Abstract
Background
In 2018, Femoral Neck System (FNS), a dedicated fixator for femoral neck fractures, was introduced. This device has been in increasing use because it provides excellent rotational and angular stability. However, the shortest bolt of FNS is 75 mm long. Thus, it is not usable when the axial length of the proximal femur (ALPF), the distance between the innominate tubercle and the surface of the femoral head, is less than 80 mm. In this study, we investigated the incidence and associated factors of small ALPF (< 80 mm) in femoral neck fracture patients.
Methods
We measured the ALPF on preoperative computed tomography (CT) scans of 261 patients (166 women and 55 men), who were operated due to nondisplaced or impacted femoral neck fractures. The ALPF was measured on reconstructed oblique coronal images along the femoral neck. We evaluated the distribution of ALPF, calculated the incidence of small ALPF (< 80 mm), and correlated it with patient’s height, weight, body mass index, age, bone mineral density (T-score), and caput-column-diaphysis angle.
Results
The ALPF ranged from 67.4 mm to 107.1 mm (mean, 88.4 mm; standard deviation, 7.2 mm). In 19 patients (8.6%, 19 / 221), the length was < 80 mm. The ALPF was strongly correlated with height (correlation coefficient = 0.707, R2 = 0.500, p < 0.001) and moderately correlated with weight (correlation coefficient = 0.551, R2 = 0.304, p < 0.001). The T-score was moderately correlated with the ALPF (correlation coefficient = 0.433, R2 = 0.187, p < 0.001). The age was moderately correlated with the ALPF (correlation coefficient =–0.353, R2 = 0.123, p < 0.001).
Conclusions
A considerable percentage of femoral neck fracture patients (8.6%) had small proximal femurs (ALPF < 80 mm), which cannot be operated with FNS. We recommend measuring the ALPF using reconstructed oblique coronal CT images or scaled hip radiographs: en face view of the femoral neck prior to surgery in patients with short stature and/or low body weight. If the ALPF is < 80 mm, the surgeon should prepare other fixation devices.
Keywords: Femoral neck fracture, Valgus impacted, Femoral neck system, FNS
Nondisplaced or impacted femoral neck fractures are usually treated with internal fixation.1,2,3,4,5) Traditionally, multiple pinning and sliding hip screws have been used for the fixation.6,7) In 2018, Femoral Neck System (FNS; DePuy Synthes, Zuchwil, Switzerland), a dedicated fixation modality for femoral neck fractures, was introduced. Biomechanical studies have shown that this device can provide excellent angular and rotational stability.8,9) It is expected to reduce the rate of fixation failure and thus its use is currently increasing as an alternative to conventional fixation devices. In 2019, we started to use FNS for femoral neck fractures and experienced cases that could not be operated with this device because the proximal femur was too small.
The aims of this study were to assess the prevalence of small proximal femurs, which cannot be operated with FNS and investigate associated factors of the small proximal femur in patients who had nondisplaced or valgus-impacted femoral neck fractures.
METHODS
Ethical Approval
The design and protocol of this retrospective study were approved by the Institutional Review Board of Seoul National University Bundang Hospital (No. B-2102-667-113). As a retrospective study, informed consent was waived. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Patient Selection and Demographics
We reviewed electronic medical records, radiographs, and computed tomography (CT) scans of 261 patients, who underwent internal fixation due to femoral neck fractures at our institution from July 2003 to June 2019. We excluded 19 patients who did not have preoperative CT scans and 21 patients with Garden type III/IV displaced femoral neck fractures. The remaining 221 patients were the participants of this study.
There were 166 women and 55 men with a mean age of 68.5 years (standard deviation [SD], ± 15.8) at the time of surgery. The mean height was 159.2 cm (SD, ± 9.0), the mean weight was 54.8 kg (SD, ± 11.4), and the mean body mass index was 21.5 kg/m2 (SD, ± 3.5). According to the Garden classification, there were 204 type I fractures with valgus impaction and 17 undisplaced type II fractures. According to the Pauwels’ classification of the fracture angulation, there were 17 type I (< 30°) fractures, 167 type II (30°–50°) fractures, and 37 type III (> 50°) fractures. All of the 221 patients underwent bone mineral densitometry and their mean T-score was –2.5 (SD, ± 1.1) (Table 1).
Table 1. Demographics of 221 Patients with Femoral Neck Fractures.
| Variable | Value | |
|---|---|---|
| Male : female | 55 (24.9) : 166 (75.1) | |
| Age (yr) | 68.5 ± 15.8 | |
| Height (cm) | 159.2 ± 9.0 | |
| Weight (kg) | 54.8 ± 11.4 | |
| Body mass index (kg/m2) | 21.5 ± 3.5 | |
| DXA (T-score) | –2.5 ± 1.1 | |
| CCD angle (°) | 135.3 ± 4.7 | |
| Garden classification | ||
| Type I (with valgus impaction) | 204 | |
| Type II (undisplaced) | 17 | |
| Pauwels’ classification | ||
| Type I (< 30°) | 17 | |
| Type II (30°–50°) | 167 | |
| Type III (> 50°) | 37 | |
Values are presented as number (%) or mean ± standard deviation.
DXA: dual-energy X-ray absorption, CCD: caput-column-diaphysis.
Instrument Information and Indications for FNS
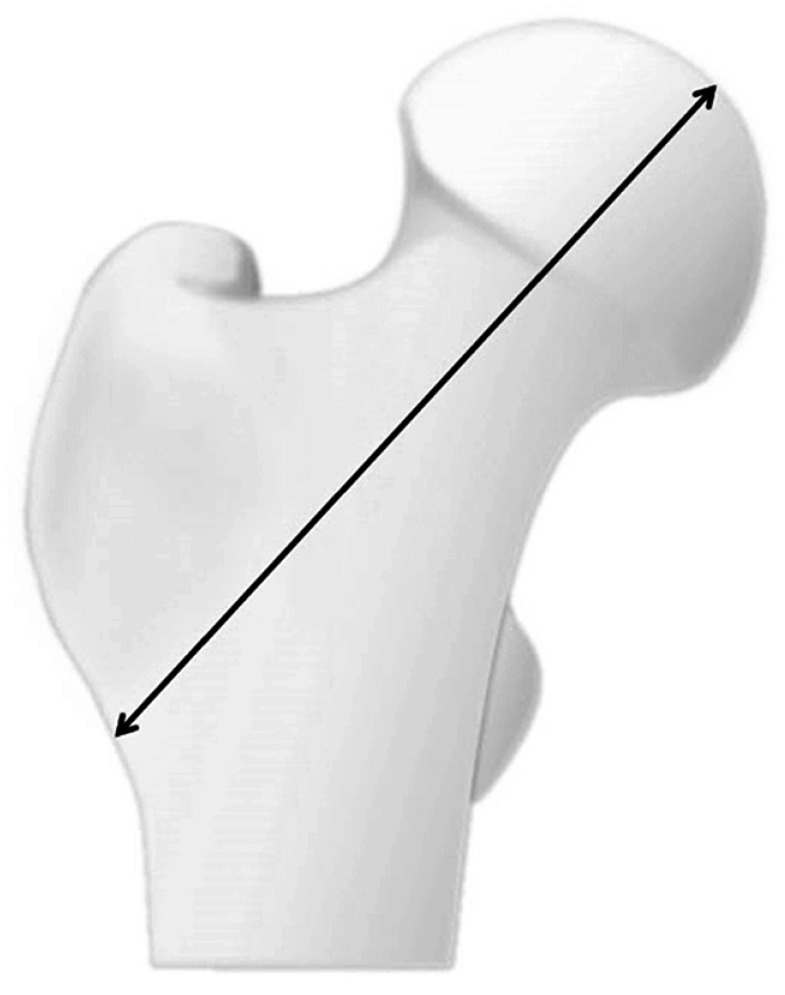
The FNS consists of three parts: barrel plate, bolt, and anti-rotational screw. Barrel plate has 130° caput-column-diaphysis (CCD) angle (Fig. 1). The length of bolt and anti-rotational screw ranges from 75 mm to 130 mm in 5-mm increments. The length of the bolt should be shorter than the measured depth of the central guide wire, which is inserted into the subchondral bone of the femoral head, by more than 5 mm to avoid cut-through of the bolt outside the femoral head. To use a 75-mm bolt, the axial length of the proximal femur (ALPF), which refers to the distance between the lateral cortex below the innominate tubercle of the greater trochanter and the surface of the femoral head along the femoral neck axis (Fig. 2), should exceed 80 mm. Therefore, when the ALPF is less than 80 mm, the femoral neck fracture cannot be fixed with FNS.
Fig. 1. Femoral Neck System (DePuy Synthes, Zuchwil, Switzerland) consisting of three parts: barrel plate, bolt, and anti-rotational screw. The barrel plate has 130° caput-column-diaphysis (CCD) angle.

Fig. 2. The axial length of the proximal femur is the distance between the lateral cortex below the innominate tubercle of the greater trochanter and the surface of the femoral head along the femoral neck axis.
CT Measurement of the ALPF
The preoperative CT scans were taken with a 16-slice CT scanner (Mx8000 IDT; Philips, Eindhoven, the Netherlands). Two orthopedic surgeons (JWP and HSK) measured the ALPF of the fractured femurs. The measurements were done on reconstructed CT images using 4.5 version of Extended Brilliance Workstation.
The axial image, which best showed the femoral neck in the greatest length, was selected. On this image, the axis of the femoral neck was defined as the line connecting the center of the femoral neck and that of the femoral head (Fig. 3A). From the reconstructed three-dimensional image of the proximal femur, an oblique coronal image along the femoral neck axis was reformatted (Fig. 3B).10) On the oblique coronal image, the axis of the proximal femur, which was 130° to the lateral cortex of the proximal femur and passed the center of the femoral neck base, was defined. Then, the distance between the two points on the axis, one below the innominate tubercle and one on the surface of the femoral head, was measured (Fig. 3C).
Fig. 3. (A) The axial image, which best shows the femoral neck in the greatest length, was selected. On this image, the axis of the femoral neck was defined as the line connecting the center of the femoral neck and that of the femoral head. (B) Oblique coronal image along the femoral neck axis was reformatted using 4.5 version of Extended Brilliance Workstation (Philips, Cleveland, OH, USA). (C) On the oblique coronal image, the axis of the proximal femur, which was 130° to the lateral cortex of the proximal femur and passed the center of the femoral neck base, was defined. Then, the distance between the two points on the axis, one below the innominate tubercle and one on the surface of the femoral head, was measured.
CT Measurement of the CCD Angle
On the oblique coronal CT image, CCD angle of the fractured femoral neck was measured. The CCD angle was defined as the angle between the line connecting the center of the angulated femoral head and the center of the femur neck base and the axis of the proximal diaphysis (Fig. 4). One evaluator who was blinded to the first measurement (JKK) repeated the measurement at least 1 week later, and two evaluators (JWP and HSK) independently measured the APFLs of 20 randomly selected patients. To investigate the reliability of radiologic measurement, the intraclass correlation coefficient (ICC) was used.11) The ICCs exceeding 0.8 are considered excellent for a 95% confidence interval. Both inter- and intraobserver reliabilities were excellent (ICC: 0.921–0.967 and 0.814–0.896, respectively).
Fig. 4. The Caput-column-diaphysis angle of the fractured femoral neck was defined as the angle (a) between the line connecting the center of the angulated femoral head and the center of the femur neck base and the axis of the proximal diaphysis.

Statistical Method
The correlations between the APFL and the height, weight, and body mass index were tested by Pearson correlation coefficient. A p-value < 0.05 was considered statistically significant. Statistical analysis was performed using IBM SPSS ver. 25 (IBM Corp.).
RESULTS
The ALPF ranged from 67.4 mm to 107.1 mm (mean ± SD, 88.4 ± 7.2 mm). Nineteen patients (7.2%, 19 / 221) had ALPF < 80 mm (Fig. 5). The mean ALPF was 86.2 mm (SD, ± 5.9) in women and 95.3 mm (SD, ± 6.4) in men (p < 0.001). The ALPF was strongly correlated with height (correlation coefficient = 0.707, R2 = 0.500, p < 0.001) (Fig. 6), moderately correlated with weight (correlation coefficient = 0.551, R2 = 0.304, p < 0.001) (Fig. 7), and weakly correlated with body mass index (correlation coefficient = 0.192, R2 = 0.037, p = 0.004).
Fig. 5. Histogram of axial length of the proximal femur.
Fig. 6. Scatter plot of patient’s height and axial length of the proximal femur.
Fig. 7. Scatter plot of patient’s weight and axial length of the proximal femur.
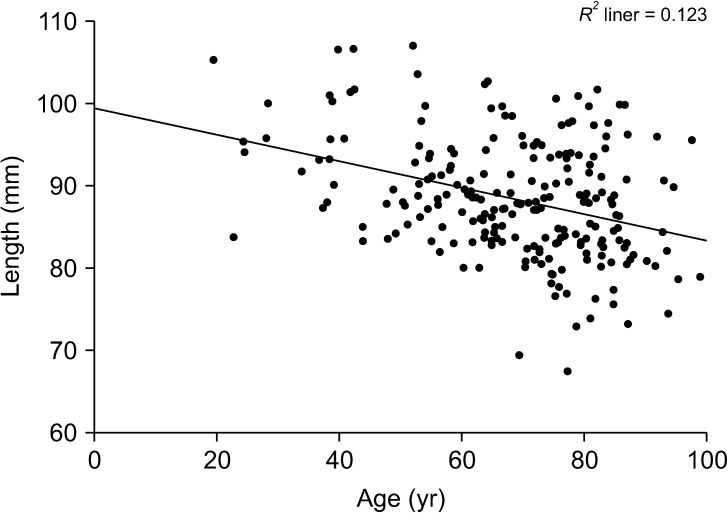
The CCD angle ranged from 116.91° to 142.67° (mean ± SD, 135.3° ± 4.7°). There was no significant correlation between the ALPF and CCD angle (p = 0.171). The T-score (correlation coefficient = 0.433, R2 = 0.187, p < 0.001) (Fig. 8) and age (correlation coefficient = –0.353, R2 = 0.123, p < 0.001) (Fig. 9) moderately correlated with the ALPF. There were significant differences in height (149.1 ± 6.4 cm vs. 160.1 ± 8.6 cm, p < 0.001), weight (45.8 ± 8.3 kg vs. 55.7 ± 11.3 kg, p < 0.001), age (80.1 ± 9.3 years vs. 67.4 ± 15.8 years, p < 0.001), and T-score (–3.4 ± 1.1 vs. –2.4 ± 1.0, p < 0.001) between 19 patients with ALPF < 80 and 202 patients with ALPF > 80 mm.
Fig. 8. Scatter plot of patient’s T-score and axial length of the proximal femur.
Fig. 9. Scatter plot of patient’s age and axial length of the proximal femur.
DISCUSSION
In our measurement of the ALPF in patients with valgus-impacted or nondisplaced femoral neck fractures using three-dimensional CT scans, the ALPF was shorter than 80 mm in 8.6% (19 / 221). In these patients, the FNS could not be used for the fixation. The ALPF of our patients was shorter than that reported in studies from Western countries. It is difficult to exactly measure the ALPF on radiographs because radiographs have inconsistent magnifications, and the position of the proximal femur is uncontrolled. Thus, only a few studies reported the geometry of the proximal femur of hip fracture patients. One study from the United States measured the ALPF of 22 Caucasian women, who had sustained a hip fracture after the age of 58 years. In that study, the mean ALPF was 116.3 mm (SD, ± 4.1).12) In another study from Sweden involving 125 hip fracture patients, among 92 women with a mean age of 78 years (SD, ± 9) and 33 men with a mean age 76 years (SD, ± 10), the ALPF was 124.2 mm (SD, ± 18.7).13) The discrepancy of the ALPF between our study and studies from Western countries might be explained by two factors: ethnic difference and the measurement method. Nakamura et al.14) compared 57 Japanese women and 119 Caucasian women in the United States, who were aged 50–79 years. In their study, the length of the femoral neck was shorter (4.4 cm vs. 5.6 cm, p < 0.0001) and the femoral neck-shaft angle was smaller (128° vs. 130°, p < 0.01) in Japanese women. We used three-dimensional CT scan and elaborate software program, which enabled us to measure the actual length of the proximal femoral axis, while the length was measured on simple radiographs in previous studies.
In valgus-impacted femoral neck fractures, the length of the femoral neck is shortened as much as the impacted portion at the fracture site. When the valgus-impaction is reduced, the original length of the femoral neck length can be restored.15,16) One study reported that the reduction also enhanced the stability of the fixation compared to in situ fixation.17) However, other studies recommended in situ fixation in the elderly osteoporotic patients because the reduction might lead to a fixation failure.18,19)
In our study, 19 patients with valgus-impacted fractures could not be operated with the FNS because ALPF was shorter than 80 mm. We measured the ALPF of the contralateral uninjured femurs in 16 of 19 patients. While the ALPF of the contralateral femur was < 80 mm in 4 patients, it was > 80 mm in the remaining 12 patients. If the valgus-impaction had been reduced, these 12 patients could have been operated with FNS.
We note limitations of this study. First, it was done in South Korea. In our patients, the mean height was 159.2 cm (SD, ± 9.0), the mean weight was 54.8 kg (SD, ± 1.4), and the mean body mass index was 21.5 kg/m2 (SD, ± 3.5). Our results might not be generalized in Caucasians and other ethnicities. Second, we used three-dimensional CT scans and an elaborate software program for the measurement. The CT scan is costly and the measurement using the software program is a time-consuming procedure. Third, the posttraumatic femoral neck deformities, coxa valga (CCD angle > 135°), and coxa vara (CCD angle < 120°), might have affected the ALPF. In our study, 135 patents had coxa valga deformity, and only 1 had coxa vara deformity. Due to the paucity of coxa vara deformity, we could not perform statistical analysis to correlate the neck deformities and the ALPF. Forth, we did not evaluate the relationship between the magnitude of impaction and the ALPF. To exactly measure the magnitude of femoral neck impaction, radiographs before the trauma is necessary. However, these radiographs were unavailable and we could not measure the impaction magnitude. Nevertheless, there have been no studies that measured the actual length of the proximal femoral axis using reconstructed oblique coronal image of CT scan.
The FNS is a useful device to treat femoral neck fractures and has several merits. It affords a better angular stability compared to conventional cannulated screw fixation and has little lateral protrusion.8,20) However, some patients have an ALPF < 80 mm, and they cannot be operated with this device. In patients with short stature and/or low weight, the ALPF should be measured before surgery using CT scan or scaled radiographs. If an ALPF is < 80 mm, the surgeon should prepare other device to fix the femoral neck fracture.
ACKNOWLEDGEMENTS
This study was supported by AO Trauma Asia Pacific Research grants 2021 (AOTAP21-12).
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377(21):2053–2062. doi: 10.1056/NEJMcp1611090. [DOI] [PubMed] [Google Scholar]
- 2.Bhandari M, Devereaux PJ, Tornetta P, 3rd, et al. Operative management of displaced femoral neck fractures in elderly patients: an international survey. J Bone Joint Surg Am. 2005;87(9):2122–2130. doi: 10.2106/JBJS.E.00535. [DOI] [PubMed] [Google Scholar]
- 3.Shah AK, Eissler J, Radomisli T. Algorithms for the treatment of femoral neck fractures. Clin Orthop Relat Res. 2002;(399):28–34. doi: 10.1097/00003086-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Su EP, Su SL. Femoral neck fractures: a changing paradigm. Bone Joint J. 2014;96(11 Supple A):43–47. doi: 10.1302/0301-620X.96B11.34334. [DOI] [PubMed] [Google Scholar]
- 5.Zielinski SM, Meeuwis MA, Heetveld MJ, et al. Adherence to a femoral neck fracture treatment guideline. Int Orthop. 2013;37(7):1327–1334. doi: 10.1007/s00264-013-1888-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang LL, Zhang Y, Ma X, Liu Y. Multiple cannulated screws vs. dynamic hip screws for femoral neck fractures: a meta-analysis. Orthopade. 2017;46(11):954–962. doi: 10.1007/s00132-017-3473-8. [DOI] [PubMed] [Google Scholar]
- 7.Slobogean GP, Sprague SA, Scott T, McKee M, Bhandari M. Management of young femoral neck fractures: is there a consensus? Injury. 2015;46(3):435–440. doi: 10.1016/j.injury.2014.11.028. [DOI] [PubMed] [Google Scholar]
- 8.Stoffel K, Zderic I, Gras F, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131–137. doi: 10.1097/BOT.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 9.Schopper C, Zderic I, Menze J, et al. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Translat. 2020;24:88–95. doi: 10.1016/j.jot.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jarrett DY, Oliveira AM, Zou KH, Snyder BD, Kleinman PK. Axial oblique CT to assess femoral anteversion. AJR Am J Roentgenol. 2010;194(5):1230–1233. doi: 10.2214/AJR.09.3702. [DOI] [PubMed] [Google Scholar]
- 11.Kottner J, Audige L, Brorson S, et al. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64(1):96–106. doi: 10.1016/j.jclinepi.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Peacock M, Turner CH, Liu G, Manatunga AK, Timmerman L, Johnston CC., Jr Better discrimination of hip fracture using bone density, geometry and architecture. Osteoporos Int. 1995;5(3):167–173. doi: 10.1007/BF02106096. [DOI] [PubMed] [Google Scholar]
- 13.Karlsson KM, Sernbo I, Obrant KJ, Redlund-Johnell I, Johnell O. Femoral neck geometry and radiographic signs of osteoporosis as predictors of hip fracture. Bone. 1996;18(4):327–330. doi: 10.1016/8756-3282(96)00004-x. [DOI] [PubMed] [Google Scholar]
- 14.Nakamura T, Turner CH, Yoshikawa T, et al. Do variations in hip geometry explain differences in hip fracture risk between Japanese and white Americans? J Bone Miner Res. 1994;9(7):1071–1076. doi: 10.1002/jbmr.5650090715. [DOI] [PubMed] [Google Scholar]
- 15.Yoon BH, Kim YS, Koo KH. A simple percutaneous technique to reduce valgus-impacted femoral neck fractures. Clin Orthop Surg. 2020;12(2):258–262. doi: 10.4055/cios19156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noda M, Takahashi M, Nukuto K, et al. Innovative technique of minimally invasive closed reduction for impacted femoral neck fractures (MICRIF) J Orthop Surg (Hong Kong) 2019;27(1):2309499019832418. doi: 10.1177/2309499019832418. [DOI] [PubMed] [Google Scholar]
- 17.Park YC, Um KS, Kim DJ, Byun J, Yang KH. Comparison of femoral neck shortening and outcomes between in situ fixation and fixation after reduction for severe valgus-impacted femoral neck fractures. Injury. 2021;52(3):569–574. doi: 10.1016/j.injury.2020.10.028. [DOI] [PubMed] [Google Scholar]
- 18.Probe R, Ward R. Internal fixation of femoral neck fractures. J Am Acad Orthop Surg. 2006;14(9):565–571. doi: 10.5435/00124635-200609000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Otremski I, Katz A, Dekel S, Salama R, Newman RJ. Natural history of impacted subcapital femoral fractures and its relevance to treatment options. Injury. 1990;21(6):379–381. doi: 10.1016/0020-1383(90)90124-d. [DOI] [PubMed] [Google Scholar]
- 20.Stiasny J, Dragan S, Kulej M, Martynkiewicz J, Plochowski J, Dragan SL. Comparison analysis of the operative treatment results of the femoral neck fractures using side-plate and compression screw and cannulated AO screws. Ortop Traumatol Rehabil. 2008;10(4):350–361. [PubMed] [Google Scholar]