Abstract
Introduction:
Children with congenital heart disease (CHD) often experience feeding intolerance due to aspiration, inability to tolerate feed volume, or reflux within the first few months of life, requiring a surgically placed gastrostomy tube (GT) for durable enteral access. However, complications such as GT dislodgement, cellulitis, and leakage related to GT use are common. GT-related complications can lead to unscheduled pediatric surgery clinic or emergency room (ER) visits, which can be time consuming for the family and increase overall healthcare costs. We sought to identify factors associated with GT complications within 2 wk after GT surgery and 1-y after discharge home following GT placement in infants with CHD.
Methods:
We performed a retrospective cohort study using the Society of Thoracic Surgeons database and electronic medical records from a tertiary children’s hospital. We identified infants <1 y old underwent CHD surgery followed by GT surgery between September 2013-August 2018. Demographics, pre-operative feeding regimen, comorbidities, and GT-related utilization were measured. Postoperative GT complications (e.g., GT cellulitis, leakage, dislodgement, obstruction, and granulation tissue) within 2 wk after the GT surgery and an unplanned pediatric surgery clinic or ER visit within 1-y after discharge home were captured. Bivariate comparisons and multivariable logistic regression evaluated factors associated with GT complications and unplanned clinic or ER visits. A Kaplan–Meier failure curve examined the timing of ER/clinic visits.
Results:
Of 152 infants who underwent CHD then GT surgeries, 66% (N = 101) had post-operative GT complications. Overall, 83 unscheduled clinic visits were identified after discharge, with 37% (N = 31) due to concerns about granulation tissue. Of 137 ER visits, 48% (N = 66) were due to accidental GT dislodgement. Infants who were hospitalized for ≥2 wk after GT surgery had more complications than those discharged home within 2 wk of the GT surgery (40.6% versus 15.7%, P = 0.002). Infants receiving oral nutrition before CHD surgery (38.6% versus 60%, P=<0.001) or with single ventricle defects (19.8% versus 37.3%, P = 0.02) had fewer GT complications. After adjusting for type of cardiac anomaly, infants receiving oral nutrition prior to CHD surgery had a decreased likelihood of GT complications (odds ratio OR 0.46; 95% confidence intervals CI:0.23-0.93). A Kaplan–Meier failure curve demonstrated that 50% of the cohort experienced a complication leading to an unscheduled ER/clinic visit within 6 mo after discharge.
Conclusions:
Unplanned visits to the ER or pediatric surgery clinic occur frequently for infants with CHD requiring a surgically placed GT. Oral feedings before cardiac surgery associated with fewer GT complications. Prolonged hospitalization associated with more GT complications. Optimizing outpatient care and family education regarding GT maintenance may reduce unscheduled visits for this high-risk, device-dependent infant population.
Keywords: Complications, Congenital heart disease, Gastrostomy tube, Infants
Introduction
Congenital heart disease (CHD) is a common birth defect with an estimated prevalence of 6.9 cases per 1000 live births in North America.1,2 Approximately 39-80% of infants with CHD require gastrostomy tube (GT) placement3,4 due to concerns for aspiration, inability to orally take the feeding volume, or poor weight gain5,6. However, complications such as GT dislodgement, cellulitis, and leakage are common after hospital discharge and require unplanned pediatric surgery clinic or emergency room (ER) visits.7-10
Children with GT malfunctions and dislodgements commonly visit the ER.8 ER visits are costly for families caring for CHD infants who pay an average of $1266 for these visits, whereas, families of children without CHD pay an average of $741.11 Hence, GT-related complications increase the time, medical, financial burden on the infant and family. One way to reduce these unexpected costs from complications of GTs is scheduling visits as well as setting time aside for unexpected visits to an outpatient specialty surgical clinic for families of CHD children with GTs.9 Surgeons have attempted to address these complications by employing alternate techniques for suturing and dressing surgical wounds.12,13 Despite a reduction in GT-related issues, complications still persist, including granulation tissue formation and tube dislodgement requiring ER visits.12
Our study aims to identify clinical factors associated with GT complications within 1-y following discharge. We sought to identify potentially modifiable clinical factors associated with GT surgery complications, such as preoperative oral feeding abilities of infants with CHD and the timing of complications. Our goal is to identify infants at highest risk for GT surgery complications to tailor long-term follow-up care both pre- and postoperatively.
Material and Methods
Setting and population
We performed a retrospective cohort study using the Society of Thoracic Surgeons database and the electronic medical record from 2014 to 2019 from a tertiary level children’s hospital in Los Angeles. We enrolled infants less than 1 y of age with CHD who underwent CHD surgery followed by GT surgery between January 2014-October 2019. We excluded children who: 1) were greater than 1 y old at time of GT placement, 2) lost to follow-up, 3) had a thoracic surgery, or 4) expired during their hospitalization related to their CHD surgery (as we could not assess our primary outcome). We assessed GT complications for 1 y following discharge. The Children’s Hospital Los Angeles Institutional Review Board approved this study (−18-00,509) and waiver of informed consent.
Primary outcome
We defined the “GT complications” outcome dichotomously (yes versus no) as any complication within the 2-wk inpatient period after GT placement or an unplanned pediatric surgery clinic or ER visit related to the GT within 1 y of discharge following GT surgery. GT complications included cellulitis, leakage, obstruction, granulation tissue formation, dislodgement, and other GT related issues during the timeframes listed above.
Patient characteristics
Data abstracted included patient demographics, such as admission age at cardiac surgery, sex, race, ethnicity, insurance status, and gestational age. Cardiac operative variables included single ventricular or biventricular defects, age at cardiac surgery, type of CHD operation, cardiopulmonary bypass time (minutes), aortic cross clamp time (minutes), and total mechanical vent time (days). GT variables included percent of oral feedings consumed prior to cardiac surgery, age (days) at first oral feed attempt, nasojejunal tube before a GT surgery, indication for GT placement, age at GT surgery, type of GT placed, and any complications during their inpatient stay related to the GT placement. Variables collected upon discharge were: 1) feeding modality and 2) percent of goal feeds taken orally. Information collected after discharge were: 1) 30-d readmission related to the GT, 2) 30-d and 1-y mortality, 3) whether the patient was using the GT at 1 y postoperatively, and 4) unscheduled pediatric surgery clinic or ER visits related to the GT.
Statistical analysis
Descriptive statistics evaluated the relationship between patient characteristics and any GT complication. Chi-square and Fisher-exact tests (for categorical variables) and Wilcoxon-rank sum tests (for continuous variables) assessed associations between individual preoperative, operative, and discharge characteristics and GT complications. Multivariable logistic regression analysis analyzed clinically relevant covariates chosen a priori and by covariates with significant differences between groups (P < 0.05). Predictors included single ventricular defect, patient feeding orally before CHD surgery, noncardiac abnormalities, and syndrome or chromosomal abnormalities. We evaluated Akaike information criterion, negative log-likelihood, and c-statistic to select the model with the smallest values while maintaining a high c-statistic for the final model.
A Kaplan–Meier (KM) failure graph was created for unscheduled pediatric surgery clinic or emergency room (ER) visit related to GT complications within one-y. The failure graph was calculated using Stata/SE version 15.1 (StataCorp LLC, College Station, Texas). All other analyses were conducted with twosided significance, α = 0.05. Data were analyzed using Statistical Analysis System software 9.4 (SAS Institute, Inc, Cary, North Carolina).
Results
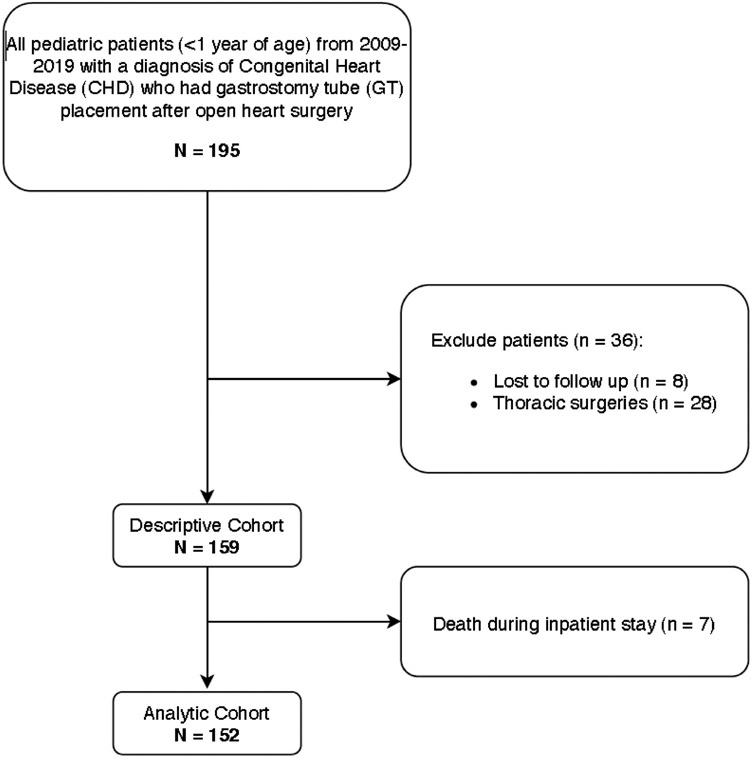
We identified 152 infants with CHD who underwent CHD surgery followed by GT surgery (Fig. 1). We list the CHD diagnosis types in Table 1. Of those, 101 (66%) presented with a post-operative GT a GT complication (Table 2). Demographics, cardiac surgery factors and GT surgery factors did not differ between groups. Granulation tissue (37%) was the primary reason for an unscheduled clinic visit, and GT dislodgement (48%) was the most common reason for unscheduled ER visit (Table 3). Bivariate comparisons showed that continued hospitalization for greater than 2 wk after GT surgery was associated with GT complications (40.6% versus 15.7%, P = 0.002). Conversely, patient receiving oral feeds before undergoing cardiac surgery (38.6% versus 60%, P = 0.01) and infants with SV defects demonstrated fewer GT complications (19.8% vs 37.3%, P = 0.02) (Table 4). After adjusting for SV defect and noncardiac abnormalities, infants receiving oral feeds before cardiac surgery were significantly less likely to experience a GT complication within a year after discharge (odds ratio OR = 0.46, 95% confidence interval CI = 0.23, 0.93) (Table 5). The KM failure curve demonstrated that 25%-50% of unscheduled GT complication visits occurred between 44 and 201 d after discharge (Fig. 2).
Fig. 1 –
Flow diagram for cohort selection.
Table 1 –
List of the types of Congenital Heart Defects in study subjects.
| Defect type | N = 152 | % |
|---|---|---|
| Aortic Arch Hypoplasia or Coarctation of the Aorta | 16 | 11 |
| Atrial Septal defect | 2 | 1 |
| Atrioventricular Septal defect | 10 | 7 |
| Double Chambered Right ventricle | 1 | 2 |
| L-Transposition of the great Arteries | 3 | 7 |
| Double Outlet Right ventricle | 11 | 7 |
| Hypoplastic Left heart syndrome | 10 | 3 |
| Interrupted aortic Arch | 5 | 1 |
| Mitral Valve Disease/Stenosis | 2 | 2 |
| Hemitruncus (Anomalous origin of right pulmonary artery from aorta) | 1 | 1 |
| Pulmonary Atresia with Intact ventricular Septum | 3 | 3 |
| Pulmonary Atresia with ventricular Septal defect | 2 | 1 |
| Pulmonary Stenosis | 4 | 14 |
| Shone’s syndrome | 2 | 12 |
| Other single ventricle physiology | 21 | 5 |
| Tetralogy of Fallot | 18 | 4 |
| D-Transposition of the great Arteries | 7 | 1 |
| Total Anomalous Pulmonary Venous Connection | 6 | 1 |
| Ebstein’s anomaly | 2 | 16 |
| Vascular Ring | 2 | 11 |
| Ventricular Septal defect | 24 | 1 |
Table 2 –
Bivariate comparisons of cohort demographics for any complication within a year of gastrostomy tube (GT) surgery.
| Demographics | No complication |
Complication |
P-value | ||
|---|---|---|---|---|---|
|
N = 51 (34%) |
N = 101 (66%) |
||||
| N | (%) | N | (%) | ||
| Demographics | |||||
| Female sex | 24 | 47.1 | 49 | 48.5 | 0.9 |
| White race | 12 | 23.5 | 20 | 19.8 | 0.6 |
| Hispanic ethnicity | 32 | 62.8 | 66 | 65.4 | 0.8 |
| Public insurance | 34 | 66.7 | 78 | 77.2 | 0.2 |
| Syndrome or chromosomal abnormalities | 27 | 52.9 | 54 | 53.5 | 1.0 |
| Median | IQR | Median | IQR | ||
| Gestational age, weeks | 37.0 | 36.0-39.0 | 38.0 | 36.0-38.0 | 0.9 |
| Age (days) at first oral attempt | 23.0 | 3.0-45.0 | 16.0 | 2.0-37.0 | 0.2 |
| Cardiac operative variables | |||||
| Cardiopulmonary bypass (CPB) during heart surgery | 44 | 86.3 | 89 | 88.1 | 0.7 |
| CPB time, minutes (mean SD) | 67.7 | 47.3 | 66.5 | 43.9 | 0.8 |
| GT operative variables | |||||
| Indication for GT - poor oral intake | 41 | 80.4 | 70 | 69.3 | 0.1 |
| GT surgery type- open | 16 | 31.4 | 39 | 38.6 | 0.6 |
| Median | IQR | Median | IQR | ||
| Age (days) at GT placement | 85.0 | 51.0-166.0 | 80.0 | 49.0-126.0 | 0.9 |
| Total percent of goal oral feeding tolerated before GT | 0.0 | 0.0-11.6 | 0.0 | 0.0-8.0 | 0.6 |
| Outpatient variables | |||||
| GT use at 1-y | 35 | 68.6 | 74 | 73.3 | 0.9 |
Table 3 –
Reasons for unscheduled clinic or emergency room (ER) visits due to gastrostomy tube (GT) complication.
| Demographics | Visit type |
|||
|---|---|---|---|---|
| Clinic |
ER |
|||
|
N = 83 |
N = 137 |
|||
| N | % | N | % | |
| GT cellulitis | 12 | 14.5 | 17 | 12.4 |
| GT leakage | 21 | 25.3 | 21 | 15.3 |
| GT obstruction | 1 | 1.2 | 1 | 0.7 |
| GT granulation tissue | 31 | 37.3 | 4 | 2.9 |
| GT falling out | 12 | 14.5 | 66 | 48.2 |
| Other | 6 | 7.2 | 28 | 20.4 |
Table 4 –
Clinical factors correlated with gastrostomy tube (GT) complications within a year.
| Demographics | No complications |
Complications |
P-value | ||
|---|---|---|---|---|---|
|
n = 51 (34%) |
n = 101 (66%) |
||||
| N | % | N | % | ||
| Patient received oral feeds before cardiac surgery | 31 | 60.8 | 39 | 38.6 | 0.01 |
| Single ventricular defect | 19 | 37.25 | 20 | 19.8 | 0.02 |
| Remained inpatient >2 wk after GT surgery | 8 | 15.7 | 41 | 40.6 | 0.001 |
| Age at time of cardiac surgery (days) | 48.6 | 66.5 | 77.6 | 94.0 | 0.05 |
| Total mechanical vent time (days) | 21.7 | 19.7 | 21.1 | 27.2 | 0.06 |
Table 5 –
Multivariable logistic regression of factors associated with gastrostomy tube (GT) complications in infants who received oral feeds before GT surgery versus not adjusted for single versus biventricular CHD and noncardiac abnormalities.
| Demographics | OR | 95% CI | |
|---|---|---|---|
| Single ventricular defect | 0.49 | 0.23 | 1.06 |
| Patient received oral feeds before cardiac surgery | 0.46 | 0.23 | 0.93 |
| Non-cardiac abnormalities | 0.96 | 0.48 | 1.94 |
Fig. 2 –
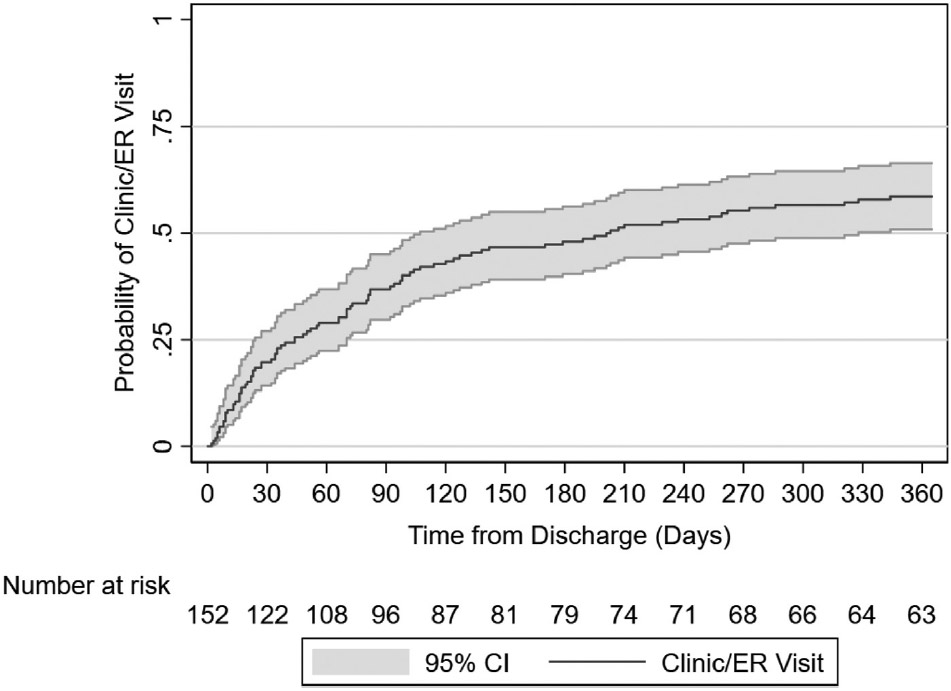
Kaplan–Meier Failure Curve of unscheduled pediatric surgery clinic or emergency room (ER) visit related to gastrostomy tube complications and the number of infants at risk at each time point.
Discussion
In summary, most infants with CHD requiring GT placement for durable enteral access experienced GT-related complications, including granulation tissue or GT dislodgement. Approximately, half of all inpatient and ER visits related to GT complications occurred between 6 wk and 6 mo after GT placement. Infants requiring hospitalization for >2 wk after GT surgery more often had GT complications. Conversely, infants tolerating oral feedings before cardiac surgery and those with single ventricle defects had fewer GT-related complications. These findings indicate that overall clinical disease burden likely influences an infant’s risk of long-term GT complications.
Like previous reports, CHD infants receiving a GT for enteral access often experience a GT complication. Goldberg et al. (2010) found granulation tissue complications in 68% of children with GTs similar to our results of 66%.7 On the other hand, McSweeney et al. (2013), however, found that about 11% of children within their study experienced at least one GT related complication, however, their cumulative incidence rates for complications increased to 15% by a median follow up of 5.4 y as they followed patients for 10 y after GT placement with some loss to follow-up.14 Their lower complication rate may be explained by McSweeney et al. investigating an older cohort of children (mean age of 22 mo) over a longer timeframe compared to our younger cohort (mean age of 3.8 mo) over a shorter period. Similarly, Landisch et al. (2016), noted that approximately, 7.6% of infants with laparoscopically placed GTs experienced tube dislodgements.15 This reduced rate of complications may be related to their short study time frame of 3 mo compared to our 1-y follow-up timeframe. Ours is the first report to utilize a KM failure curve of complications after GT placement in CHD infants, demonstrating that most clinic/ER visits occurred early following discharge.
Other investigators noted similar types of GT complications as compared to our study in which most of these complications lead to ER visits. Naiditch et al. (2010) concluded that from those children under 5 y old going to the ER for GT related complications, 58% developed granulation tissue and 28% experienced tube dislodgements. Most of this cohort received an open GT placement.16 Savaadra et al. (2009) found GT dislodgement as the leading reason for ER visits.8 Although, these studies did not address clinical factors associated with GTs, they confirmed similar GT complications rates and thus costly burden of these ER visits17 providing further support for the need of family resources to provide cost-effective care. Of note, most of these expenses do not incorporate the lost income and time parents and caretakers of children with CHD also experience.
Infants tolerating oral feedings before CHD surgery demonstrated fewer GT-associated complications. Previous studies reported that infants with CHD who fed orally had decreased length of hospitalizations compared to those with GTs.18 It is reasonable that the infants with CHD who fed orally may be more clinically stable and thus may have had shorter hospital stays, fewer complications, and heals sooner from their surgeries. Since those infants fed before their GT surgery, they may have had more practice feeding orally or had better oral feeding skills initially than those infants with more complications and thus, were able to fully eat by mouth sooner, leading to a shorter time of using the GT, and therefore less complications.
Interestingly, infants in the present study with single ventricle cardiac defects experienced fewer GT complications. These findings were somewhat counter-intuitive as infants with single ventricle defects require more complex cardiac surgery and are generally considered more critically ill, and often experience increased medical complications.19 Our findings may be institutionally dependent. These infants with single ventricle defects were seen in our outpatient cardiology clinics and other subspecialty clinics more frequently after discharge because of their higher acuity. More frequent opportunities to interface with the healthcare team may have indirectly contributed to fewer unscheduled ER visits for GT complications as these complications may have been identified and treated sooner in outpatient clinics. Since a large proportion of the GT complications (25-50%) occur between the 6 wk to 6 mo timeframe, scheduled clinic visits during that period may decrease unnecessary ER visits, especially in high-risk infants like those with SV heart defects.20,21
Our study had several limitations. First, our retrospective study relied on medical record documentation and could not control for outcome variables in a standardized fashion. Nevertheless, our outcomes of interest were all part of standards of care for the assessment of GTs. Moreover, we did not have missing data for any of our patients regarding their GT or other issues in which they went to clinic or the ER visits. Furthermore, our study did not capture visits that occur outside of our institution. However, most of these patients had complex CHD and transferred to our institution for further management given the need for multidisciplinary care that other local hospitals do not offer. Next, we did not have a control group for comparison, so it is unclear if infants without CHD who have GTs would have similar complication rates. The literature, however, in children with CHD (referred to above) demonstrated GT complication levels similar to our study’s findings. Lastly, our study may only be generalizable to CHD infants at our institution. We are a tertiary center and see the most critically-ill infants with CHD, which may limit generalizability of our findings.
Conclusions
Infants with CHD commonly have GT-related complications, with approximately, 25% resulting in an unscheduled clinic or ER visit within 60-d of hospital discharge. Infants receiving oral feedings before cardiac surgery and infants with single ventricle physiology are less likely to experience complications. Thus, closer follow-up with the healthcare team may reduce GT complications. Another possible strategy to decrease GT-related complications is improved maintenance through enhanced family education regarding GT care and maintenance for high-risk CHD infants. Quality improvement efforts to optimize family education regarding GT care and management and increased follow-up may decrease the need for unplanned clinic/ER visits related to GTs and therefore, decrease health care costs in this device dependent population.
Availability of Data
Available upon request.
Acknowledgments
We thank all of the participants and families of this study, the members of the HOPE Lab and Brain Development Lab at Children’s Hospital Los Angeles.
Funding
This study was supported by Southern California Clinical and Translational Sciences Institute (NCATS) through Grant UL1TR0001855. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Level of Evidence
Level III.
Disclosure
None declared
Meeting Presentation
This study was presented as an abstract at the Association for Academic Surgery (AAS) in February 2022.
REFERENCES
- 1.Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American heart association. Circulation. 2020;141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 2.Wu W, He J, Shao X. Incidence, and mortality trend of congenital heart disease at the global, regional, and national level 1990-2017. Med (Baltimore). 2020;99:e20593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cu SR, Sidman JD. Rates and risks of gastrostomy tubes in infants with cleft palate. Arch Otolaryngol Head Neck Surg. 2011;137:275–281. [DOI] [PubMed] [Google Scholar]
- 4.Rossi AF, Fishberger S, Hannan RL, et al. Frequency and indications for tracheostomy and gastrostomy after congenital heart surgery. Pediatr Cardiol. 2009;30:225–231. [DOI] [PubMed] [Google Scholar]
- 5.Stacy A, Killen S, Patrick O’Neal Maynord, Johnson Melissa, Xu Meng. Chris Slaughter. Pediatrics. 2019;144:346. [Google Scholar]
- 6.Jadcherla SR, Vijayapal AS, Leuthner S. Feeding abilities in neonates with congenital heart disease: a retrospective study. J Perinatol. 2009;29:112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elizabeth Goldberg, Sharon Barton, Xanthopoulos Melissa S, Nicolas Stettler, Liacouras Chris A. A descriptive study of complications of gastrostomy tubes in children. J Pediatr Nurs. 2010;25:72–80. [DOI] [PubMed] [Google Scholar]
- 8.Saavedra H, Losek JD, Shanley L, Titus MO. Gastrostomy tube-related complaints in the pediatric emergency department. Pediatr Emerg Care. 2009;25:728–732. [DOI] [PubMed] [Google Scholar]
- 9.Correa JA, Fallon SC, Murphy KM, et al. Resource utilization after gastrostomy tube placement: defining areas of improvement for future quality improvement projects. J Pediatr Surg. 2014;49:1598–1601. [DOI] [PubMed] [Google Scholar]
- 10.Burman L, Diaz M, Viktorsdóttir MB, et al. Wound infection after laparoscopic-assisted gastrostomy in infants. Surg J (N Y). 2019;5:e96–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edelson JB, Rossano JW, Griffis H, et al. Emergency department visits by children with congenital heart disease. J Am Coll Cardiol. 2018;72:1817–1825. ISSN 0735-1097. [DOI] [PubMed] [Google Scholar]
- 12.Steen EH, Tuley JM, Balaji S, Lee TC, Keswani SG. Advances in Wound Care. 2020:211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mason CA, Skarda DE, Bucher BT. Outcomes after laparoscopic gastrostomy suture techniques in children. J Surg Res. 2018;232:26–32. [DOI] [PubMed] [Google Scholar]
- 14.McSweeney ME, Jiang H, Deutsch AJ, Atmadja M, Lightdale JR. Long-term outcomes of infants and children undergoing percutaneous endoscopy gastrostomy tube placement. J Pediatr Gastroenterol Nutr. 2013;57:663–667. [DOI] [PubMed] [Google Scholar]
- 15.Landisch RM, Colwell RC, Densmore JC. Infant gastrostomy outcomes: the cost of complications. J Pediatr Surg. 2016;51:1976–1982. [DOI] [PubMed] [Google Scholar]
- 16.Naiditch JA, Lautz T, Barsness KA. Postoperative complications in children undergoing gastrostomy tube placement. J Laparoendosc Adv Surg Tech A. 2010;20:781–785. [DOI] [PubMed] [Google Scholar]
- 17.Horwitz LI, Green J, Bradley EH. US emergency department performance on wait time and length of visit. Ann Emerg Med. 2010;55:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McSweeney ME, Kerr J, Amirault J, Mitchell PD, Larson K, Rosen R. Oral feeding reduces hospitalizations compared with gastrostomy feeding in infants and children who aspirate. J Pediatr. 2016;170:79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piggott KD, Babb J, Yong S, et al. Risk factors for gastrostomy tube placement in single ventricle patients following the norwood procedure. Semin Thorac Cardiovasc Surg. 2018;30:443–447. [DOI] [PubMed] [Google Scholar]
- 20.Richards MK, Li CI, Foti JL, et al. Resource utilization after implementing a hospital-wide standardized feeding tube placement pathway. J Pediatr Surg. 2016;51:1674–1679. [DOI] [PubMed] [Google Scholar]
- 21.Berman L, Hronek C, Raval MV, et al. Pediatric gastrostomy tube placement: lessons learned from high-performing institutions through structured interviews. Pediatr Qual Saf. 2017;2:e016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available upon request.