Abstract
Background & objectives:
Information on recent cancer statistics is important for planning, monitoring and evaluating cancer control activities. This article aims to provide an update on the cancer incidence estimates in India by sex, age groups and anatomical sites for the year 2022.
Methods:
The National Cancer Registry Programme Report 2020, reported the cancer incidence from 28 Population-Based Cancer Registries (PBCRs) for the years 2012-2016. This was used as the basis to calculate cancer estimates in India. Information pertaining to the population at risk was extracted from the Census of India (2001 and 2011) for the estimation of age–sex stratified population. PBCRs were categorised into the respective State and regions of the country to understand the epidemiology of cancer. The age-specific incidence rate for each specific anatomical site of cancer was applied to the estimated population to derive the number of cancer cases in India for 2022.
Results:
The estimated number of incident cases of cancer in India for the year 2022 was found to be 14,61,427 (crude rate:100.4 per 100,000). In India, one in nine people are likely to develop cancer in his/her lifetime. Lung and breast cancers were the leading sites of cancer in males and females, respectively. Among the childhood (0-14 yr) cancers, lymphoid leukaemia (boys: 29.2% and girls: 24.2%) was the leading site. The incidence of cancer cases is estimated to increase by 12.8 per cent in 2025 as compared to 2020.
Interpretation & conclusions:
The cancer incidence is continuing to increase in India. The new estimates will be helpful in planning cancer prevention and control activities through the intervention of early detection, risk reduction and management.
Keywords: Cancer, estimates, incidence, India, National Cancer Registry Programme, projection
According to the Global Cancer Observatory (GLOBOCAN) estimates, there were 19.3 million incident cancer cases worldwide for the year 20201. India ranked third after China and the United States of America2. GLOBOCAN predicted that cancer cases in India would increase to 2.08 million, accounting for a rise of 57.5 per cent in 2040 from 20202.
Planning, monitoring and evaluation of cancer control activities requires recent statistics in any region. This is usually achieved through the Population-Based Cancer Registries (PBCRs). Cancer is not a nationally notable disease in India. Thus, the data collection from PBCRs involves active retrospective data abstraction, laborious and a complex process of analysis and reporting. Trained registry staff typically go to different resource centers (hospitals, vital statistics departments and diagnostic laboratories) for collecting data on a standardized core form3. This delays the process of real-time reporting and bringing out the most recent cancer statistics. Globally, there is usually a lag of 2-4 yr between actual cancer registry data and the publication of results (e.g. US cancer registry, GLOBOCAN)3,4. Thus, providing estimates at periodic intervals is the best way for informing cancer prevention and control programmes. Hence, efforts to provide timely cancer estimates based on the recently available data for formulating appropriate cancer control measures are proposed5,6.
In India, the systematic collection of data on cancer through the PBCRs and Hospital-Based Cancer Registries is in existence since 1981 under the National Cancer Registry Programme (NCRP), National Centre for Disease Informatics and Research (NCDIR) of the Indian Council of Medical Research (ICMR-NCDIR), Bengaluru.
One of the primary objectives of NCRP is to generate reliable data on the magnitude and patterns of cancer in India and provide future estimates. Our previous publication estimated 1.39 million new (incident) cancer cases in the year 20205. The present article is aimed to provide detailed estimates of cancer incidence in India by sex, age groups and anatomical sites for the year 2022 and the projected rise in cases for 2025, using the same datasets and methodology5. In addition, five-year and broad age group-wise cancer estimates were also calculated for the year 2022. Noticeably, GLOBOCAN followed a similar approach for 2020 after publishing the 2018 cancer estimates1,7.
Material & Methods
The present study was carried out at ICMR-National Centre for Disease Informatics & Research, Bengaluru, Karnataka, India. The study used secondary data for analyses and was granted exemption from review approval by the Institutional Ethics Committee of ICMR-NCDIR (Ref: NCDIR/IEC/3060/2022).
Data sources: NCRP reports 2020 described cancer incidence by sex, 16 age groups (0-4, 5-9, 10-14, 15-19, 20-24, 25-29, 30-34, 35-39, 40-44, 45-49, 50-54, 55-59, 60-64, 65-69, 70-74 and 75+; in yrs) and anatomical sites across the 28 PBCRs in India from the year 2012 to 20168. The anatomical sites follow the International Statistical Classification of Diseases and Related Health Problems (ICD-10, 10th revision)9. The population at risk was extracted from the Census of India, Registrar General and General Census Commissioner of India for the years 2001 and 2011 by State/Union Territory (UT) and sex10.
Estimation of Cancer Incidence in India for 2022: Crude incidence rate (CR) per 100,000 was calculated by dividing the total number of cases by the total population. Age-specific incidence rate (ASIR) per 100,000 was derived by dividing the number of cancer cases by the total population in that particular age group. Age-adjusted rate (AAR) was the weighted average of ASIR and world standard population11. In the absence of any other competing cause of death, cumulative risk refers to the likelihood that a given individual will be diagnosed with cancer during his or her lifetime between the ages of 0 and 74 years. This was expressed as ‘1 in how many’ are likely to develop cancer during their lifetime.
The PBCRs with a minimum three years’ data and incidence rate, consistent with previous years, were included for estimation. The coverage of PBCRs is varied across India, with full/less/no coverage among the States/UTs. The North-East (NE) region has better representativeness over the rest of India, with four NE States (Sikkim, Manipur, Mizoram and Tripura) having 100 per cent PBCR coverage and each NE State with at least one fully functional PBCR. Of the 28 PBCRs rural, urban and semi-urban distributions were one (3.5%), 12 (42.9%) and 15 (53.6%), respectively. There was no sampling method used in selecting PBCRs. The PBCRs of the respective State/region were used to differentiate between rural and urban settings wherever feasible. For example, Chennai and Dindigul PBCRs’ rates were used to describe Tamil Nadu State urban and rural rate, respectively12. Patiala PBCRs cover both urban and rural areas and have been used for the Punjab State8. For regions with less/no PBCR coverage, the pooled incidence rates (combination of rural and urban) were used for the rest of India except for Delhi, Punjab district, Maharashtra and the southern region.
First, the representation of PBCRs by State/region wise was assigned for estimating cancer burden (Supplementary Table I). Then, the Indian States/UT-wise population by five-year age groups till 2022 were calculated using the difference distribution method from the 2001 to 2011 census growth rate13. Thereafter, the ASIR of each specific anatomical site from 2012 to 2016 was applied to the estimated population to derive the number of cancer cases in India for 2022. Cancer estimates for each specific anatomical site were added to get the total estimate of all site cancer (ICD 10: C00-C97). The pooled age, sex- and site-specific incidence rates were computed using the population-weighted average of the rates from the PBCRs. The estimation of cancer incidence was done assuming that the 28 PBCRs represent the country with a constant incidence rate over time.
Supplementary Table I.
State/region wise representation of Population-Based Cancer Registry in India
| Regions | State/UT | PBCR representation |
|---|---|---|
| North | Chandigarh | Pooled Rest of India |
| Delhi | Delhi | |
| Haryana | Pooled Rest of India | |
| Himachal Pradesh | Pooled Rest of India | |
| Jammu and Kashmir, Ladakh | Pooled Rest of India | |
| Punjab | Patiala | |
| Uttarakand | Pooled Rest of India | |
| North East | Arunachal Pradesh | Pooled (West Arunachal, Pasighat) |
| Assam | Pooled (Cachar, Kamrup, Dibrugarh) | |
| Manipur | Manipur state | |
| Meghalaya | Meghalaya | |
| Mizoram | Mizoram state | |
| Nagaland | Kohima, Dimapur | |
| Sikkim | Sikkim state | |
| Tripura | Tripura state | |
| East | Bihar | Pooled Rest of India |
| Jharkhand | Pooled Rest of India | |
| Orissa | Pooled Rest of India | |
| West Bengal | Pooled Rest of India | |
| Central | Chattisgarh | Pooled Rest of India |
| Madhya Pradesh | Pooled Rest of India | |
| Rajasthan | Pooled Rest of India | |
| Uttar Pradesh | Pooled Rest of India | |
| West | Dadra and Nagar Haveli | Pooled Rest of India |
| Daman and Diu | Pooled Rest of India | |
| Goa | Pooled Maharashtra | |
| Gujarat | Pooled Rest of India | |
| Maharashtra | Pooled Maharashtra | |
| South | Andhra Pradesh | Pooled South |
| Telangana | Pooled South | |
| Andaman and Nicobar Islands | Pooled South | |
| Karnataka | Pooled South | |
| Kerala | Pooled Thiruvananthapuram district, Kollam district | |
| Lakshadweep | Pooled South | |
| Puducherry | Chennai-U, Dindigul-R | |
| Tamil Nadu | Chennai-U, Dindigul-R |
Pooled south, PBCRs of Chennai, Bangalore, Thiruvanathapuram district, Kollam district, Hyderabad, Dindigul; Pooled Maharashtra, All PBCRs from Maharashtra (Mumbai, Aurangabad, Nagpur, Pune, Wardha district, Barshi rural, Osmanabad and Beed); Pooled rest of India, All PBCRs from other than north-east region. U, urban; R, rural; PBCR, Population-Based Cancer Registry
The same process has been executed to estimate the cancer cases for the year 2025. The statistical analysis and graphs were generated using in-house software Population-Based Cancer Registry Data Management (PBCRDM) version 2.1 and Microsoft Excel.
Results
Table I presents the estimated cancer incidence, number of cases, crude rate and cumulative risk by sex and anatomical sites in India for the year 2022. The estimated number of cancer cases and crude incidence rate in India for the year 2022 was 14,61,427 (100.4 per 100,000), with a greater number of female cases 7,49,251 (105.4 per 100,000) estimated compared to that in males 7,12,176 (95.6 per 100,000). The estimated AAR for all sites of cancer in India would be 107.0 per 100,000. The leading five sites with the highest cancer burden in both sexes were organs of the digestive system (2,88,054), breast (2,21,757), genital system (2,18,319), oral cavity and pharynx (1,98,438) and respiratory system (1,43,062). The cumulative risk to develop cancer in his/her lifetime between 0 and 74 yr was one in every nine persons for all sites of cancer in both sexes, one in 67 for lung cancers in males and one in 29 for breast cancer in females.
Table I.
Estimated number, incidence rate and cumulative risk for all cancer sites in India by sex-2022
| Site | Male | Female | Both sexes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Cases | CR | AAR | Cum-risk | Cases | CR | AAR | Cum-risk | Cases | CR | AAR | Cum-risk | |
| All sites | 712,176 | 95.6 | 105.7 | 1 in 9 | 749,251 | 105.4 | 109.0 | 1 in 9 | 1,461,427 | 100.4 | 107.0 | 1 in 9 |
| Oral cavity and pharynx | 145,844 | 19.6 | 21.2 | 1 in 42 | 52,594 | 7.4 | 7.7 | 1 in 115 | 198,438 | 13.6 | 14.4 | 1 in 62 |
| Tongue | 41,845 | 5.6 | 6.0 | 1 in 147 | 14,611 | 2.1 | 2.1 | 1 in 400 | 56,456 | 3.9 | 4.1 | 1 in 215 |
| Mouth | 60,164 | 8.1 | 8.6 | 1 in 103 | 23,675 | 3.3 | 3.5 | 1 in 241 | 83,839 | 5.8 | 6.1 | 1 in 144 |
| Pharynx | 3177 | 0.4 | 0.5 | 1 in 1793 | 1168 | 0.2 | 0.2 | 1 in 5482 | 4345 | 0.3 | 0.3 | 1 in 2704 |
| Other oral cavity | 40,658 | 5.5 | 6.1 | 1 in 137 | 13,140 | 1.8 | 1.9 | 1 in 475 | 53,798 | 3.7 | 4.0 | 1 in 213 |
| Digestive system | 172,025 | 23.1 | 25.9 | 1 in 32 | 116,029 | 16.3 | 17.0 | 1 in 50 | 288,054 | 19.8 | 21.4 | 1 in 39 |
| Oesophagus | 34,272 | 4.6 | 5.2 | 1 in 159 | 21,300 | 3.0 | 3.1 | 1 in 263 | 55,572 | 3.8 | 4.2 | 1 in 198 |
| Stomach | 34,353 | 4.6 | 5.2 | 1 in 160 | 18,353 | 2.6 | 2.7 | 1 in 319 | 52,706 | 3.6 | 3.9 | 1 in 213 |
| Small intestine | 2255 | 0.3 | 0.3 | 1 in 2498 | 1533 | 0.2 | 0.2 | 1 in 3877 | 3788 | 0.3 | 0.3 | 1 in 3041 |
| Colon | 21,595 | 2.9 | 3.2 | 1 in 260 | 16,512 | 2.3 | 2.4 | 1 in 348 | 38,107 | 2.6 | 2.8 | 1 in 298 |
| Rectum | 22,985 | 3.1 | 3.4 | 1 in 244 | 15,767 | 2.2 | 2.3 | 1 in 372 | 38,752 | 2.7 | 2.8 | 1 in 295 |
| Anus, anal canal | 3037 | 0.4 | 0.4 | 1 in 1865 | 2131 | 0.3 | 0.3 | 1 in 2682 | 5168 | 0.4 | 0.4 | 1 in 2200 |
| Liver and intrahepatic bile duct | 28,020 | 3.8 | 4.3 | 1 in 189 | 11,306 | 1.6 | 1.7 | 1 in 514 | 39,326 | 2.7 | 3.0 | 1 in 276 |
| Gallbladder and other biliary | 12,997 | 1.7 | 1.9 | 1 in 423 | 20,570 | 2.9 | 3.0 | 1 in 283 | 33,567 | 2.3 | 2.5 | 1 in 339 |
| Pancreas | 12,511 | 1.7 | 1.9 | 1 in 429 | 8557 | 1.2 | 1.3 | 1 in 656 | 21,068 | 1.4 | 1.6 | 1 in 519 |
| Respiratory system | 108,848 | 14.6 | 16.2 | 1 in 48 | 34,214 | 4.8 | 4.8 | 1 in 165 | 143,062 | 9.8 | 10.4 | 1 in 74 |
| Larynx | 28,542 | 3.8 | 4.3 | 1 in 184 | 3498 | 0.5 | 0.5 | 1 in 1629 | 32,040 | 2.2 | 2.4 | 1 in 331 |
| Lung and bronchus | 75474 | 10.1 | 11.6 | 1 in 67 | 27,897 | 3.9 | 4.1 | 1 in 209 | 103,371 | 7.1 | 7.8 | 1 in 101 |
| Other respiratory organs | 4832 | 0.6 | 0.3 | 1 in 1274 | 2819 | 0.4 | 0.2 | 1 in 2149 | 7651 | 0.5 | 0.2 | 1 in 1602 |
| Bones and joints | 8426 | 1.1 | 1.1 | 1 in 1011 | 6087 | 0.9 | 0.8 | 1 in 1365 | 14,513 | 1.0 | 1.0 | 1 in 1160 |
| Soft tissue | 8380 | 1.1 | 1.2 | 1 in 844 | 6895 | 1.0 | 1.0 | 1 in 1050 | 15,275 | 1.0 | 1.1 | 1 in 936 |
| Skin (excluding basal and squamous) | 11,745 | 1.6 | 1.7 | 1 in 510 | 9412 | 1.3 | 1.4 | 1 in 641 | 21,157 | 1.5 | 1.5 | 1 in 569 |
| Melanoma of the skin | 3145 | 0.4 | 0.5 | 1 in 1909 | 2479 | 0.3 | 0.4 | 1 in 2288 | 5624 | 0.4 | 0.4 | 1 in 2081 |
| Other non-epithelial skin | 8600 | 1.2 | 1.3 | 1 in 696 | 6933 | 1.0 | 1.0 | 1 in 891 | 15,533 | 1.1 | 1.1 | 1 in 782 |
| Breast | 5649 | 0.8 | 0.8 | 1 in 1021 | 216,108 | 30.4 | 31.2 | 1 in 29 | 221,757 | 15.2 | 16.0 | 1 in 56 |
| Genital system | 54,625 | 7.3 | 8.4 | 1 in 105 | 163,694 | 23.0 | 23.9 | 1 in 37 | 218,319 | 15.0 | 16.0 | 1 in 53 |
| Uterine cervix | - | - | - | - | 79,103 | 11.1 | 11.6 | 1 in 75 | 79,103 | 11.1 | 11.6 | 1 in 75 |
| Uterine corpus | - | - | - | - | 27,922 | 3.9 | 4.2 | 1 in 190 | 27,922 | 3.9 | 4.2 | 1 in 190 |
| Ovary | - | - | - | - | 46,126 | 6.5 | 6.7 | 1 in 133 | 46,126 | 6.5 | 6.7 | 1 in 133 |
| Vulva | - | - | - | - | 2258 | 0.3 | 0.3 | 1 in 2454 | 2258 | 0.3 | 0.3 | 1 in 2454 |
| Vagina and other genital, female | - | - | - | - | 7961 | 1.1 | 1.2 | 1 in 747 | 7961 | 1.1 | 1.2 | 1 in 747 |
| Placenta | - | - | - | - | 324 | 0.0 | 0.0 | 1 in 31,252 | 324 | 0.0 | 0.0 | 1 in 31,252 |
| Prostate | 43,691 | 5.9 | 6.8 | 1 in 125 | - | - | - | - | 43,691 | 5.9 | 6.8 | 1 in 125 |
| Testis | 4521 | 0.6 | 0.6 | 1 in 2092 | - | - | - | - | 4521 | 0.6 | 0.6 | 1 in 2092 |
| Penis and other genital, male | 6413 | 0.8 | 1.0 | 1 in 917 | - | - | - | - | 6413 | 0.8 | 1.0 | 1 in 917 |
| Urinary system | 34,942 | 4.7 | 5.3 | 1 in 158 | 11,861 | 1.7 | 1.8 | 1 in 500 | 46,803 | 3.2 | 3.5 | 1 in 240 |
| Urinary bladder | 21,523 | 2.9 | 3.3 | 1 in 250 | 5713 | 0.8 | 0.8 | 1 in 1011 | 27,236 | 1.9 | 2.0 | 1 in 402 |
| Kidney and renal pelvis | 12,963 | 1.7 | 2.0 | 1 in 442 | 5930 | 0.8 | 0.9 | 1 in 1036 | 18,893 | 1.3 | 1.4 | 1 in 619 |
| Ureter and other urinary organs | 456 | 0.1 | 0.1 | 1 in 10,755 | 218 | 0.0 | 0.0 | 1 in 21,739 | 674 | 0.0 | 0.1 | 1 in 14,422 |
| Eye and orbit | 1326 | 0.2 | 0.2 | 1 in 6887 | 977 | 0.1 | 0.2 | 1 in 9049 | 2303 | 0.2 | 0.2 | 1 in 7799 |
| Brain and other nervous system | 20,811 | 2.8 | 2.9 | 1 in 341 | 13,296 | 1.9 | 1.9 | 1 in 546 | 34,107 | 2.3 | 2.4 | 1 in 419 |
| Endocrine system | 9682 | 1.3 | 1.4 | 1 in 708 | 27,847 | 3.9 | 3.8 | 1 in 280 | 37,529 | 2.6 | 2.5 | 1 in 402 |
| Thyroid | 8967 | 1.2 | 1.2 | 1 in 758 | 27,253 | 3.8 | 3.7 | 1 in 285 | 36,220 | 2.5 | 2.4 | 1 in 416 |
| Adrenal gland | 715 | 0.1 | 0.1 | 1 in 10,776 | 594 | 0.1 | 0.1 | 1 in 13,920 | 1309 | 0.1 | 0.1 | 1 in 12,146 |
| Lymphoma | 34,116 | 4.6 | 4.9 | 1 in 197 | 21,233 | 3.0 | 3.1 | 1 in 296 | 55,349 | 3.8 | 4.0 | 1 in 236 |
| Hodgkin lymphoma | 7561 | 1.0 | 1.0 | 1 in 1150 | 4113 | 0.6 | 0.6 | 1 in 1866 | 11,674 | 0.8 | 0.8 | 1 in 1416 |
| Non-Hodgkin lymphoma | 26,497 | 3.6 | 3.8 | 1 in 238 | 17,070 | 2.4 | 2.5 | 1 in 352 | 43,567 | 3.0 | 3.2 | 1 in 284 |
| Malig Imn.Prol D | 58 | 0.0 | 0.0 | 1 in 103,646 | 50 | 0.0 | 0.0 | 1 in 163,299 | 108 | 0.0 | 0.0 | 1 in 127,221 |
| Multiple myeloma | 11,261 | 1.5 | 1.7 | 1 in 465 | 8165 | 1.1 | 1.2 | 1 in 646 | 19,426 | 1.3 | 1.5 | 1 in 541 |
| Leukaemia | 33,604 | 4.5 | 4.8 | 1 in 239 | 21,969 | 3.1 | 3.2 | 1 in 352 | 55,573 | 3.8 | 4.0 | 1 in 284 |
| Lymphoid leukaemia | 14,546 | 2.0 | 2.1 | 1 in 609 | 7638 | 1.1 | 1.2 | 1 in 1137 | 22,184 | 1.5 | 1.7 | 1 in 790 |
| Myeloid leukaemia | 15,531 | 2.1 | 2.2 | 1 in 474 | 11,788 | 1.7 | 1.7 | 1 in 616 | 27,319 | 1.9 | 1.9 | 1 in 536 |
| Leukaemia unspecified | 3527 | 0.5 | 0.5 | 1 in 2292 | 2543 | 0.4 | 0.4 | 1 in 2974 | 6070 | 0.4 | 0.4 | 1 in 2585 |
| Other and unspecified primary sites | 50,892 | 6.8 | 7.6 | 1 in 114 | 38,870 | 5.5 | 5.7 | 1 in 153 | 89,762 | 6.2 | 6.6 | 1 in 131 |
Cum-risk, cumulative risk of developing cancer in 0-74 yr of age; CR, crude rate; AAR, age-adjusted rate; Malig Imn.Prol D, malignant immunoproliferative diseases
Fig. 1 presents the estimated top five leading sites of cancer; among males these were lung (10.6%), mouth (8.4%), prostate (6.1%), tongue (5.9%) and stomach (4.8%). The estimated top five leading sites of cancer among females included breast (28.8%), cervix (10.6%), ovary (6.2%), corpus uteri (3.7%) and lung (3.7%). Liver cancer (3.9%) was among the leading ten cancers in males and not in females, whereas thyroid (3.6%) and gallbladder (2.7%) cancers were in top ten among females but not in males.
Fig. 1.
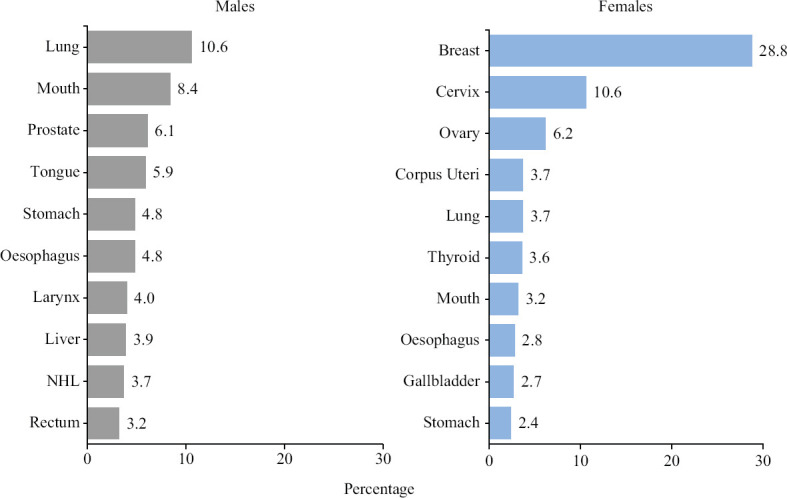
Estimated proportion of top 10 leading sites of cancer in India by sex – 2022.
Table II provides gender disaggregated, estimated top five leading sites of cancer (%) in India by age group (0-14, 15-39, 40-64, 65+ age group) for the year 2022. In the childhood group (0-14 yr) lymphoid leukaemia is the leading site for both boys (29.3%) and girls (24.3%), followed by the brain nervous system (NS) (boys: 12.4% and girls: 14.3%). In the adolescent and young adult group (15-39 yr), among males, the leading sites are mouth (12.0%), tongue (8.8%), brain NS (7.0%), myeloid leukaemia (6.5%) and non-Hodgkin lymphoma (NHL) (5.9%); among females, breast (27.3%), thyroid (12.2%), ovary (7.3%), cervix (7.1%) and myeloid leukaemia (3.7%). In 40-64 years’ age group, among males, the leading sites included the lung (11.0%), mouth (10.9%) and tongue (7.3%). Among females, the leading sites were breast (33.0%), cervix (12.3%) and ovary (6.5%); this age group had a high incidence of cases in both males (3,41,230) and females (4,25,918). Above 65 yr of age, prostate (12.3%) was the second-leading site after lung (13.1%) in males. Above 40 yr of age, lung cancer was the top most common cancer among males while breast cancer topped in females.
Table II.
The estimated top five leading sites of cancer (number and proportion) in India by age group (0-14, 15-39, 40-64, 65+ age group) and sex for the year 2022
| Males | Females | ||
|---|---|---|---|
|
|
|
||
| Cancer site | n (%) | Cancer site | n (%) |
| 0-14 yr | |||
| Lymphoid leukaemia (C91) | 6233 (29.3) | Lymphoid leukaemia (C91) | 3328 (24.3) |
| Brain and NS (C70-C72) | 2643 (12.4) | Brain and NS (C70-C72) | 1956 (14.3) |
| NHL (C82-86, C96) | 1679 (7.9) | Bone (C40-C41) | 1140 (8.3) |
| Hodgkin’s disease (C81) | 1513 (7.1) | Myeloid leukaemia (C92-C94) | 1099 (8.0) |
| Myeloid leukaemia (C92-C94) | 1498 (7.0) | NHL (C82-86, C96) | 783 (5.7) |
| Other sites | 7742 (36.3) | Other sites | 5403 (39.4) |
| All sites | 21,308 (100.0) | All sites | 13,709 (100.0) |
| 15-39 yr | |||
| Mouth (C03-C06) | 9013 (12.0) | Breast (C50) | 25,710 (27.3) |
| Tongue (C01-C02) | 6597 (8.8) | Thyroid (C73) | 11,453 (12.2) |
| Brain and NS (C70-C72) | 5230 (7.0) | Ovary (C56) | 6877 (7.3) |
| Myeloid leukaemia (C92-C94) | 4881 (6.5) | Cervix (C53) | 6714 (7.1) |
| NHL (C82-86, C96) | 4444 (5.9) | Myeloid leukaemia (C92-C94) | 3503 (3.7) |
| Other sites | 44,707 (59.7) | Other sites | 39,909 (42.4) |
| All sites | 74,872 (100.0) | All sites | 94,166 (100.0) |
| 40-64 yr | |||
| Lung (C33-34) | 37,376 (11.0) | Breast (C50) | 140,384 (33.0) |
| Mouth (C03-C06) | 37,067 (10.9) | Cervix (C53) | 52,560 (12.3) |
| Tongue (C01-C02) | 24,951 (7.3) | Ovary (C56) | 27,562 (6.5) |
| Oesophagus (C15) | 18,390 (5.4) | Corpus uteri (C54) | 18,108 (4.3) |
| Stomach (C16) | 17,741 (5.2) | Lung (C33-34) | 14,341 (3.4) |
| Other sites | 205,705 (60.3) | Other sites | 172,963 (40.6) |
| All sites | 341,230 (100.0) | All sites | 425,918 (100.0) |
| 65+yr | |||
| Lung (C33-34) | 36,013 (13.1) | Breast (C50) | 49,946 (23.2) |
| Prostate (C61) | 33,695 (12.3) | Cervix (C53) | 19,814 (9.2) |
| Oesophagus (C15) | 14,668 (5.3) | Lung (C33-34) | 11,793 (5.5) |
| Stomach (C16) | 14,435 (5.3) | Ovary (C56) | 11,188 (5.2) |
| Mouth (C03-C06) | 14,035 (5.1) | Mouth (C03-C06) | 9060 (4.2) |
| Other sites | 161,920 (58.9) | Other sites | 113,657 (52.8) |
| All sites | 274,766 (100.0) | All sites | 215,458 (100.0) |
NHL, non-Hodgkin lymphoma; NS, nervous system
Fig. 2 presents the estimated cancer cases and ASIR by five-year age group and gender for India in 2022. The ASIR for all sites of cancer started increasing from 25 years of age in both males and females. However, the ASIR among females aged 25-59 yr was higher than in males. Above 60 yr, the male ASIR was higher than females and it peaked at 75+ yr with 710.6 per 100,000. While in females, the ASIR dropped to 451.7 per 100,000 at 75+ yr. The highest number of cancer cases were in the 60-64 yr age group (males: 1,06,296 and females: 1,05,139).
Fig. 2.
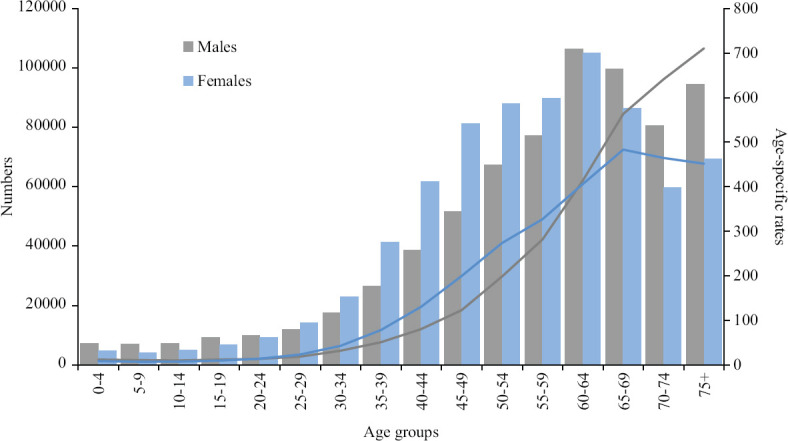
Estimated age-wise number and incidence rate for all sites of cancer by sex – 2022.
Table III provides the estimated leading sites of cancer cases by different periods (2015, 2020 and 2025) for leading sites of cancer. While in males, all site - cancers are likely to increase to 7,63,575 in 2025 from 6,01,737 in 2015, in females all site - cancers are likely to increase to 8,06,218 in 2025 from 6,27,202 in 2015. The projected leading cancer cases of the lung and breast would be 81,219 and 2,32,832 among males and females, respectively, for the year 2025. Cancer cases considered together for all sites are expected to increase by 27.7 per cent from 2015 to 2025.
Table III.
Estimated trends in number of cancer cases for the leading sites (ICD-10 codes) in India in 2015, 2020 and 2025
| Males | Females | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Cancer site (ICD 10) | 2015 | 2020 | 2025 | Cancer site (ICD 10) | 2015 | 2020 | 2025 |
| Lung (C33-34) | 63,087 | 71,788 | 81,219 | Breast (C50) | 180,252 | 205,424 | 232,832 |
| Mouth (C03-C06) | 50,779 | 57,380 | 64,519 | Cervix (C53) | 65,978 | 75,209 | 85,241 |
| Prostate (C61) | 36,419 | 41,532 | 47,068 | Ovary (C56) | 38,607 | 43,886 | 49,644 |
| Tongue (C01-C02) | 35,336 | 39,902 | 44,861 | Corpus uteri (C54) | 23,175 | 26,514 | 30,121 |
| Stomach (C16) | 28,815 | 32,713 | 36,938 | Lung (C33-34) | 23,163 | 26,490 | 30,109 |
| Others | 387,301 | 436,106 | 488,970 | Others | 296,027 | 335,235 | 378,271 |
| All sites | 601,737 | 679,421 | 763,575 | All sites | 627,202 | 712,758 | 806,218 |
ICD, International Classification of Diseases 10th Revision
Discussion
In India, the incidence of cancer cases is likely to increase from 1.46 million in 2022 to 1.57 million in 2025. The national average for the year 2022 of crude rate of incidence per 100,000 is 100.4; for males, 95.6 and females, 105.4. Lung and breast cancers in males and females, respectively, remain to be the leading sites of cancer. Lymphoid leukaemia, followed by brain NS is the leading site of cancer in the childhood age group among both sexes. ASIR increased with increasing age and it was higher in the female reproductive age group (15-49 yr). Lung cancer was estimated to be 1,03,371 cases in 2022 and it featured in the top five leading sites for both males and females. The current estimates for cancer in India increased by five per cent (14,61,427 in 2022 compared to 13,92,179 in 2020)5.
The NCRP, India, started with three PBCRs located at Bangalore, Mumbai and Chennai in 1982. Based on the data from the three PBCRs, the cancer burden in India was projected for the year 200114. With the expansion of PBCRs, cancer estimate updates were published based on available PBCRs5,15-18. Recently, GLOBOCAN estimated the cancer incidence for India for the year 2020 using ASIR from 27 PBCRs of 2012-2014 data and cancer incidence in five continents4,19. China had estimated the incidence for the year 2022, assuming that the ASIR in 2020 would continue to be constant20. The present study used recently available 28 PBCRs ASIR of 2012-2016 with a better representation of States to arrive at the projection. The decadal census of 2021 has been delayed due to the COVID-19 pandemic. Post-censal estimates of the 2001-2011 census growth rate were used for the population at risk in India10,13. The factors influencing population, such as fertility, mortality and migration, were not incorporated for estimation. NCRP estimate was 5.1 per cent higher than the GLOBOCAN for the year 20202. This difference could be attributable to the difference in methodology, use of recent data and assumptions.
The PBCRs included in the analysis covered approximately 10 per cent of the population in India. Data from some of the populous States (e.g. Uttar Pradesh and Bihar) is not yet available for analysis. India’s current NCRP coverage is 16.4 per cent, and the country’s urban and rural population coverage rates are 31.6 and 9.5 per cent, respectively. Furthermore, the rural component of PBCRs is not presented in the majority of States. It is therefore recommended that cancer registration be expanded to include a more representative population in each State of India for more reliable projections and to strengthen cancer control activities. Having cancer as a notifiable disease in the country will improve the coverage and provide a better representation as well. Time trends in the cancer incidence rate approach were not followed; rather we assumed the recent available incidence rate (constant) as a conservative approach for this estimation. The increase in cancer cases was attributable to the changes in population dynamics and its growth. India is expected to see an increase in the older age population, and especially the proportion of the population (>60 yr) is expected to increase from 8.6 per cent in 2011 to 9.7 per cent in 2022 (Supplementary Figure (1.3MB, tif) )10. There would be changes in estimated cancer incidence, which depends upon the risk factors, improvement in case findings, introduction of screening programmes and cancer detection and diagnosis techniques. The COVID-19 pandemic made an impact on the reduction in new cancer registration and delivery of oncology services in India, which was not considered for estimation21. As per the International Association of Cancer Registries/International Agency for Research on Cancer (IARC) standards, the PBCRs’ quality indicators were followed and published in CI5 volumes4.
Mortality data were incomplete due to poor coverage of the Civil Registration System, and there are certain limitations in getting cancer as the cause of death. The collection of accurate mortality data has been a big challenge and its quality varies across the PBCRs. Hence, the approach of estimating incidence from mortality or survival was not attempted. Methodological characteristics for cancer estimations were presented from various sources (Supplementary Table II). The longer period (>25 yr) of data is available only from six (5-urban and 1-rural) out of 28 PBCRs. Due to the unavailability of a longer period of data from most of the PBCRs, statistical modelling techniques such as Age-Period-Cohort could not be included. There were several challenges to starting a PBCR in low- and middle-income countries. A sample of regional PBCRs or a series of regional PBCRs with 10 per cent of coverage would get considerable benefit for cancer control purposes22. In these circumstances, this is the best available cancer data in the country for estimation. GLOBOCAN, IARC has used the same PBCRs to estimate the burden for India and similarly for some of the neighbouring countries in the South Asia region19.
Supplementary Table II.
Differences in burden estimation methods for India by selected sources
| Characteristics | GLOBOCAN1,2 | GBD27 | NCRP |
|---|---|---|---|
| Data sources | PBCRs (27) from the NCRP 2012-2014 and Dindigul, Mansa, Sangrur PBCRs incidence data | PBCRs (42) and Sample Registration System, cause of death data from India. Cancer registry data were used as the gold standard | PBCRs (28) from the NCRP, 2020 report of 2012-2016 and Dindigul PBCR incidence data |
| Population estimates | North East States, India’s rural and urban population derived from United Nation and Census of India, 2011 | Not mentioned | State wise population estimation based on Census of India, 2011 |
| Exclusion | Hospital-Based Cancer Registry | Hospital-Based Cancer Registry | Hospital-Based Cancer Registry |
| Method | Weighted average of the most recent local rates applied to 2020 population | Mortality estimates arrived by multiplying incidence with modelled mortality-incidence ratio The estimation of cancer incidence is based on registry data from India | Weighted average of the most recent local rates (2012-2016) applied to 2022 population |
| Cancer measure | Age specific incidence rate by site, sex and age | Mortality data from vital registration used as base to calculate the different measures | Age-specific incidence rate by site, sex and age |
| Outcome | Incidence and rates for India | Cancer mortality, incidence and DALY’s by State/India | Incidence and rates for India |
GLOBOCAN, Global Cancer Observatory; GBD, Global Burden of Disease; PBCR, Population-Based Cancer Registry; NCRP, National Cancer Registry Programme; DALY, Disability-Adjusted Life Years
A review on the burden of cancer in India attributed the increases to improved cancer diagnostics, cancer data capture and continuing epidemiologic transition23. Tobacco-related/lifestyle/ageing-related cancer incidence rate has increased over time for the tongue, mouth, colon, rectum, liver, lung, breast, corpus uteri, ovary, thyroid, prostate, gallbladder, pancreas, kidney, urinary bladder, brain, NHL and lymphoid leukaemia. Meanwhile, a decrease in cancer incidence rate was observed for the hypopharynx, oesophagus, stomach and cervix24-26. Alcohol use (30.1%) was the leading attributable risk factor for pharyngeal cancer related Disability Adjusted Life Years (DALYs). Tobacco use and air pollution (43% each) were the attributable risk factors for lung cancer DALYs, whereas dietary factors (43.2%) were attributable to colorectal cancer27.
Globally, half of the cancer burden was seen in the 65+ age group, while it is one-third of cancer in India2. However, half of the estimated cancer burden is in the 40-64 yr age group in India. The childhood cancer burden accounts for three per cent of boys and 1.8 per cent of girls in the age group of 0-14 yr. The rural population of India reported a lower childhood cancer incidence rate that could be attributed to under-reporting28,29. A study on adolescent and young adult cancers showed a significant increase in the incidence among males observed over time30. The incidence of cancer cases is estimated to increase to 12.8 per cent in 2025 compared to 2020. A recent publication from NCRP projected the burden of cancer to 29.8 million DALYs by 2025 in India31.
In summary, the cancer incidence burden is continuing to increase in India. Among the top five cancers in females, breast cancer was found to be the highest, followed by three female genital organs cervix, ovary and corpus uteri. Among males, three sites; lung, mouth and tongue were limited with tobacco-related cancers. A preventable measure needs to be taken for reducing the future burden of cancer. The new estimates are helpful for cancer prevention and control activities through the intervention of early detection, risk reduction and management in India. Appropriate research is, however, needed to delve deeper into the reasons of cancer burden and provide affordable solutions.
Population pyramids for proportion (%) of census 2011 and estimated 2022 by sex, age group in India.
Acknowledgment:
The authors acknowledge the contribution of the Population-Based Cancer Registries under the National Cancer Registry Programme contributed data.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global cancer observatory:Cancer today. Lyon, France: International Agency for Research on Cancer; 2020. [accessed on August 5, 2022]. Available from:https://gco.iarc.fr/today . [Google Scholar]
- 3.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 4.Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, et al. Lyon: International Agency for Research on Cancer Scientific Publications; 2017. Cancer incidence in five continents volume XI. [Google Scholar]
- 5.Mathur P, Sathishkumar K, Chaturvedi M, Das P, Sudarshan KL, Santhappan S, et al. Cancer statistics, 2020:Report from National Cancer Registry Programme, India. JCO Glob Oncol. 2020;6:1063–75. doi: 10.1200/GO.20.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bray F, Parkin DM. Evaluation of data quality in the cancer registry:Principles and methods. Part I:Comparability, validity and timeliness. Eur J Cancer. 2009;45:747–55. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 7.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 8.ICMR-National Centre for Disease Informatics and Research (NCDIR). Report of National Cancer Registry Programme 2020. Bengaluru (India): [accessed on June 20, 2022]. Available from: https://ncdirindia.org/All_Reports/PBCR_Annexures/Default.aspx . [Google Scholar]
- 9.World Health Organization (WHO) International statistical classification of diseases and related health problems. Geneva (Switzerland): WHO; 1994. [Google Scholar]
- 10.Office of the Registrar General &Census Commissioner, India. Population Census 2011. Table C-14:Population in Five-Year Age Group by Residence and Sex. New Delhi (India): 2011. [accessed on May 20, 2022]. Available from:http://www.censusindia.gov.in . [Google Scholar]
- 11.Segi M. Cancer mortality for selected sites in 24 countries (1950-1957) Sendai, Japan: The Department of Public Health, Tohoku University School of Medicine; 1960. [Google Scholar]
- 12.Swaminathan R, Shanta V on Behalf of the TNCRP Study Group. Tamil Nadu Cancer Registry Project. Chennai (India): Cancer Institute (W. I. A.); 2020. Cancer Incidence and Mortality (Year 2016), Incidence Trend (2012-2016) and Estimates (2017-2020) for Tamil Nadu State. [Google Scholar]
- 13.Takiar R, Shobana B. Cancer incidence rates and the problem of denominators –A new approach in Indian cancer registries. Asian Pac J Cancer Prev. 2009;10:123–6. [PubMed] [Google Scholar]
- 14.Murthy NS, Juneja A, Sehgal A, Prabhakar AK, Luthra UK. Cancer projection by the turn of century-Indian science. Indian J Cancer. 1990;27:74–82. [PubMed] [Google Scholar]
- 15.Murthy NS, Chaudhry K, Rath GK. Burden of cancer and projections for 2016, Indian scenario:Gaps in the availability of radiotherapy treatment facilities. Asian Pac J Cancer Prev. 2008;9:671–7. [PubMed] [Google Scholar]
- 16.Swaminathan R, Shanta V, Ferlay J, Balasubramanian S, Bray F, Sankaranarayanan R. Trends in cancer incidence in Chennai city (1982-2006) and statewide predictions of future burden in Tamil Nadu (2007-16) Natl Med J India. 2011;24:72–7. [PubMed] [Google Scholar]
- 17.Takiar R, Nadayil D, Nandakumar A. Projections of number of cancer cases in India (2010-2020) by cancer groups. Asian Pac J Cancer Prev. 2010;11:1045–9. [PubMed] [Google Scholar]
- 18.D'Souza NDR, Murthy NS, Aras RY. Projection of cancer incident cases for India till 2026. Asian Pac J Cancer Prev. 2013;14:4379–86. [PubMed] [Google Scholar]
- 19.Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018:GLOBOCAN sources and methods. Int J Cancer. 2018;144:1941–53. doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- 20.Xia C, Dong X, Li H, Cao M, Sun D, He S, et al. Cancer statistics in China and United States, 2022:Profiles, trends, and determinants. Chin Med J (Engl) 2022;135:584–90. doi: 10.1097/CM9.0000000000002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ranganathan P, Sengar M, Chinnaswamy G, Agrawal G, Arumugham R, Bhatt R, et al. Impact of COVID-19 on cancer care in India: A cohort study. Lancet Oncol. 2021;22:970–6. doi: 10.1016/S1470-2045(21)00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bray F, Znaor A, Cueva P, Korir A, Swaminathan R, Ullrich A, et al. Planning and developing population-based cancer registration in low- or middle-income settings. Lyon (France): International Agency for Research on Cancer; 2014. [PubMed] [Google Scholar]
- 23.Smith RD, Mallath MK. History of the growing burden of cancer in India:From antiquity to the 21st century. J Glob Oncol. 2019;5:1–15. doi: 10.1200/JGO.19.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Centre for Disease Informatics and Research. Time trends in cancer incidence rates 1982-2010. Bengaluru (India): National Cancer Registry Programme, ICMR-NCDIR; 2013. [accessed on June 20, 2022]. Available from: https://www.ncdirindia.org/All_Reports/TREND_REPORT_1982_2010/ [Google Scholar]
- 25.Nath A, Sathishkumar K, Das P, Sudarshan KL, Mathur P. A clinicoepidemiological profile of lung cancers in India –Results from the National Cancer Registry Programme. Indian J Med Res. 2022;155:264–72. doi: 10.4103/ijmr.ijmr_1364_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sathishkumar K, Vinodh N, Badwe RA, Deo SVS, Manoharan N, Malik R, et al. Trends in breast and cervical cancer in India under National Cancer Registry Programme:An age-period-cohort analysis. Cancer Epidemiol. 2021;74:101982. doi: 10.1016/j.canep.2021.101982. [DOI] [PubMed] [Google Scholar]
- 27.India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the states of India:The global burden of disease study 1990-2016. Lancet Oncol. 2018;19:1289–306. doi: 10.1016/S1470-2045(18)30447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swaminathan R, Sankaranarayanan R. Under-diagnosis and under-ascertainment of cases may be the reasons for low childhood cancer incidence in rural India. Cancer Epidemiol. 2010;34:107–8. doi: 10.1016/j.canep.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Arora RS. Why is the incidence of childhood cancer lower in rural India? Cancer Epidemiol. 2010;34:105–6. doi: 10.1016/j.canep.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 30.Mathur P, Nath A, Sathish Kumar K. Adolescent and young adult cancers in India-Findings from the National Cancer Registry Programme. Cancer Epidemiol. 2022;78:102124. doi: 10.1016/j.canep.2022.102124. [DOI] [PubMed] [Google Scholar]
- 31.Kulothungan V, Sathishkumar K, Leburu S, Ramamoorthy T, Stephen S, Basavarajappa D, et al. Burden of cancers in India – Estimates of cancer crude incidence, YLLs, YLDs and DALYs for 2021 and 2025 based on National Cancer Registry Program. BMC Cancer. 2022;22:527. doi: 10.1186/s12885-022-09578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Population pyramids for proportion (%) of census 2011 and estimated 2022 by sex, age group in India.


