Abstract
Background
Lateral elbow tendinopathy (LET) has an array of modalities described for its management. The present study analyzed two modalities used for managing the condition.
Methods
The present study included 64 non-athletes with LET who failed conservative treatment that included avoiding strenuous activities, ice-fomentation, non-steroidal anti-inflammatory drugs, bracing, and physiotherapy for 6 months. A random allocation of the participants was done, with one group injected with platelet-rich plasma (PRP) and the other group with corticosteroids. The procedure was performed by the same blinded orthopedic surgeon after localizing the pathology using ultrasound. Visual analog scale (VAS) scores, disabilities of the arm, shoulder and hand (DASH) scores, Patient-Rated Tennis Elbow Evaluation (PRTEE) scores, and handgrip strengths were recorded by blinded observers other than the surgeon administering the injection.
Results
The average age of the patients was 40 years. The mean VAS score at the latest follow-up of 2 years in the PRP group was 1.25 and it was significantly better than the score of 3.68 in the steroid group (p < 0.001). The mean DASH score at the latest follow-up of 2 years in the PRP group was 4.00 and it was significantly better than the score of 7.43 in the steroid group (p < 0.001). The mean PRTEE score at the latest follow-up of 2 years in the PRP group was 3.96 and it was significantly better than the score of 7.53 in the steroid group (p < 0.001). The scores were better in the steroid group at a short-term follow-up of 3 months (p < 0.05), while they were better in the PRP group at a long-term follow-up of 2 years (p < 0.05). Hand-grip strength was comparable in the PRP group (84.43 kg force) and steroid group (76.71 kg force) at the end of the 2-year follow-up with no statistically significant difference (p = 0.149).
Conclusions
Corticosteroid injections alleviated symptoms of LET over short-term follow-up providing quicker symptomatic relief; however, the effect faded off over the long term. PRP injections provided a more gradual but sustained improvement over the long-term follow-up, indicating the biological healing potential of PRP.
Keywords: Elbow, Tendinopathy, Ultrasound, Platelet-rich plasma, Corticosteroids
Lateral elbow tendinopathy (LET), loosely termed as “tennis elbow” is a gradual-onset degeneration of the extensor tendons near their site of origin at the lateral epicondyle. The extensor carpi radialis brevis (ECRB) is usually the commonest tendon affected, with other extensors also involved in a few cases. Although it was thought to be a purely inflammatory pathology as evidenced by the use of “itis”, the paradigm has now shifted, with degenerative etiology assumed to be more significant in the causation of this condition due to a better understanding of the underlying pathophysiology and the histological changes of fibroangiomatous hyperplasia. With the advances in the field of orthobiologics, the utilization of platelet-rich plasma (PRP) in a wide range of musculoskeletal conditions has increased tremendously. PRP is thought to stimulate repair of the tendon via increasing the concentration of growth factors in the local milieu, thereby helping in reversing the pathology responsible for the condition. Corticosteroids, on the other hand, mainly target the inflammation associated with the lesion and provide comfort till the initial wave of inflammation is ongoing without modifying the natural course of the disease. Based on this hypothesis, this study was designed to assess the efficacy of ultrasound (US)-guided PRP injections over US-guided steroid injections in patients with LET over a long-term follow-up of 2 years.
METHODS
After obtaining clearance from the Institutional Ethics Committee of Seth GS Medical College and KEM Hospital (No. EC/OA-16/2018) and written informed consent from all patients, the trial was conducted at the Department of Orthopaedics of our tertiary apex institute over 2 years from November 2019 to November 2021. A total of 84 patients were assessed for eligibility as per the inclusion criteria, following which 16 were excluded as they did not satisfy the inclusion criteria. Five patients had a history of diabetes. Four patients had a history of cervical radiculopathy. Three patients had anemia. Three patients were professional athletes. One patient had a history of rheumatoid arthritis (Table 1). Athletes, pregnant women, and patients with a history of anemia, bleeding disorders, and systemic disorders such as diabetes, hepatitis, and rheumatoid arthritis were excluded from the study. Those with a history of cervical radiculopathy and previous surgery for elbow tendinosis were also excluded. Patients who participated in a workers’ compensation program and those with a known allergy to corticosteroids were excluded. Sixty-eight patients who satisfied the inclusion criteria were randomly divided into two groups using a standardized randomization process with a random number generator (IBM SPSS ver. 26.0; IBM Corp., Armonk, NY, USA). Two patients in each group were lost to follow-up due to coronavirus disease 2019 (COVID-19) travel restrictions and hence, the total number of patients analyzed was 64 (Fig. 1). As chronic hyperglycemia can increase the risk of LET,1) patients with diabetes were excluded from the study. Although steroids or PRP would provide relief from the symptoms of LET, the underlying pathology of chronic hyperglycemia would have led to poor response to treatment along with an increase in the risk of recurrence, and diabetes would thus act as a confounding variable. Patients with US-guided steroid injections were assigned to one group, while patients with PRP injections were assigned to the other.
Table 1. Inclusion and Exclusion Criteria for the Enrollment of the Patients for the Study.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Age > 20 years and < 65 years | Athletes |
| History of persistent elbow pain for a minimum of 3 months | Pregnancy (as follow-up would be difficult) |
| Point tenderness at the lateral epicondyle of the elbow | Patients with a history of anemia, bleeding disorder, and systemic disorders such as diabetes, hepatitis, and rheumatoid arthritis |
| Pain not responding to analgesics, physical therapy, and bracing for a minimum of 6 months | History of cervical radiculopathy (as it is a differential diagnosis for LET) |
| Patients who underwent surgery previously for elbow tendinosis | |
| Patients with a known allergy to corticosteroids | |
| Patients who participated in a workers’ compensation program or any ongoing or planned legal action as a consequence of elbow pain |
LET: lateral elbow tendinopathy
Fig. 1. Consolidated Standards of Reporting Trials (CONSORT) 2010 flow diagram for the present randomized controlled trial showing the method of randomization. US: ultrasound, PRP: platelet-rich plasma, COVID: coronavirus disease.
The Technique of Injection
Thirty milliliters of blood was drawn from the peripheral vein of each patient. The blood drawn in one group was used for the preparation of PRP, while the blood was drawn from the participants in the other group to eliminate bias. US of the elbow performed by a dedicated radiologist (CR) helped to localize the site of pathology involving the ECRB fibers at their origin. A solution consisting of 1 mL of saline and 1 mL (40 mg) of triamcinolone acetonide was injected after the localization of the pathological lesion. For preparing PRP, blood was withdrawn from the patient using a 24 mL syringe that was preloaded with a solution of citrate phosphate dextrose. PRP preparation was performed using the standardized PRP method described in the literature.2) Differential centrifugation of the sample was done in two spins consisting of 1,800 rpm for 15 minutes for separating erythrocytes and white blood cells from other components of blood, followed by a second spin at 3,500 rpm for 10 minutes to concentrate the platelets. Approximately 3 mL of the obtained PRP was injected into the lesion after localization was achieved using US. The injections were given by an orthopedic surgeon (PK) who was unaware of the content of the injection he was administering as the syringe was covered using electrical insulation tape (black color). Oral antibiotics were administered to all patients 3 days after the procedure. The same protocol consisting of daily ice fomentation was followed in both groups. Non-steroidal anti-inflammatory drugs were avoided in both groups as they tend to interfere with platelet function. All patients were instructed to not participate in strenuous activities. The patients were asked to follow up at timely intervals and two observers (senior orthopedic residents; RMP and SP) blinded to the treatment independently assessed the patient for the mentioned parameters: visual analog scale (VAS) scores, disabilities of the arm, shoulder and hand (DASH) scores, Patient-Rated Tennis Elbow Evaluation (PRTEE) scores, and handgrip strength at timely intervals of 2 weeks, 1 month, 3 months, 6 months, 1 year, and 2 years. Among the values measured by the two independent observers, the better values were taken into consideration. Handgrip strength was calculated using the Jamar Hydraulic hand dynamometer (Bolingbrook, IL). We calculated the mean of three efforts (force in kg) with intervening 1-minute rest intervals. Successful treatment was defined as more than a 50% reduction in VAS or DASH score without re-intervention in 6 months. Failure was defined as less than 25% reduction in VAS or DASH score without re-intervention in 6 months or an increase in VAS or DASH score in 6 months. Improvement was defined as a reduction in VAS or DASH score up to 25%–50% of baseline. Recurrence was defined as an increase in VAS or DASH score above 50% of baseline any time after initially successful treatment. Considering a median level of 50%, the criteria for successful treatment was defined as more than 50% reduction in VAS or DASH score without re-intervention in 6 months.3)
Microsoft Excel (ver. 2007; Redmond, WA, USA) and SPSS for Windows software (IBM Corp.) were used for analyzing the data. The means of the two groups were compared using the unpaired t-test with the level of significance set at 0.05. The analysis of the scores at presentation and at successive intervals was done using the paired t-test with the level of significance set at 0.05.
RESULTS
The average age of the patients was 40 years with a range from 22 to 60 years. Left-sided involvement was seen in 21 cases, while right-sided involvement was seen in the remaining 43 cases. Of the total sample size, 29 were men and 35 were women. There was no difference in the baseline demographic characteristics between the two groups. The mean VAS score, DASH score, and PRTEE score at the latest follow-up of 2 years were 1.25, 4.00, and 3.96, respectively in the PRP group, whereas the mean VAS score, DASH score, and PRTEE score in the steroid group were 3.68, 7.43, and 7.53, respectively. The VAS scores were better in the steroid group at a short-term follow-up of 3 months (p < 0.001), while they were better in the PRP group at a long-term follow-up of 2 years (p < 0.001) (Table 2, Fig. 2). The DASH scores were better in the steroid group at a short-term follow-up of 3 months (p = 0.039), while they were better in the PRP group at a long-term follow-up of 2 years (p < 0.001) (Table 3, Fig. 3). The PRTEE scores were better in the steroid group at a short-term follow-up of 3 months (p = 0.048), while they were better in the PRP group at a long-term follow-up of 2 years (p < 0.001) (Table 4, Fig. 4). Treatment was successful in 31 patients in the PRP group (96%), out of which 2 patients showed a recurrence due to an increase in VAS score after 6 months. Treatment was considered improved in 1 patient in the PRP group, but he showed recurrence in 6 months after treatment. Treatment was successful in 20 patients in the steroid group (62%), of which 6 showed recurrence in 6 months. Treatment was considered improved in 12 patients in the steroid group, of which 4 showed recurrence in 6 months. The handgrip strengths showed improvement in both groups. However, there was no significant difference between the two groups at follow-up of 2 years (p = 0.149) (Table 5, Fig. 5). The improvement in VAS scores at a follow-up of 2 years was statistically significant in both groups (p < 0.001) (Table 2). The improvement in DASH scores at a follow-up of 2 years was statistically significant in both groups (p < 0.001) (Table 3). Similarly, the improvement in PRTEE scores at a follow-up of 2 years was statistically significant in both groups (p < 0.001) (Table 4). This suggests that both PRP and steroid injections significantly improved the functional outcomes in terms of VAS score, DASH score, and PRTEE score. No other adverse events such as infection or tendon rupture were reported in both groups. Recurrences in both groups were managed by a repeat US-guided PRP injection by a senior orthopedic surgeon (PK) and most of them responded to the repeat PRP injection. The threshold was set at two injections. If treatment was not successful at 6 months of follow-up or if recurrence occurred again, magnetic resonance imaging (MRI) was done to look for the exact status of the tendon and surrounding soft tissue and to rule out other pathologies that also present with lateral elbow pain. There were 2 failures of treatment as per our pre-defined criteria. One was given a US-guided steroid, while the other was given US-guided PRP. The patient who had been given steroids had a diseased ECRB tendon on MRI and had relief with arthroscopic debridement surgery. The other patient who had been given a US-guided PRP injection had a chondral lesion in the radial head that was visualized on elbow arthroscopy and was not even visible on MRI. This would perhaps explain the absence of relief and can be incriminated as the cause of failure. The patient was managed with a microfracture technique and achieved relief.
Table 2. Comparison of VAS Scores between US-Guided PRP Group and US-Guided Steroid Group at Timely Intervals.
| VAS score | Group | p-value | |
|---|---|---|---|
| PRP (n = 32) | Steroid (n = 32) | ||
| Presentation | 7.75 ± 0.56 | 8.62 ± 0.49 | < 0.001* |
| 2 wk | 5.37 ± 1.33 | 3.62 ± 0.87 | < 0.001* |
| p-value | 0.104 | < 0.001† | |
| 1 mo | 3.50 ± 1.68 | 2.06 ± 0.84 | < 0.001* |
| p-value | 0.019† | < 0.001† | |
| 3 mo | 2.53 ± 1.16 | 2.06 ± 0.84 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
| 6 mo | 1.75 ± 0.71 | 3.28 ± 1.11 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
| 1 yr | 1.37 ± 0.70 | 3.59 ± 0.83 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
| 2 yr | 1.25 ± 0.62 | 3.68 ± 0.93 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
Values are presented as mean ± standard deviation.
VAS: visual analog scale, US: ultrasound, PRP: platelet-rich plasma.
Statistically significant: *Unpaired t-test. †Paired t-test.
Fig. 2. Schematic representation using a line graph showing the declining trend of visual analog scale (VAS) scores in the ultrasound-guided platelet-rich plasma (PRP) group and steroid group over 2 years.
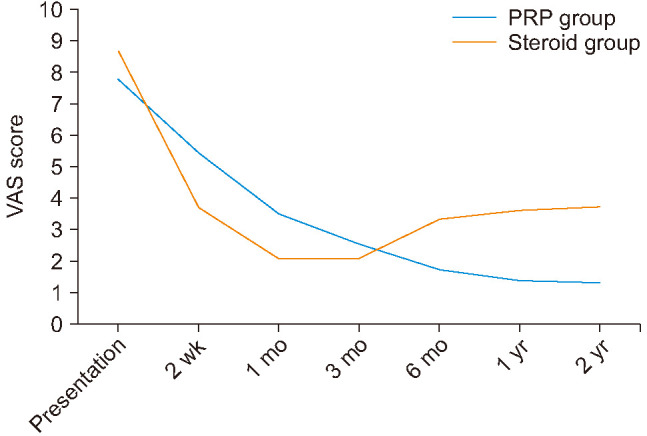
Table 3. Comparison of DASH Scores between US-Guided PRP Group and US-Guided Steroid Group at Timely Intervals.
| DASH score | Group | p-value | |
|---|---|---|---|
| PRP (n = 32) | Steroid (n = 32) | ||
| Presentation | 41.71 ± 10.15 | 43.65 ± 9.22 | 0.427 |
| 2 wk | 38.84 ± 8.44 | 29.50 ± 9.83 | < 0.001* |
| p-value | 0.828 | 0.297 | |
| 1 mo | 22.34 ± 7.25 | 19.31 ± 4.13 | 0.044* |
| p-value | 0.125 | 0.019† | |
| 3 mo | 11.00 ± 6.36 | 8.46 ± 2.32 | 0.039* |
| p-value | 0.012† | < 0.001† | |
| 6 mo | 6.59 ± 3.02 | 6.34 ± 2.32 | 0.712 |
| p-value | < 0.001† | < 0.001† | |
| 1 yr | 5.31 ± 1.80 | 7.4 ± 1.77 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
| 2 yr | 4.00 ± 1.50 | 7.43 ± 1.29 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
Values are presented as mean ± standard deviation.
DASH: disabilities of the arm, shoulder and hand, US: ultrasound, PRP: platelet-rich plasma.
Statistically significant: *Unpaired t-test. †Paired t-test.
Fig. 3. Schematic representation using a line graph showing the declining trend of disabilities of the arm, shoulder and hand (DASH) scores in the ultrasound-guided platelet-rich plasma (PRP) group and steroid group over 2 years, indicating improvement in the functional outcome.

Table 4. Comparison of PRTEE Scores between US-Guided PRP Group and US-Guided Steroid Group at Timely Intervals (n = 64).
| PRTEE | Group | p-value | |
|---|---|---|---|
| PRP (n = 32) | Steroid (n = 32) | ||
| Presentation | 43.40 ± 9.53 | 45.34 ± 10.09 | 0.433 |
| 2 wk | 39.50 ± 9.15 | 30.68 ± 10.18 | 0.001* |
| p-value | 0.768 | 0.310 | |
| 1 mo | 23.53 ± 7.19 | 19.5 ± 3.76 | 0.007* |
| p-value | 0.100 | 0.019† | |
| 3 mo | 10.81 ± 5.36 | 8.71 ± 2.41 | 0.048* |
| p-value | 0.005† | < 0.001† | |
| 6 mo | 6.87 ± 2.75 | 6.06 ± 2.07 | 0.188 |
| p-value | < 0.001† | < 0.001† | |
| 1 yr | 5.18 ± 1.71 | 7.25 ± 1.58 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
| 2 yr | 3.96 ± 1.51 | 7.53 ± 1.19 | < 0.001* |
| p-value | < 0.001† | < 0.001† | |
Values are presented as mean ± standard deviation.
PRTEE: Patient-Rated Tennis Elbow Evaluation, US: ultrasound, PRP: platelet-rich plasma.
Statistically significant: *Unpaired t-test. †Paired t-test.
Fig. 4. Schematic representation using a line graph showing the declining trend of Patient-Rated Tennis Elbow Evaluation (PRTEE) scores in the ultrasound-guided platelet-rich plasma (PRP) group and steroid group over 2 years, indicating improvement in the functional outcome. PRTEE score: validated patient outcome measure designed particularly for tennis elbow patients.

Table 5. Comparison of Handgrip Strength between US-Guided PRP Group and US-Guided Steroid Group at Timely Intervals (n = 64).
| Handgrip strength (kg force) | Group | p-value* | |
|---|---|---|---|
| PRP (n = 32) | Steroid (n = 32) | ||
| Presentation | 35.31 ± 15.50 | 33.03 ± 12.83 | 0.524 |
| 2 wk | 35.25 ± 15.55 | 33.03 ± 12.83 | 0.536 |
| p-value† | 0.997 | 1.000 | |
| 1 mo | 45.34 ± 16.85 | 44.18 ± 15.30 | 0.775 |
| p-value† | 0.662 | 0.685 | |
| 3 mo | 53.03 ± 17.51 | 51.87 ± 15.95 | 0.783 |
| p-value† | 0.451 | 0.459 | |
| 6 mo | 61.46 ± 72.38 | 59.06 ± 16.09 | 0.582 |
| p-value† | 0.725 | 0.291 | |
| 1 yr | 72.37 ± 20.23 | 69.25 ± 19.28 | 0.529 |
| p-value† | 0.150 | 0.175 | |
| 2 yr | 84.43 ± 22.46 | 76.71 ± 19.71 | 0.149 |
| p-value† | 0.076 | 0.103 | |
Values are presented as mean ± standard deviation.
US: ultrasound, PRP: platelet-rich plasma.
*Unpaired t-test. †Paired t-test.
Fig. 5. Schematic representation using a line graph showing improvement in hand grip strength in the ultrasound-guided platelet-rich plasma (PRP) group and steroid group over 2 years measured using a calibrated Jamar hydraulic handheld dynamometer.

DISCUSSION
The present prospective triple-blinded study was designed to compare the efficacy of concentrated autologous platelets to steroids in patients with LET. There was an improvement in the patients managed with PRP, as well as those managed with steroids in terms of VAS scores, DASH scores, and PRTEE scores. However, although the patients managed with steroid injections showed better functional outcomes in the initial short-term period of 3 months as compared to those managed with PRP injections, the latter group showed a sustained improvement in functional outcomes, which was significantly better as compared to that in the former group at the long-term follow-up of 2 years. As the duration of symptoms of LET ranges from 6 months to 24 months,4) we defined short-term follow-up as duration till 3 months after injection. A follow-up more than 1 year after injection was considered long term.
This study thus demonstrated the durability of the results of PRP injection over the long term in terms of better pain control and improvement in functional scores. This can be attributed to the biological healing of the diseased muscle fibers due to the release of various growth factors and alteration in the natural history of the disease. Although LET was historically considered an inflammatory condition, recent findings have suggested its etiology to be degenerative due to the lack of inflammatory cells in the histological samples of patients.5) Repetitive use of the tendon leads to stretching that eventually progresses to microtears when the tendon does not withstand the forces acting upon it. The microtears coalesce and increase in number leading to the next stage of the disease process, which is tendinosis. The patients classically present with disturbing elbow pain that is located around 1 to 2 cm distal to the lateral epicondyle with a normal elbow range of motion in the initial stages. The management of this condition includes an array of techniques including avoidance of activities that put a strain on the extensors, physical therapy, daily ice fomentation, counterforce braces, and anti-inflammatory medications. Patients not responding to these initial modalities are given injections of steroids, PRP, or autologous blood. Other less-described modalities of management include percutaneous radiofrequency thermal treatment, extracorporeal shockwave therapy, acupuncture, and botulinum toxin A injections.5) After exhausting all the above-mentioned options, surgery consisting of open and arthroscopic approaches is considered. Corticosteroids act by putting a halt to the ongoing inflammatory cascade and provide a sense of relief from pain. As they mainly improve outcomes in the short term, it is wise to restrict their use in cases requiring a faster rehabilitation such as a sportsman who is in his mid-season of tennis play. Potential complications associated with their use include fat atrophy and wasting of the muscles.
On the other hand, PRP aims to enhance tendon healing as it contains numerous growth factors that include platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), transforming growth factor β, insulin-like growth factor (IGF), and fibroblast growth factor.6) Gosens et al.7) conducted a trial involving 100 patients with LET who were managed with a steroid injection or PRP injection. VAS scores and DASH scores were evaluated at regular follow-up and the PRP group was treated more successfully than the steroid group. They determined that the scores returned to the baseline level at 2 years for the steroid group but showed an improvement in the PRP group. The present study reported similar findings, but we also used the PRTEE score for evaluation, since it has more specificity when LET is concerned. A study by Gautam et al.8) analyzing changes in the common extensor tendon on ultrasonographic evaluation after injection of PRP or corticosteroid in cases with tennis elbow concluded that PRP enhanced healing of the pathology, while corticosteroids led to the degeneration of the tendon, although they provided relief in the short term. Although the authors compared the outcomes using the VAS score, modified Mayo score, DASH score, Oxford Elbow score, and handgrip strength, the study had a limited sample size and involved administration of injections using the peppering technique and not with the aid of US.8) Although corticosteroids provide rapid relief from pain, they were shown to have negative effects on collagen and tendon cell viability in rotator cuff tears.9) This damage is usually evident in the long run and can be considered one of the reasons for the recurrence of the pathology. Another cause for the recurrence could be the immediate mobilization of the elbow after a quicker relief from pain.10) The way PRP acts in resolving the symptoms is not yet completely understood. It has been postulated that PRP improves the early healing of tendon defects by increasing the expression of IGF-1.11)
The tenocytes are also protected from the damaging effects of steroids by PRP.12) An increase in the concentration of growth factors in the local milieu including VEGF, PDGF, and IGF has been demonstrated following the injection of PRP. However, due to the process of regeneration and healing being slow and taking around 3 months or more, the benefits of PRP are not evident in the short term. Another disadvantage is the higher cost associated with the use of PRP. Ultrasonographic evaluation is routinely used for the detection of the pathology of tendons, including ruptures and calcifications. The use of US in our study helped in the localization of the pathology. Mishra et al.14) stated that US guidance should be included as a part of future investigations to enhance needle placement. A novel cadaveric study showed that the overall accuracy of blind injections for the treatment of LET is lower and the chances of delivering the drug to the intra-articular location are higher.15) Even though there are many studies comparing corticosteroid and PRP injections for LET, our study stood out in the sense that it utilized US localization before injection, which led to better delivery of the drug at the diseased site. The prospective nature of the study, triple-blinded design, and relatively long duration of follow-up were some of the highlights of our study. Table 6 highlights in brief the existing literature and compares our study with the previously published studies. Limitations of our study were the relatively small sample size and inability to include a control group as we did not receive approval for the same from the Ethics Committee.
Table 6. Comparison of the Methods and Conclusion of the Present Study with the Existing Literature.
| Study | Method | Use of ultrasonography | Year | Conclusion | Follow-up duration |
|---|---|---|---|---|---|
| Peerbooms et al.13) | Double-blinded | No | 2010 | PRP in chronic LET more significantly reduced pain and increased function than corticosteroid injection. | 1 yr |
| Gosens et al.7) | Double-blinded | No | 2011 | The effects of PRP in improving function exceeded the effects of steroids, even after a follow-up of 2 years. | 2 yr |
| Gautam et al.8) | Yes | 2015 | PRP healed the lesion biologically, while corticosteroids provided short-term relief at the cost of tendon degeneration. | 6 mo | |
| This study | Triple-blinded | Yes | 2022 | While corticosteroids were superior in the short term, PRP provided sustained relief in the long term and also played a part in biological healing. | 2 yr |
PRP: platelet-rich plasma, LET: lateral elbow tendinopathy.
US-guided steroids, as well as PRP injections, improved the functional outcome and hand grip strength in nonresponsive cases of LET. However, symptomatic relief in pain and overall improvement in the functional outcome as evident by various scores was swift in onset and lasted for a brief period in the steroid group, whereas patients injected with PRP demonstrated gradational and sustained improvement over long-term follow-up, suggesting a biological augmentation prospect of PRP in the pathophysiology of patients with LET.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Chaitanya Rane, MD, Seth GS Medical College and KEM Hospital, for performing the ultrasound scans of our patients.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Otoshi K, Takegami M, Sekiguchi M, et al. Chronic hyperglycemia increases the risk of lateral epicondylitis: the Locomotive Syndrome and Health Outcome in Aizu Cohort Study (LOHAS) Springerplus. 2015;4:407. doi: 10.1186/s40064-015-1204-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhurat R, Sukesh M. Principles and methods of preparation of platelet-rich plasma: a review and author’s perspective. J Cutan Aesthet Surg. 2014;7(4):189–197. doi: 10.4103/0974-2077.150734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manikandan S. Measures of central tendency: median and mode. J Pharmacol Pharmacother. 2011;2(3):214–215. doi: 10.4103/0976-500X.83300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johns N, Shridhar V. Lateral epicondylitis: current concepts. Aust J Gen Pract. 2020;49(11):707–709. doi: 10.31128/AJGP-07-20-5519. [DOI] [PubMed] [Google Scholar]
- 5.Vaquero-Picado A, Barco R, Antuna SA. Lateral epicondylitis of the elbow. EFORT Open Rev. 2017;1(11):391–397. doi: 10.1302/2058-5241.1.000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pavlovic V, Ciric M, Jovanovic V, Stojanovic P. Platelet rich plasma: a short overview of certain bioactive components. Open Med (Wars) 2016;11(1):242–247. doi: 10.1515/med-2016-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gosens T, Peerbooms JC, van Laar W, den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2011;39(6):1200–1208. doi: 10.1177/0363546510397173. [DOI] [PubMed] [Google Scholar]
- 8.Gautam VK, Verma S, Batra S, Bhatnagar N, Arora S. Platelet-rich plasma versus corticosteroid injection for recalcitrant lateral epicondylitis: clinical and ultrasonographic evaluation. J Orthop Surg (Hong Kong) 2015;23(1):1–5. doi: 10.1177/230949901502300101. [DOI] [PubMed] [Google Scholar]
- 9.Puzzitiello RN, Patel BH, Forlenza EM, et al. Adverse impact of corticosteroids on rotator cuff tendon health and repair: a systematic review of basic science studies. Arthrosc Sports Med Rehabil. 2020;2(2):e161–e169. doi: 10.1016/j.asmr.2020.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borkholder CD, Hill VA, Fess EE. The efficacy of splinting for lateral epicondylitis: a systematic review. J Hand Ther. 2004;17(2):181–199. doi: 10.1197/j.jht.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Dhillon RS, Schwarz EM, Maloney MD. Platelet-rich plasma therapy: future or trend? Arthritis Res Ther. 2012;14(4):219. doi: 10.1186/ar3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zargar Baboldashti N, Poulsen RC, Franklin SL, Thompson MS, Hulley PA. Platelet-rich plasma protects tenocytes from adverse side effects of dexamethasone and ciprofloxacin. Am J Sports Med. 2011;39(9):1929–1935. doi: 10.1177/0363546511407283. [DOI] [PubMed] [Google Scholar]
- 13.Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38(2):255–262. doi: 10.1177/0363546509355445. [DOI] [PubMed] [Google Scholar]
- 14.Mishra AK, Skrepnik NV, Edwards SG, et al. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med. 2014;42(2):463–471. doi: 10.1177/0363546513494359. [DOI] [PubMed] [Google Scholar]
- 15.Keijsers R, van den Bekerom MP, Koenraadt KL, et al. Injection of tennis elbow: hit and miss? A cadaveric study of injection accuracy. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2289–2292. doi: 10.1007/s00167-016-4212-0. [DOI] [PubMed] [Google Scholar]



