self’.24 Our participants experienced socially enforced gendered caregiving obligations and navigated decisions about whether to devote their limited time, energy and money to caregiving for others or self-management. Our participants feared that if they prioritized diabetes self-management over caregiving, they would be viewed as selfish or neglectful and were concerned they would be penalised by their communities. Tellingly, participants described improving self-management and optimising glycaemia when they ended ‘toxic’ romantic relationships or established new boundaries with demanding extended family members. However, these changes came at a cost: some participants experienced (or feared) destabilization of a social network that they valued and needed to survive. Our findings suggest the value of considering cultural norms about gendered responsibility in the delivery of clinical care to women. Future intervention development may also benefit from a strengths-oriented perspective and consider ways to leverage the motivation, skills, social connectedness, and self-worth that caregiving can foster.
Our findings suggest that policy interventions to reduce the financial, logistical and emotional challenges of caregiving may have a positive impact on diabetes self-management and clinical outcomes. We recommend that future research investigate the health impact and cost-savings of programs that help with caregiving, such as unconditional cash transfers or universal guaranteed income. One model for how to evaluate the health impacts of anti-poverty interventions is the Baby’s First Years study, which examines the health impact of providing unconditional cash transfers to low-income parents in the general population in the first three years of life.25 If this type of intervention were tested among women with diabetes, it could identify the cost-savings associated with the reduction in diabetes-related health complications, which are a major financial burden on health systems (for example, in the United States, diabetes costs the healthcare system over $111.2 billion dollars per year, almost half of which is through the public insurance, Medicaid26).
In addition, our findings highlight the importance of addressing mental health symptoms, decreasing mental health stigma and increasing both awareness of and access to mental health resources. Our findings underscore how critical it is to continue investigating the integration of mental healthcare into diabetes management, so that women’s self-management and care-seeking are not impeded by the intertwined stigmas against diabetes27 and, as was more prominent among our participants, stigma against mental health. Because caregiving responsibilities may make it logistically difficult for women to attend medical appointments, it will also be important to consider how to reduce the travel burden on this patient population by incorporating mental health services into primary care, increasing accessibility by telehealth, and offering a wide range of hours. This is particularly important because acute and chronic stresses—including those associated with self-management and caregiving strain – can cause blood glucose spikes as well as oxidative stress and chronic inflammation that can directly increase insulin resistance and inhibit beta cell function.28 To further reduce stress related to the mothering role, we may look to oncology for interventions that increase skills for reducing the childhood psychological distress that can emerge from parental chronic illness.29
6.1 |. Limitations
We note certain limitations. Because participants were recruited from the community, we cannot confirm their diabetes diagnosis. Since the objective of our parent study was to understand preconception care, and we did not provide a definition of caregiving to participants or ask them to define it, we may not have fully characterised the phenomenon of caregiving. Qualitative research, by design, is not intended to be generalizable therefore, we caution against extrapolating our findings outside the Northeast United States. By requiring that the interviews were conducted in English, we did not capture the impact that language barriers can have on self-management. Conceptually, we analyzed caregiving as a culturally normative experience in the lives of cisgender women. We see value in increasing knowledge about how cisgender men with intensive caregiving responsibility also manage their diabetes, both as fathers and in other capacities. We also encourage future research about chronic illness management experiences of transgender and gender non-conforming individuals who are also caregivers. Other limitations include selection bias in that those who responded to our recruitment material are possibly different from those who did not. In addition, our data may overstate caregiving as a motivator if our respondents answered in socially desirable ways that emphasised their caregiving behaviours. Lastly, we cannot rule out that the introduction of researcher bias. However, by using an iterative codebook, group consensus and team coding we likely reduced this risk sufficiently.
7 |. CONCLUSION
Diabetes is increasingly common in the stages of life where women are often caring for biological children as well as other individuals in their familial and social networks. Addressing the racial and ethnic inequities in diabetes necessitates greater insight into the experiences of individuals from communities that have disparately high rates of this chronic illness. Understanding how caregiving responsibilities compete for resources for diabetes self-management is crucial for tailoring policy-, provider- and individual-level intervention strategies to improve health and well-being.
Novelty statement.
Increasingly, women of reproductive age are diagnosed with type 2 diabetes, but little is known about how caregiving responsibilities—common in that stage of life—affect disease self-management.
This qualitative study found that caregiving responsibilities, particularly parenting, both enhanced women’s motivation for self-management and presented financial and logistical challenges to adherence to diet, exercise and medication regimens.
Care delivery may be enhanced by the development of treatment plans that take into consideration how caregiving responsibilities can positively influence psychological aspects of disease self-management but complicate personal health economics.
ACKNOWLEDGEMENTS
While conducting this study, Laura Britton was supported by the National Institutes of Health/National Institute of Nursing Research (NIH/NINR, T32NR007969, PI: Bakken). Dr. Britton also received funding from Sigma, Alpha Zeta chapter and the Rita and Alex Hillman Foundation. Dr. Marshall received support from the National Institutes of Health/National Institute on Minority Health and Health Disparities (NIH/NIMHD, K01MD016169, PI: Marshall). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH/NINR, NIH/NIMHD or other funders.
Funding information
National Institute of Nursing Research; National Institute on Minority Health and Health Disparities
Footnotes
CONFLICT OF INTEREST
Britton, Kaur, Zork and Marshall report no conflict of interest. George is a speaker and consultant for AstraZeneca, Genentech and Sanofi Regeneron Teva.
DATA AVAILABILITY STATEMENT
I confirm that my Data Availability Statement (pasted below) complies with the Expects Data Policy. Research data are not shared.
REFERENCES
- 1.World Health Organization. Global Report on Diabetes. 2016. https://www.who.int/publications/i/item/9789241565257. Accessed June 22, 2022.
- 2.American Diabetes Association. Standards of medical care in diabetes—2021. Diabetes Care. 2021;44:S21–S226. [Google Scholar]
- 3.National Institute for Health and Care Excellence. Diabetes in pregnancy: Management from preconception to the postnatal period. 2015. nice.org.uk/guidance/ng3. Accessed June 22, 2022. [PubMed]
- 4.Mayberry LS, Osborn CY. Family involvement is helpful and harmful to patients’ self-care and glycemic control. Patient Educ Couns. 2014;97(3):418–425. doi: 10.1016/j.pec.2014.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Torenholt R, Schwennesen N, Willaing I. Lost in translation-the role of family in interventions among adults with diabetes: a systematic review. Diabet Med. 2014;31(1):15–23. doi: 10.1111/dme.12290 [DOI] [PubMed] [Google Scholar]
- 6.Merriam Webster. Caregiver. https://www.merriam-webster.com/dictionary/caregiver. Accessed August 29, 2022.
- 7.Deputy NP, Kim SY, Conrey EJ, Bullard KM. Prevalence and changes in preexisting diabetes and gestational diabetes among women who had a live birth—United States, 2012–2016. MMWR Morb Mortal Wkly Rep. 2018;67(43):1201–1207. doi: 10.15585/mmwr.mm6743a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parker K, Patten E. The sandwich generation. 2013. https://www.pewresearch.org/social-trends/2013/01/30/the-sandwich-generation/. Accessed June 22, 2022.
- 9.Sandelowski M. What’s in a name? Qualitative description revisited. Res Nurs Heal. 2010;33(1):77–84. doi: 10.1002/nur.20362 [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. National diabetes statistics report, 2020.
- 11.Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (Korean Soc Nurs Sci). 2012;6(4):121–127. doi: 10.1016/j.anr.2012.08.004 [DOI] [PubMed] [Google Scholar]
- 12.Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful? Establishing cut points for the diabetes distress scale. Diabetes Care. 2012;35(2):259–264. doi: 10.2337/dc11-1572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res. 2009;18(9):1263–1278. doi: 10.1007/s11136-009-9540-9 [DOI] [PubMed] [Google Scholar]
- 14.Kallio H, Pietil A, Johnson M, Kangasniemi M. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72(12):2954–2965. doi: 10.1111/jan.13031 [DOI] [PubMed] [Google Scholar]
- 15.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 16.Guba EG. Criteria for assessing the trustworthiness of naturalistic inquiries. Educ Commun Technol. 1981;29(2):75–91. [Google Scholar]
- 17.Samuel-Hodge CD, Cene CW, Corsino L, Thomas C, Svetkey LP. Family diabetes matters: a view from the other side. J Gen Intern Med. 2013;28(3):428–435. doi: 10.1007/s11606-012-2230-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun M, Oliwa T, Peek ME, Tung EL. Negative patient descriptors: documenting racial bias in the electronic health record. Health Aff. 2022;41(2):203–211. doi: 10.1377/hlthaff.2021.01423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giurge LM, Whillans AV, Yemiscigil A. A multicountry perspective on gender differences in time use during COVID-19. Proc Natl Acad Sci U S A. 2021;118(12):e2018494118. doi: 10.1073/pnas.2018494118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilder ME, Kulie P, Jensen C, et al. The impact of social determinants of health on medication adherence: a systematic review and meta-analysis. J Gen Intern Med. 2021;36(5):1359–1370. doi: 10.1007/s11606-020-06447-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parsons J, Sparrow K, Ismail K, Hunt K, Rogers H, Forbes A. A qualitative study exploring women’s health behaviours after a pregnancy with gestational diabetes to inform the development of a diabetes prevention strategy. Diabet Med. 2019;36(2):203–213. doi: 10.1111/dme.13794 [DOI] [PubMed] [Google Scholar]
- 22.Harreiter J, Fadl H, Kautzky-Willer A, Simmons D. Do women with diabetes need more intensive action for cardiovascular reduction than men with diabetes? Curr Diab Rep. 2020;20(11):61. doi: 10.1007/s11892-020-01348-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chlebowy DO, Hood S, LaJoie AS. Gender differences in diabetes self-management among African American adults. West J Nurs Res. 2013;35(6):703–721. doi: 10.1177/0193945912473370 [DOI] [PubMed] [Google Scholar]
- 24.Levinas E. Totality and Infinity: Essay on Exteriority. Springer Science and Business Media; 1969. [Google Scholar]
- 25.Noble KG, Magnuson K, Gennetian LA, et al. Baby’s first years: design of a randomized controlled trial of poverty reduction in the United States. Pediatrics. 2021;148(4):e2020049702. doi: 10.1542/peds.2020-049702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–884. doi: 10.1001/jama.2020.0734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Celik A, Forde R, Racaru S, Forbes A, Sturt J. The impact of type 2 diabetes on women’s health and well-being during their reproductive years: a mixed-methods systematic review. Curr Diabetes Rev. 2021;18(2):15–20. doi: 10.2174/1573399817666210118144743 [DOI] [PubMed] [Google Scholar]
- 28.Luc K, Schramm-Luc A, Guzik TJ, Mikolajczyk TP. Oxidative stress and inflammatory markers in prediabetes and diabetes. J Physiol Pharmacol. 2019;70(6):809–824. doi: 10.26402/jpp.2019.6.01 [DOI] [PubMed] [Google Scholar]
- 29.Rauch PK, Muriel AC. The importance of parenting concerns among patients with cancer. Crit Rev Oncol Hematol. 2004;49(1):37–42. doi: 10.1016/S1040-8428(03)00095-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
I confirm that my Data Availability Statement (pasted below) complies with the Expects Data Policy. Research data are not shared.


