Abstract
Background
Among the determinants of nonadherence, polypharmacy (common in people with multiple pathologies and especially in elderly patients), plays a major role.
Objective
In patients who are subject to polypharmacy involving different classes of medications, the first aim is to assess the impact of medication importance given by patients on (i) medication adherence and (ii) the respective effect of intentionality and habit in medication importance and medication adherence. The second objective is to compare the importance given to medication and adherence in the different therapeutic classes.
Patients and Methods
Patients taking 5–10 different medications for at least 1 month were included in a cross-sectional survey in three private practices in one region in France.
Results
This study included 130 patients (59.2 % female) with 851 medications in total. The mean ± standard deviation (SD) age was 70.5 ± 12.2 years. The mean ± SD of medications taken was 6.9 ± 1.7. Treatment adherence had a strong positive correlation with the patient-perceived medication importance (p < 0.001). Counter-intuitively, taking a large number of medications (≥7) was associated with being fully adherent (p = 0.02). A high intentional nonadherence score was negatively associated with high medication importance (p = 0.003). Furthermore, patient-perceived medication importance was positively associated with taking treatment by habit (p = 0.03). Overall nonadherence more strongly correlated with unintentional nonadherence (p < 0.001) than with intentional nonadherence (p = 0.02). Compared to the antihypertensive class, a decrease in adherence by medication was observed in psychoanaleptics (p < 0.0001) and drugs used in diabetes class (p = 0.002), and a decrease in importance in lipid-modifying agents class (p = 0.001) and psychoanaleptics (p < 0.0001).
Conclusion
The perception of the importance of a medicine is associated with the place of intentionality and habit in patient adherence. Therefore, explaining the importance of a medicine should become an important part of patient education.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40801-023-00361-7.
Key Points
| Although it may appear to be intuitive, this quantitative study demonstrated that medication adherence positively correlated with the importance given by individual patients to their different medications. |
| We observed that intentional nonadherence was negatively associated with high medication importance. Patient-perceived medication importance was positively associated with taking treatment by habit (unintentional adherence). |
| Drugs in the psychoanaleptic and lipid-modifying therapeutic classes were considered less important than those in the antihypertensive class. In addition, adherence was lower for drugs in the anti-diabetic and psychoanaleptic classes than those in the antihypertensive class, with the poorest adherence observed for drugs in the psychoanaleptic class. |
| Explaining the importance of medicines should be essential to patient education. |
Introduction
Medication nonadherence is a frequent [1] and serious problem because of its association with morbidity and mortality [2–4] and its effect on healthcare expenditure [5]. Adherence to medication involves three steps, namely initiation, implementation, and persistence [6]. Nonadherence has numerous determinants [7, 8], such as factors associated with therapy. Among these factors, polypharmacy, which frequent occurs in people with multiple pathologies, especially in elderly patients, plays a major role [9–14]. Polypharmacy may increase the burden of disease and therapy [15] and increase the difficulty of understanding the purpose of each prescribed medication. Thus, the importance given to each medication may differ from that given by their physicians. Sidorkiewicz et al., showed that up to 20 % of patients subject to polypharmacy had low adherence to medications that were considered important by their physicians [16].
Nonadherence may be intentional (deliberate choice by the patient) or unintentional (not dependent on the patient's will, e.g., not taking the medication because of forgetfulness) [17]. Conversely, adherence may also be intentional (having reasons to take the treatment) or unintentional (medication being taken out of habit) [18, 19]. Patients might initially begin taking their medications intentionally and consequently transition toward forming a habit, thereby making the act of taking medications automatic. In other words, just as a distinction is made between unintentional and intentional nonadherence [20], a distinction can be made between intentional adherence, which requires the formation of an intention, and unintentional adherence, which relies on habit [19].
Therefore, the current study primarily aimed to assess the association between perception regarding the importance of the different medications and adherence in people subject to polypharmacy. Our secondary aims were to determine whether the relative importance given to each medication and adherence medication was associated with (i) the type of intentionality, i.e., whether adherence or nonadherence was intentional or unintentional, according to the definitions given above, and (ii) taking medicines out of habit, and (iii). to compare adherence as well as medication importance in the different therapeutic classes (drugs used in diabetes, antihypertensive drugs, lipid-modifying agents, and psychoanaleptic drugs).
Material and Methods
Ethics, Conformity to Publication Reporting Guideline, and Data Availability
This study complied with the Declaration of Helsinki. Approval was obtained from the IRB Ouest II, Angers, RCB identification number: 2019-A02464-53; SI/CPP identification number: 19.09.17.46723 (2019/79). This Institutional Review Board (IRB) validated the following statement written in the research protocol: “the fact that patients answer the questionnaire, after being informed in writing (information sheet placed in the office and explanatory leaflet given to the patient) and orally, will be considered as consent. There will therefore be no written consent to sign.” This study conforms with the STROBE guideline. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Study Design, Settings, and Patient Recruitment
This quantitative, cross-sectional study used a questionnaire administered in three private medical practices in France. The responses to the questionnaire made it possible to calculate different scores, described below, which were the subject of a quantitative study. This study was the MD thesis work of one of the authors (AC) who is referred to below as the investigator. The medical practices were selected through this investigator’ professional network: she contacted the three medical practices where she knew one of the doctors to ask them to participate in the study. They included one in Abbeville (urban), one in Château-Thierry (urban), and one in Woincourt (rural). The 14 doctors from these three practices worked in a group or in multidisciplinary health centers comprising at least three general practitioners (GPs). However, only two had received training in patient education (40 hours in France). These two doctors were following 51 (31.9 %) patients in the study. This information was noted on each patient questionnaire. Doctors engaged in various practices were informed orally and/or by e-mail by the investigator or colleagues who were contacted in advance. Once their agreement was obtained, the investigator visited their offices for two to three consecutive days on dates compatible with the prerogatives of the research, which in particular was the availability of a dedicated room for completing the questionnaires.
Patients were informed about the study by placing information sheets in the waiting rooms. In addition, each doctor explained the purpose of the study to eligible patients and gave them a detailed information leaflet. After giving oral consent, patients were interviewed face-to-face by the investigator to complete the questionnaire in a dedicated room in the private practice. Completing the questionnaire in an interview was justified by the fact that self-administration of the questionnaire could create fatigue due to the number of medications tested, resulting in incomplete answers and unusable questionnaires. This hindrance was immediately apparent in two pilot tests.
Eligibility
The inclusion criteria were patients aged ≥18 years and prescribed at least 5, and no more than 10, different medications for at least one month. Over-the-counter medications and pro re nata prescriptions were excluded. Exclusion criteria were language barrier, cognitive and/or auditory impairment, inability to provide oral consent, persons under guardianship, and treatment being prepared and administered by a third party. Homeopathic prescriptions were excluded.
Questionnaire (Appendix 1 in Supplementary Material) and Score Calculation (Appendix 2 in Supplementary Material)
The questionnaire comprises four parts: (i) patient’s sociodemographic characteristics (age, sex, and socio-professional category according to INSEE – Institut national de la statistique et des études économiques [20]); (ii) assessment of the overall treatment adherence using the Girerd questionnaire [21]. This questionnaire, created in 2001, was initially used for assessing adherence with arterial hypertension. It was chosen because its use has been extended to all chronic treatment and is nowadays recommended by French health insurance providers to assess adherence; (iii) assessment of adherence on a medication-by-medication basis, using the questionnaire developed and validated by Sidorkiewicz et al. [16], containing five questions regarding persistence, omission of a medication dose during the day, omissions for several consecutive days, occasional omissions, and late intake; and (iv) three final questions: the first question, which was derived from the first question of “The Adherence Estimator” [22], assessed the patient-given medication importance by using a visual analog scale ranging from 0 to 10, as used by Sidorkiewicz et al. [16]; the second question aimed to distinguish between intentional or unintentional treatment nonadherence in general, which was elaborated on after a review of the literature and study by Gadkari et al. [23], and the third question assessed the influence of habit on adherence [19].
Score Definition
The mean (± standard deviation [SD]) patient-given medication importance score result was calculated from the mean value of the importance scores given by the 130 patients for each of the 851 medications. The following adherence scores were calculated (Appendix 2 in Supplementary Material): (1) a “general adherence score” based on the sum of positive responses to the six-question Girerd questionnaire, ranging from 0 (perfect adherence) to 6 (poor adherence). The score can be categorized into three classes—0 positive response: perfect adherence; 1–2 positive responses: moderate adherence; and ≥ 3 positives responses: poor adherence [21]; (2) a “medication-by-medication adherence score” based on part 3 of the study questionnaire, ranging from 1 (medication stopped) to 6 (perfect adherence); (3) an “intentional nonadherence score” based on the sum of number of answers ticked to questions 2.1 to 2.5, 2.8, 2.9, and 2.11 in part 4 of the questionnaire, ranging from 0 (perfect adherence: 0 answers ticked) to 8 (poor adherence: 8 answers ticked); (4) an “unintentional nonadherence score” based on the sum of number of answers ticked to questions 2.6, 2.7, and 2.10 in part 4 of the questionnaire, ranging from 0 (perfect adherence: 0 answers ticked) to 3 (poor adherence: 3 answers ticked); and (5) a “lumped intentionality adherence score” calculated by combining the intentional and unintentional nonadherence scores (sum of number of answers ticked), ranging from 1 (poor adherence) to 4 (perfect adherence).
Statistics
The sample size was set based on the study by Sidorkiewicz et al. [16], which investigated the association with patients’ adherence to the importance given by the doctor to a medication. The number of patients required was 130, with approximately 500 medications. A post hoc power calculation was performed.
Data are described with mean (± SD) or median (interquartile range) used for quantitative data and frequency (percentage) for qualitative data. Different statistical techniques were used in the analysis. Moreover, these methods were used in a conforming manner while respecting the assumptions of uses (homoscedasticity, linearity, etc.).
The correlation between patient-perceived medication importance and medication-by-medication adherence was assessed using a correlation coefficient test for repeated measures [24, 25]. To evaluate this main criteria, a method that accounts for the non-independence of the data (repeated measurements) was applied, unlike the common method of averaging each participant. The repeated measures correlation (rmcorr) assesses the overall within-individual association, taking into account the non-independence between observations using an analysis of covariance (ANCOVA), but with an unusual model specification to statistically adjust the inter-individual variability. A graphical representation was also created representing the global regression line as well as the individual regression lines. The assumptions for using rmcorr have also been verified.
In addition, multivariate analysis was performed using mixed-effects logistic regression to determine the impact of medication importance on medication-by-medication adherence, dichotomized at a threshold of 9 (median) and 6 (median), respectively. The model was adjusted for several factors: age, gender, socio-professional category, duration of medication use > 1 year, medication taken by habit, and number of medication dichotomized at a threshold of 7. We dichotomized the scores to improve causal inference. Moreover, the distribution of the data allowed an easier interpretation of the results. The thresholds were selected according to the distribution (threshold at the median) to balance the groups, resulting in a better comparison between groups of individuals with high or low measured values. Odds ratios (ORs) with 95 % confidence intervals (CI) were reported.
The association of intentional or unintentional nonadherence, as well as medication habit with medication importance, was evaluated using a logistic regression model based on generalized estimating equations to account repeated measure (patients with multiple treatments). The ORs with 95 % CI were also reported. The models evaluating association between intentional or unintentional nonadherence with medication importance were adjusted for several factors: age, gender, socio-professional category, duration of medication use > 1 year, GP trained in patient education, number of medication dichotomized at a threshold of 7, general patient adherence score (Girerd questionnaire) dichotomized at a threshold of 5 (median) and medication-by-medication adherence dichotomized at a threshold of 6 (median). For the intentional nonadherence score, scores 4 and 5 were grouped with score 3 because of small numbers (no patient had a score > 5).
The correlation between intentionality (intentional and unintentional nonadherence) or lump intentionality adherence score with patient's general adherence was assessed by Spearman’s rank correlation test. The correlation between the intentional and unintentional nonadherence scores was also evaluated by Spearman’s rank correlation test. Correlation coefficients and 95 % CI obtained by the bootstrapping method were reported.
To compare medication-by-medication adherence score and importance medication between the four therapeutic classes (drugs used in diabetes, antihypertensive, lipid-modifying agents, and psychoanaleptics), a univariate linear mixed model was used. We grouped drugs from the same pharmacological class according to the 2nd level of the WHO Anatomical Therapeutic Chemical (ATC) classification [26] and reported the results for the four most prevalent classes (A10: drugs used in diabetes, C02: antihypertensives, C10: lipid-modifying agents, and N06: psychoanaleptics).
The correlation between medication-by-medication adherence score and importance medication in the four groups was performed using Spearman’s rank correlation test. A mean of medication-by-medication adherence score and importance medication was calculated per patient and 95 % CI was obtained by the bootstrapping method.
Finally, only one patient failed to answer all the medication questionnaire items on adherence; however, this did not affect the score calculation as the patient had stopped taking the medication. There were no missing data, as can be observed in the descriptive Tables. A p-value of <0.05 was considered statistically significant.
All statistical data were analyzed using R Project for Statistical Computing, version 3.5.2 (The R Foundation for Statistical Computing, Vienna, Austria, http://www.r-project.org/).
Results
One hundred and thirty-four patients, treated by 14 GPs, who had been taking 867 medications in total, were recruited between December 2019 and March 2020. In four patients, two of their medications represented two different dosages of the same medication, and we decided to exclude them from the final analysis. Thus, 130 patients were examined, of which 24 were recruited from rural areas (18.5 %) and 106 from urban areas (81.5 %), corresponding to a total of 851 medications.
Patient Characteristics
The mean age (±SD) of the patients was 70.5 ± 12.2 years; most were females (77/130, 59.2 %). The mean (±SD) of medications taken was 6.9 ± 1.7 (details in Table 1). In the Girerd questionnaire, 60.8 % (79/130) of patients answered positively at least once to all six questions (i.e., moderate or poor overall adherence). In addition, 50.7 % (66/130) of the patients gave at least one reason for not taking their medication (intentional nonadherence), and 53.1 % (69/130) gave at least one response suggesting unintentional nonadherence. The majority (125/130, 96.2 %) reported taking their medication out of habit.
Table 1.
Characteristics of the study population
| Patients (N = 130) | |
|---|---|
| Age, years | 70.5 ± 12.2 |
| Sex, female | 77 (59.2 %) |
| Socio-professional category | |
| Farmer | 1 (0.8 %) |
| Craftsman, tradesman, and company director | 0 (0 %) |
| Executive, higher intellectual profession | 0 (0 %) |
| Intermediate profession | 4 (3.1 %) |
| Employee | 12 (9.2) % |
| Manual worker | 1 (0.8 %) |
| Retired | 104 (80 %) |
| No activity | 8 (6.2 %) |
| Number of medications | |
| 5 | 48 (36.9 %) |
| 6 | 25 (19.2 %) |
| 7 | 23 (17.7 %) |
| 8 | 14 (10.8 %) |
| 9 | 11 (8.5 %) |
| 10 | 9 (6.9 %) |
| Adherence score according to Girerd score (inverted scale score) | |
| 0 (poor adherence–6 positive responses) | 0 (0 %) |
| 1 (poor adherence–5 positive responses) | 0 (0 %) |
| 2 (poor adherence–4 positive responses) | 2 (1.5 %) |
| 3 (poor adherence–3 positive responses) | 6 (4.6 %) |
| 4 (moderate adherence–2 positive responses) | 27 (20.8 %) |
| 5 (moderate adherence–1 positive response) | 44 (33.8 %) |
| 6 (perfect adherence–0 positive response) | 51 (39.2 %) |
| Interpretation of the adherence score according to Girerd’s definitions [21] | |
| Perfect adherence (0 positive answer) | 51 (39.2 %) |
| Moderate adherence problems (1–2 positive answers) | 71 (54.6 %) |
| Poor adherence (≥ 3 positive answers) | 8 (6.2 %) |
| Intentional nonadherence score (number of answers ticked) | |
| 0 | 64 (49.2 %) |
| 1 | 38 (29.2 %) |
| 2 | 16 (12.3 %) |
| 3 | 12 (9.2 %) |
| 4 | 0 (0 %) |
| 5 | 0 (0 %) |
| 6 | 0 (0 %) |
| 7 | 0 (0 %) |
| 8 | 0 (0 %) |
| Unintentional nonadherence score (number of answers ticked) | |
| 0 | 61 (46.9 %) |
| 1 | 34 (26.2 %) |
| 2 | 31 (23.8 %) |
| 3 | 4 (3.1 %) |
| Treatment uptake by habit | 125 (96.2 %) |
Characteristics are expressed as mean (± standard deviation) or number of patients (%) Numbers in brackets in the columns on the right represent percentages
Table 2 shows that 93.1 % (769/851) of the medications had been taken for more than 1 year, and in 72.3 % (615/851) of the cases, the highest medication-by-medication adherence score (6, “perfect adherence,” see Appendix 2 in Supplementary Material) was reached. The mean (±SD) patient-given medication importance score was 8.7 ± 1.8. The median score (min–max) for the importance given to medication by the patient was 9.5 [0–10] (detailed data not shown).
Table 2.
Analysis by medication
| Medications (N = 851) | |
|---|---|
| Duration of treatment | |
| <6 months | 56 (6.8 %) |
| 6 months to 1 year | 1 (0.1 %) |
| >1 year | 769 (93.1 %) |
| Discontinued permanently | 11 (1.3 %) |
| Systematic skipping | 13 (1.5 %) |
| Not taking for several days | |
| No | 773 (90.9 %) |
| Yes, sometimes for 2–3 days | 45 (5.3 %) |
| Yes, sometimes for 6–7 days or more | 32 (3.8 %) |
| Intermittent skipping | |
| No | 664 (78.1 %) |
| Yes, 1–2 times a month | 114 (13.4 %) |
| Yes, once a week or more | 72 (8.5 %) |
| Late intake | |
| No | 755 (91.3 %) |
| Yes, >4 hours | 72 (8.7 %) |
| Yes, >12 hours | 0 (0 %) |
| Level of medication-by-medication adherence (inverted scale score) | |
| Medication discontinuation (score: 1) | 11 (1.3 %) |
| Very poor adherence (score: 2) | 40 (4.7 %) |
| Poor adherence (score: 3) | 74 (8.7 %) |
| Average adherence (score: 4) | 77 (9 %) |
| Good adherence (score: 5) | 34 (4 %) |
| Perfect adherence (score: 6) | 615 (72.3 %) |
| Importance of the medication (scale from 0 to 10) | 8.7 ± 1.8 |
Characteristics are expressed as mean (± standard deviation) or number of patients (%) Numbers in brackets in the columns on the right represent percentages
Association Between Perception Regarding the Importance of the Different Medications and Adherence (Primary Aim)
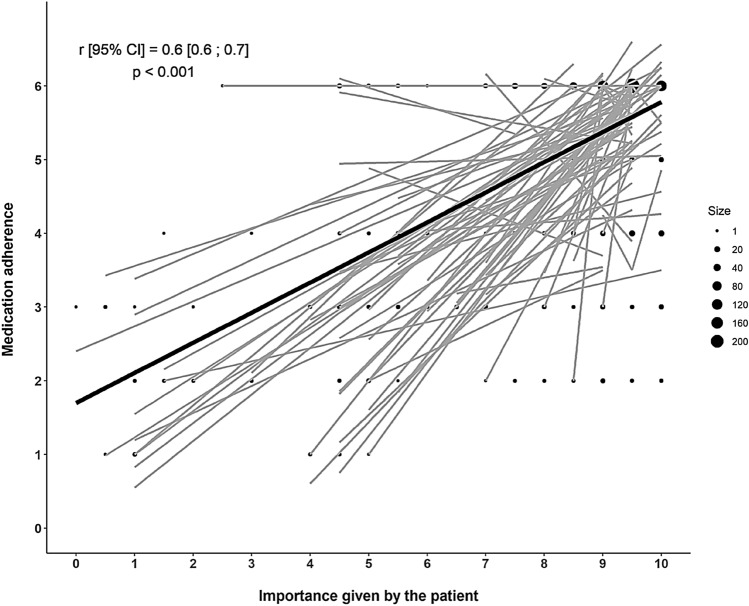
Figure 1 illustrates the correlation between the medication-by-medication adherence score and the importance attributed to a given medication by patients. As presented in Fig. 1 by the dot size, which corresponds to the number of observations in the figure, the medications with high adherence were often those that patients considered as important. Figure 1 also illustrates the individual regression lines per patient, with the common regression line in bold. The correlation coefficient for all patients was 0.6 (95 % CI = 0.6–0.7; p < 0.001).
Fig. 1.
Correlation between the level of medication-by-medication adherence and the medication importance given by the patient. Importance was assessed by a visual scale from 0 to 10. For the purpose of this analysis, medication-by-medication adherence scores were inverted by considering 1 as poor adherence and 6 as good adherence (Table 1). The size of the dots corresponds to the number of observations. The impact of patient-perceived medication importance on medication-by-medication adherence was assessed using a correlation coefficient test for repeated measures. The individual regression lines per patient and the common regression line (bold) are also shown. CI confidence interval
Furthermore, the association between patient-perceived medication importance and medication-by-medication adherence is shown in Table 3. The mixed-effects logistic regression model shows that the patient-perceived importance of medication and the intake of numerous medications (≥7) were positively associated with treatment medication-by-medication adherence (OR [95 % CI] = 8.4 [4.8; 14.6], p < 0.001 and 2.3 [1.1; 4.8], p = 0.02, respectively).
Table 3.
Impact of medication importance given by patients on medication adherence
| OR | 95 % CI | p | ||
|---|---|---|---|---|
| Importance of medication >9 | 8.4 | 4.8 to 14.6 | <0.001 | |
| Age, years | 1.0 | 0.99 to 1.1 | 0.18 | |
| Sex, male | 1.7 | 0.82 to 3.3 | 0.16 | |
| Socio-professional category: Retired/no occupation | 0.7 | 0.2 to 2.2 | 0.53 | |
| Duration of medication use >1 year | 1.2 | 0.6 to 2.5 | 0.53 | |
| Medication taken by habit | 1.9 | 0.3 to 11.0 | 0.48 | |
| Number of medications ≥ 7 | 2.3 | 1.1 to 4.8 | 0.02 | |
CI confidence interval, OR odds ratio
Results of the analysis using a mixed-effects logistic regression model
Association Between Intentional and Unintentional, Nonadherence and High Medication Importance (Score >9) (First Secondary Aim)
Table 4 shows the results of a logistic regression model based on generalized estimating equation analyzing the determinants of high medication importance (score > 9) in an analysis including intentional nonadherence. A high intentional nonadherence score (≥3) was negatively associated with high medication importance (OR [95 % CI] = 0.2 [0.08; 0.6], p = 0.003). In contrast, perfect medication-by-medication adherence (score of 6) was associated with high medication importance (OR [95 % CI] = 4.0 [2.6; 6.1], p < 0.001), consistent with previous results. Patients treated by a GP trained in patient education had a 0.5 reduction in the risk of having an importance score above 9 (95 % CI = 0.3–0.9, p = 0.03).
Table 4.
Determinants of high medication importance (score >9) in an analysis including intentional nonadherence
| OR | 95 % CI | p | |
|---|---|---|---|
| Intentional nonadherence score | |||
| 0 | 1 | – | – |
| 1 | 0.8 | 0.4 to 1.6 | 0.50 |
| 2 | 0.4 | 0.2 to 1.2 | 0.12 |
| ≥3 | 0.2 | 0.08 to 0.6 | 0.003 |
| Age, years | 1.0 | 1.0 to 1.0 | 0.74 |
| Sex, male | 0.6 | 0.3 to 1.2 | 0.15 |
| Socio-professional category: retired/no occupation | 1.8 | 0.5 to 6.0 | 0.34 |
| Number of medications ≥7 | 1.2 | 0.7 to 2.2 | 0.53 |
| Duration of medication >1 year | 1.2 | 0.8 to 2.0 | 0.39 |
| Medication-by-medication adherence by medication: Score of 6 (perfect adherence) | 4.0 | 2.6 to 6.1 | <0.001 |
| Overall adherence score: score ≥ 5 | 1.4 | 0.7 to 2.5 | 0.33 |
| GP trained in patient education | 0.5 | 0.3 to 0.9 | 0.03 |
CI confidence interval, GP general practitioners, OR odds ratio
Results of the analysis using a generalized estimating equations logistic regression model to account multiple medication by patient
Table 5 shows the results of a generalized estimating equation logistic regression model analyzing the factors that influenced patients to give high medication importance (score > 9) in an analysis including unintentional nonadherence. An unintentional adherence score of zero was associated with patient-perceived medication importance. Only one factor was again significantly associated with the importance given to the medication: patients with a perfect (score of 6) adherence medication-by-medication adherence score (OR [95 % CI] = 3.7 [2.4; 5.7], p < 0.001). Again, the patients who were treated by a GP trained in patient education had a 0.5 reduction in the risk of having an importance score above 9, although the threshold for statistical significance was not reached (95 % CI = 0.3–1.1, p = 0.07).
Table 5.
Determinants of high medication importance (score >9) in an analysis including unintentional nonadherence
| OR | 95 % CI | p-value | |
|---|---|---|---|
| Unintentional nonadherence score | |||
| 0 | 1 | – | – |
| 1 | 0.8 | 0.4 to 1.8 | 0.61 |
| 2 | 0.6 | 0.3 to 1.2 | 0.14 |
| 3 | 1.0 | 0.3 to 3.5 | 0.96 |
| Age, years | 1.0 | 1.0 to 1.0 | 0.93 |
| Sex, male | 0.8 | 0.4 to 1.5 | 0.47 |
| Socio-professional category: retired/no occupation | 1.6 | 0.5 to 5.2 | 0.40 |
| Number of medications ≥7 | 1.3 | 0.7 to 2.4 | 0.40 |
| Duration of medication >1 year | 1.2 | 0.8 to 1.9 | 0.44 |
| Medication-by-medication adherence: score of 6 (perfect adherence) | 3.7 | 2.4 to 5.7 | <0.001 |
| Overall adherence score: score ≥5 | 1.3 | 0.7 to 2.5 | 0.43 |
| GP trained in patient education | 0.5 | 0.3 to 1.1 | 0.07 |
CI confidence interval, GP general practitioners, OR odds ratio
Results of the analysis using a generalized estimating equations logistic regression model to account multiple medication by patient
No correlation was observed between the intentional and unintentional nonadherence scores (r [95 % CI] = 0.1 [−0.1; 0.3], p = 0.2). The adherence score calculated from the Girerd questionnaire (inverted scale) was negatively associated with the intentional (r [95 % CI] = −0.2 [−0.4; −0.04], p = 0.02) and unintentional (r [95 % CI] = −0.5 [−0.6; −0.3], p < 0.001) nonadherence scores. The adherence score calculated from the Girerd questionnaire was positively correlated with the lumped adherence score calculated from the intentional and unintentional nonadherence scores (r [95 % CI] = 0.5 [0.3; 0.6], p = 0.001).
Association Between Habit Strength and Adherence to Medications That Were Considered Unimportant and Important (Second Secondary Aim)
According to the logistic regression model based on generalized estimating equation, patient-perceived medication importance was positively associated with treatment taken by habit (OR [95 % CI], 6.4 [1.3; 32.7], p = 0.03), meaning that a medication considered important by the patient was taken more by habit than those considered unimportant.
Medication Importance and Medication-by-Medication Adherence Between Therapeutic Classes (Third Secondary Aim)
According to the mixed linear models, a significant decrease in importance was observed in the therapeutic classes of psychoanaleptic (β ± standard error [SE]: −1.04 ± 0.20, p < 0.0001) and lipid-modifying agents (β ± SE: −0.58 ± 0.18, p = 0.001) compared to the antihypertensive class. For adherence, a significant decrease was observed in drugs used in diabetes and psychoanaleptic classes compared to the antihypertensive class, with a greater decrease for the psychoanaleptic class.
Simultaneously, a positive correlation was observed between the adherence score by medication and the importance given by the patient in antihypertensive therapeutic class (r [IC95 %] = 0.19 [−0.01; 0.39], p = 0.04), lipid-modifying agents (r [IC95 %] = 0.30 [0.02; 0.53], p = 0.007) and psychoanaleptic (r [IC95 %] = 0.51 [0.21; 0.73], p = 0.0003). No correlation was observed in drugs used in diabetes class (r [95 % CI] = −0.03 [−0.35; 0.30], p = 0.86).
Discussion
Main Findings
Although it may appear to be intuitive that people would refrain from taking a medication without clear knowledge regarding its purpose or importance, this quantitative study demonstrated that medication adherence positively correlated with the importance given by individual patients to their different medications. More specifically, the intentional nonadherence score was negatively associated with high medication importance. Patient-perceived medication importance was positively associated with taking treatment by habit (unintentional adherence). Finally, drugs in the psychoanaleptic and lipid-modifying therapeutic classes were considered less important than those in the antihypertensive class. In addition, adherence was lower for drugs in the anti-diabetic and psychoanaleptic classes than the antihypertensive class, with the poorest adherence observed for drugs in the psychoanaleptic class.
Association Between Patient-Perceived Medication Importance and Adherence
The Health Belief Model (HBM) predicts better health behaviors if the perceived importance of the medication is added [27]. The importance given to a medication by a patient may be multifactorial, depending not only on the indication but also on several factors such as the prescriber, being generic/not generic, the dosage, the curative or preventive effect, or patient’s knowledge of the medication [28]. The study by Sidorkiewicz [16] showed that patient adherence had no correlation with doctor-perceived medication importance. Our observation that the importance given to a medication by the patient influences adherence, is another example of a discrepancy between patients’ and doctors’ perceptions [29–31]. In the analysis by therapeutic class, this association was not found for anti-diabetic drugs. This may be because most data concerning this therapeutic class were in the high importance and adherence scores.
Intentionality and Adherence
Our study demonstrated that high intentional nonadherence scores were associated with low patient-perceived medication importance (p = 0.003). One previous study found that patients showing intentional nonadherence had lower perceptions of the need for their new medication and had greater concerns about taking it than those showing adherence [32].
Although intentional and unintentional nonadherence showed no correlation, their dichotomy is not exclusive, considering that one may be a predictive marker of the other. Indeed, Gadkari’s study suggests that the importance of unintentional nonadherence may lie in its potential prognostic significance for future intentional nonadherence [33]. This point is echoed in the present study. The general adherence score based on the Girerd questionnaire was negatively associated with the intentional (r = −0.2) and unintentional (r = −0.5) nonadherence scores. The comparison of these correlation lines suggested that unintentional nonadherence had more association with nonadherence than intentional adherence. This observation is consistent with a study on cardiovascular treatments suggesting that intervention strategies to improve adherence should primarily target unintentional nonadherence and include information and tools to avoid forgetfulness [33]. This intervention should occur within 6 months of treatment initiation because it is during this period that the frequency of unintentional nonadherence increases [34]. Nevertheless, our study revealed an excellent correlation between the Girerd adherence score and the lumped adherence calculated by combining the intentional and unintentional nonadherence scores (p < 0.001). Therefore, tackling both intentional and unintentional sides of nonadherence is important to improve patient adherence [19].
Habit in Adherence
Habit strength was first considered in HBMs in the late 1970s through Triandis’ Theory of Interpersonal Behavior [35]. The intervention of habit strength in adherence has been shown in a theoretical paper [36] and several empirical studies [18, 19, 37–40]. In our study, patient-given medication importance was positively associated with taking treatment by habit (p = 0.03). It is tempting to speculate that this result is a consequence of the impact of importance on initial adherence, that is, a medication that is considered important is a medication that ends up being taken by habit.
Influence of the Number of Medications on Adherence
In our study, having more than seven medications was associated with being fully adherent (p = 0.02). This result is indeed counter-intuitive and is not consistent with the literature. In the Girerd adherence questionnaire [21], having the impression of taking too many tablets is a factor of nonadherence, leading to the patient favoring combined forms of medication [41, 42]. One possible explanation is that these patients frequently used a pillbox/semainier, which promotes better adherence [12]. Another explanation could indicate to patients that more treatments mean a more severe condition, and the more dependent they were on their treatment to maintain their health. A previous study showed that the influence of disease perceptions, treatment beliefs, and disease burden had an important role in predicting treatment adherence [43].
Surprisingly, this study showed that the patients who were treated by a GP trained in patient education showed a 0.5 reduction in the risk of having an importance score of >9, with p-values of 0.03 and 0.07 when intentional or unintentional nonadherence was included in the logistic regression models, respectively. Provided that these serendipitous observations are not by chance alone, they may suggest that doctors have not been trained to explain the importance of medication as a topic for patient education.
Strengths and Limitations of the Study
One of the strengths of this study is that the administered questionnaire was derived from literature reviews and validated questionnaires [15, 18–23]. Despite the small number of medications that may have been considered as unimportant, such as phlebotonic drugs (they were not removed from the study), we were able to demonstrate the effect of patient-perceived importance on medication adherence with 130 patients, as was also confirmed by a post hoc power calculation (providing a 90 % power with alpha risk of 5 % and coefficient correlation of 0.6). Furthermore, the questionnaires were administered by a person other than the usual GP; thus, the social desirability bias might have been reduced. Finally, our study showed the excellent correlation between the adherence score via the Girerd questionnaire [21] and the “lumped adherence” calculated by combining the intentional and unintentional nonadherence scores (p < 0.001). Hence, it confirms the interest and reliability of using this type of score to assess adherence. Nevertheless, we recognize that an objective or quasi-objective method (e.g., pharmacy claims data) supporting adherence results would have been preferable.
However, this study has limitations. The number of participation refusals could not be precisely estimated because refusal was formulated directly to the GPs conducting the inclusion, without a precise count. Reasons for refusal included lack of time, another appointment scheduled after the consultation, and a relative waiting for the patient outside the practice. The current study involved only 134 patients who were recruited from three private practices in one region of France, which might hamper the generalizability of the results. We attempted to minimize selection bias by asking health professionals to recruit all consecutive eligible patients during the recruitment period. Finally, we chose not to use a self-administered questionnaire; even though the questionnaire is composed of simple questions, it covered many medicines and we believed that this might result in fatigue and prevent a complete response. The patients were interviewed face-to-face by an investigator to complete the questionnaire, and we recognize that this may have increased the social desirability bias (i.e., patient presented as being adherent because they were being interviewed and their details readily available). However, we endeavored to reduce social desirability bias by introducing the questionnaire with standardized non-judgmental sentences aiming at reducing the overestimation of self-reported adherence. Moreover, we excluded patients who were prescribed over 10 medications, to reduce respondent burden; however, this may have decreased the number of included patients with a high burden of treatment, which impacts medication adherence in the literature [15].
Conclusion: Implication for Practice
Prescription writing is a major opportunity to practice patient education during the consultation, but it is an act that frequently puts patients aside. Indeed, the prescription is written primarily for the pharmacist for medication dispensation. The patient then uses this prescription to prepare her/his pillbox or to take her/his treatment at the prescribed dosage. We suggest that patient adherence to medications can be improved if doctors use the time during writing prescriptions to make the patient aware of the importance of the medications being prescribed, and if the prescription is used to promote better collaboration between health professionals at each stage of the care process, including receiving advice from the pharmacist [44] and educational interventions by nurses.
Finally, asking patients how important for them the medications are can be a quick and very informative way of improving communication, which in turn, improves trust [45], which is necessary to achieve adherence [46–48]. A patient who values his or her treatment may be more adherent in the context of a shared medical decision [49].
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
The authors did not receive support from any organisation for conducting this study and preparing the manuscript.
Declarations
Author Contribution
GR and MF were the research directors of AC who conducted the interviews. All authors contributed to the design of the study and analysis of the results. NS and MB conducted the statistical analyses. GR drafted the manuscript, which was discussed by all the authors who approved its final form. All authors therefore made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Conflict of interest
The authors did not receive support from any organization for conducting this study and preparing the manuscript. The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
This study complied with the Declaration of Helsinki. Approval was obtained from the IRB Ouest II, Angers, RCB identification number: 2019-A02464-53; SI/CPP identification number: 19.09.17.46723 (2019/79). This study conforms with the STROBE guideline.
Consent to participate
The IRB validated the following statement written in the research protocol: “the fact that patients answer the questionnaire, after being informed in writing (information sheet placed in the office and explanatory leaflet given to the patient) and orally, will be considered as consent. There will therefore be no written consent to sign.”
Consent for publication
Not applicable.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
- 1.Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy. 2008;28:437–443. doi: 10.1592/phco.28.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bansilal S, Castellano JM, Garrido E, et al. Assessing the impact of medication adherence on long-term cardiovascular outcomes. J Am Coll Cardiol. 2016;68:789–801. doi: 10.1016/j.jacc.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Khunti K, Seidu S, Kunutsor S, Davies M. Association between adherence to pharmacotherapy and outcomes in type 2 diabetes: a meta-analysis. Diabetes Care. 2017;40:1588–1596. doi: 10.2337/dc16-1925. [DOI] [PubMed] [Google Scholar]
- 4.Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, Magid DJ. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 5.Mennini FS, Marcellusi A, von der Schulenburg JM, et al. Cost of poor adherence to anti-hypertensive therapy in five European countries. Eur J Health Econ. 2015;16:65–72. doi: 10.1007/s10198-013-0554-4. [DOI] [PubMed] [Google Scholar]
- 6.Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73:691–705. doi: 10.1111/j.1365-2125.2012.04167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reach G. The Mental Mechanisms of Patient Adherence to Long-Term Therapies, Mind and Care. Springer, Berlin, 2015.
- 8.Peh KQE, Kwan YH, Goh H, et al. An adaptable framework for factors contributing to medication adherence: results from a systematic review of 102 conceptual frameworks. J Gen Intern Med. 2021;36:2784–2795. doi: 10.1007/s11606-021-06648-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Payne RA, Avery AJ. Polypharmacy: one of the greatest prescribing challenges in general practice. Br J Gen Pract. 2011;61:83–84. doi: 10.3399/bjgp11X556146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13:57–65. doi: 10.1517/14740338.2013.827660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burnier M, Polychronopoulou E, Wuerzner G. Hypertension and drug adherence in the elderly. Front Cardiovasc Med. 2020;7(7):49. doi: 10.3389/fcvm.2020.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pasina L, Brucato AL, Falcone C, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31:283–289. doi: 10.1007/s40266-014-0163-7. [DOI] [PubMed] [Google Scholar]
- 13.Kurczewska-Michalak M, Lewek P, Jankowska-Polańska B, et al. Polypharmacy management in the older adults: A scoping review of available interventions. Front Pharmacol. 2021;26(12):734045. doi: 10.3389/fphar.2021.734045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deprescription SG. The prescription metabolism. J Pharmacol Pharmacother. 2016;7:133–137. doi: 10.4103/0976-500X.189680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tran VT, Montori VM, Eton DT, Baruch D, Falissard B, Ravaud P. Development and description of measurement properties of an instrument to assess treatment burden among patients with multiple chronic conditions. BMC Med. 2012;10:68. doi: 10.1186/1741-7015-10-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sidorkiewicz S, Tran VT, Cousyn C, Perrodeau E, Ravaud P. Discordance between drug adherence as reported by patients and drug importance as assessed by physicians. Ann Fam Med. 2016;14:415–421. doi: 10.1370/afm.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lehane E, McCarthy G. Intentional and unintentional medication nonadherence: a comprehensive framework for clinical research and practice? A discussion paper. Int J Nurs Stud. 2007;44:1468–1477. doi: 10.1016/j.ijnurstu.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Phillips LA, Cohen J, Burns E, Abrams J, Renninger S. Self-management of chronic illness: The role of “habit” versus reflective factors in exercise and medication adherence. J Behav Med. 2016;39:1076–1091. doi: 10.1007/s10865-016-9732-z. [DOI] [PubMed] [Google Scholar]
- 19.Reach G, Benarbia L, Bruckert E, Kevorkian JP, Farnier M, Mourad JJ, Vaisse BC. Intentionality in adherence to long-term therapies. Results from an online survey of 3,001 patients with cardio-metabolic pathologies in France. Patient Prefer Adherence. 2021;15:1739–1753. doi: 10.2147/PPA.S318116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.PCS 2003-4-professions intermédiaires, Insee [Internet]. cited on 17 févr 2018. Available on: https://www.insee.fr/fr/metadonnees/pcs2003/categorieSocioprofessionnelleAgregee/4.
- 21.Girerd X, Hanon O, Anagnostopoulos K, Ciupek C, Mourad JJ. Consoli S [Assessment of antihypertensive compliance using a self-administered questionnaire: development and use in a hypertension clinic] Presse Med. 2001;30:1044–1048. [PubMed] [Google Scholar]
- 22.McHorney CA. The adherence estimator: A brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr Med Res Opin. 2009;25:215–238. doi: 10.1185/03007990802619425. [DOI] [PubMed] [Google Scholar]
- 23.Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: How unintentional is it really? BMC Health Serv Res. 2012;12:98. doi: 10.1186/1472-6963-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bakdash JZ, Marusich LR. Repeated measures correlation. Front Psychol. 2017;8:456. doi: 10.3389/fpsyg.2017.00456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bland JM, Altman DG. Calculating correlation coefficients with repeated observations: Part 2—Correlation between subjects. BMJ. 1995;310:633. doi: 10.1136/bmj.310.6980.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2017 [Available from: https://www.whocc.no/atc_ddd_index/.
- 27.Orji R, Vassileva J, Mandryk R. Towards an effective health interventions design: an extension of the health belief model. Online J Public Health Inform. 2012;4:4. doi: 10.5210/ojphi.v4i3.4321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lau DT, Briesacher BA, Mercaldo ND, et al. Older patients’ perceptions of medication importance and worth: an exploratory pilot study. Drugs Aging. 2008;25:1061–1075. doi: 10.2165/0002512-200825120-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duckworth KE, Morrell R, Russell GB, et al. Goals and adverse effects: rate of concordance between patients and providers. J Oncol Pract. 2019;15:e798–e806. doi: 10.1200/JOP.19.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoge A, Pétré B, Streel S, Dardenne N, Husson E, Guillaume M, Scheen A. P80 Le diabète de type 2 vécu par le patient: Résultats de l’enquête EDUDORA2 étudiant les représentations des patients et des médecins généralistes. Diabetes Metab. 2014;40:A49. [Google Scholar]
- 31.Desthieux C, Hermet A, Granger B, Fautrel B, Gossec L. Patient-physician discordance in global assessment in rheumatoid arthritis: A systematic literature review with meta-analysis. Arthritis Care Res (Hoboken). 2016;68:1767–1773. doi: 10.1002/acr.22902. [DOI] [PubMed] [Google Scholar]
- 32.Clifford S, Barber N, Horne R. Understanding different beliefs held by adherers, unintentional nonadherers, and intentional nonadherers: Application of the necessity-concerns framework. J Psychosom Res. 2008;64:41–46. doi: 10.1016/j.jpsychores.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Van der Laan DM, Elders PJM, Boons CCLM, Nijpels G, Hugtenburg JG. Factors associated with nonadherence to cardiovascular medications: a cross-sectional Study. J Cardiovasc Nurs. 2019;34:344–352. doi: 10.1097/JCN.0000000000000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molloy GJ, Messerli-Bürgy N, Hutton G, Wikman A, Perkins-Porras L, Steptoe A. Intentional and unintentional non-adherence to medications following an acute coronary syndrome: a longitudinal study. J Psychosom Res. 2014;76:430–432. doi: 10.1016/j.jpsychores.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Triandis HC. Values, attitudes, and interpersonal behavior. Nebr Symp Motiv. 1980;27:195–259. [PubMed] [Google Scholar]
- 36.Reach G. Role of habit in adherence to medical treatment. Diabet Med. 2005;22:415–420. doi: 10.1111/j.1464-5491.2004.01449.x. [DOI] [PubMed] [Google Scholar]
- 37.Reach G, Pellan M, Crine A, Touboul C, Ciocca A, Djoudi Y. Holistic psychosocial determinants of adherence to medication in people with type 2 diabetes. Diabetes Metab. 2018;44:500–507. doi: 10.1016/j.diabet.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 38.Phillips LA, Burns E, Leventhal H. Time-of-day differences in treatment-related habit strength and adherence. Ann Behav Med. 2021;20(55):280–285. doi: 10.1093/abm/kaaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bolman C, Arwert TG, Völlink T. Adherence to prophylactic asthma medication: Habit strength and cognitions. Heart Lung. 2011;40:63–75. doi: 10.1016/j.hrtlng.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 40.Murphy J, Eustace N, Sarma KM, Molloy GJ. Habit strength and adherence to oral contraceptives: the role of time- and place-based cues. Int J Behav Med. 2018;25:431–437. doi: 10.1007/s12529-018-9729-9. [DOI] [PubMed] [Google Scholar]
- 41.Leslie KH, McCowan C, Pell JP. Adherence to cardiovascular medication: a review of systematic reviews. J Public Health (Oxf) 2019;41:e84–e94. doi: 10.1093/pubmed/fdy088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kawalec P, Holko P, Gawin M, Pilc A. Effectiveness of fixed-dose combination therapy in hypertension: systematic review and meta-analysis. Arch Med Sci. 2018;14:1125–1136. doi: 10.5114/aoms.2018.77561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rajpura J, Nayak R. Medication adherence in a sample of elderly suffering from hypertension: evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J Manag Care Pharm. 2014;20:58–65. doi: 10.18553/jmcp.2014.20.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mino-León D, Reyes-Morales H, Flores-Hernández S. Effectiveness of involving pharmacists in the process of ambulatory health care to improve drug treatment adherence and disease control. J Eval Clin Pract. 2015;21:7–12. doi: 10.1111/jep.12207. [DOI] [PubMed] [Google Scholar]
- 45.Thom DH, Stanford Trust Study Physicians. Physician behaviors that predict patient trust. J Fam Pract. 2001;50:323-328. [PubMed]
- 46.Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract. 2004;5:26. doi: 10.1186/1471-2296-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nguyen GC, LaVeist TA, Harris ML, Datta LW, Bayless TM, Brant SR. Patient trust-in-physician and race are predictors of adherence to medical management in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1233–1239. doi: 10.1002/ibd.20883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zikmund-Fisher BJ, Hofer TP, Klamerus ML, Kerr EA. First things first: Difficulty with current medications is associated with patient willingness to add new ones. Patient. 2009;2:221–231. doi: 10.2165/11313850-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ratanawongsa N, Karter AJ, Parker MM, et al. Communication and medication refill adherence: the diabetes study of Northern California. JAMA Intern Med. 2013;173:210–218. doi: 10.1001/jamainternmed.2013.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.