Abstract
Objective
To compare risks of cardiovascular outcomes between patients with type 2 diabetes and patients with established coronary heart disease.
Design
Cross sectional study and cohort study using routinely collected datasets.
Setting
Tayside, Scotland (population 400 000) during 1988-95.
Subjects
In the cross sectional study, among patients aged 45-64, 1155 with type 2 diabetes were compared with 1347 who had had a myocardial infarction in the preceding 8 years. In the cohort study 3477 patients of all ages with newly diagnosed type 2 diabetes were compared with 7414 patients who had just had a myocardial infarction.
Main outcome measures
Risk ratios for death from all causes, cardiovascular death, and hospital admission for myocardial infarction were calculated by Cox proportional hazards analysis and adjusted for age and sex.
Results
In the cross sectional study the adjusted risk ratio for death from all causes was 2.27 (95% confidence interval 1.82 to 2.83) for patients who had had myocardial infarction compared with those with diabetes, and the risk ratio for hospital admission for myocardial infarction was 1.33 (1.14 to 1.55). In the cohort study, patients who had just had a myocardial infarction had a higher risk of death from all causes (adjusted risk ratio 1.35 (1.25 to 1.44)), cardiovascular death (2.93 (2.54 to 3.41)), and hospital admission for myocardial infarction (3.10 (2.57 to 3.73)).
Conclusions
Patients with type 2 diabetes were at lower risk of cardiovascular outcomes than patients with established coronary heart disease.
What is already known on this topic
A recent influential study suggested that patients with type 2 diabetes without established cardiovascular disease have as high a risk of cardiovascular events and death as non-diabetic patients who have had a myocardial infarction
Some clinicians therefore advocate aggressive treatment of cardiovascular risk factors in the presence of diabetes
What this study adds
Patients with type 2 diabetes are at lower risk of death from all causes or cardiovascular causes and of hospital admission for myocardial infarction than patients with established coronary heart disease
Introduction
The increased risk of cardiovascular disease in type 2 diabetes is well recognised1 and is associated with both diabetes specific risk factors2 and increased frequency of conventional risk factors for cardiovascular disease.3 A recent study by Haffner et al suggested that the risk of death from coronary heart disease in patients with type 2 diabetes may even be as high as in patients who have had a myocardial infarction.4 This observational study in Finland examined the seven year incidence of cardiovascular events among 890 patients with diabetes who had no history of myocardial infarction and 69 patients without diabetes who had previously had a myocardial infarction. The risk of death from coronary heart disease was not significantly different between the two groups, with an adjusted hazard ratio of 1.2 (95% confidence interval 0.6 to 2.4).
The authors of this study proposed that patients with diabetes should be treated as if they had existing coronary heart disease. The role of primary prevention of coronary heart disease in patients with diabetes has since come under much scrutiny, with some diabetologists advocating aggressive treatment of cardiovascular risk factors. The National Cholesterol Education Program and the American Diabetes Association have recommended lower goals for low density lipoprotein cholesterol both in patients with coronary heart disease and in those with diabetes.5 However, others argue that treatment decisions should not be based on individual risk factors in isolation.6
An important weakness of Haffner et al's study was the lack of power to detect differences between the two groups. Other larger studies have found a high risk of cardiovascular disease for patients with diabetes, but one lower than that for patients with coronary heart disease.7 Haffner et al's patients were also a self selected group in that they represented the 80% of eligible subjects who attended a clinic visit for the study.
The aim of the present investigation was to compare risks of cardiovascular outcomes between patients with diabetes and patients with established coronary heart disease. We carried out two studies: in the first we used a design similar to that of Haffner et al,4 and in the second we compared patients with newly diagnosed diabetes for cardiovascular risk with those who had just had a myocardial infarction.
Subjects and methods
Data sources
We carried out the work with the DARTS/MEMO Collaboration using routine data sources for the population of Tayside, Scotland, which can be record linked using a unique patient identifier.8,9 These include a register of all patients with type 1 and type 2 diabetes in Tayside from 1988 (which has been validated and shown to have high sensitivity and specificity for the diagnosis of diabetes9), a record of all inpatient hospital admissions in Tayside from 1980 with diagnostic codes from ICD-9 (international classification of diseases, ninth revision), and records of death certificates from the registrar general with ICD-9 coded causes of death from 1988. The study population comprised patients who were alive and resident in Tayside in January 1987 and who were either still alive in Tayside at the end of the study or who had died (thus excluding emigrants from Tayside).
Cross sectional study
We identified a cross section of patients aged 45-64 years at the study index date (1 January 1988). This was the age range used by Haffner et al.4 We defined a diabetic group, which included all patients with type 2 diabetes diagnosed before the index date. Any patient for whom a diagnosis of type 1 diabetes was not made (that is, diagnosed at <35 years old and requiring insulin treatment) was judged to have type 2 diabetes. We also defined a group of patients who had had a myocardial infarction: all patients aged 45-64 who had an inpatient hospital admission with myocardial infarction (ICD-9 code 410.9) between January 1980 and December 1987. We excluded any patient who was in both groups. Follow up was from January 1988 to December 1995.
The outcomes were mortality (any cause), ascertained from death certification records, and hospital admission with a primary diagnosis of myocardial infarction (ICD-9 410.9). We used a Cox proportional hazards model to calculate risk ratios (with 95% confidence intervals), adjusted for age and sex, for the risks of the outcomes in the myocardial infarction group compared with those in the diabetic group.
Cohort study
We identified two cohorts of patients. The diabetic cohort included any patient in the study population with type 2 diabetes diagnosed between January 1988 and December 1995. Their study index date was their date of diagnosis of diabetes. The myocardial infarction cohort included any patient who had a first hospital admission with a primary or secondary diagnosis of myocardial infarction (ICD-9 410.9) between January 1988 and December 1995. Their study index date was their date of hospital admission. Any patient in either cohort who had a hospital admission for myocardial infarction between January 1980 and December 1987 was excluded from the study, as were patients with type 2 diabetes diagnosed on the same day as their first myocardial infarction.
The outcomes in this study during follow up to December 1995 were mortality (any cause), cardiovascular mortality (with the underlying cause of death recorded on the death certificate coded as a cardiovascular death), and hospital admission for myocardial infarction (any hospital admission with a primary or secondary diagnosis code of 410.9). Any patient who died within 28 days after their index date was excluded from further analyses. This was to eliminate deaths that were due directly to the myocardial infarction. We constructed Kaplan-Meier survival curves to compare probability of death between the study cohorts. We used a Cox proportional hazards model to compare the risks, with adjustment for age and sex.
Results
Our study population consisted of 263 175 patients.
Cross sectional study
We identified 1155 patients (42% women) with diabetes, with a mean age of 57 years and a mean duration of diabetes of 6.04 years. We identified 1347 patients (28% women) with myocardial infarction, with a mean age of 57 and a mean time since infarction of 3.5 years.
In the eight year follow up 438 (32.5%) of the patients in the myocardial infarction group died, and 274 (20.3%) were hospitalised for a further infarction. In the diabetic group 284 (24.6%) died, and 113 (9.8%) were hospitalised for an infarction. The adjusted risk ratio for mortality in the myocardial infarction group compared with the diabetic group was 1.33 (95% confidence interval 1.14 to 1.55), while that for hospital admission for myocardial infarction was 2.27 (1.82 to 2.83) (table 1). The risks of these outcomes seemed to be greater for men than women, and the risks increased with age (although age was a weaker predictor of hospital admission for myocardial infarction than of death).
Table 1.
Risk of death from all causes and hospital admission for myocardial infarction in cross sectional study of patients with type 2 diabetes and those who had had a myocardial infarction
|
Diabetic group
|
MI group
|
Risk ratio (95% CI)* | ||||
|---|---|---|---|---|---|---|
| No of patients | No of events | No of patients | No of events | |||
| Death from all causes | ||||||
| Age (years): | ||||||
| 45-49 | 102 | 8 | 106 | 23 | 0.34 (0.24 to 0.49) | |
| 50-54 | 260 | 39 | 237 | 60 | 0.48 (0.38 to 0.59) | |
| 55-59 | 299 | 68 | 366 | 100 | 0.61 (0.51 to 0.73) | |
| 60-64 | 494 | 169 | 638 | 255 | 1.00 | |
| Sex: | ||||||
| Men | 668 | 182 | 974 | 334 | 1.35 (1.15 to 1.61) | |
| Women | 487 | 102 | 373 | 104 | 1.00 | |
| Diagnosis: | ||||||
| MI | — | — | 1347 | 438 | 1.33 (1.14 to 1.55) | |
| Diabetes | 1155 | 284 | — | — | 1.00 | |
| Hospital admission for myocardial infarction | ||||||
| Age (years): | ||||||
| 45-49 | 102 | 5 | 106 | 22 | 0.71 (0.47 to 1.06) | |
| 50-54 | 260 | 19 | 237 | 50 | 0.81 (0.61 to 1.06) | |
| 55-59 | 299 | 27 | 366 | 75 | 0.85 (0.67 to 1.08) | |
| 60-64 | 497 | 62 | 638 | 127 | 1.00 | |
| Sex: | ||||||
| Men | 668 | 71 | 974 | 208 | 1.28 (1.03 to 1.61) | |
| Women | 487 | 42 | 373 | 66 | 1.00 | |
| Diagnosis: | ||||||
| MI | — | — | 1347 | 274 | 2.27 (1.82 to 2.83) | |
| Diabetes | 1155 | 113 | — | — | 1.00 | |
MI=myocardial infarction.
Adjusted for all covariates, derived from Cox regression analysis.
Cohort study
For the diabetic cohort, we identified 3477 patients (49% women), with a mean age of 66, of whom 3403 (98%) were included in the statistical analyses (patients who did not die within 28 days after their index date). For the myocardial infarction cohort, we identified 7414 patients (46% women), with a mean age of 71, of whom 5350 (72%) were included in the statistical analyses.
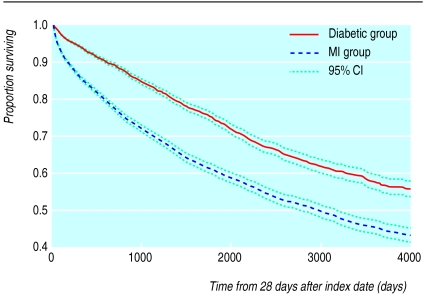
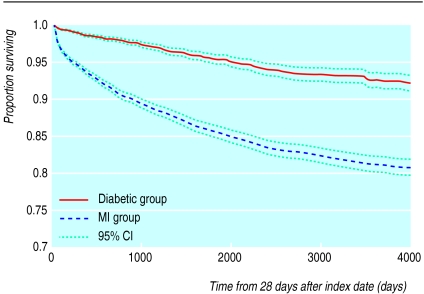
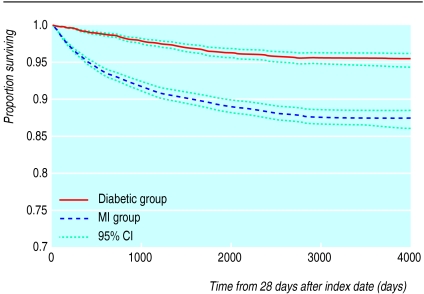
During the subsequent follow up, there were 1196 deaths in the diabetic cohort (35.1% of the patients in the analyses), of which 222 were cardiovascular deaths, and 142 patients were hospitalised for myocardial infarction. In the myocardial infarction cohort there were 2596 deaths (48.8% of patients in the analyses), of which 1077 were cardiovascular deaths, and 656 patients were hospitalised for myocardial infarction. The Kaplan-Meier survival curves show that the diabetic cohort had lower risks for death from all causes (fig 1), cardiovascular deaths (fig 2), and hospitalisation for myocardial infarction (fig 3). The reduced risk seemed to be mainly in the early period of follow up, with the gradients of the curves converging after the first 1000 days or so.
Figure 1.
Kaplan-Meier survival curve showing time to death from any cause in patients with newly diagnosed type 2 diabetes and patients who had just had a myocardial infarction (MI)
Figure 2.
Kaplan-Meier survival curve showing time to death from cardiovascular causes in patients with newly diagnosed type 2 diabetes and patients who had just had a myocardial infarction (MI)
Figure 3.
Kaplan-Meier survival curve showing time to hospital admission for myocardial infarction in patients with newly diagnosed type 2 diabetes and patients who had just had a myocardial infarction (MI)
Table 2 indicates that patients in the myocardial infarction cohort had an increased risk of death from any cause compared with patients in the diabetic cohort, with an adjusted risk ratio of 1.35 (95% confidence interval 1.25 to 1.44). The risk increased with age, and men were at greater risk than women (adjusted risk ratio 1.19 (1.12 to 1.26)). Patients in the myocardial infarction cohort had a threefold higher risk of death from a cardiovascular cause than patients in the diabetic cohort (adjusted risk ratio 2.93 (2.54 to 3.41)), and the risk of cardiovascular death increased with age, but there was no difference between men and women. The myocardial infarction cohort also had an increased risk of hospital admission for myocardial infarction (adjusted risk ratio 3.10 (2.57 to 3.73)). The risks of hospital admission were higher in the age groups 60-69 and 70-79 than in the group aged ⩾80, but there was no difference between men and women.
Table 2.
Risk of death from all causes, death from cardiovascular causes, and hospital admission for myocardial infarction in cohort study of patients with newly diagnosed type 2 diabetes and those who had just had a myocardial infarction
|
Diabetic group
|
MI group
|
Risk ratio (95% CI)* | ||||
|---|---|---|---|---|---|---|
| No of patients | No of events | No of patients | No of events | |||
| Death from all causes | ||||||
| Age (years): | ||||||
| <50 | 441 | 30 | 397 | 41 | 0.05 (0.04 to 0.07) | |
| 50-59 | 677 | 92 | 870 | 191 | 0.12 (0.10 to 0.13) | |
| 60-69 | 1005 | 295 | 1457 | 548 | 0.25 (0.23 to 0.27) | |
| 70-79 | 840 | 434 | 1565 | 920 | 0.51 (0.47 to 0.55) | |
| >79 | 440 | 345 | 1061 | 896 | 1.00 | |
| Sex: | ||||||
| Men | 1734 | 604 | 3062 | 1352 | 1.19 (1.12 to 1.26) | |
| Women | 1669 | 592 | 2288 | 1244 | 1.00 | |
| Diagnosis: | ||||||
| MI | — | — | 5350 | 2596 | 1.35 (1.25 to 1.44) | |
| Diabetes | 3403 | 1196 | — | — | 1.00 | |
| Death from cardiovascular causes | ||||||
| Age (years): | ||||||
| <50 | 441 | 6 | 397 | 17 | 0.10 (0.07 to 0.16) | |
| 50-59 | 677 | 12 | 870 | 86 | 0.22 (0.18 to 0.27) | |
| 60-69 | 1005 | 61 | 1457 | 235 | 0.42 (0.36 to 0.48) | |
| 70-79 | 840 | 87 | 1565 | 389 | 0.70 (0.61 to 0.80) | |
| >79 | 440 | 56 | 1061 | 350 | 1.00 | |
| Sex: | ||||||
| Men | 1734 | 113 | 3062 | 559 | 1.07 (0.95 to 1.19) | |
| Women | 1669 | 109 | 2288 | 518 | 1.00 | |
| Diagnosis: | ||||||
| MI | — | — | 5350 | 1077 | 2.93 (2.54 to 3.41) | |
| Diabetes | 3403 | 222 | — | — | 1.00 | |
| Hospital admission for myocardial infarction | ||||||
| Age (years): | ||||||
| <50 | 441 | 11 | 397 | 48 | 1.18 (0.85 to 1.62) | |
| 50-59 | 677 | 20 | 870 | 106 | 1.25 (0.96 to 1.62) | |
| 60-69 | 1005 | 49 | 1457 | 213 | 1.61 (1.28 to 1.99) | |
| 70-79 | 840 | 50 | 1565 | 189 | 1.41 (1.13 to 1.75) | |
| >79 | 440 | 12 | 1061 | 100 | 1.00 | |
| Sex: | ||||||
| Men | 1734 | 69 | 3062 | 385 | 1.00 (0.87 to 1.15) | |
| Women | 1669 | 73 | 2288 | 271 | 1.00 | |
| Diagnosis: | ||||||
| MI | — | — | 5350 | 656 | 3.10 (2.57 to 3.73) | |
| Diabetes | 3403 | 142 | — | — | 1.00 | |
MI=myocardial infarction.
Adjusted for all covariates, derived from Cox regression analysis.
Discussion
We found that patients with type 2 diabetes were at lower risk of death from all causes, death from cardiovascular causes, and hospital admission for myocardial infarction than patients with established coronary heart disease. Thus, our results do not support the hypothesis that patients with diabetes have as high a cardiovascular risk as patients with established coronary heart disease.
Although routine data sources should always be used cautiously,10 the inpatient hospital admissions data and mortality data that we used were derived from nationally collected datasets, a previous study showed that ICD-9 coding for myocardial infarction was accurate in Tayside,11 and the diabetes register, which has complete population based coverage, has been well used and validated.9
Comparison with other studies
For our cross sectional study, we used a design similar to that used by Haffner et al in their Finnish study.4 The patient groups were slightly different in that we included patients whose diabetes was treated by diet only (not included in the Finnish study), and patients in the myocardial infarction group were restricted to those whose myocardial infarction occurred in the preceding eight years. Patients in the myocardial infarction group were clearly at an increased risk of death and hospital admission for myocardial infarction, after adjustment for the differences in age and sex between the two groups. Although we were unable to adjust for differences in cardiovascular risk factors at baseline (smoking status, hypertension, low density and high density lipoprotein cholesterol concentrations, and total cholesterol and triglyceride concentrations), such adjustments in the Finnish study reduced the hazard ratio for death from coronary heart disease only slightly, from 1.4 (95% confidence interval 0.7 to 2.6) to 1.2 (0.6 to 2.4). In our study a substantial decrease would be required for the difference in risk of hospital admission for myocardial infarction to be no longer significant. An important point is the narrow width of the confidence intervals in our study.
Although we could not make a direct comparison between the results from the two studies, as we were unable to determine mortality from coronary heart disease in our patient groups, it is interesting that the result for overall mortality in our study falls within the confidence interval for mortality from coronary heart disease in the Finnish study. We believe that our study highlights the lack of power in the earlier study. It also shows that the cardiovascular risk profile is clearly different in patients with diabetes compared with those who have had a myocardial infarction.
Another concern with the Finnish study was its cross sectional design. Patients were recruited into the study on the basis of existing diabetes (mean duration eight years) and previous myocardial infarction (mean time since infarction not given).4 It is possible that the rates of cardiovascular disease in the two groups varies with time since diagnosis of diabetes and time since myocardial infarction. Our second study therefore compared rates between patients with newly diagnosed diabetes and those who had just had a myocardial infarction. This comparison may have more clinical relevance. Again, the results showed higher risks of death from all causes, cardiovascular deaths, and hospital admission for myocardial infarction in patients who had had a myocardial infarction compared with patients with diabetes.
Implications of results
Our results have important implications for clinical practice, in that we should be cautious about basing treatment decisions on individual risk factors for cardiovascular disease in isolation, as Byrne and Wild have discussed in more detail.6
Acknowledgments
We thank the members of the DARTS/MEMO Collaboration and members of the DARTS Steering Group for their support. MEMO is part of the MRC Health Services Research Collaboration.
Footnotes
Funding: JMME held a Wellcome Trust training fellowship in health services research (Ref 050212). JW is funded by an Aventis fellowship in health economics.
Competing interests: None declared
References
- 1.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-year cardiovascular mortality for men screened in the multiple risk factor intervention trial. Diabetes Care. 1993;16:434–444. doi: 10.2337/diacare.16.2.434. [DOI] [PubMed] [Google Scholar]
- 2.Stratton IM, Adler AI, Neil AW, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Claudi T, Midthjell K, Holmen J, Fougner K, Kruger O, Wiseth R. Cardiovascular disease and risk factors in persons with type 2 diabetes diagnosed in a large population screening: the Nord-Trøndelag diabetes study, Norway. J Intern Med. 2000;248:492–500. doi: 10.1046/j.1365-2796.2000.00759.x. [DOI] [PubMed] [Google Scholar]
- 4.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laasko M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–243. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 5.Haffner SM. Is all coronary heart disease prevention in type 2 diabetes mellitus secondary prevention? J Clin Endocrinol Metab. 2000;85:2108–2110. [Google Scholar]
- 6.Byrne CD, Wild SH. Diabetes care needs evidence based interventions to reduce risk of vascular disease. BMJ. 2000;320:1554–1555. [PMC free article] [PubMed] [Google Scholar]
- 7.Simons LA, Simons J. Diabetes and coronary heart disease. N Engl J Med. 1998;339:1714–1716. doi: 10.1056/NEJM199812033392314. [DOI] [PubMed] [Google Scholar]
- 8.Evans JMM, McDevitt DG, MacDonald TM. The Tayside Medicines Monitoring Unit (MEMO): a record-linkage system for pharmacovigilance. Pharm Med. 1995;9:177–184. [Google Scholar]
- 9.Morris AD, Boyle DIR, MacAlpine R, Emslie-Smith A, Jung RT, Newton RW, et al. The diabetes audit and research in Tayside, Scotland (DARTS) study: electronic record-linkage to create a diabetes register. BMJ. 1997;315:524–528. doi: 10.1136/bmj.315.7107.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Calltorp J, Adami HO, Astrom H, Fryklund L, Rossner S, Trolle Y, et al. Country profile: Sweden. Lancet. 1996;347:587–594. doi: 10.1016/s0140-6736(96)91278-7. [DOI] [PubMed] [Google Scholar]
- 11.McAlpine R, Pringle S, Pringle T, Lorimer R, MacDonald T. A study to determine the sensitivity and specificity of hospital discharge diagnosis data used in the MICA study. Pharmacoepidemiol Drug Safety. 1998;7:311–318. doi: 10.1002/(SICI)1099-1557(199809/10)7:5<311::AID-PDS371>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]