Abstract
Normal pressure hydrocephalus typically presents with a clinical triad of progressively worsening symptoms, including gait disturbance, urinary incontinence, and cognitive deficits. Occasionally, it may also manifest with significant psychiatric symptoms, which can delay early diagnosis and treatment. We present a rare case of chronic hydrocephalus in a 54-year-old patient who initially presented with symptoms of mania, which led to a delay in diagnosis and treatment. Our case highlights the importance of considering organic causes for psychiatric symptoms, especially in older patients. Early diagnosis and treatment of conditions such as hydrocephalus can prevent delays and improve patient outcomes.
Keywords: Idiopathic chronic hydrocephalus, Normal pressure hydrocephalus, Encephalic MRI, Psychiatric symptoms
Background
Idiopathic chronic hydrocephalus is characterized by the dilatation of the ventricular system with normal opening cerebrospinal fluid pressure. It typically presents with a clinical triad of progressively worsening symptoms, including gait disturbances, urinary incontinence, and cognitive impairment. Although rare, it also manifests with predominant psychiatric symptoms, which can delay early diagnosis and treatment. We present an unusual case of idiopathic chronic hydrocephalus that was initially revealed by symptoms of mania, emphasizing the importance of recognizing psychiatric implications in patients with this condition.
Case presentation
In this report, we present an unusual case of 54-years-old male who was single and worked as a civil employee in a public institution. He had a history of chronic smoking, and a childhood diagnosis of a hydrocephalus, which had been treated with three shunts between the ages of 5 and 7 years. His treatment had been successful, with good clinical and radiological outcomes, and he had normal psychomotor development. He had no previous medical or psychiatric history, including no history of hypomania or depression, and had a good socio-professional functioning.
The patient's symptoms started two months before his admission with a progressive onset of irritability, logorrhea, insomnia, wandering, excessive cigarette use, and excessive spending. He also showed psychomotor instability with tantrums. Over time, his symptoms worsened, and he began to exhibit agitation and aggressiveness, prompting his family to seek medical care for him.
During the psychiatric evaluation, the patient was conscious, well oriented, with familiar contact, he exhibited hypermimia and a euphoric mood with an appropriate affect. He also displayed logorrhea, tachyphemia and tachypsychia. Additionally, he had a megalomaniac delusion with multiple projects and impaired judgment. The somatic examination, including the neurological assessment did not reveal any abnormalities.
Following a request from a third party, the patient was admitted to our department and started on medication, which included Olanzapine 10 mg/d, sodium Valproate 1500 mg/d, and Levomepromazine 300 mg/d.
A complete biological workup and a brain CT scan were ordered but not performed, as the patient left the hospital the next morning against medical advice.
The patient's progress was marked by poor adherence to treatment and noncompliance with scheduled appointments, and subsequently he was lost to follow up.
However, a year and a half later, the patient returned to the psychiatric emergency department presenting the same symptoms of psychomotor instability.
The patient's family reported that he did not return to his premorbid state and that his pre-existing symptoms had worsened. He was smoking 20 packs of cigarettes per day, and his irritability and fits of anger had worsened, leading to issues at work. Additionally, urinary incontinence with gait disorder had developed. During the psychiatric evaluation, the patient was conscious and well oriented, but unstable and contact with him was difficult due to his irritable and angry mood. He presented with logorrheic speech, a megalomaniac delusion, multiple projects, and perturbed judgment.
Neurological examination revealed a gait disorder, but there were no other particularities.
Following a request from a third party, the patient was admitted to our department and started on medication, which included Olanzapine 10 mg/d, sodium Valproate 1500 mg/d, Levomepromazine 300 mg/d and Alprazolam 1.5 mg/d.
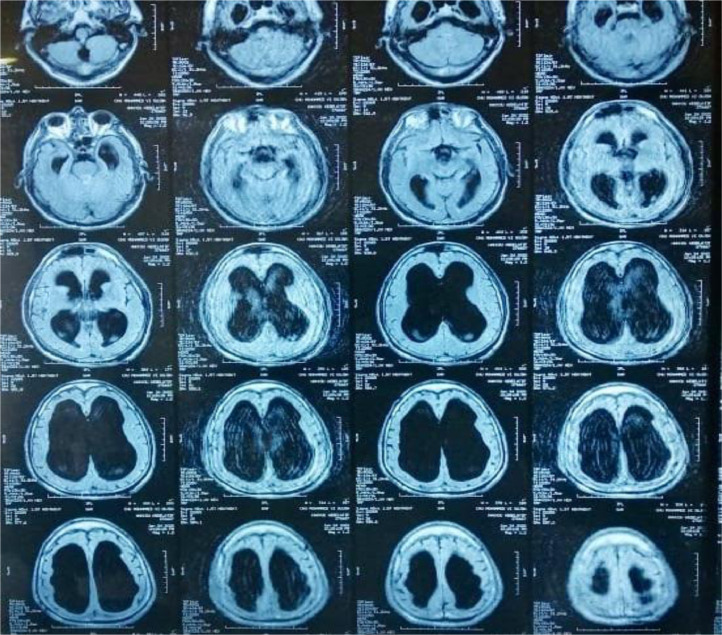
The MRI showed a quadric ventricular hydrocephalus. (Figs. 1 and 2)
Fig. 1.
Brain MRI axial section T2 showing quadric ventricular hydrocephalus.
Fig. 2.
Brain MRI axial section FLAIR sequence, showing quadric ventricular hydrocephalus, without signs of trans ependymal resorption.
To summarize, during his first admission, the patient presented with psychiatric symptoms suggestive of a maniac episode but left the hospital against medical advice before the necessary tests could be performed to exclude a suspected organic cause due to his onset of symptoms. In his second admission, a year and a half later, the patient returned with worsening symptoms including urinary incontinence and gait disorder. A quadric ventricular hydrocephalus was identified on MRI. The patient was diagnosed with idiopathic cerebral hydrocephalus and neurosurgery was solicited.
After 3 therapeutic depletive lumbar punctures (cerebrospinal fluid tap test), there was a moderate improvement in the psychiatric symptomatology, but no improvement in the gait disorder, incontinence, or memory disorders, and the decision to perform a shunt was difficult to make. The patient was discharged on antipsychotic and mood-stabilizing treatment, after stabilizing their psychomotor instability, attenuating manic symptoms and delusion, and improving their sleep and judgment.
The are several elements in our clinical case that suggest a possible link between chronic hydrocephalus and psychiatric symptoms. Firstly, the late age of onset of the psychiatric symptomatology is significant, along with the absence of any psychiatric history or drug use. Additionally, the psychiatric symptoms observed do not completely meet the criteria for a mood disorder (for example, hypermnesia instead of memory deficiency during manic episodes), and the symptoms of the triad (gait disorder, urinary incontinence, and cognitive decline) following the psychiatric symptomatology, with worsening during the course of the disease, support the hypothesis of chronic hydrocephalus as an underlying cause. All of these factors support the idea of a potential relationship between the hydrocephalus and the patient's psychiatric symptomatology.
Discussion
Chronic adult hydrocephalus, also known as normal pressure hydrocephalus, is characterized by a symptomatic increase in cerebral ventricular volume related to a disorder of cerebrospinal fluid (CSF) physiology. The classic triad of symptoms includes gait disturbance, urinary incontinence, and cognitive decline, but psychiatric symptoms and syndromes may also occur, usually appearing after the main symptomatology [1], [2], [3]. However, in our case the psychiatric symptoms were prominent and preceded the typical symptomatology.
Numerous studies have described the association between chronic hydrocephalus and psychiatric symptomatology. This relationship may be related to alterations in the activity of central serotonergic, dopaminergic, and noradrenergic neurotransmitters, and it is important to differentiate true psychiatric symptoms from misperceptions resulting from the patient's compromised ability to organize perceptual information. Patients with normal pressure hydrocephalus may develop frontal-dominant symptoms, such as personality changes, anxiety, depression, psychotic syndromes, obsessive-compulsive disorder, Othello syndrome, shoplifting, and mania [3], [4], [5], [6], [7], [8], [9].
In a study that included 35 patients with idiopathic chronic hydrocephalus, 25 of them (71.42%) presented with psychiatric disorders. The most frequently observed disorders were depression and anxiety syndromes in 17 patients, followed by psychotic syndromes in 7 patients, and bipolar disorder in 1 patient [8].
Based on studies, it is reported that 93% of patients with normal pressure hydrocephalus will experience improvement in their gait after undergoing surgery, while only 50% may experience improvement in cognitive and neuropsychiatric symptoms. Improvement in incontinence and gait is typically observed within 3 months postsurgery, while cognitive improvement may take longer. If surgical intervention does not improve psychiatric symptoms, pharmacological and nonpharmacological treatments may be necessary to improve the patient's quality of life and that of their caregivers [10], [11], [12].
Conclusion
The unusual presentation of hydrocephalus in our case highlights the importance of considering an organic cause for any late-onset psychiatric symptoms, particularly in the presence of cognitive impairment, gait disturbances, or urinary incontinence. The decision to perform a shunt can be challenging, as it is difficult to predict the prognosis and course of the disease in patients. Therefore, it is crucial to request brain imaging systematically in all elderly patients with psychiatric disorders, with or without neurological symptoms, to ensure timely diagnosis and appropriate treatment.
Patient consent
Data collection was made after written consent for the patient. We carried out this case report with respect for patient anonymity and confidentiality of information. (Full written informed consent from parents is available)
Footnotes
Acknowledgements: This research did not receive any grant from funding agencies in public, commercial or not for profit sectors.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH. Symptomatic occult hydrocephalus with ‘normal’ cerebrospinal-fluid pressure. A treatable syndrome. N Engl J Med. 1965;273:117–126. doi: 10.1056/NEJM196507152730301. [DOI] [PubMed] [Google Scholar]
- 2.Bret P, Guyotat J, Chazal J. Is normal pressure hydrocephalus a valid concept in 2002? A reappraisal in five questions and proposal for a new designation of the syndrome as ‘chronic hydrocephalus. J Neurol Neurosurg Psychiatry. 2002;73(1):9–12. doi: 10.1136/jnnp.73.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nassar BR, Lippa CF. Idiopathic normal pressure hydrocephalus. Gerontol Geriatr Med. 2016;2 doi: 10.1177/2333721416643702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acar M, Erol A. Obsessive compulsive symptoms presented during the course of chronic normal pressure hydrocephalus: a case report. Düşünen Adam - Psikiyatri ve Nörolojik Bilimler Dergisi. 2018;31(2):215–221. [Google Scholar]
- 5.Kogan M, Agyei J, Cuddahee KJ, Gibbons KJ. Normal pressure hydrocephalus with primary presentation of psychiatric disturbance: Case report. J Neurol Surg A Cent Eur Neurosurg. 2019;80(5):404–408. doi: 10.1055/s-0039-1685185. [DOI] [PubMed] [Google Scholar]
- 6.Kwentus JA, Hart RP. Normal pressure hydrocephalus presenting as mania. J Nerv Ment Dis. 1987;175(8):500–502. doi: 10.1097/00005053-198708000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Morin V, Bonafos A, Masson M, Vederine FE. Symptomatologie psychotique et hydrocéphalie : à propos d'un cas. Ann Médico-psychol, revue Psychiatr. 2017;175(10):929–932. [Google Scholar]
- 8.Oliveira MF, Oliveira JRM, Rotta JM, Pinto FCG. Psychiatric symptoms are present in most of the patients with idiopathic normal pressure hydrocephalus. Arq Neuro-Psiquiatr. 2014;72:435–438. doi: 10.1590/0004-282x20140047. [DOI] [PubMed] [Google Scholar]
- 9.Anna Yusim, Anbarasan D, Bernstein C, Boksay I, Dulchin M, Lindenmayer JP, et al. Normal pressure hydrocephalus presenting as othello syndrome: case presentation and review of the literature. AJP. 2008;165(9):1119–1125. doi: 10.1176/appi.ajp.2008.07111820. [DOI] [PubMed] [Google Scholar]
- 10.Kito Y, Kazui H, Kubo Y, Yoshida T, Takaya M, Wada T, et al. Neuropsychiatric symptoms in patients with idiopathic normal pressure hydrocephalus. Behav Neurol. 2009;21(3):165–174. doi: 10.3233/BEN-2009-0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Markianos M, Lafazanos S, Koutsis G, Sfagos C, Seretis A. CSF neurotransmitter metabolites and neuropsychiatric symptomatology in patients with normal pressure hydrocephalus. Clin Neurol Neurosurg. 2009;111(3):231–234. doi: 10.1016/j.clineuro.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Pinner G, Johnson H, Bouman WP, Isaacs J. Psychiatric manifestations of normal-pressure hydrocephalus: a short review and unusual case. Int Psychogeriatr. 1997;9(4):465–470. doi: 10.1017/s1041610297004602. [DOI] [PubMed] [Google Scholar]