Dear Editor,
Cutaneous Rosai-Dorfman disease (C-RDD) is a rare histiocytic proliferation in the skin.[1] It presents with a varied spectrum of manifestations and confounding histological features. We report a case of C-RDD observed in our clinic.
A 52-year-old female patient presented with an asymptomatic, pink colored, raised lesion of size 4 × 5 cm over the junction of the left cheek and pre-auricular area for 2 months. The lesion started as a small, pin-head-sized lesion that progressed over 2 months into a firm, well-defined nodulo-plaque with surface nodularity and fine scaling [Figure 1a]. There was no pain, tenderness, or discharge from the lesion. A 5 mm sub-mental lymph node was seen on ultrasonography which was not amenable to fine needle aspiration cytology. Diascopy [Figure 2a] revealed multiple yellow-brown globules, suggestive of apple-jelly nodules. Dermoscopy [Figure 2b] also showed similar yellow-brown globules against an erythematous background along with scaling. We had differential diagnoses of atypical mycobacterial infection, angiolymphoid hyperplasia with eosinophilia, and cutaneous lymphoma. Tissue cultures for organisms were negative. Histopathology showed a dense and diffuse infiltrate of histocytes extending from papillary dermis to subcutis admixed with plenty of plasma cells, lymphocytes, and neutrophils [Figure 3a]. We empirically prescribed doxycycline and clarithromycin for 2 weeks. The patient reviewed with us after 4 months due to the COVID-19 pandemic. She had complete resolution of the lesion [Figure 1b]. A review of the histopathology revealed histiocytes that were larger, showing emperipolesis [Figure 3b] and S-100 positivity [Figure 4]. Based on the characteristic histological appearance and clinical response, we made a final diagnosis of C-RDD.
Figure 1.

(a) asymptomatic, firm, well-defined erythematous, nodulo-plaque with surface nodularity and fine scaling over the left pre-auricular area seen at baseline and (b) complete resolution of the lesion after 4 months
Figure 2.
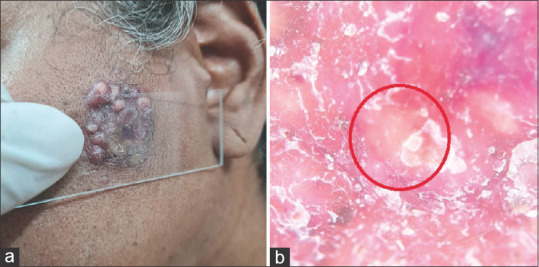
(a) Diascopy demonstrating multiple yellow-brown globules, suggestive of apple-jelly nodules. (b) Dermoscopy showing multiple yellow globules (red circle) against an erythematous background, suggestive of apple-jelly nodules, and scaling (DermLite DL200, 10×)
Figure 3.

Histopathological examination of the lesions showing (a) epidermal ulceration with dense inflammatory infiltrates in the entire dermis (H and E, 40×) consisting of (b) large histiocytosis with emperipolesis (black arrows) in a background of plasma cells, lymphocytes, and polymorphs (H and E, 400×)
Figure 4.

Immunohistochemistry showing S-100 positive histiocytes in the dermis (black arrows, S-100IHC, 400×)
C-RDD is commonly seen in females (1.5:1) and in the fifth decade.[2,3] The underlying pathogenesis of the C-RDD may be related to infections, immune deficiencies, genetic factors, or neoplasia. Around 43% of patients with RDD have extra-nodal involvement. The most common extra-nodal site involved is skin (11%). C-RDD presents as solitary or multiple, firm, infiltrated, red-to-brown, and nodulo-plaques. The lesions are usually asymptomatic. Superficial scaling is seen in some cases.[4] Rarely, they may present with ulceration, tenderness, or pruritus.
Dermoscopy reveals multiple foci of yellow discoloration against an erythematous background, as seen in our case.[5] In addition, branching vessels that are larger at the periphery and become thinner as they reach the center may be seen.[5] The tubers on a plaque appearance, often described as apple-jelly nodules in diascopy, is seen in granulomatous disorders like lupus vulgaris, lupoid leishmaniasis, sarcoidosis, lupoid rosacea, and pseudolymphoma. There is a paucity of information about the presence of apple jelly nodules in RDD.
Dermoscopic differentials for yellowish globules on an erythematous background include angiolymphoid hyperplasia with eosinophilia, sarcoidosis, and juvenile xanthogranuloma. A dermoscopic examination of angiolymphoid hyperplasia with eosinophilia reveals a polymorphous vascular pattern consisting of dotted and linear vessels on a pale red-to-pink background.[6] Sarcoidosis shows diffuse or localized structureless yellowish-orange areas with well-focused linear or branching vessels under a dermoscope.[7] In addition, follicular plugs, scar-like depigmentation, scaling, and pigmentation structures can be seen.[8] Dermoscopy of juvenile xanthogranuloma reveals multiple, polymorphous vessels and yellow globules against a diffuse orange-yellow background and surrounding erythema (setting-sun pattern).[9]
C-RDD is a dermal-based lesion with a nodular and poorly circumscribed infiltrate. The nodular dermal granulomas correlate with the yellow globules seen in diascopy and dermoscopy. Emperipolesis occurs in the form of an intact hematolymphoid cell within a vacuole or floating freely in the cytoplasm of a histiocyte. Plasma cells and neutrophils often present as micro-abscesses.
While the most effective treatment is excision, spontaneous resolution is also seen.[2] Treatment options include corticosteroids, methotrexate, dapsone, thalidomide, and isotretinoin. The presence of apple-jelly nodules in C-RDD is an interesting observation that may prove helpful for dermatologists.
Informed consent
Obtained.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol. 1969;87:63–70. [PubMed] [Google Scholar]
- 2.Al-Khateeb THH. Cutaneous Rosai-Dorfman disease of the face: A comprehensive literature review and case report. J Oral Maxillofac Surg. 2016;74:528–40. doi: 10.1016/j.joms.2015.09.017. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed A, Crowson N, Magro CM. A comprehensive assessment of cutaneous Rosai-Dorfman disease. Ann Diagn Pathol. 2019;40:166–73. doi: 10.1016/j.anndiagpath.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Lu C-I, Kuo T, Wong W-R, Hong H-S. Clinical and histopathologic spectrum of cutaneous Rosai-Dorfman disease in Taiwan. J Am Acad Dermatol. 2004;51:931–9. doi: 10.1016/j.jaad.2004.04.030. [DOI] [PubMed] [Google Scholar]
- 5.Wang F, Zhou H, Luo D-Q, Han J-D, Chen M-K. Dermatoscopic findings in cutaneous Rosai-Dorfman disease and response to low-dose thalidomide. J Dtsch Dermatol Ges. 2014;12:350–2. doi: 10.1111/ddg.12256. [DOI] [PubMed] [Google Scholar]
- 6.Akay BN, Fatih Atak M, Farabi B. Dermoscopic features of two cases of angiolymphoid hyperplasia with eosinophilia and review of the literature. Dermatol Pract Concept. 2021;11:e2021003. doi: 10.5826/dpc.1102a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loo Lim AY, Tang PY, Oh CC. Dermoscopy in cutaneous sarcoidosis. Dermatol Online J. 2021;27:14. doi: 10.5070/D327955144. [DOI] [PubMed] [Google Scholar]
- 8.Chauhan P, Adya KA. Dermatoscopy of cutaneous granulomatous disorders. Indian Dermatol Online J. 2021;12:34–44. doi: 10.4103/idoj.IDOJ_543_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta P, Vinay K, Bishnoi A, Chatterjee D, Dogra S. Dermatoscopy and clinicopathological correlation of juvenile xanthogranuloma in skin of colour:A series of six patients. J Eur Acad Dermatol Venereol. 2022;36:e884–6. doi: 10.1111/jdv.18319. [DOI] [PubMed] [Google Scholar]


