Abstract
Background
Ogden type IV tibial tuberosity fractures, defined as a type of fracture with posterior–inferior metaphyseal extension (Salter-Harris type II variant), are uncommon but challenging pediatric fractures. The purpose of this study was to investigate the clinical and radiological presentation and associated surgical outcomes.
Methods
Ten previously healthy patients who had been surgically treated at the authors’ institution between 2015 and 2018 with at least 2 years of postoperative follow-up were included. Demographic, clinical, and radiological characteristics and treatment/follow-up data were investigated.
Results
All included patients were male. All injuries resulted from jump-landings. Unacceptable remaining angular deformity after closed reduction, particularly increased posterior tibial slope angle, was the leading cause of surgery. All preoperative magnetic resonance images (MRIs) showed entrapped periosteum on the anteromedial side of the proximal tibial physis. Surgical removal of the entrapped periosteum achieved successful reduction. Metaphyseal fracture angles between the fracture plane of the metaphyseal beak and the posterior tibial condyle on the axial image of MRI were relatively constant, with an average of 24.3° ± 6.0°. Mean bone age at the time of trauma was older than mean chronological age (16.4 ± 1.0 years vs. 14.6 ± 1.1 years, respectively; p = 0.005). All patients reached skeletal maturity within 2 postoperative years, with little posttraumatic residual height growth (mean, 1.6 ± 0.7 cm from injury to skeletal maturity). At final follow-up, no patients showed significant angular deformity, tibial length discrepancy, or functional deficit.
Conclusions
In healthy adolescents, Ogden type IV tibial tuberosity fractures typically occur by jump-landing injuries, when they have little residual growth remaining. Therefore, accurate fracture reduction was required because of limited remodeling potential. Patients with unacceptable reduction should be investigated for entrapped periosteum on the anteromedial side of the physis because it was the primary obstacle in achieving adequate reduction.
Keywords: Tibial tuberosity fracture, Ogden type IV, Growth plate, Surgery, Periosteal entrapment
Tibial tuberosity fractures occur primarily in active adolescent boys and are usually accompanied by growth plate damage.1,2) When ossification progresses, the tibial tuberosity becomes vulnerable to tensile force, resulting in an avulsion fracture.3) Injury is primarily caused by movements that require sudden contraction of the quadriceps muscle or knee flexion against contraction, occurring mostly in sports involving jump-landings.4) This tensile force causes the patella tendon to pull the tibial apophysis, causing a fracture originating from the distal part of the tibial tuberosity.5) It is relatively rare, comprising less than 1% of the total physeal injuries.6,7) However, proper assessment and treatment would be vital because it may cause deformity due to the nature of growth plate injury.
Ogden type IV tibial tuberosity fractures, defined as a type of fracture with the presence of posterior-inferior metaphyseal fracture extension,8) are regarded as a variant form of type II Salter-Harris growth plate injury and a common indication for surgery.9) Additionally, the major age group associated with this injury is adolescents with bone growth remaining, so understanding its presentation and clinical outcomes is essential. Although tibial tuberosity fractures in the adolescent group are well reported, few studies have investigated this specific Ogden type IV tibial tuberosity fracture.
This study therefore aimed to investigate the characteristics of Ogden type IV fractures in adolescents. We obtained preoperative magnetic resonance imaging (MRI) for all patients to review the fractures in detail. In addition, we evaluated residual growth until patients reached skeletal maturity and postoperative outcomes, including length discrepancies, angular deformities, and functional scores.
METHODS
Patient Selection
This study was approved by the Institutional Review Board of Asan Medical Center (No. 2021-0837). Informed consent was waived. The authors’ institute is a level I pediatric trauma center. Among the 23 patients aged 11–16 years who were surgically treated under the diagnosis of a tibial tuberosity avulsion fracture between January 2015 and December 2018, 13 with Ogden type IV were retrospectively reviewed. Among them, patients with underlying disease that could potentially affect the musculoskeletal system (2 girls with underlying osteogenesis imperfecta) and 1 patient with an additional fracture line extending to the epiphysis of the proximal tibia were excluded.10) Finally, 10 patients were included in the analysis. No cases of bilateral involvement were observed. All patients were followed up postoperatively for more than 2 years.
Diagnostic and Treatment Protocol for Ogden Type IV Tibial Tuberosity Fractures
Since 2015, the authors have treated patients with tibial tuberosity fractures according to the authors’ diagnostic and treatment protocol. Patients were assessed with anteroposterior (AP) and lateral simple radiographs of the knee and lower leg for their initial workup. Bone age was evaluated using radiographs of hand–wrist AP view, elbow AP–lateral view, and pelvis AP view with gonad shield. In the Ogden type IV fractures, knee MRI was obtained mainly for the purpose of identifying periosteal interposition at the fracture gap. Surgery was performed for patients with > 5° angulation or 1 cm displacement after manual reduction. All 10 patients were surgically indicated as the fracture angulation remained at more than 10° despite manual reduction.
The operation was performed under general anesthesia in the supine position. First, an oblique skin incision was made anteromedially to expose the anteromedial side of the proximal tibial physis. When the entrapped periosteum was identified at the physeal gap, surgical repositioning was performed. Next, the anteromedial side of the proximal tibial metaphysis was reduced and gently pushed toward the posterolateral side to maintain the reduction anatomically. The fracture was then fixed with two or three (three in most cases) appropriately sized screws (mainly, 6.5-mm cancellous screws) starting from medial and lateral to the tibial tuberosity (without violating the tibial apophysis) through the posterior metaphyseal beak. The screw on the lateral side of the tibial tuberosity was inserted percutaneously. One or two screws were intentionally inserted perpendicular to the metaphyseal fracture plane, expected by the metaphyseal fracture angle. Care was taken throughout the procedure to minimize damage to the growth plate.
Postoperative care included a long leg cast for 4–6 weeks with toe-touch weight-bearing. After removal of the cast, gentle knee range-of-motion exercises and crutch gait with tolerable weight-bearing were recommended for 1 month. Thereafter, patients were encouraged to return to their previous activity levels gradually. If a patient had limited knee motion at this time, tailored rehabilitation and physical therapy were initiated; however, these were often not required. Patients routinely visited the outpatient clinic for examination every 3–6 months till 24 months after surgery. AP and lateral radiographs of both knees and lower legs and full-length standing AP radiographs of both lower extremities including the hip, knee, and ankle in the standing position with the patella facing forward (teleradiograph) were obtained. Patients answered the Functional Status Questionnaire at the 2-year postoperative follow-up. Functional scores included Single Assessment Numeric Evaluation (SANE) score, Pediatrics Outcomes Data Collection Instrument (PODCI), and child-friendly EQ-5D version (EQ-5D-Y).11,12,13) Patients were asked to rate their injured knee as a percentage of normal (0%–100% scale with 100% being normal) to determine their SANE score. The Adolescent Outcomes Questionnaire (self-report for youths, 11–18 years of age) was used to measure PODCI, and 21 items corresponding to transfer/basic mobility and sports/physical fitness were evaluated. After scoring with 0–3 points for each item, the % score was calculated (0: severely disabled, 100: not disabled at all). Metal implant removal was usually performed between 6 months and 2 years after surgery after fracture unification was confirmed.
Radiological Evaluation
The evaluations of the patients are shown in Fig. 1. Simple radiographs were obtained preoperatively, immediately after surgery, and at each follow-up visit. Radiographs taken after the patient could stand upright appropriately and within postoperative 3 months were defined as initial, and those taken at 2-year postoperative follow-up were defined as final. The following two parameters were used for the fracture angulation in the sagittal and coronal planes. The posterior tibial slope was defined as the angle between the anatomical axis of the tibia and the tibial plateau on the lateral radiograph. The proximal tibial valgus angle was calculated in the coronal plane, defined as the angle between the anatomical axis of the tibia and the tibial plateau on the AP radiograph. Both angles were then compared with those of the contralateral uninjured side and were subsequently assigned a positive number when the fractured side had antecurvatum in the sagittal plane and valgus in the coronal plane. Tibial length discrepancy (TLD) and leg length discrepancy (LLD) were measured using a teleradiograph, and positive values were assigned when the fractured side was longer than the contralateral, uninjured side.
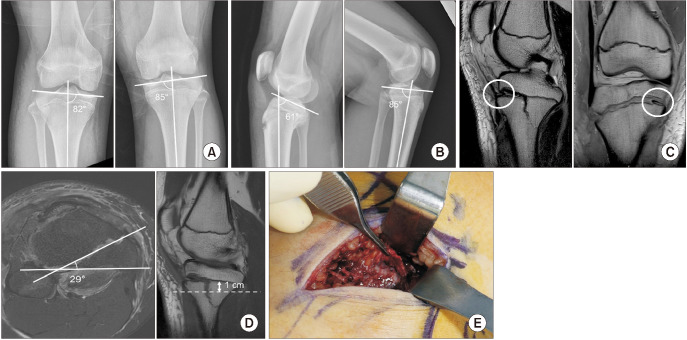
Fig. 1. A 14-year-old boy diagnosed with a right-side Ogden type IV tibial tuberosity fracture, who was injured while playing basketball (case 7). The preoperative radiographs showed remaining –3° of proximal tibial valgus angle and 24° of posterior tibial slope compared with the contralateral side on anteroposterior (A) and lateral (B) views after closed reduction in knee extension status. On the magnetic resonance imaging, there was anteromedial side periosteal entrapment (C, white circles) and the tibial metaphyseal angle was 29° on the axial plane where posterior beak of metaphyseal fracture most clearly seen, inferior to the physis (D, dotted line). (E) Periosteal entrapment was confirmed on the anteromedial side of the proximal tibia during surgery.
Three methods were used to assess skeletal maturity at the time of the injury. Bone age was calculated using the Greulich-Pyle method from hand and wrist AP radiographs, the Sauvegrain method from elbow AP and lateral radiographs,14,15) and Risser staging was assessed by ossification of iliac apophysis using teleradiographs.16)
Preoperative knee MRI was investigated for the metaphyseal fracture angle, presence of periosteal entrapment, and other knee joint pathologies. Metaphyseal fracture angle was measured on the axial view, inferior to the physis where posterior beak of a metaphyseal fracture is most clearly seen (around 1 cm distal to the proximal tibial physis). It was defined as an angle between the fracture plane of the metaphyseal beak and the posterior tibial condyle. All radiographs were stored and measured using the Picture Archiving and Communication System (Peta ver. 2.0; Asan Medical Center PACS).
Investigated Variables
Demographic factors, injury mechanisms, and postoperative complications were investigated in addition to the aforementioned radiological parameters. Chronological age, height, body mass index, sex, dominant leg, and fractured side were included in the demographics. The postoperative complications were determined according to the classification by Dindo et al.17)
Statistical Analysis
The Wilcoxon signed-rank test was used to compare the initial and final radiographic parameters and chronological age and associated bone age. A p-value of < 0.05 was considered statistically significant. All statistical analyses were conducted using IBM SPSS Statistics for Windows (ver. 21, IBM Corp.).
RESULTS
The demographics and injury characteristics of the included patients are presented in Table 1, their skeletal ages and posttraumatic growth in Table 2, radiological investigations in Table 3, and functional outcomes in Table 4.
Table 1. Demographics and Injury Characteristics of the Included Patients.
| Case | Age (yr)* | Sex | Dominant leg† | Injured side | Injury mechanism | BMI (at the time of injury) |
|---|---|---|---|---|---|---|
| 1 | 15.8 | Male | Right | Left | Jump-landing, badminton | 22.2 |
| 2 | 15.5 | Male | Right | Right | Jump-landing, basketball | 21.2 |
| 3 | 15.4 | Male | Right | Left | Jump-landing, soccer | 23.5 |
| 4 | 15.1 | Male | Right | Left | Jump-landing, basketball | 25.4 |
| 5 | 14.9 | Male | Right | Right | Jump-landing, basketball | 23.1 |
| 6 | 14.7 | Male | Right | Right | Jump-landing, basketball | 25.9 |
| 7 | 14.4 | Male | Right | Right | Jump-landing, basketball | 25.2 |
| 8 | 14.2 | Male | Left | Left | Jump-landing, soccer | 20.2 |
| 9 | 13.6 | Male | Right | Right | Jump-landing, basketball | 20.5 |
| 10 | 12.2 | Male | Right | Left | Jump-landing, high jump | 20.9 |
| Mean±SD | 14.6 ± 1.1 | Male: 10 | Right: 9, left: 1 | Right: 5, left: 5 | Jump-landing injury: 10 | 22.8 ± 2.1 |
BMI: body mass index, SD: standard deviation.
*Chronological age at the time of injury. †Preferred foot for kicking.
Table 2. The Results of Skeletal Maturity and Posttraumatic Growth of the Included Patients.
| Case | Skeletal maturity at the time of injury | Height (cm) | TLD (cm)* | LLD (cm)* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bone age (yr)† | Bone age (yr)‡ | Risser grade | Initial§ | FinalII | Height growth¶ | Initial§ | FinalII | Initial§ | FinalII | |
| 1 | 17 | > 15 | 4 | 175.0 | 176.3 | 1.3 | 0.0 | 0.0 | 0.0 | 1.2 |
| 2 | 17 | > 15 | 4 | 165.2 | 166.6 | 1.4 | 0.2 | 0.4 | 0.3 | 0.9 |
| 3 | 17 | > 15 | 3 | 179.8 | 180.9 | 1.1 | –0.1 | 0.3 | 0.0 | 0.5 |
| 4 | 16 | > 15 | 4 | 174.6 | 176.1 | 1.5 | 0.1 | –0.1 | 0.2 | 0.8 |
| 5 | 16 | > 15 | 4 | 177.5 | 179.8 | 2.4 | 0.2 | 0.2 | 0.3 | 0.9 |
| 6 | 17 | > 15 | 4 | 173.6 | 174.6 | 1.0 | –0.3 | –0.7 | –1.0 | 0.4 |
| 7 | 16 | > 15 | 4 | 163.0 | 164.7 | 1.7 | –0.2 | –0.1 | –0.3 | 0.7 |
| 8 | 17 | > 15 | 4 | 167.2 | 168.3 | 1.1 | 0.1 | –0.1 | –0.3 | 0.5 |
| 9 | 17 | > 15 | 4 | 168.0 | 169.4 | 1.4 | 0.0 | 0.1 | 0.3 | 1.1 |
| 10 | 14 | > 15 | 3 | 163.8 | 167.0 | 3.2 | 0.5 | –0.5 | –0.3 | 0.6 |
| Mean±SD | 16.4 ± 1.0 | - | - | 170.8 ± 6.0 | 172.4 ± 5.9 | 1.6 ± 0.7 | 0.1 ± 2.3 | –0.1 ± 0.3 | –0.1 ± 0.4 | 0.8 ± 0.3 |
TLD: tibial length discrepancy, LLD: leg length discrepancy, SD: standard deviation.
*Positive value means the injured side is longer. †Bone age according to Greulich and Pyle.14) ‡Bone age according to Sauvegrain.15) §Checked within posttraumatic 3 months after the patient could stand upright appropriately. ∥At postoperative 2 years. All patients reached skeletal maturity at postoperative 2 years (final heights). ¶Height growth from initial to final (skeletally mature).
Table 3. Radiological Investigations of the Included Patients.
| Case | Posterior tibial slope (°)* | Proximal tibial valgus angle (°)* | Preoperative MRI | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Preop | Initial† | Final‡ | Preop | Initial† | Final‡ | Metaphyseal fracture angle (°)§ | Presence of periosteal entrapment | Other intralesion | |
| 1 | 10 | 2 | –6 | –1 | –2 | –2 | 12 | (+), AMII | - |
| 2 | 18 | –2 | –1 | –2 | –2 | –3 | 24 | (+), AMII | - |
| 3 | 12 | 0 | –5 | –2 | 0 | 1 | 29 | (+), AMII | - |
| 4 | 12 | 1 | 1 | 2 | –1 | –1 | 26 | (+), AMII | - |
| 5 | 14 | 4 | 3 | 1 | –2 | –2 | 27 | (+), AMII | - |
| 6 | 10 | 6 | 5 | 2 | –1 | 2 | 32 | (+), AMII | - |
| 7 | 24 | –1 | 0 | –3 | –2 | 0 | 29 | (+), AMII | PCL ganglion |
| 8 | 16 | 0 | 1 | 0 | –1 | 1 | 22 | (+), AMII | - |
| 9 | 12 | 0 | 2 | 0 | –2 | –2 | 25 | (+), AMII | - |
| 10 | 8 | –1 | –5 | –12 | –5 | –2 | 17 | (+), AMII | - |
| Mean±SD | 13.6 ± 4.7 | 0.9 ± 2.5 | –0.5 ± 3.7 | –1.5 ± 4.1 | –1.8 ± 1.3 | –0.8 ± 1.7 | 24.3 ± 6.0 | ||
MRI: magnetic resonance imaging, Preop: preoperative, AM: anteromedial, PCL: posterior cruciate ligament, SD: standard deviation.
*Compared with the contralateral uninjured side. †Checked within postoperative 3 months after the patient could stand upright appropriately. ‡At postoperative 2 years. All patients reached skeletal maturity at postoperative 2 years (final heights). §Measured on the MRI axial view at the level of 1 cm inferior to the physis. ∥Periosteum was confirmed to be entrapped on the anteromedial side of proximal tibial physis.
Table 4. Functional Outcomes at Final Follow-up (Postoperative 2 Years) of the Included Patients.
| Case | SANE | PODCI (%) | EQ-5D-Y |
|---|---|---|---|
| 1 | 100 | 100 | 100 |
| 2 | 100 | 100 | 100 |
| 3 | 80 | 100 | 100 |
| 4 | 95 | 100 | 100 |
| 5 | 93 | 100 | 100 |
| 6 | 85 | 98 | 100 |
| 7 | 90 | 99 | 100 |
| 8 | 100 | 100 | 100 |
| 9 | 100 | 99 | 90 |
| 10 | 100 | 100 | 100 |
| Mean ± SD | 94.3 ± 7.3 | 99.6 ± 0.7 | 99.0 ± 3.2 |
SANE: Single Assessment Numeric Evaluation, PODCI: Pediatric Outcomes Data Collection Instrument, EQ-5D-Y: child-friendly EQ-5D version, SD: standard deviation.
Preoperative Evaluation
All injuries were caused by jump-landing in male adolescents during various sporting activities (most commonly, basketball) (Table 1). Notably, the two patients excluded from the study because of underlying osteogenesis imperfecta (see the ‘Patient selection’ in Method section) were females who had been injured outside of sporting activity. Although their mean age was 14.6 ± 1.1 years (Table 1), their skeletal maturity was older: mean bone age by Greulich-Pyle method was 16.4 ± 1.0 years (p = 0.005). All patients presented with full skeletal maturity on their elbow radiographs and near full skeletal maturity on their pelvic radiographs (Table 2).
All patients underwent surgery to treat the unacceptable angular deformity remaining after closed reduction, especially the increased posterior tibial slope compared with the opposite uninjured side (Table 3). In all cases, preoperative MRIs showed entrapped periosteum on the anteromedial side of the proximal tibial physis, metaphyseal fracture line on the axial image started from posterolateral cortex and ended on the medial cortex of the tibia, and metaphyseal fracture angles were relatively consistent (24.3° ± 6.0°) (Table 3).
Operative Findings
The presence and location of the entrapped periosteum on the preoperative MRIs (entrapped on the anteromedial side of the proximal tibia) were confirmed during surgery (Fig. 1). The entrapped periosteum was the primary obstacle to adequate reduction, which was only successfully achieved after its removal in all cases. All reduced fractures were fixed securely and in a physeal-sparing manner using screws based on the metaphyseal fracture angle on the preoperative MRIs.
Postoperative Growth and Outcomes
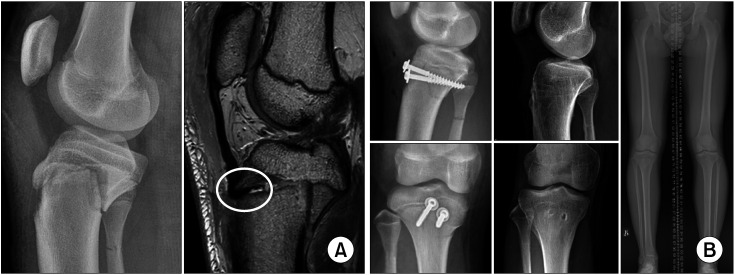
All patients reached Risser grade 5 (skeletally fully matured) during follow-up. Only minimal residual height growth was required for patients to achieve skeletal maturity (1.6 ± 0.7 cm) (Table 2). Although a statistically significant LLD was observed at the final follow-up (p = 0.005) (−0.1 ± 0.4 cm at initial vs. 0.8 ± 0.3 cm at final) (Table 2, Fig. 2), it was clinically insignificant. There was no significant TLD at the final follow-up (0.1 ± 2.3 cm at initial vs. −0.1 ± 0.3 cm at final, p = 0.526)(Table 2). No patients had significant postoperative complications, and there were no significant angular deformities or functional deficits at final follow-up (Table 4).
Fig. 2. A 13-year-old-boy diagnosed with a right-side Ogden type IV tibial tuberosity fracture (case 9). (A) He presented unacceptably increased posterior tibial slope with knee extension (left) and the main obstacle to adequate reduction was entrapped periosteum (white circle on right). (B) After the entrapped periosteum removed, the fracture was fixed with two screws by using the physeal sparing technique (left column). At the final follow-up, the patient did not present any significant angular deformity or length discrepancy (middle and right columns).
DISCUSSION
The authors investigated Ogden type IV tibial tuberosity fractures in adolescents, which are equivalent to the Salter-Harris type II growth plate injury. All the included patients were previously healthy males and their injuries occurred during various sporting activities. Preoperative MRIs revealed entrapped periosteum on the anteromedial side of the physis in all cases, which were confirmed during surgery as the main obstacle to adequate reduction. All patients had older bone ages at the time of injury compared with chronological age, and they reached skeletal maturity within 2 years of postoperative follow-up with minimal height growth.
Although it should be noted that those with underlying musculoskeletal disease had been already excluded from the study, all the included patients were male and their fractures resulted from jump-landing while participating in various sports (Table 1). Sex differences in fracture occurrence are well reported, highlighting that males are 10 times more at risk than females, which is largely attributed to greater male participation in more intense physical activities than female participation.18,19) It is important to note that boys typically have more muscle mass and strength than girls in late adolescence.2,20) Therefore, a sudden and forceful quadriceps contraction can cause violent tensile forces on the patella tendon, which overcomes physeal strength.2,21)
Two adolescent girls, who were excluded because of their underlying osteogenesis imperfecta, did not suffer any sports-induced injuries. One patient injured herself during rapid walking on the playground (chronological age of 14 years, bone age by Greulich–Pyle method of 14 years), and the others while jumping rope (chronological age of 11 years, bone age by Greulich-Pyle method of 10 years) (data not shown). Therefore, a typical Ogden type IV fracture appears to result from a jump-landing injury in active, healthy adolescent patients who are approaching skeletal maturity. However, if a patient exhibits characteristics of atypical features, the possibility of underlying musculoskeletal disorders should be considered.
The metaphyseal fracture line on the axial view presented a constant direction, with the posterior tibial cortex dividing into posteromedial and anterolateral sections (Table 3, Fig. 1D). This means that the anterolateral fragment was separated from the proximal tibial epiphysis, but the posteromedial fragment beak was connected to the proximal tibial epiphysis. This specific fracture pattern may arise due to the nature of the physeal closure pattern. Physeal closure of the proximal tibia occurs from the posterior to the anterior in medial to lateral directions.22) Early union of the posteromedial side may cause the constant posteromedial beak of metaphysis in Ogden type IV tibial tuberosity fractures. In addition, radiological skeletal maturity also appeared towards the end of skeletal growth (Table 2), with little expected growth remaining. The constant metaphyseal fracture pattern and older bone age are indicative of a precise transitional fracture. Transitional fractures typically occurred at the end of growth, at which bone remodeling ability would be lower compared with that of younger patients. Therefore, achieving accurate fracture reduction for those with displacement is essential. Additionally, since most patients have already reached their skeletal maturity, there would be no need to routinely evaluate bone age in Ogden type IV tibial tuberosity fractures unless a patient shows atypical presentation.
Periosteal entrapment was observed in the anteromedial aspect of proximal tibial physis on MRI in all patients, which was also confirmed consistently during surgery. There are limited data on the incidence and pattern of periosteal entrapment in tibial tuberosity fractures; therefore, our results will be of importance in surgical planning. In addition, a successful reduction was achieved only after the entrapped periosteum was repositioned. Thus, the surgical removal of periosteal entrapment on the anteromedial side of the physeal gap should be considered with unacceptable angulation/displacement after closed reduction. Indeed, several injuries may accompany a tibial tuberosity fracture, including knee joint damage to the articular cartilage, coronary ligament, or a meniscal tear,4,18,22) but no traumatic intra-articular pathologies were detected (Table 3). The traumatic force seems to have a limited impact on the knee joint. Considering our data, we question whether routine MRI is necessary to confirm intra-articular abnormalities in this type of fracture.
Fixation of the fracture was achieved using screws to minimize damage to the growth plate and showed excellent outcomes at the 2-year postoperative follow-up, including minimal fracture site angulation and favorable functional scores without major complications (Tables 3 and 4). We believe that a relatively strong fixing force could be achieved because at least one or two screws had been intentionally inserted perpendicular to the fracture plane, anticipated by the metaphyseal fracture angle. Because those patients are near the end of skeletal maturity and have little remaining growth (Table 2), the remodeling potential would be limited. Therefore, more accurate reduction is needed for Ogden type IV fractures. If it is difficult to maintain fracture reduction with only metaphyseal screws, more aggressive internal fixation, even violating the growth plate should be considered. Complications associated with tibial tuberosity fractures such as compartment syndrome or vascular compromise can have devastating results.23) Fortunately, no such complications occurred in the study, but close attention should be paid to prevent and detect such complications early during diagnosis and treatment.
At final follow-up, tibial lengths were almost equal, but the fractured side leg was longer than the uninjured side, although this was clinically insignificant. The increased LLD typically occurred on the femoral side rather than the tibia (Table 2). Overgrowth of the fractured limb is well described and may be explained by the effect of growth plate hyperactivity near the fracture site.24) In the late adolescent period, residual growth in the femur remains more than that of the tibia.25) Fracture of the proximal tibia may cause hyperactivation in the physes around the knee joint, and since residual growth remains primarily in the distal femur, the femur is susceptible to overgrowth. However, it is unclear whether this LLD originated from actual overgrowth or is actually a measurement error due to the small sample size. Further research with a larger sample size would be required to validate these findings.
It is important to remember the following considerations when interpreting the present results. First, the study included only a small sample size and had no comparison group. It was mainly because of the rarity of this type of fracture. The limitations of this small sample size and lack of a comparison group could possibly pose validity problems. However, patient information was collected sequentially without missing data, and evaluation of the patients was systematically performed according to our institution's protocol. Although the number of patients was small and further research with larger sample sizes and comparison groups are needed, we believe that this study provides useful clinical information on Ogden type IV fractures in a controlled study design. Second, our results do not indicate that preoperative MRI is required for Ogden type IV fractures. Rather, there seems little need for preoperative MRI in these fractures in patients without clinical signs of knee joint pathology. Third, we identified a few cases of Ogden type IV fractures with very small metaphyseal beaks, but they were accidentally excluded from the analysis. The patients included in our study showed clear Salter-Harris type 2 fractures on X-ray, with a metaphyseal beak of at least 1 cm. Therefore, further studies are needed for cases with only a small metaphyseal fracture extension. Finally, there was no diversity in sex after excluding two female patients with underlying osteogenesis imperfecta. However, this extreme sex ratio may partly be influenced by region, wherein adolescent girls’ participation in active sports is less common than that of adolescent boys.
Ogden type IV tibial tuberosity fractures typically occur from a jump-landing injury when little residual bone growth remains in healthy adolescents. As they have reached skeletal maturity and only little remodeling potential is remained, accurate fracture reduction is needed. In addition, periosteal entrapment is highly suspected on the anteromedial side of the physis in patients with unacceptable reduction, and surgical repositioning is required for them.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Schiller J, DeFroda S, Blood T. Lower extremity avulsion fractures in the pediatric and adolescent athlete. J Am Acad Orthop Surg. 2017;25(4):251–259. doi: 10.5435/JAAOS-D-15-00328. [DOI] [PubMed] [Google Scholar]
- 2.Zrig M, Annabi H, Ammari T, Trabelsi M, Mbarek M, Ben Hassine H. Acute tibial tubercle avulsion fractures in the sporting adolescent. Arch Orthop Trauma Surg. 2008;128(12):1437–1442. doi: 10.1007/s00402-008-0628-4. [DOI] [PubMed] [Google Scholar]
- 3.McKoy BE, Stanitski CL. Acute tibial tubercle avulsion fractures. Orthop Clin North Am. 2003;34(3):397–403. doi: 10.1016/s0030-5898(02)00061-5. [DOI] [PubMed] [Google Scholar]
- 4.Howarth WR, Gottschalk HP, Hosalkar HS. Tibial tubercle fractures in children with intra-articular involvement: surgical tips for technical ease. J Child Orthop. 2011;5(6):465–470. doi: 10.1007/s11832-011-0369-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jakoi A, Freidl M, Old A, Javandel M, Tom J, Realyvasquez J. Tibial tubercle avulsion fractures in adolescent basketball players. Orthopedics. 2012;35(8):692–696. doi: 10.3928/01477447-20120725-07. [DOI] [PubMed] [Google Scholar]
- 6.Franz P, Luderowski E, Tuca M. Tibial tubercle avulsion fractures in children. Curr Opin Pediatr. 2020;32(1):86–92. doi: 10.1097/MOP.0000000000000870. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton SW, Gibson PH. Simultaneous bilateral avulsion fractures of the tibial tuberosity in adolescence: a case report and review of over 50 years of literature. Knee. 2006;13(5):404–407. doi: 10.1016/j.knee.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Ryu RK, Debenham JO. An unusual avulsion fracture of the proximal tibial epiphysis: case report and proposed addition to the Watson-Jones classification. Clin Orthop Relat Res. 1985;(194):181–184. [PubMed] [Google Scholar]
- 9.Andrews KA, Gillette M, Shah RV, Mckean LA, Sanford CG. Type IV tibial tubercle fracture-Salter-Harris type II variant. J Surg Case Rep. 2019;2019(7):rjz209. doi: 10.1093/jscr/rjz209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pace JL, McCulloch PC, Momoh EO, Nasreddine AY, Kocher MS. Operatively treated type IV tibial tubercle apophyseal fractures. J Pediatr Orthop. 2013;33(8):791–796. doi: 10.1097/BPO.0b013e3182968984. [DOI] [PubMed] [Google Scholar]
- 11.Daltroy LH, Liang MH, Fossel AH, Goldberg MJ. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. Pediatric Outcomes Instrument Development Group. Pediatric Orthopaedic Society of North America. J Pediatr Orthop. 1998;18(5):561–571. doi: 10.1097/00004694-199809000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Wille N, Badia X, Bonsel G, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res. 2010;19(6):875–886. doi: 10.1007/s11136-010-9648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales: outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214–221. doi: 10.1177/03635465990270021701. [DOI] [PubMed] [Google Scholar]
- 14.Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. Redwood City: Stanford University Press; 1959. [Google Scholar]
- 15.Dimeglio A, Charles YP, Daures JP, de Rosa V, Kabore B. Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Joint Surg Am. 2005;87(8):1689–1696. doi: 10.2106/JBJS.D.02418. [DOI] [PubMed] [Google Scholar]
- 16.Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–119. [PubMed] [Google Scholar]
- 17.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cole WW, 3rd, Brown SM, Vopat B, Heard WM, Mulcahey MK. Epidemiology, diagnosis, and management of tibial tubercle avulsion fractures in adolescents. JBJS Rev. 2020;8(4):e0186. doi: 10.2106/JBJS.RVW.19.00186. [DOI] [PubMed] [Google Scholar]
- 19.Telford RM, Telford RD, Olive LS, Cochrane T, Davey R. Why are girls less physically active than boys?: findings from the LOOK longitudinal study. PLoS One. 2016;11(3):e0150041. doi: 10.1371/journal.pone.0150041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bassett AJ, Ahlmen A, Rosendorf JM, Romeo AA, Erickson BJ, Bishop ME. The biology of sex and sport. JBJS Rev. 2020;8(3):e0140. doi: 10.2106/JBJS.RVW.19.00140. [DOI] [PubMed] [Google Scholar]
- 21.Carius BM, Long B. Osgood-Schlatter disease as a possible cause of tibial tuberosity avulsion. Cureus. 2021;13(2):e13256. doi: 10.7759/cureus.13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agarwalla A, Puzzitiello R, Stone AV, Forsythe B. Tibial tubercle avulsion fracture with multiple concomitant injuries in an adolescent male athlete. Case Rep Orthop. 2018;2018:1070628. doi: 10.1155/2018/1070628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pretell-Mazzini J, Kelly DM, Sawyer JR, et al. Outcomes and complications of tibial tubercle fractures in pediatric patients: a systematic review of the literature. J Pediatr Orthop. 2016;36(5):440–446. doi: 10.1097/BPO.0000000000000488. [DOI] [PubMed] [Google Scholar]
- 24.Etchebehere EC, Caron M, Pereira JA, et al. Activation of the growth plates on three-phase bone scintigraphy: the explanation for the overgrowth of fractured femurs. Eur J Nucl Med. 2001;28(1):72–80. doi: 10.1007/s002590000395. [DOI] [PubMed] [Google Scholar]
- 25.Anderson M, Messner MB, Green WT. Distribution of lengths of the normal femur and tibia in children from one to eighteen years of age. J Bone Joint Surg Am. 1964;46:1197–1202. [PubMed] [Google Scholar]