Abstract
Age is a strong risk factor for cardiovascular disease. Accordingly, most cardiovascular risk prediction models have included age as an independent risk factor. There is much evidence that effective management of cardiovascular risk factors improves clinical outcomes even in older adults. However, there are concerns that intensive treatment for older adults increases the risk of adverse events. For hypertensive patients, intensive blood pressure reduction with combination therapy increases the risk of syncope, acute kidney injury, and falls. Intensive glucose-lowering therapy among older patients with diabetes increases the risk of hypoglycemia or cognitive impairment. These findings suggest that a balanced approach for older adults is required to increase the benefits and decrease the risk of side effects. In contrast to older people, the estimated 10-year cardiovascular risk in young and healthy individuals is low. However, the lifetime cardiovascular risk in these patients is actually high. The 2021 European Society of Cardiology guideline on cardiovascular disease prevention in clinical practice has been published. It proposed a different risk stratification and recommendation for treatment according to age group, based on the concept of avoiding undertreatment in young people and overtreatment in older persons. Although the guideline recommends age-dependent risk stratification, risk categories should not be applied to the mandatory initiation of drug treatment. In all age groups, other factors such as lifetime cardiovascular risk, treatment benefit and harm, comorbidities, frailty, and patient preferences should be considered when managing patients for primary prevention.
Keywords: Aged, Cardiovascular diseases, Guideline, Prevention
INTRODUCTION
Age is a major risk factor for cardiovascular disease (CVD). The prevalence of CVD, such as hypertension, ischemic heart disease, atrial fibrillation, and heart failure, increases with population aging.1 Moreover, older adults older than 70 years of age represent two-thirds of cases of atherosclerotic cardiovascular disease (ASCVD) mortality.2 However, the treatment of CVD risk factors for older patients needs to balance the benefits and risks. Older persons are generally at high-risk of developing adverse drug events and side effects. Nonetheless, the treatment benefit is limited to the older population because of their limited life expectancy. Therefore, the thresholds or cutoff values for CVD risk factor management should be less strict for healthy older individuals than for younger individuals. In contrast, the relative risk of CVD is usually lower in younger populations than in older populations. As a result, younger patients are usually regarded as low-risk patients in most risk-prediction models. However, the future lifetime risk of CVD is much greater in younger patients with multiple risk factors than in older patients. Accordingly, the benefit of risk factor treatment is much greater among younger patients than among older patients in the long term. A balanced approach for both younger and older persons that considers the benefits and harms of treating the risk factors of CVD should is needed.
Therefore, it is important to select individuals who can benefit from preventive treatment. For this purpose, CVD risk prediction models were developed and used to identify high-risk patients with future CVD events and those who can benefit from risk factor treatment. This approach is also important to avoid unnecessary treatment of low-risk patients, thus enhancing the cost-effectiveness and safety related to the treatment of CVD risk factors. In this regard, a recent guideline highlighted the importance of lifetime risk reduction because it is a more effective and beneficial approach to reduce the overall risk with a preventative strategy than the conventional approach.3 In this concept, the cutoff levels are different according to age groups to avoid undertreatment in the young and overtreatment in older persons. Prediction models incorporating lifetime risk may also be useful in patient-centered clinical decision-making because they deal with other characteristics, such as susceptibility to CVD and patient preferences.4 In this review, the problems of previous risk evaluation and prediction models are discussed and then a new concept of recommendation that reflects the importance of lifetime risk and optimized therapy for the primary prevention of CVD among younger and older individuals is introduced.
PROBLEMS WITH THE RISK EVALUATION AND MANAGEMENT MODEL
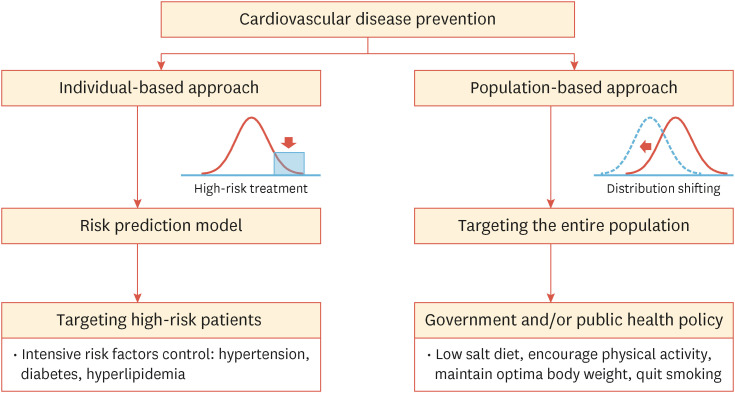
There are 2 different strategies for the prevention of CVD (Fig. 1).5 The first one is the “individual-based approach,” which identifies high-risk patients and targets those with a decreased CVD risk. The second approach is the “population-based approach,” which targets the overall population and aims to decrease the risk level among the whole population. The population-based approach is generally performed through national campaigns or policies, such as the recommendation of a low-salt diet, encouraging physical activity, and maintaining optimal blood pressure. Although the effect of a small reduction in the overall CVD risk is unexceptionally large, it is not easy to practice or sustain population-based global risk reduction.
Fig. 1. Two different strategies for cardiovascular disease prevention.
In contrast, the individual-based approach is effective and feasible, and is usually performed in daily clinical practice. However, a substantial number of CVD events occur among intermediate- or low-risk groups; thus, this approach should be facilitated by a well-established risk prediction model and intensive treatment for the high-risk group. In the individual-based approach, assessment of the CVD risk is the initial and essential part of CVD prevention strategies. Accordingly, most guidelines suggest an appropriate risk prediction model; thus, there are several available risk stratification models such as the Framingham risk score, pooled cohort equations, Assessing Cardiovascular Risk using the Scottish Intercollegiate Guidelines Network, Systematic Coronary Risk Evaluation (SCORE), Prospective Cardiovascular Münster Study, and Qresearch Cardiovascular Disease Risk Algorithm to evaluate the future risk of CVD.6,7 However, previous reports showed that the estimated risk was higher than the actual events rate. Liu et al.8 reported that the Framingham risk assessment tool overestimated the actual CVD event in a Chinese cohort study. In addition, the American College of Cardiology (ACC)/American Heart Association (AHA) 2013 pooled cohort equations overestimated the risk of CVD among the Korean population.9 These findings might be related to the differences in ethnic backgrounds or CVD prevalence in Asian countries. However, a study of a European population aged 55 years or older also significantly overestimated the actual risk of CVD events. This overestimation might lead to the overtreatment of risk factors, such as statin therapy for hypercholesterolemia. In fact, the ACC/AHA guidelines recommended statin therapy for nearly all men and two-thirds of women, proportions exceeding those with the Adult Treatment Panel-III or European Society of Cardiology (ESC) guidelines.10 This is derived from the fact that the risk stratification model was developed from a previous cohort study. However, the incidence of CVD decreased, and the management of CVD risk factors improved during this period.11 Accordingly, the risk prediction model frequently overestimated the actual event rate of CVD.12
In addition, the risk of CVD is highly age-dependent; thus, age is the strongest predictor of CVD in risk prediction models. However, the relationship between traditional risk factors and CVD is attenuated with aging, leading to the overestimation of CVD risk and potential benefit from risk factor treatment in older persons.13 This incorrect prediction leads to unnecessary treatment, polypharmacy, increased risk of adverse drug events, reduced quality of life, and increased medical costs among older patients. Moreover, healthy older people with minimal or no CVD risk factors can be classified as candidates for statin treatment only according to their age. In addition, traditional risk prediction models predict all-cause mortality, but not non-fatal cardiovascular events. Thus, CVD risk is overestimated in older people because of the increased risk of non-cardiovascular mortality. This also leads to the overestimation of CVD risk and overtreatment of CVD risk factors in older adults.
The benefit of treatment for CVD risk factors tends to decrease with age. The relative risk of developing CVD associated with higher systolic blood pressure and diastolic blood pressure is lower at older ages than at younger ages. However, the high blood pressure-related absolute CVD risk is higher in older persons due to the higher incidence rate of CVD events at an older age.14 Further, there is limited evidence favoring the treatment of risk factors among older adults.
For this reason, the pooled cohort risk equations have poor performance in risk prediction for older individuals.15 Finally, the lifetime benefit of risk factor treatment is smaller in older people than in younger people due to the limitation of life.
UNDERSTANDING THE CONCEPT OF LIFETIME RISK EVALUATION AND MANAGEMENT
The prevention of CVD through risk factor management should be performed from a lifetime perspective. The 10-year CVD risk in young and healthy people is low, even in the presence of high-risk profiles; however, the lifetime CVD risk is substantially high.16 These characteristics should be considered in the decision-making process for managing younger individuals. For example, in apparently healthy adults (<50 years), a 10-year CVD risk >7.5% is classified as a very high-risk group because this risk relates to a high lifetime risk; thus, treatment of CVD risk factors should be recommended.17
Accordingly, recent guidelines have incorporated the concept of “lifetime risk” in treatment recommendations to highlight the importance of treatment for younger individuals with substantial risk factor burden who do not yet have a high 10-year risk of CVD.18 The early treatment will result in small absolute risk reductions at younger ages; however, the benefit of early intervention will be larger over one’s lifespan.
The lifetime benefit from risk factor management can be estimated by combining lifetime risk models derived from previous studies.19 There are online calculators to estimate the lifetime CVD risk and benefit of CVD risk factor management, such as smoking cessation, lipid lowering, and blood pressure lowering on an individual patient level.20 Yet, there are no definite thresholds for the lifetime benefit to recommend or initiate the intervention. Additionally, the estimated lifetime benefit should be considered based on the duration of treatment. The duration of lifelong risk factor treatment is longer among young individuals than among older people. This characteristic should be considered in a shared decision-making process between healthcare providers and patients. Besides the expected treatment harms and costs that must be considered, the desired treatment benefit needs to be established. Lifetime benefits are easy to interpret and may improve communication in shared decision-making processes. This may also increase patient engagement, self-efficacy, and the motivation to adhere to lifestyle changes and drug treatment.17
RECENT UPDATE OF RISK PREDICTION MODEL AND CARDIOVASCULAR PREVENTION GUIDELINE
Age is a major risk factor for CVD; thus, older individuals are considered a high-risk group. However, the benefit of lifelong management of risk factors is greater in younger individuals. Thus, the risk thresholds for treatment should be lower in younger people. In addition, it should be noted that the total CVD risk is a continuum; all cutoff values to define risk categories are arbitrary. In general, CVD risk can be labelled as “high” when the chance of developing CVD is high, and a reduction in CVD risk is effective and cost-efficient. However, cutoff values should differ according to the economic conditions and prevalence of the disease in specific countries.
SCORE is a risk estimation system endorsed by the ESC and integrated in the ESC prevention guideline.21 The SCORE system is based on a dataset from 12 large European cohorts including 205,000 participants free of CVD at baseline, aged 40 to 65 years. The model estimates the risk of the first fatal CVD event within the next 10 years. Two versions of SCORE were produced, low- and high-risk countries, and 4 different risk categories (low, moderate, high, and very high-risk) were suggested. The SCORE model has several advantages and limitations as well. The model is based on risk factor levels and CVD mortality rates in cohorts examined many years ago. Nevertheless, the incidence of ASCVD has declined recently; thus, the model may have overestimated the total ASCVD risk. In addition, there is a huge variation in the incidence between many European countries. To overcome this limitation, a new model, SCORE 2, was developed, validated, and published.22 SCORE 2 provides risk estimates for fatal and non-fatal CVD events. It has also been systematically recalibrated using contemporary CVD rates among 4 distinct European regions defined by varying CVD risk levels. SCORE 2 is limited to adults aged <70 years. However, approximately two-thirds of all CVD deaths in Europe occur in the population aged 75 years and older. Moreover, CVD is responsible for substantial morbidity and a reduction in quality of life. Thus, the SCORE 2 working group developed and published an updated SCORE 2 Older Persons system for the prediction of CVD risk for adults older than 70 years of age.23
In the 2021 ESC prevention guideline, the cutoff values for ASCVD risk differ according to age group to avoid undertreatment in young individuals and overtreatment in older persons (Table 1).17 As age is a major driver of CVD risk, the lifelong risk factor treatment benefit is higher in younger people than in older people, and the suggested risk thresholds for preventive treatments are lower for younger patients than for older patients.
Table 1. Atherosclerotic cardiovascular disease risk categories based on SCORE 2 and SCORE 2 Older Persons (10-year risk of a fatal or a non-fatal cardiovascular disease event) in healthy people according to age.
| Risk group | <50 yr | 50–69 yr | ≥70 yr |
|---|---|---|---|
| Low to moderate-risk | <2.5% | <5% | <7.5% |
| High-risk | 2.5% to <7.5% | 5% to <10% | 7.5% to <15% |
| Very high-risk | ≥7.5% | ≥10% | ≥15% |
SCORE, Systematic Coronary Risk Evaluation.
Similar age-dependent different recommendations for CVD risk factor management have been published in the United States (U.S.) as well. The U.S. Preventive Services Task Force recommended prescribing a statin for primary prevention of CVD in adults aged 40–75 year who have one or more CVD risk factor and an estimated 10-year CVD risk >10%. However, it stated that the current evidence is insufficient to assess the balance between the benefits and harms of starting statin therapy for primary prevention among healthy adults older than 75 years of age.24 This statement was based on the lack of evidence regarding the benefits of statin therapy among older patients, especially for primary prevention purposes.25 A recent study regarding the effect of ezetimibe on Japanese adults aged over 75 years showed that it decreased the risk of primary outcome (a composite of sudden cardiac death, myocardial infarction, coronary revascularization, or stroke) among patients without a history of any CVD or stroke. The efficacy and safety of ezetimibe for the primary prevention of CVD should be tested in another ethnic group.26
Aspirin therapy for primary prevention has changed among older patients. Due to the lack of benefits among relatively healthy older adults, aspirin therapy was not recommended for primary prevention purposes in patients aged 60 years or older.27
Similarly, the goal of glucose control should differ based on the health status of older adults with diabetes mellitus. For healthy adults aged over 65 years who have a longer life expectancy, the recommended target hemoglobin A1c (HbA1c) goal is less than 7.0%–7.5%. However, the target goal is less than 8.0% for older adults with complex medical conditions or impaired functional status. The guidelines recommend that the HbA1c level alone should not be relied on, but instead glucose control decisions should be based on avoiding hypoglycemia and symptomatic hyperglycemia in frail or dependent older adults with a very limited life expectancy because the benefit of intensive glucose control in these patients is uncertain.28
REVIEW OF RECENT KOREAN DYSLIPIDEMIA GUIDELINE
The recent guideline highlighted the importance of aggressive management of dyslipidemia in high-risk patients. Thus, the new Korean Guidelines for the Management of Dyslipidemia (the 5th edition) recommended a stricter (lower) target goal for patients with coronary artery disease. In addition, for high-risk diabetes patients, patients having diabetes for more than 10 years, major risk factors (age [men ≥45 years, women ≥55 years], family history of premature ASCVD, hypertension, smoking, and low high-density lipoprotein-cholesterol level [<40 mg/dL]), or target organ damage (albuminuria, chronic kidney disease [estimated glomerular filtration rate <60 mL/min/1.73 m2], retinopathy, neuropathy, left ventricular hypertrophy), the target goal of low-density lipoprotein (LDL) cholesterol management changed from less than 70 mg/dL to 55 mg/dL. Finally, patients with acute myocardial infarction are recommended to receive statin therapy irrespective of their LDL cholesterol level.
However, there was no difference in the recommendation of statin therapy based on the age of the patients. A recent publication regarding the risk score of future CVD in 182 countries showed that the Korean middle age group (40–64 years) had the lowest 10-year risk of CVD. Based on the risk prediction model, only 1% of them were at high-risk of CVD. In other words, if you focus on the high-risk group, we may lose a substantial number of patients who had a considerable life-time risk of future CVD. Moreover, the life-expectancy of Korean people exceed that of people in other countries and Korea is estimated to become the most aged country in the world by 2030.29 Accordingly the early management of dyslipidemia is of greater importance among the relatively healthy Korean adults.
FUTURE PERSPECTIVE OF RISK STRATIFICATION; BIOMARKER, ARTIFICIAL INTELLIGENCE (AI), AND PERSONALIZED PREDICTION
In the 2021 ESC guideline, the population was divided into 3 distinct age groups (<50, 50–69, and >70 years), and the cutoff values for the risk groups were different according to the 3 age groups. However, age is continuous, and there was no reason to support a rapid change among the 3 different age groups. As a result, any increase in age is associated with an increase in the cutoff values for CVD risk thresholds. In addition, there may be a group of individuals showing heterogeneity, even in the same age group. Accordingly, one should always remember its purpose when using these cutoff values in risk stratification. There is no definite risk threshold, which implies mandatory treatment for risk factors. The decision to begin risk factor management is a matter of individual considerations and shared decision-making. Being in a certain risk group should not be translated to initiating statin or antihypertensive drug treatment.
In this regard, novel biomarkers can provide precise information that is helpful for decisions related to risk factor management. In the 2021 ESC prevention guideline, any tests for potential risk modifiers such as genetic risk scores and circulating or urinary biomarkers are not recommended. Yet, risk estimation can be improved by the evaluation of subclinical ASCVD. Among them, the coronary artery calcium score (CACS) is a good surrogate marker of subclinical ASCVD and independently predicts the risk of ASCVD. Risk estimates provided by the CACS can improve the accuracy of the ASCVD risk, especially among individuals in the moderate-risk group. However, the CACS has a limited ability to reclassify the ASCVD risk into low or very high ASCVD risk groups. Carotid ultrasonography, which can detect atheromatous plaques, is an alternative method for risk evaluation. These surrogate markers are especially helpful for decision-making regarding drug treatment in the intermediate ASCVD risk group. Further studies regarding the clinical efficacy and cost-effectiveness of imaging biomarker-based risk evaluations are required.
Genetic risk scores will also be helpful in identifying individuals at an increased risk for coronary heart disease. Thus, people with a higher genetic risk can receive the largest clinical benefit from statin therapy.30 Thus, with the use of a genetic risk score, we can provide different treatment strategies, although their risk groups are the same. However, the polygenic risk score for CVD was not captured by guideline-based clinical risk algorithms and was not reflected in current daily clinical practice.31 In the near future, with the increase in genetic testing, which will enable us to know about the genetic risk score more easily, incorporation of the genetic risk score into guideline-based primary prevention algorithms will improve risk prediction and individual-based personal treatment.
Finally, AI, a field of computer science that can mimic human thought processes, learning capacity, and knowledge storage, can help identify the high-risk group and estimate the risk of the population. A previous study showed that a machine learning model can predict the presence and extent of subclinical atherosclerosis in young, asymptomatic individuals.32 The information derived from AI can be used to select high-risk individuals who can benefit from intensive risk factor management. Although there is limited evidence supporting the role of AI-based risk prediction in clinical practice, it will open a new era in risk prediction and risk management in the near future. In particular, diverse data can be gathered with the use of various wearable devices, social media, electronic health data, and multiple “omic” data. Accordingly, the power of AI in CVD risk prediction and management will be greater in terms of processing big data to predict future risk.33
CONCLUSIONS
It is beneficial to treat hypertension, diabetes mellitus, and dyslipidemia, even among older persons. However, the absolute and relative risks associated with the presence of well-established CVD risk factors should be individualized considering age, (sub)clinical organ damage, and other risk factors. In particular, current guidelines underscore the importance of the lifetime risk of CVD and propose different recommendations according to age group. Guidelines can be referred to when we treat patients in our clinic, but we should not follow the recommendation without considering the patients’ characteristics. In the near future, clinical, biochemical, and imaging parameters will be used to stratify cardiovascular risk and provide more detailed information regarding the risk management of individual patients. AI will provide a big data-based individualized risk evaluation and targeted approach for the prevention of CVD.
Footnotes
Funding: None.
Conflict of Interest: The author has no conflicts of interest to declare.
Data Availability Statement: Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1.Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 2.Spencer-Bonilla G, Chung S, Sarraju A, Heidenreich P, Palaniappan L, Rodriguez F. Statin use in older adults with stable atherosclerotic cardiovascular disease. J Am Geriatr Soc. 2021;69:979–985. doi: 10.1111/jgs.16975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkelmans GF, Gudbjörnsdottir S, Visseren FL, Wild SH, Franzen S, Chalmers J, et al. Prediction of individual life-years gained without cardiovascular events from lipid, blood pressure, glucose, and aspirin treatment based on data of more than 500 000 patients with type 2 diabetes mellitus. Eur Heart J. 2019;40:2899–2906. doi: 10.1093/eurheartj/ehy839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emberson J, Whincup P, Morris R, Walker M, Ebrahim S. Evaluating the impact of population and high-risk strategies for the primary prevention of cardiovascular disease. Eur Heart J. 2004;25:484–491. doi: 10.1016/j.ehj.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Siontis GC, Tzoulaki I, Siontis KC, Ioannidis JP. Comparisons of established risk prediction models for cardiovascular disease: systematic review. BMJ. 2012;344:e3318. doi: 10.1136/bmj.e3318. [DOI] [PubMed] [Google Scholar]
- 7.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 8.Liu J, Hong Y, D’Agostino RB, Sr, Wu Z, Wang W, Sun J, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004;291:2591–2599. doi: 10.1001/jama.291.21.2591. [DOI] [PubMed] [Google Scholar]
- 9.Jung KJ, Jang Y, Oh DJ, Oh BH, Lee SH, Park SW, et al. The ACC/AHA 2013 pooled cohort equations compared to a Korean Risk Prediction Model for atherosclerotic cardiovascular disease. Atherosclerosis. 2015;242:367–375. doi: 10.1016/j.atherosclerosis.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 10.Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, Steyerberg EW, et al. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014;311:1416–1423. doi: 10.1001/jama.2014.2632. [DOI] [PubMed] [Google Scholar]
- 11.Matheny M, McPheeters ML, Glasser A, Mercaldo N, Weaver RB, Jerome RN, et al. Systematic review of cardiovascular disease risk assessment tools. Rockville (MD): Agency for Healthcare Research and Quality (US); 2011. [PubMed] [Google Scholar]
- 12.Rana JS, Tabada GH, Solomon MD, Lo JC, Jaffe MG, Sung SH, et al. Accuracy of the atherosclerotic cardiovascular risk equation in a large contemporary, multiethnic population. J Am Coll Cardiol. 2016;67:2118–2130. doi: 10.1016/j.jacc.2016.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeFilippis AP, Young R, McEvoy JW, Michos ED, Sandfort V, Kronmal RA, et al. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur Heart J. 2017;38:598–608. doi: 10.1093/eurheartj/ehw301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383:1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nanna MG, Peterson ED, Wojdyla D, Navar AM. The accuracy of cardiovascular pooled cohort risk estimates in U.S. older adults. J Gen Intern Med. 2020;35:1701–1708. doi: 10.1007/s11606-019-05361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329. doi: 10.1056/NEJMoa1012848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Visseren FL, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–3337. doi: 10.1093/eurheartj/ehab484. [DOI] [PubMed] [Google Scholar]
- 18.Jaspers NE, Blaha MJ, Matsushita K, van der Schouw YT, Wareham NJ, Khaw KT, et al. Prediction of individualized lifetime benefit from cholesterol lowering, blood pressure lowering, antithrombotic therapy, and smoking cessation in apparently healthy people. Eur Heart J. 2020;41:1190–1199. doi: 10.1093/eurheartj/ehz239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 20.Pedretti RF, Hansen D, Ambrosetti M, Back M, Berger T, Ferreira MC, et al. How to optimize the adherence to a guideline-directed medical therapy in the secondary prevention of cardiovascular diseases: a clinical consensus statement from the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2023;30:149–166. doi: 10.1093/eurjpc/zwac204. [DOI] [PubMed] [Google Scholar]
- 21.Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 22.SCORE2 Working Group and ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42:2439–2454. doi: 10.1093/eurheartj/ehab309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.SCORE2-OP Working Group and ESC Cardiovascular Risk Collaboration. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur Heart J. 2021;42:2455–2467. doi: 10.1093/eurheartj/ehab312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Preventive Services Task Force. Mangione CM, Barry MJ, Nicholson WK, Cabana M, Chelmow D, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2022;328:746–753. doi: 10.1001/jama.2022.13044. [DOI] [PubMed] [Google Scholar]
- 25.Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393:407–415. doi: 10.1016/S0140-6736(18)31942-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouchi Y, Sasaki J, Arai H, Yokote K, Harada K, Katayama Y, et al. Ezetimibe Lipid-Lowering Trial on Prevention of Atherosclerotic Cardiovascular Disease in 75 or Older (EWTOPIA 75): a randomized, controlled trial. Circulation. 2019;140:992–1003. doi: 10.1161/CIRCULATIONAHA.118.039415. [DOI] [PubMed] [Google Scholar]
- 27.US Preventive Services Task Force. Davidson KW, Barry MJ, Mangione CM, Cabana M, Chelmow D, et al. Aspirin use to prevent cardiovascular disease: US Preventive Services Task Force recommendation statement. JAMA. 2022;327:1577–1584. doi: 10.1001/jama.2022.4983. [DOI] [PubMed] [Google Scholar]
- 28.ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 13. Older adults: standards of care in diabetes-2023. Diabetes Care. 2023;46:S216–S229. doi: 10.2337/dc23-S013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389:1323–1335. doi: 10.1016/S0140-6736(16)32381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mega JL, Stitziel NO, Smith JG, Chasman DI, Caulfield M, Devlin JJ, et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet. 2015;385:2264–2271. doi: 10.1016/S0140-6736(14)61730-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aragam KG, Dobbyn A, Judy R, Chaffin M, Chaudhary K, Hindy G, et al. Limitations of contemporary guidelines for managing patients at high genetic risk of coronary artery disease. J Am Coll Cardiol. 2020;75:2769–2780. doi: 10.1016/j.jacc.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sánchez-Cabo F, Rossello X, Fuster V, Benito F, Manzano JP, Silla JC, et al. Machine learning improves cardiovascular risk definition for young, asymptomatic individuals. J Am Coll Cardiol. 2020;76:1674–1685. doi: 10.1016/j.jacc.2020.08.017. [DOI] [PubMed] [Google Scholar]
- 33.Krittanawong C, Zhang H, Wang Z, Aydar M, Kitai T. Artificial intelligence in precision cardiovascular medicine. J Am Coll Cardiol. 2017;69:2657–2664. doi: 10.1016/j.jacc.2017.03.571. [DOI] [PubMed] [Google Scholar]