Abstract
Objective
Non-high-density lipoprotein cholesterol (non-HDL-C) may be equivalent to or superior to low-density lipoprotein cholesterol (LDL-C) for the prediction of cardiovascular disease (CVD). However, studies comparing the predictive values of LDL-C and non-HDL-C levels for CVD have yielded conflicting results. In this study, we evaluated the relationship between non-HDL-C, LDL-C, and CVD using a large-scale population dataset from the National Health Information Database (NHID).
Methods
We performed a retrospective observational cohort study of 3,866,366 individuals ≥ 20 years, from 2009 to 2018, using the NHID. The participants were divided into LDL-C and non-HDL-C quartiles. The outcome variables included stroke, myocardial infarction (MI), and both. All outcomes were analyzed using Cox proportional hazards regression analysis while controlling for baseline covariates (age, sex, smoking, drinking, regular exercise, body mass index, diabetes, hypertension, and statin use).
Results
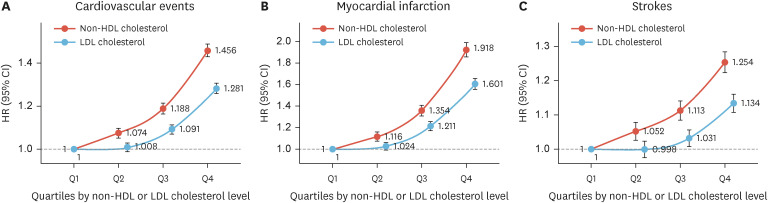
During 9.1 years of mean follow-up, stroke was diagnosed in 60,081 (1.55%), MI in 31,234 (0.81%), and both stroke and MI in 88,513 (2.29%) participants. Multivariate-adjusted hazard ratios (HRs) for patients in the highest non-HDL-C quartile demonstrated that these patients had a higher risk of stroke (HR, 1.254; 95% confidence interval [CI], 1.224–1.285), MI (HR, 1.918; 95% CI, 1.853–1.986), and both (HR, 1.456; 95% CI, 1.427–1.486) compared with participants in the lowest quartile. These were higher than the HRs for patients in the highest LDL-C quartile for stroke (HR, 1.134; 95% CI, 1.108–1.160), MI (HR, 1.601; 95% CI, 1.551–1.653), and both (HR, 1.281; 95% CI, 1.257–1.306).
Conclusion
In our large population study, higher non-HDL-C levels were associated with CVD than LDL-C levels.
Keywords: Statin, Cholesterol, Cardiovascular disease, Myocardial infarction, Stroke
INTRODUCTION
Extensive evidence from epidemiological, genetic, and clinical intervention studies on the pathophysiology of cholesterol-rich low-density lipoprotein (LDL) is directly implicated in the development of Atherosclerotic Cardiovascular Disease (ASCVD).1,2 Large randomized placebo-controlled trials have demonstrated a coherent and consistent negative relationship between the reduction in LDL cholesterol levels and ASCVD risk.2 Therefore, most guidelines target lowering LDL cholesterol to prevent ASCVD and recommend treatment goals for LDL cholesterol levels.3,4,5 Three drug classes (statins, proprotein convertase subtilisin/kexin type 9 [PCSK9] inhibitors, and ezetimibe) successfully lowered LDL cholesterol levels and prevented ASCVD and relative death. Although they achieved the LDL cholesterol goal, there was substantial uneliminated dyslipidemia-related residual risk.6 Although LDL cholesterol plays a principal role in the development of ASCVD, evidence for a causal relationship between other apolipoprotein B (apoB)-containing lipoproteins including very low-density lipoproteins (VLDLs) and their remnants, intermediate density lipoproteins (IDLs), and lipoprotein(a) [Lp(a)], and ASCVD is emerging.7,8,9
Non-high-density lipoprotein (HDL) cholesterol is calculated as total cholesterol minus HDL cholesterol and is a measure of the cholesterol content of atherogenic apoB-containing lipoproteins: VLDL, IDL, LDL, chylomicron remnants, and Lp(a).10 Numerous observational studies have established a positive association between LDL cholesterol levels and ASCVD risk; however, few have focused on non-HDL cholesterol levels and ASCVD risk.10 In this study, we evaluated the relationship between non-HDL-C, LDL-C, and cardiovascular disease (CVD) using a large-scale population dataset from the National Health Information Database (NHID).
MATERIALS AND METHODS
1. Study database
This is a retrospective, cohort study obtained and analyzed from the NHID, a public database on healthcare utilization and screening that contains sociodemographic and mortality information for the entire population of South Korea. The NHID, which is produced by the National Health Insurance Service, was launched in 2000 by integrating 375 insurance associations and contains data from 2002 to 2018. It provides longitudinal data for 97% of the Korean population, linked to the National Death Registry and National Health Screening Program.11,12 This program was initiated in 2009 and includes a medical interview, postural examination, chest X-ray examination, blood tests (including fasting glucose and triglyceride levels), urine tests, dental screening, and additional functions. The study protocol was approved by the Institutional Review Board of Hanyang University Guri Hospital (GURI 2020-03-021). The requirement for informed consent was waived by the board.
2. Study participants
From the NHID, 4,234,337 people aged ≥20 years participated in the national health screening program in 2009. Among the 4,234,337 participants, we excluded 367,971 participants (171,970 individuals lacking complete data, 57,344 with a history of myocardial infarction (MI), and 138,657 with a history of stroke). Consequently, 3,866,366 eligible participants were enrolled in this national cohort study.
3. Definitions of study outcomes
The outcomes of the study were newly diagnosed MI, stroke, or both. Stroke was defined as International Classification of Diseases 10th Revision (ICD-10) codes I63 or I64 during hospitalization with claims for brain magnetic resonance imaging or brain computerized tomography, and MI was defined as ICD-10 codes I21 or I22 during hospitalization. The study population was followed up from baseline to the date of death, the onset of a cardiovascular event, or until December 31, 2018, whichever came first. The secondary outcomes of the study were prespecified as the individual components of the primary outcome.
4. Clinical and laboratory measurements
All participants completed a questionnaire on their medical history, use of tobacco and alcohol, and exercise habits. Smoking habits were categorized as a non-smoker, ex-smoker, or current smoker. Alcohol habits were classified as non-drinkers, moderate drinkers (<30 g/day), or heavy drinkers (≥30 g/day). Regular exercise was defined as vigorous-intensity exercise three or more times per week or moderate-intensity exercise five or more times per week. Body mass index (BMI) was calculated as body weight (kg) divided by height (m2). Blood pressure (BP) was measured using a standard procedure with a sphygmomanometer after resting for more than 5 minutes. Blood samples were collected after an overnight fast. Serum glucose, total cholesterol, triglyceride (TG), HDL cholesterol, and LDL cholesterol levels were measured. We calculated the glomerular filtration rate using the four-variable Modification of Diet in Renal Disease Study equation.13 Baseline comorbidities included hypertension (ICD-10 codes I10–I13 or I15 and treatment with antihypertensive medications, systolic BP ≥140 mmHg, or diastolic BP ≥90 mmHg), type 2 diabetes (ICD-10 codes E11–E14 and antidiabetic drugs or fasting glucose level ≥126 mg/dL), and hyperlipidemia (ICD-10 code E78 with lipid-lowering agents or serum total cholesterol ≥240 mg/dL).
5. Data analyses
The baseline characteristics were analyzed using descriptive statistics. Categorical variables were described as frequencies and percentages. Continuous variables were described as mean ± standard deviation (SD) for normally distributed data and as geometric mean and 95% confidence interval (CI) for non-normally distributed data. We compared the baseline non-HDL and LDL cholesterol quartile characteristics of the participants. Continuous variables were compared using one-way analysis of variance, whereas categorical variables were compared using the chi-square test. The follow-up duration of each non-HDL and LDL cholesterol quartile group was determined. The incidence rates of stroke, MI, and cardiovascular events (MI or stroke) were estimated for each non-HDL and LDL cholesterol quartile over the entire follow-up period. All outcomes were analyzed using Cox proportional hazards regression analysis while controlling for baseline covariates. Statistical significance was set at a two-tailed p value less than 0.05. Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and the R program (version 3.4.1; The R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org).
RESULTS
1. Baseline characteristics of participants
The characteristics of the quartile groups, based on non-HDL cholesterol levels, are shown in Table 1. The group with higher non-HDL levels were older, more likely to be men, current smokers, heavy drinkers, and statin users; less likely to have lower household income; had a higher BMI, fasting plasma glucose level, total cholesterol level, LDL cholesterol level, TG level, systolic blood pressure, and diastolic blood pressure; had a lower HDL cholesterol level, and had a higher prevalence of diabetes, hypertension, and dyslipidemia. Similar patterns of baseline characteristics were noted in the quartile groups according to LDL cholesterol level (Supplementary Table 1). The proportion of statin users (n=248,494) among the participants was 6.43%.
Table 1. Characteristics according to quartiles of non-HDL cholesterol level of 5,586,048 persons from the National Health Information Database in 2009 in Korea.
| Variables | Non-HDL quartiles | |||||
|---|---|---|---|---|---|---|
| Q1 (<114 mg/dL) | Q2 (≥114 and <138 mg/dL) | Q3 (≥138 and <164 mg/dL) | Q4 (≥164 mg/dL) | p-value | ||
| No. of participants | 959,579 | 986,931 | 965,906 | 953,950 | ||
| Age (yr) | 42.23±14.34 | 45.58±13.7 | 47.85±13.16 | 49.85±12.67 | <0.001 | |
| <65 yr | 871,369 (90.81) | 881,681 (89.34) | 849,273 (87.93) | 823,461 (86.32) | ||
| ≥65 yr | 88,210 (9.19) | 105,250 (10.66) | 116,633 (12.07) | 130,489 (13.68) | ||
| Sex | <0.001 | |||||
| Men | 468,696 (48.84) | 540,932 (54.81) | 566,993 (58.7) | 560,940 (58.8) | ||
| Women | 490,883 (51.16) | 445,999 (45.19) | 398,913 (41.3) | 393,010 (41.2) | ||
| Household income | <0.001 | |||||
| Lower 20% | 180,249 (18.78) | 173,950 (17.63) | 162,869 (16.86) | 160,005 (16.77) | ||
| Smoking | <0.001 | |||||
| Non-smoker | 609,254 (63.49) | 593,849 (60.17) | 551,184 (57.06) | 527,588 (55.31) | ||
| Ex-smoker | 112,111 (11.68) | 137,949 (13.98) | 150,023 (15.53) | 149,082 (15.63) | ||
| Current-smoker | 238,214 (24.82) | 255,133 (25.85) | 264,699 (27.4) | 277,280 (29.07) | ||
| Alcohol drinking | <0.001 | |||||
| None/mild | 463,319 (48.28) | 493,971 (50.05) | 492,201 (50.96) | 505,301 (52.97) | ||
| Moderate | 418,322 (43.59) | 414,596 (42.01) | 394,946 (40.89) | 369,990 (38.79) | ||
| Heavy | 77,938 (8.12) | 78,364 (7.94) | 78,759 (8.15) | 78,659 (8.25) | ||
| Regular physical activity | 166,478 (17.35) | 180,489 (18.29) | 179,636 (18.6) | 171,720 (18.0) | <0.001 | |
| Body mass index (kg/m2) | 22.36±3.07 | 23.36±3.11 | 24.13±3.09 | 24.86±3.09 | <0.001 | |
| Glucose (mg/dL) | 93.4±20.51 | 95.38±21.12 | 97.56±22.77 | 101.34±28.06 | <0.001 | |
| Total cholesterol (mg/dL) | 155.55±19.11 | 181.51±14.88 | 203.06±14.6 | 240.97±26.89 | <0.001 | |
| HDL-cholesterol (mg/dL) | 61.31±28.4 | 55.77±13.61 | 53.26±12.92 | 51.42±12.32 | <0.001 | |
| Non-HDL-cholesterol (mg/dL) | 94.25±25.61 | 125.74±6.87 | 149.79±7.43 | 189.55±24.27 | <0.001 | |
| LDL-cholesterol (mg/dL) | 77.61±16.87 | 102.48±14.75 | 121.16±17.89 | 151.61±30.48 | <0.001 | |
| Difference between Non-HDL and LDL cholesterol (mg/dL) | 16.64±26.09 | 23.27±13.77 | 28.63±17.04 | 37.94±25.61 | <0.001 | |
| Triglyceride* (mg/dL) | 79.47 (79.4–79.55) | 100.77 (100.66–100.87) | 123.55 (123.42–123.68) | 159.65 (159.47–159.82) | <0.001 | |
| SBP (mmHg) | 118.76±14.48 | 121.19±14.64 | 123.3±14.73 | 125.57±15.05 | <0.001 | |
| DBP (mmHg) | 73.97±9.75 | 75.6±9.85 | 76.97±9.91 | 78.42±10.07 | <0.001 | |
| Type 2 diabetes | 64,788 (6.75) | 68,151 (6.91) | 76,725 (7.94) | 98,431 (10.32) | <0.001 | |
| Hypertension | 178,911 (18.64) | 221,904 (22.48) | 255,923 (26.5) | 299,924 (31.44) | <0.001 | |
| Dyslipidemia | 70,770 (7.38) | 53,793 (5.45) | 58,437 (6.05) | 447,585 (46.92) | <0.001 | |
| Statin | 71,865 (7.49) | 54,074 (5.48) | 47,357 (4.9) | 75,198 (7.88) | <0.001 | |
HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure; DBP, diastolic blood pressure.
*Geometric mean (95% confidence interval).
2. Non-HDL & LDL cholesterol level and cardiovascular events (MI or stroke)
There were 88,513 (2.29%) cardiovascular events in the 9.14-year mean follow-up period (Table 2). The incidence rate of cardiovascular events was 2.51 per 1,000 person-years. Patients in the lowest quartile of non-HDL cholesterol level (1.70 per 1,000 person-years) and 2nd quartile of LDL cholesterol (2.10 per 1,000 person-years) showed the lowest incidence rate of cardiovascular events (Table 2). The age- and sex-adjusted hazard ratios (HR) for MI and/or stroke increased for the 2nd (1.074; 95% CI, 1.051–1.097), 3rd (1.188; 95% CI, 1.164–1.213), and 4th (1.456; 95% CI, 1.427–1.486) non-HDL quartiles compared to the 1st quartile (p for trend <0.001, Table 2). In addition, in a multivariate-adjusted model for age, sex, alcohol consumption, regular physical activity, BMI, diabetes, hypertension, and statin medication, there was a significant and progressive increase in the risk of cardiovascular events with increasing non-HDL cholesterol levels (Fig. 1A). However, cardiovascular events had a U-shaped association with LDL cholesterol levels in age- and sex-adjusted models, and a J-shaped association with LDL cholesterol levels in a multivariate-adjusted model for age and sex, alcohol consumption, regular physical activity, BMI, diabetes, hypertension, and statin medication (Fig. 1A).
Table 2. Number, incidence rate, and hazard ratio for cardiovascular events (myocardial infarction or stroke) Stratified by non-HDL and LDL cholesterol.
| Variables | No. of patients | No. of event | Duration, person-years | Rate, events per 1,000 person-years | Non-adjusted | Model 1 | Model 2 | |
|---|---|---|---|---|---|---|---|---|
| Non-HDL cholesterol | ||||||||
| Q1 | 959,579 | 14,927 | 8,773,254 | 1.70 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | |
| Q2 | 986,931 | 19,105 | 9,038,909 | 2.11 | 1.242 (1.215–1.269) | 1.050 (1.027–1.072) | 1.074 (1.051–1.097) | |
| Q3 | 965,906 | 23,255 | 8,835,420 | 2.63 | 1.547 (1.515–1.579) | 1.174 (1.150–1.199) | 1.188 (1.164–1.213) | |
| Q4 | 953,950 | 31,226 | 8,684,464 | 3.60 | 2.113 (2.072–2.155) | 1.491 (1.462–1.520) | 1.456 (1.427–1.486) | |
| p for trend | <0.001 | <0.001 | <0.001 | |||||
| LDL cholesterol | ||||||||
| Q1 | 976,661 | 19,187 | 8,904,531 | 2.15 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | |
| Q2 | 975,502 | 18,776 | 8,936,121 | 2.10 | 0.974 (0.955–0.994) | 0.942 (0.923–0.961) | 1.008 (0.988–1.029) | |
| Q3 | 934,272 | 21,091 | 8,553,002 | 2.47 | 1.144 (1.121–1.166) | 1.008 (0.988–1.028) | 1.091 (1.069–1.113) | |
| Q4 | 979,931 | 29,459 | 8,938,393 | 3.30 | 1.528 (1.501–1.556) | 1.196 (1.174–1.218) | 1.281 (1.257–1.306) | |
| p for trend | <0.001 | <0.001 | <0.001 | |||||
Model 1: adjusted for age and sex.
Model 2: adjusted for age and sex, alcohol consumption, regular physical activity, body mass index, diabetes, hypertension, and statin use.
HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Fig. 1. The risk of cardiovascular events, myocardial infarction, and stroke stratified by the quartile of non-HDL and LDL cholesterol levels after adjusting for age and sex, alcohol consumption, regular physical activity, body mass index, diabetes, hypertension, and statin medication.
HR, hazard ratio; CI, confidence interval; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
3. Non-HDL & LDL cholesterol level and myocardial infarction, and stroke
There were 31,234 (0.81%) MI and 60,081 (1.55%) stroke cases during the follow-up period. The incidence rates of MI and stroke were 0.88 and 1.70 per 1,000 person-years, respectively (Supplementary Tables 2 and 3). In a multivariate-adjusted model for age, sex, alcohol consumption, regular physical activity, BMI, diabetes, hypertension, and statin medication use, there was a significant and progressive increase in the risk of MI and stroke with increasing non-HDL cholesterol level quartiles (Fig. 1B and C). However, MI and stroke had a J-shaped association with LDL cholesterol levels in a multivariate-adjusted model for age and sex, alcohol consumption, regular physical activity, BMI, diabetes, hypertension, and statin medication use (Fig. 1B and C).
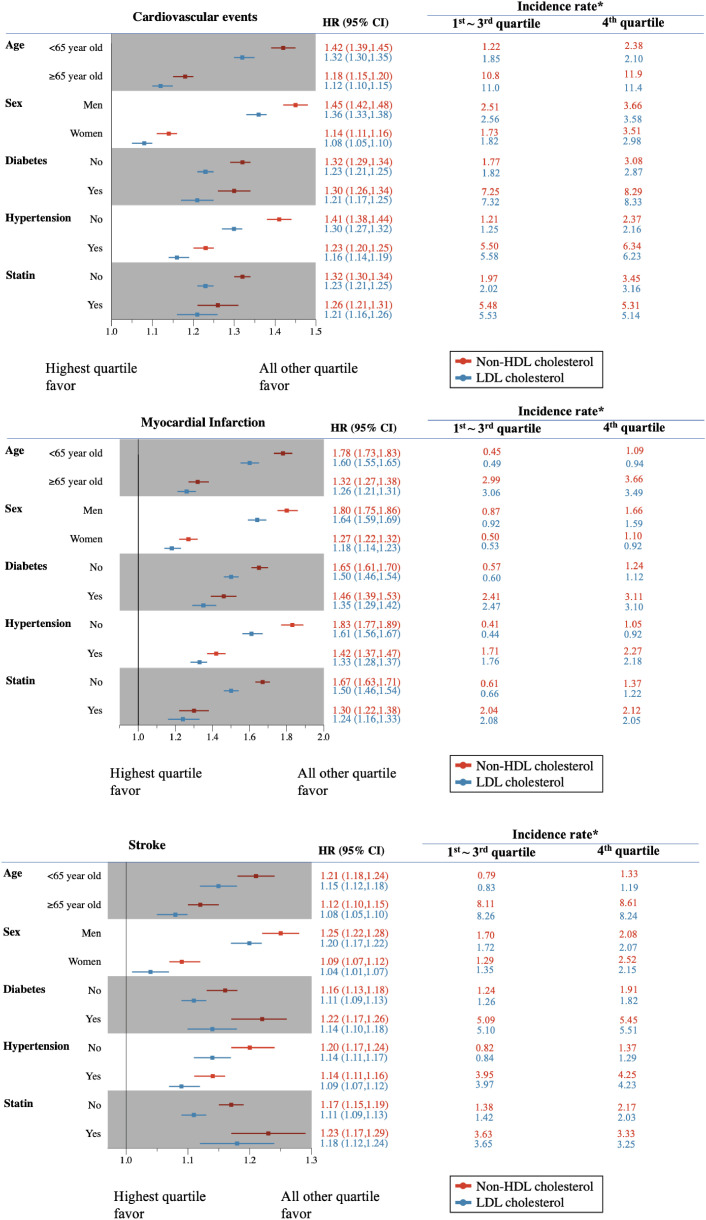
4. Sensitivity analysis: effects of clinical variables on the associations between Non-HDL & LDL cholesterol level and cardiovascular events, MI, and stroke
The associations between non-HDL cholesterol levels and study outcomes were constant across subgroups according to age, sex, diabetes, hypertension, and statin use after multivariate adjustment (Fig. 2). The associations between LDL cholesterol level and study outcomes were constant across subgroups according to age, sex, diabetes, hypertension, and statin use after multivariate adjustment, except for the association between LDL cholesterol level and stroke in women (Fig. 2). All subgroups showed a higher risk of study outcomes in the highest quartile of non-HDL cholesterol compared with all other quartiles of non-HDL cholesterol than that in the highest quartile of LDL cholesterol compared with all other quartiles of LDL cholesterol (Fig. 2). When participants were divided into decile or Korean dyslipidemia guidelines recommended the target by non-HDL and LDL cholesterol levels, above 118 mg/dL non-HDL cholesterol level and above 103 mg/dL LDL cholesterol level was associated with a higher risk of cardiovascular events (MI or stroke) compared to the lowest decile of non-HDL and LDL cholesterol levels (Fig. 3).
Fig. 2. The risk of cardiovascular events, myocardial infarction, and stroke according to the prespecified subgroup comparing the highest quartile of non-HDL or LDL cholesterol level with all others after adjusting for age and sex, alcohol consumption, regular physical activity, body mass index, diabetes, hypertension, and statin medication (*events per 1,000 person-years).
HR, hazard ratio; CI, confidence interval; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Fig. 3. The risk of cardiovascular events according to (A) the decile of non-HDL cholesterol & LDL-cholesterol level comparing with the lowest decile of non-HDL or LDL cholesterol level, and (B) Korean dyslipidemia guideline recommended target of non-HDL cholesterol and LDL cholesterol levels after adjusting for age and sex, alcohol consumption, regular physical activity, body mass index, diabetes, hypertension, and statin medication use (*events per 1,000 person-years).
HDL, high-density lipoprotein; LDL, low-density lipoprotein; HR, hazard ratio; CI, confidence interval.
DISCUSSION
We investigated the association between non-HDL-C and LDL-C levels and CVD using a longitudinal national representative cohort dataset. High non-HDL cholesterol was associated with a significantly increased risk of upcoming cardiovascular events, and these findings were consistent even after adjusting for possible confounders, such as other cardiovascular risk factors, and in all subgroup analyses. Patients with higher non-HDL cholesterol levels were more likely to have a higher risk of CVD than those with higher LDL cholesterol. Although the results of an observational study should be interpreted with caution, this large nationwide observational study with 3,866,366 participants showed that high non-HDL levels could be a significant predictor of future cardiovascular events than LDL cholesterol levels.
Studies focusing on the association between non-HDL cholesterol levels and CVD are limited. The Systolic Hypertension in Elderly Program (1996) was one of the first studies to describe an association between non-HDL cholesterol levels and CVD risk.14 In this study, one SD increase in non-HDL cholesterol and LDL cholesterol levels was associated with a 1.32 (95% CI, 1.13–1.54) and 1.19 (95% CI, 1.02–1.39) times relative risk increasement, respectively.14 The Women’s Health Study done on 15,632 women aged ≥45 years showed that the extreme quintiles of apoB and non-HDL cholesterol had comparable associations with the risk of upcoming cardiovascular events (2.50 [95% CI, 1.68–3.72] and 2.51 [95% CI, 1.69–3.72], respectively), and both were stronger than that for the extreme quintiles of LDL cholesterol (1.75; 95% CI, 1.30–2.38).15 However, other study with 44,234 patients showed that HRs per 1 SD change of LDL cholesterol which was measured directly instead of Friedewald formula, and non-HDL cholesterol change for upcoming cardiovascular events were similar; 1.38 (95% CI, 1.09–1.73) and 1.42 (95% CI, 1.06–1.91), respectively.16 The European Prospective Investigation of Cancer-Norfolk prospective population study showed that the association between non-HDL-cholesterol and LDL-C and the risk of CHD was largely comparable with the HRs per 1 SD increase of 1.26 (95% CI, 1.20–1.31) for non-HDL cholesterol and 1.22 (95% CI, 1.17–1.27) for LDL cholesterol.17 Consistent with the findings of the previous studies, we confirmed that the highest quartile of non-HDL cholesterol was significantly associated with an increased risk of upcoming cardiovascular events when compared with the lowest quartile of non-HDL cholesterol (HR, 1.397; 95% CI, 1.367–1.428), and it was stronger than that for the highest quartile of LDL cholesterol (HR, 1.202; 95% CI, 1.177–1.227). Non-HDL cholesterol was consistently useful for predicting upcoming cardiovascular events regardless of age, sex, presence or absence of diabetes, hypertension, and statin use. A meta-analysis of eight statin trials comprising 38,153 statin-treated patients showed that non-HDL-C (HR, 1.16; 95% CI, 1.12–1.19) had the strongest association with cardiovascular events when compared with LDL-C (HR, 1.13; 95% CI, 1.10–1.17).18
Most dyslipidemia guidelines recommend LDL cholesterol as a primary target and non-HDL cholesterol as secondary goals.3,4,19 The guideline recommended that the specific goal for non-HDL cholesterol should be 30 mg/dL higher than the corresponding LDL cholesterol goal, which assumed 150 mg/dL of TG level.3,4,19 However, a recent study suggested that LDL cholesterol levels of 70 and 100 mg/dL correspond to non-HDL-C levels of 93 and 125 mg/dL, respectively in healthy participants.17 Another study reported that LDL cholesterol levels of 74 mg/dL corresponded to 92 mg/dL of non-HDL cholesterol levels.20 These studies proposed that a conversion factor of 30 mg/dL may be too high. Our study results support this opinion. In our study, the difference between non-HDL cholesterol and LDL cholesterol levels was 22 mg/dL in the lowest decile, 32 mg/dL in the highest decile, and 30 mg/dL in patients with >140 mg/dL of LDL cholesterol level (Fig. 3). Around the LDL cholesterol goal (<55, 70, 100, 116 mg/dL), a conversion factor of 30 mg/dl may have been too high in our study.
The strength of our study is that we used a large-scale nationwide database representing the entire Korean population. Second, we conducted fully adjusted analyses with all available confounding factors and sensitivity analyses for cardiovascular risk factors. However, this study has some limitations. First, the retrospective observational study design has inherent limitations. Although the analyses were adjusted for most available demographic and clinical variables, some unidentified parameters could have affected the results. Second, we defined MI and stroke using claims data; however, this may not be a completely accurate method for determining the number of cases. To overcome this problem, we defined outcomes with the operational definition by combining diagnosis during hospitalization and prescription records, such as brain magnetic resonance imaging and brain computerized tomography.
In conclusion, we demonstrated that higher non-HDL cholesterol level is associated with a higher risk of cardiovascular events and that this association is stronger than that of LDL cholesterol levels using a longitudinal national representative cohort dataset. However, this did not indicate a causal relationship because of the inherent limitations of the observational study design.
Footnotes
Funding: This study was supported by a big data analysis grant from the Korean Society of Lipids and Atherosclerosis (KSOLA2020-03-006).
The funding agency had no role in the design, collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Conflict of Interest: The authors have no conflicts of interest to declare.
The funding source had no role in the collection of the data or in the decision to submit the manuscript for publication. Jung Hwan Park is an editor of Journal of Lipid and Atherosclerosis; however, he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Data Availability Statement: The data that support the findings of this study are available from the National Health Insurance Sharing Service (NHISS, https://nhiss.nhis.or.kr/). However, restrictions apply regarding the availability of the data, which were used with permission for the present study, and are therefore not publicly available. However, they may be made available through the corresponding author, upon reasonable request and with permission from the NHISS.
- Conceptualization: Hong S, Lee CB, Kim DS.
- Data curation: Hong S, Han K.
- Formal analysis: Han K.
- Funding acquisition: Hong S.
- Investigation: Hong S, Park JH, Yu SH, Lee CB.
- Methodology: Hong S, Park JH, Yu SH, Lee CB.
- Project administration: Hong S, Yu SH.
- Resources: Hong S.
- Software: Hong S.
- Supervision: Lee CB, Kim DS.
- Visualization: Hong S.
- Writing - original draft: Hong S.
- Writing - review & editing: Han K, Park JH, Yu SH, Lee CB, Kim DS.
SUPPLEMENTARY MATERIALS
Characteristics according to quartiles of LDL cholesterol levels of 5,586,048 persons from the National Health Information Database in 2,009 in Korea
Number, incidence rate, and hazard ratio for myocardial infarction and stroke stratified by non-high-density lipoprotein cholesterol level
Number, incidence rate, and hazard ratio for myocardial infarction and stroke stratified by low-density lipoprotein cholesterol levels
References
- 1.Goldstein JL, Brown MS. A century of cholesterol and coronaries: from plaques to genes to statins. Cell. 2015;161:161–172. doi: 10.1016/j.cell.2015.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38:2459–2472. doi: 10.1093/eurheartj/ehx144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205. doi: 10.1016/j.atherosclerosis.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Rhee EJ, Kim HC, Kim JH, Lee EY, Kim BJ, Kim EM, et al. 2018 Guidelines for the management of dyslipidemia in Korea. J Lipid Atheroscler. 2019;8:78–131. doi: 10.12997/jla.2019.8.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: A report of the american college of cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2019;140:e596–e646. doi: 10.1161/CIR.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braunwald E. Control of residual dyslipidaemic risk. Eur Heart J. 2022;43:3824–3825. doi: 10.1093/eurheartj/ehac359. [DOI] [PubMed] [Google Scholar]
- 7.Nordestgaard BG. Triglyceride-rich lipoproteins and atherosclerotic cardiovascular disease: new insights from epidemiology, genetics, and biology. Circ Res. 2016;118:547–563. doi: 10.1161/CIRCRESAHA.115.306249. [DOI] [PubMed] [Google Scholar]
- 8.Hegele RA, Ginsberg HN, Chapman MJ, Nordestgaard BG, Kuivenhoven JA, Averna M, et al. The polygenic nature of hypertriglyceridaemia: implications for definition, diagnosis, and management. Lancet Diabetes Endocrinol. 2014;2:655–666. doi: 10.1016/S2213-8587(13)70191-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301:2331–2339. doi: 10.1001/jama.2009.801. [DOI] [PubMed] [Google Scholar]
- 10.Verbeek R, Hovingh GK, Boekholdt SM. Non-high-density lipoprotein cholesterol: current status as cardiovascular marker. Curr Opin Lipidol. 2015;26:502–510. doi: 10.1097/MOL.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 11.Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes Metab J. 2014;38:395–403. doi: 10.4093/dmj.2014.38.5.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46:e15. doi: 10.1093/ije/dyv319. [DOI] [PubMed] [Google Scholar]
- 13.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 14.Frost PH, Davis BR, Burlando AJ, Curb JD, Guthrie GP, Jr, Isaacsohn JL, et al. Serum lipids and incidence of coronary heart disease. Findings from the Systolic Hypertension in the Elderly Program (SHEP) Circulation. 1996;94:2381–2388. doi: 10.1161/01.cir.94.10.2381. [DOI] [PubMed] [Google Scholar]
- 15.Ridker PM, Rifai N, Cook NR, Bradwin G, Buring JE. Non-HDL cholesterol, apolipoproteins A-I and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA. 2005;294:326–333. doi: 10.1001/jama.294.3.326. [DOI] [PubMed] [Google Scholar]
- 16.Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sondermeijer BM, Rana JS, Arsenault BJ, Shah PK, Kastelein JJ, Wareham NJ, et al. Non-HDL cholesterol vs. apo B for risk of coronary heart disease in healthy individuals: the EPIC-Norfolk prospective population study. Eur J Clin Invest. 2013;43:1009–1015. doi: 10.1111/eci.12129. [DOI] [PubMed] [Google Scholar]
- 18.Boekholdt SM, Arsenault BJ, Mora S, Pedersen TR, LaRosa JC, Nestel PJ, et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: a meta-analysis. JAMA. 2012;307:1302–1309. doi: 10.1001/jama.2012.366. [DOI] [PubMed] [Google Scholar]
- 19.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ballantyne CM, Pitt B, Loscalzo J, Cain VA, Raichlen JS. Alteration of relation of atherogenic lipoprotein cholesterol to apolipoprotein B by intensive statin therapy in patients with acute coronary syndrome (from the Limiting UNdertreatment of lipids in ACS With Rosuvastatin [LUNAR] Trial) Am J Cardiol. 2013;111:506–509. doi: 10.1016/j.amjcard.2012.10.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics according to quartiles of LDL cholesterol levels of 5,586,048 persons from the National Health Information Database in 2,009 in Korea
Number, incidence rate, and hazard ratio for myocardial infarction and stroke stratified by non-high-density lipoprotein cholesterol level
Number, incidence rate, and hazard ratio for myocardial infarction and stroke stratified by low-density lipoprotein cholesterol levels