Abstract
Therapeutic exercise is integral to the comprehensive rehabilitation of patients with cardiovascular disease and, as such, is recommended by the American Heart Association as a valuable and effective treatment method for such patients. The type of exercise applied to these patients is aerobic and resistance exercise with mild intensities and loads to avoid overloading the cardiovascular system. Blood flow restriction exercise is a novel exercise modality in clinical settings that has in many studies a similar effect on muscle hypertrophy, strength, and cardiovascular response to training at a 70% strength level without blood flow restriction. Since this exercise mode does not require high-intensity loads, it can be a safe method for improving muscle strength, cardiovascular endurance, and functionality in cardiovascular patients. Given that, the objective of this review is to assess and summarize existing evidence for the use of blood flow restriction in cardiovascular patients. A scoping review of existing clinical trials was conducted. Eleven studies were examined that suggested the use of blood flow restrictions in cardiovascular patients to achieve improvements in muscle strength, functionality, and cardiovascular parameters such as blood pressure decrease.
Keywords: Blood flow restriction exercise, Cardiac rehabilitation, Cardiovascular patients
Introduction
Cardiovascular pathologies are the leading cause of death in developed countries and are now turning into a global pandemic, especially as they are now also affecting populations in developing countries. Over 19 million people die annually from cardiovascular diseases (CVD)[1-3], a group of disorders that affect the heart, blood vessels (arteries, capillaries, and veins), or both[4]. The most common cardiovascular diseases, and therefore the most important for public health, are ischemic or coronary heart disease and vascular stroke. Other heart diseases with a more negligible epidemiological incidence include peripheral arterial disease, congenital heart disease, and arrhythmias. Age, gender, race, and family history are non-modifiable factors, while clinical and behavioral factors are modifiable. Clinical characteristics include obesity, hypertension, dyslipidemia, diabetes mellitus, and cholesterol. Behavioral factors include reduced physical activity, smoking, unhealthy eating habits, stressful lifestyle, and socioeconomic level.
Specialized drugs and therapeutic exercises are prescribed for treating these diseases, while specific medical interventional techniques are applied in difficult situations. Therapeutic exercise is one of the most widely documented therapeutic approaches for the functional rehabilitation of patients with cardiovascular disease. There is substantial evidence that moderate-intensity targeted training is essential for preventing ischemic heart disease, stroke, and hypertension. In addition, therapeutic exercise has improved quality of life and reduced morbidity and mortality in patients with cardiovascular disease[5-10].
Based on the findings mentioned above, patients with cardiovascular disease could benefit if they join rehabilitation programs using therapeutic exercise, given that patients with cardiac disease often have low cardiovascular function, muscle mass, and strength levels[11]. The main types of exercise that have been evaluated and applied to such patients are mild aerobic exercise (walking, stationary cycling) and limb- and trunk-strengthening exercises. In recent years, new forms of exercise have emerged that include exercise with blood flow restriction (BFR) and the use of submaximal training load. These therapeutic exercises could lead to functional adaptations equal to classical high-intensity training without requiring high-intensity exercise. Based on the above, such exercises could be a beneficial and safe suggestions even in high-risk patient groups, such as patients with cardiovascular diseases.
More specifically, restricting (not occluding) blood flow (in combination or not with exercise) is connected with positive adaptations to skeletal muscle and bones in various populations (old, young, trained, untrained)[12]. When BFR training is conducted, the blood flow to the exercising muscle is restricted by pneumatic cuffs or inflated tourniquets that are applied to the nearest part of the upper or lower extremities to reduce the amount of blood that flows back from the muscles in the extremities during a particular exercise.
Research has shown that low loads corresponding to 20–30% of one repetition maximum combined with BFR can improve muscle hypertrophy and strength to levels[13-15]. These adaptations are significant in the case of cardiovascular patients, for whom the American Heart Association currently recommends exercise using low loading and intensity[16]. Therefore, “occlusion exercise” could be a valuable tool for clinical therapists, as it accelerates patient recovery by minimizing muscle mass and strength and functional deficits that occur during periods of reduced patient mobility and activity. However, no review has yet been carried out that has systematically evaluated studies that have examined the value of exercise with BFR in patients with cardiac problems. Therefore, this scoping review aims to evaluate all recent literature regarding the impact of low-load BFR resistance training in patients with cardiovascular pathologies on muscle strength and hypertrophy, vascular function, safety, cardiovascular responses, and inflammatory markers.
Materials and Methods
This scoping review investigates the effectiveness of blood flow restriction training (BFRT) in cardiovascular patients. In it, studies in which the participants were patients with cardiovascular disorders treated with interventions using BFRT were evaluated to determine their effectiveness. This review followed the instructions of the Preferred Reference for Systematic Reviews and Meta-Analysis[17] and the Cochrane Handbook for Systematic Reviews of Interventions[18]. Databases such as PubMed, the Physiotherapy Evidence Database, and the Cochrane Central Register of Controlled Trials (CENTRAL) were used to search for research. In addition, the CENTRAL database was used to include controlled studies not appearing in the Medline and Embassy databases[19]. This ensured that most exposures were covered as well as possible[20]. The above databases were searched for published English and nonrandomized controlled epidemiological studies. Keywords used were “cardiovascular patients”, “cardiac rehabilitation”, “blood flow restriction training”, and “occlusion training”. Relevant systematic reviews were also included to reduce the possibility of missing studies. Eligibility criteria included randomized trials and randomized controlled trials that assessed the effect of exercise in patients with cardiovascular disease. Appraisal of studies and avoidance of bias was based on the Cochrane Handbook for Systematic Reviews of Interventions (Table 1)[18]. The criteria for evaluating the methodological quality of the studies are presented in Table 1 and were assessed as high risk (–), low risk (+), and undetermined risk (?).
Table 1.
Criteria for evaluating the methodological quality of the research studies[17].
| Criterion | Assessment |
|---|---|
| Random sequence generation | +/–/? |
| Allocation concealment | +/–/? |
| Blinding of the research | +/–/? |
| Blinding of the participants | +/–/? |
| Blinding of the outcome assessment | +/–/? |
| Selective reporting | +/–/? |
| Incomplete outcome data | +/–/? |
| Other potential threats | +/–/? |
+ = low risk, – = high risk, ? = unspecified risk.
The overall quality assessment of each study resulted from an evaluation of the individual elements summarized in Table 1 based on the procedures recommended by Cochrane. Based on the scoring criteria in Table 1, a study was scored as good when all eight criteria were classified as low risk (+) and adequate when one criterion was ranked as high risk (–) or if two criteria were of undetermined risk (?) and, at the same time, these criteria did not affect the outcome of the results. Subsequently, a study was classified as bad if two or more criteria were of high risk (–) or indeterminate quality (?) and if the study had one high-risk criterion (–) or two indeterminate risks (?). Outcome measures used to report BFRT effectiveness included strength adaptations and hypertrophy, cardiovascular responses and inflammatory markers. Each study was individually assessed for its qualitative and quantitative elements, and data for reviews, interventions, and intervention outcomes were recorded. Figure 1 summarizes in a flow chart the results of the overall search strategy.
Figure 1.
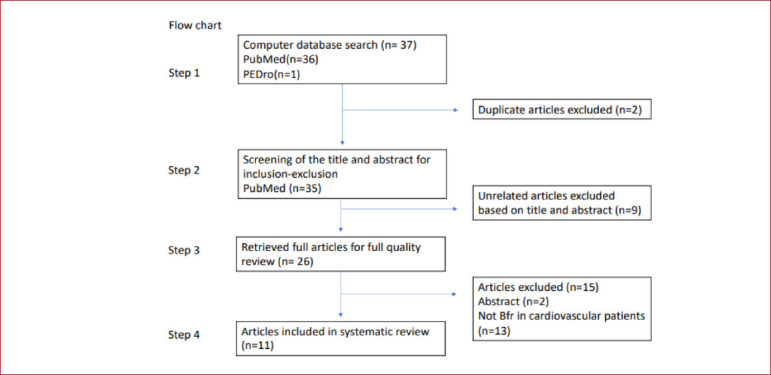
Study flow chart.
Results
Evaluation of the databases yielded 37 relevant studies (Figure 1) and no review that examined the effect of exercise with BFR in cardiovascular patients. Abstracts of specific studies were carefully assessed to confirm their relevance to the scope of the scoping review, and articles appearing in more than one database were removed. Thus, after the systematic evaluation and exclusion process (Figure 1), eleven articles that examined the effects of BFR training as a therapeutic modality in cardiovascular patients were included in the scoping review[21-31].
Characteristics of the Included Studies
All studies included in the review due to meeting the inclusion criteria are presented in Table 2.
Table 2.
Characteristics of the included studies.
| Study | Type of study | Clinical status | Sex | Age | Intervention (modality & protocol) | Intervention duration | Exercise frequency | Vascular occlusion method | Outcome measures | Outcomes results | Adverse effects |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kampic et al., 2021[30] | RCT | CAD | 18 ♂; 6 ♀ | 60 ± 2 years | IG:BFR RT with AT CG: usual care AT | 8 wks | 2 exercise sessions/week | Cuff inflation 15 - 20 mmHg>resting BSP | Leg extension muscle strength; biomarkers assessment | IG: :↑ muscle strength ↑SBP | No |
| Ogawa et al., 2021[27] | RCT | Post cardiac surgery | 3 ;♀ 18 ♂ | 69.6 ± 12.6 years | IG: KAATSU (knee ext, flx with BFR), AT; CG:usual care, AT | 12 wks | 2 times/week | Cuff pressure was first set at 100 mmHg at a mounting pressure of 20 mmHg and was gradually increased to 160–200 mmHg | Body composition; MTH; Blood biochemistry; MVIC Walking speed; HGS; knee strength | IG:↑ muscle strength, muscle size. physical function | No |
| Kambic et al., 2019[23] | RCT | CAD | 18 ♂; 6 ♀ | 60±2 y | IG: BFR RT CG:usual care (AT) | 8 wks | 2 exercise sessions/week | Cuff inflation 15 - 20mmHg>resting BSP | Leg extension muscle strength; VL muscle thickness; FMD | IG:↑ muscle strength; ↓ SBP; ↑ HR; tend toward improvement FMD | No |
| Ishizaka et al., 2019[24] | Quasi-experimental design | 1 ♀; 6 ♂ | 48±23 | Leg extension in four conditions: at 10% and 20% intensities with and without BFR | 1 day | 1 session | Pressure to 180 mmHg for BFR in the lower limbs | EMG rectus femoris, vastus lateralis, vastus medialis | At 10% intensity, BFR increased EMG of all muscles | No | |
| Groennebaek et al., 2019[31] | RCT | CHF | 36♂ | IG: BFR 66.7±7, RIC:62±9; CG:63±10 | IG: BFR RT or RIC CG: no intervention | 8 wks | 3 times/week | Proximal portion of the thighs and inflating them to 50% of individually determined arterial occlusion pressures | Blood sampling, muscle biopsies,6-MWT,maximal isometric strength, dynamic knee-extensor strength, local muscular strength-endurance capacity, MLHFQ | BFR RT, but not RIC, improves functional capacity, quality of life, and muscle mitochondrial function | No |
| Tanaka and Takarada, 2018 [26] | RCT | CHF | 30 ♂ | 60.7 ± 11.1 | IG: BFR with cycle ergometer CG: Exercise on a cycle ergometer | 6 months | 3 times/week | 208.7 ± 7.4 mmHg | Cardiopulmonary exercise testing,; blood chemistry; thigh circumference | IG: Peak VO2/W, improve exercise capacity & serum BNP levels | No |
| Barili et al., 2018 [29] | Experimental design | HA | 16 ♀ | 67.2 ± 3.7 | IG: HIAE, low intensity aerobic exercise LIAE & LIAE + BFR | 4 wks | 1 session | 130% of SBP | Blood analysis rest, post-exercise and after 30 minutes recovery | SOD: ↑ GST:↑ NPSH levels:↓ | No |
| Cezar et al., 2016[22] | RCT | HA | 23 ♀ | 63.75 ± 11.58 | IG1: Wrist flexion with BFR; IG2: low intensity wrist flexion exercise training alone; CG: no structured physical exercise program | 8 wks | 2 sessions/week | 70% of SBP | Hemodynamic; biochemical responses | BFR:↓ blood pressure, mean arterial pressure | No |
| Madarame et al., 2013[25] | Experimental design | Ischemic heart disease | 2 ♀ | 57±6 | IG: Knee extension with or without BFR CG: Knee extension without BFR | 3 wks | 1 session/week | Pressure of 200 mmHg by 50 mm width elastic cuffs | Noradrenaline; D-dimer FDP; hsCRP | No significant changes in markers of hemostasis & inflammation; IG:↑ heart rate & plasma noradrenaline concentration | No |
| Fukuda et al., 2013[21] | Experimental design | Cardiovascular diseases; (5 old myocardial infarction, 1 dilated cardiomyopathy | 6 ♂ | 69±12 | IG:Biceps flexion exercise with or without BFR; CG: Biceps flexion exercise without BFR | 1 day | 1 session | kaatsu belt inflated to 110-160 mmHg on the proximal region of both arms | Electromyography; Perceived exertion | IG: Significant EMG muscle activation, ↑RPE | No |
| Nakajima et al., 2010[28] | Experimental design | Ischemic heart disease | 7 ♂ | 52±4 | IG:Leg resistance exercises (leg press, leg extension, leg curl) with BFR | 12 wks | 2 sessions/week | Pressure of 100 mmHg & gradually to 160-250 mmHg | CSA; 1-RM voluntary force and VO2; blood sampling;hormonal analyses | IG:↑ muscle strength, mass, and endurance capacity | No |
CAD: Coronary artery disease; CHF: Chronic heart failure; AT: Aerobic training; RT: Resistance training; SBP: systolic blood pressure; BSP:Brachial systolic pressure; VL: vastus lateralis; FMD:flow mediated dilatation; KAATSU RT = low-intensity resistance training with moderate blood flow restriction, MTH = muscle thickness of thigh, MVIC = maximum voluntary isometric contraction, BFR = blood flow restriction, EMG = electromyographic activity, FDP = fibrinogen/fibrin degradation products, hsCRP = high-sensitivity C-reactive protein; BNP: brain natriuretic peptide; HGS:Hand Grip Strength; HIAE:High intensity aerobic exercise; LIAE: Low intensity aerobic exercise; RPE: Ratings of perceived exertion ;CSA: muscle cross/ sectional area; HA:hypertension; ); 6-MWT: 6-minute walk test, MLHFQ: the Minnesota Living with Heart Failure Questionnaire; RIC: remote ischemic conditioning; ♂:male; ♀:female
Trials
Six of the studies were randomized control trials[22,23,26,27,30,31], while the remaining five studies[21,23,25,28,29] included only intervention groups. The studies presented methodological similarities and differences that, as expected, probably affected the results of the studies. The dominant similarity among the studies was that the groups (intervention and control) showed no differences at baseline. The number of participants ranged from only six participants in the study by Fukuda et al.[21] to 36 in that by Groennebaek, et al.[31]. The overall number of male participants was higher than that of females, albeit without a significant difference (overall: 128 males, 51 females). A significant difference was observed in the duration of the interventions, which generally ranged from three weeks[25] to six months[26], although two of the studies were completed in a single day[21,24]. In only four studies, a re-evaluation of patients was carried out. Specifically, patients were reassessed at eight weeks in three studies[23,30,31] and three months in another[27]. The patients were evaluated only before and after the therapeutic applications in the remaining seven studies.
Of the studies analyzed, two examined hypertensive patients[22,29] and two were associated with patients with ischemic heart disease[25,28]. In two studies, the sample consisted of postoperative cardiovascular patients[24,27], while one study examined patients with coronary heart disease[23], one evaluated patient with chronic heart failure[26], one was performed in cardiovascular patients[21], and one evaluated patient with congestive heart failure[31].
Interventions
Cezar et al.[22] reported that eight weeks of wrist flexion exercise at 30% of one repetition maximum with BFR (70% of resting systolic blood pressure) could lower blood pressure in hypertensive patients receiving medication. In this study, twenty-three women were randomly divided into three subgroups. The two intervention subgroups performed three sets of wrist flexion exercises with or without BFR twice a week for eight weeks. The control group did not participate in any exercise program. Before each exercise session, blood pressure was evaluated at rest, and the result was an indicator for adapting the restriction in the BFR group. The restriction was set at 70% of the systolic blood pressure at rest for each participant and was maintained from the beginning of the training session until the last series of exercises.
Barili et al.[29] evaluated the immediate effects of low-intensity aerobic exercise with BFR on specific parameters of the cardiorespiratory system in hypertensive patients. Sixteen women aged 60–75 performed three therapeutic exercise protocols. The first protocol involved high-intensity aerobic exercise at 50% of estimated oxygen consumption, the second involved low-intensity aerobic exercise at 30% of estimated oxygen consumption, and the third involved low-intensity aerobic exercise with BFR. Blood samples were collected from the patients at rest, immediately after the completion of each training program, and after 30 minutes of recovery.
Madarame et al.[25] evaluated the hemostatic and inflammatory adaptations from the application of BFR in nine patients with ischemic heart disease. Patients participated in an exercise program in which they performed four sets of bilateral knee extension at 20% one-repetition maximum loading with BFR (4 patients) or without (5 patients). The exercise consisted of one set of 30 repetitions and three sets of 15 repetitions. Participants were instructed to hold the concentric phase for one second and the eccentric phase for one second. BFR was maintained throughout the exercise, including rest periods between sets, and released immediately after completion. Blood samples were collected before, immediately after, and one hour after training.
In the same context, Kambic et al.[23] examined the safety and efficacy of resistance exercise with BFR in patients with coronary heart disease, compared with conventional rehabilitation. Twenty-four patients were equally divided into two groups: an intervention group (BFR) and a control group. The participants in the intervention group followed an eight-week strength training program, performing a total of 16 unilateral leg extension exercise sessions twice per week, with a 48-hour rest period in between. Each training session consisted of 9, 10, and 12 repetitions in the first, second, and third sets, respectively, with 45 seconds of rest between sets. The training load was set at 30% of one repetition maximum and increased every two weeks, reaching 40% of one repetition maximum in the seventh week. The participants were guided to perform the exercise with one second in the concentric phase and two seconds in the eccentric phase. This BFR was maintained throughout the session, and the cuff was inflated between 15 and 20 mmHg greater than the resting brachial systolic pressure. Furthermore Kambic et al.[30] reproductive the protocol of their previous study (2019) and examined the acute and training induced effects of BFR-RT on hemostatic and hemodynamic responses in patients with coronary artery disease (CAD).
Ishizaka et al. examined the muscular activation of the quadriceps during the eccentric and concentric phases of knee extension[24]. The sample consisted of seven patients with cardiovascular disorders who performed the exercise under four conditions: with loads of 10% and 20% of one maximum repetition with and without BFR each time. They performed three sets of 30 bilateral repetitions with 30 seconds of rest in between. Between the different conditions, the rest period was five minutes. The occlusion was adjusted to 190 mmHg, and the cuff was inflated between sets and removed after the completion of each exercise condition.
Ogawa et al.[27] evaluated the results and safety of low-intensity exercise with BFR in muscle indices (muscle strength and mass) in cardiovascular patients’ post-surgery. Twenty men were randomly assigned to the control and resistance exercise groups with BFR. All subjects participated in an aerobic rehabilitation program, but the BFR group also performed knee strengthening and leg press exercises with BFR twice a week for three months. The participants were instructed in 1.5-second concentric and eccentric phases. Patients began exercising at a very low intensity and volume, gradually increasing to three sets of 30 repetitions per exercise with 30 seconds of rest between sets. After the second week, the one-repetition maximum was estimated, and the intensity of the exercise was adjusted to 20–30% of the one repetition maximum.
Nakajima et al.[28] found improvement in muscle strength and endurance in cardiovascular patients after a low-intensity BFR program performed twice a week for three months. The study sample consisted of seven male patients with ischemic heart disease who performed leg presses, leg extensions, and leg curls. Each exercise consisted of four sets: the first of 30 repetitions and the following 3 of 15 repetitions. The patients were instructed to follow concentric and eccentric phases for 1.5 seconds. The load was adjusted to 20–30% of one repetition maximum.
Fukuda et al.[21] examined the effects of BFR with low-intensity resistance exercise on muscle activation in cardiovascular patients. Six patients performed bicep flexion exercises with BFR. The exercise session consisted of 30 repetitions followed by three sets of 15 repetitions, with rest periods of 30 seconds between sets. The exercise duration was 2.4 seconds and included 1.2-second concentric and eccentric phases.
Tanaka and Takarada[26] evaluated the impact of aerobic exercise training on vascular occlusion in patients with chronic heart failure. In this study, thirty patients with heart failure (post-infarction) randomly participated in an aerobic training program performed on a cycle ergometer with and without the application of BFR at an intensity of 40–70% of the max VO2/W for 15 minutes three times a week for six months. Each training session began with a five-minute warm-up period, followed by adjusting the cycle ergometer resistance for everyone.
Groennebaek et al.[31], evaluated the effects of blood flow restriction with or without low-load exercise, conducted as blood flow restricted low load resistance exercise and remote ischemic conditioning, in functional capacity and quality of life in patients with congestive heart failure, who are not able to perform medium to high load resistance exercise. In this study, thirty-six patients aged 18 to 80 years, with left ventricular ejection fraction ≤ 45%, and New York Heart Association (NYHA) functional class I to III were recruited. The study was conducted in a 8-week period. Specifically, the intervention program was completed in 6 weeks and pretests were performed 1 week before the 6-week intervention, and post tests were performed 3 days after the 6-week intervention. The 6-week intervention included three sessions per week (Monday, Wednesday, and Friday) with blood flow restricted low load resistance exercise (participants performed 4 sets of bilateral knee-extensions at 30% of 1-RM) or remote ischemic conditioning (4 cycles of 5 min upper arm ischemia followed by 5 min of reperfusion), depends on the group, and at the control group the participants received al the test but they did not receive any kind of intervention. During the whole intervention period participants were instructed to continue their habitual lifestyle and physical activity level. In this study, conducted assessments regarding muscle biopsies, functional capacity, and quality of life assessments. The group that followed the blood flow restriction low resistance exercise showed that improved 6-minute walk test, increased maximum isometric strength, improved quality of life and increased mitochondrial function compared with control.
Risk of Bias
The quality assessment of the studies in the review was based on criteria for assessing the risk of bias. This rating ranged from five to six, with a maximum of eight, where a lower score indicated a higher risk of error. All studies included in the review were randomized or clinical trials (Table 3). Although the outcome assessors of the studies were blinded, the principal investigators could not be blinded. Based on the above quality review methods, the final assessment resulted in six studies of adequate quality[21,23,26,27,30,31] and five of poor quality[21,24,25,28,29].
Table 3.
Study evaluation based on the Cochrane Risk of Bias tool.
| Criteria | Studies | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ogawa et al., 2021[27] | Ishizaka et al., 2019[24] | Cezar et al., 2016[22] | Madarame et al., 2013[25] | Fukuda et al., 2013[21] | Kambic et al., 2019[23] | Kambic et al., 2021[30] | Nakajima et al., 2010[28] | Barili et al., 2018[29] | Tanaka and Takarada, 2018[26] | Groennebaek et al., 2019[31] | |
| Sequence Generation | + | + | + | + | + | + | + | + | + | + | + |
| Allocation Concealment | + | - | + | - | - | + | + | - | - | + | + |
| Blinding Of The Research | - | - | - | - | - | - | - | - | - | - | - |
| Blinding Of The Participants | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? |
| Blinding Of The Outcome Assessment | + | + | + | + | + | + | + | + | + | + | + |
| Selective Reporting | + | + | + | + | + | + | + | + | + | + | + |
| Incomplete Outcome Data | + | + | + | + | + | + | + | + | + | + | + |
| Other Potential Threats | + | + | + | + | + | + | + | + | + | + | + |
| Final Evaluation | Sufficient quality | Poor quality | Sufficient quality | Poor quality | Poor quality | Sufficient quality | Sufficient quality | Poor quality | Poor quality | Sufficient quality | Sufficient quality |
Study Findings
The review showed increased muscle strength, muscle mass improvement, and functionality after BFR training in cardiovascular patients (Table 2). Ogawa et al.[27] reported the positive effects of low-load BFR training for the reduction of cardiac surgery–induced loss in muscle mass and functionality, as opposed to the standard cardiac rehabilitation program, which appeared to be insufficient to restore functionality in such patients. Ishizaka et al.[24] and Fukuda et al.[21] both reported significant muscle activation after low-load exercises combined with blood flow restriction, which was recorded via electromyography (EMG) in cardiovascular patients. Cezar et al.[22] reported that low-load strength training with vascular occlusion for eight weeks performed twice a week can decrease systolic and diastolic blood pressure and mean arterial pressure in hypertensive women. Kambic et al.[23] arrived at the same conclusions regarding a decrease in systolic blood pressure following BFR training with low-load resistance in patients with coronary artery disease (CAD). The above findings indicate that low load resistance exercise with vascular occlusion may be a safe option for the prevention and treatment of hypertension in hypertensive patients and for improving blood pressure in CAD patients. Apart from the positive results in blood pressure, Kambic et al.[23] highlighted the significant muscle strength and functionality improvement in CAD patients who followed BFR resistance training. In their research, Madarame et al.[25] analyzed the effect of BFR low-load resistance exercise on hemostatic and inflammatory responses in patients with ischemic heart disease (IHD). Their results showed that this type of exercise does not affect exercise-induced hemostatic and inflammatory responses in stable IHD patients; thus, it can be prescribed as a safe training method. Nakajima et al.[28] showed that three-month low-intensity vascular occlusion resistance exercises can induce muscle hypertrophy and strength and increase aerobic capacity in IHD patients. Furthermore, Barili et al.[29] and Yasushi et al.[26] highlighted the benefits of aerobic exercise combined with blood flow restriction training. The first study reported low-intensity aerobic exercise with BFR to be safe and valuable in terms of muscle gains training method, and the second study suggested that BFR aerobic exercise training can enhance exercise capacity in patients with chronic heart failure. Finally, Groennebaek et al.[31], showed that blood flow restriction low load resistance exercise, in patients with congestive heart failure, enhance functional capacity, self-reported quality of life, and stimulate increases in skeletal muscle mitochondrial respiratory function and ribosomal biogenesis.
Discussion
The application of BFR in combination with specific types of exercise has recently become quite popular in the field of rehabilitation and gathered considerable research interest. In particular, although it started as a means of further enhancing muscle strength in healthy athletes, blood flow restriction training has over the last two decades become a popular therapeutic technique in different groups of patients with significant functional deficits and painful musculoskeletal conditions. The rationale for implementing BFR exercise as a musculoskeletal rehabilitation tool is based on the fact that it is a safe exercise method in clinical settings. Furthermore, it can lead to muscle hypertrophy and increased muscle strength with low to moderate intensity training through improved anabolic processes mediated by BFR. BFR limits arterial and venous blood flow and leads to the pooling of blood, which can increase the effects of exercise-induced training. Impressively, strength training at lower intensities (20–40% of maximal strength) combined with BFR led to a similar improvement in variables such as muscle hypertrophy, muscle strength, and cardiovascular fitness in athletes and non-athletes as exercising at 70% strength level without BFR[13-15].
Patients with cardiovascular disease often exhibit low levels of function, muscle mass, and muscle strength[11]. Therefore, the above negative functional adaptations are the target of cardiovascular rehabilitation programs that, by restraining the reduction of muscle mass and strength and increasing cardiopulmonary function, aim to improve the quality of life of these patients. Aerobic exercise is essential for cardiovascular rehabilitation, especially after major cardiac surgery. However, it is common for cardiovascular patients to be unable to participate in even low-intensity aerobic exercise programs, mainly due to the muscle atrophy and general weakness accompanying such pathologies. These functional deficits are significant barriers to the gradual recovery of muscle strength and function in these patients, given that the American College of Sports Medicine (ACSM) states that training loads of at least >75% of 1-RM are required for optimal improvements in muscle hypertrophy and strength in healthy adults[32]. Under these conditions, a type of exercise that would have the effectiveness of high-resistance exercises but utilizes submaximal intensity, such as BFR, could be prescribed to cardiac patients after its effects and the safety of its application had first been investigated and documented.
The results of the present review support the above view that BFR training with low-level intensity can restrain the loss of muscle mass and improve muscle hypertrophy strength and cardiovascular endurance in cardiovascular patients. The above findings agree with the existing literature regarding the general benefits of BFR training in muscle strength and hypertrophy. Loenneke et al.[33] published a meta-analysis of 11 studies comparing BFR exercise to low-intensity training and found relative improvements in muscle strength and hypertrophy compared with control groups. The same results were highlighted by Centner et al.[34] in their systematic review and meta-analysis of the effects of BFR training on muscular strength and hypertrophy in older individuals. They reported low-load BFR and walking with BFR to be effective interventions for muscle hypertrophy and strength gains in older populations. Similarly, BFR exercises have been reported to be especially promising in recovering injured and postoperative patients. Takarada et al.[35] reported that after anterior cruciate ligament (ACL) reconstruction, BFRT alone, without resistance training, decreased muscle atrophy postoperatively.
Nevertheless, the findings of the present review should be evaluated under the weight of their methodological deficits and limitations.
First, most studies in this scoping review were at moderate or high risk of bias. Therefore, its findings should be confirmed, ideally using larger sample sizes, randomization of participants, and extended follow-up durations. Additionally, the surveys included in the review were limited (only nine), and most were not randomized. The number of participants also varied considerably, with Fukuda et al.[21] including only six participants, while Tanaka and Takarada[26] evaluated 30 patients. In addition, significant differentiations were observed in the interventions’ duration and patients’ pathologies. Durations ranged from one session[21,24] to three months[27,28]. Of the studies analyzed, two examined hypertensive patients[22,29], while two dealt with patients with ischemic heart disease[25,28]. In two studies, the sample consisted of postoperative cardiovascular patients[24,27], two studies examined patients with coronary artery disease[23,30], and one was conducted on cardiovascular patients (no surgery was reported)[21]. One study evaluated the impact of aerobic exercise training on vascular occlusion in patients with chronic heart failure[26], and one other assessed the effect of blood flow restriction with or without low load resistance exercise in patients with congestive heart failure[31].
However, regardless of the reported benefits of BFR training, the safety of its use is often questioned, mainly when it is applied to patients. In support of BFR safety, a Japanese national survey reported that the most common adverse effects of BFR training, such as subcutaneous hemorrhage, sensory paresthesia (1.3%), and lightheadedness, are temporary[36]. In addition, concerns exist regarding safety and adverse events (e.g., numbness, nausea, hypertension, headache, fainting, tingling, excessive pain, central retinal vein occlusion, rhabdomyolysis) during and following exercise, particularly for those with comorbidities[37]. For example, patient’s chronic kidney disease (CKD) exhibits an elevated cardiovascular risk manifesting as coronary artery disease, heart failure etc[38]. BFR training displays similar positive health benefits to exercise training but potential implications should be considered by clinicians and researchers.
Another potential concern by cardiologists is BFR exercise’s effect on the exercise pressor reflex. The excessive restriction could lead to the overactivation of muscle reflexes and/or central command, with consequent development of sympathetic hyperreactivity and increased risk for cardiovascular-related adverse events. The existing data on the short- or long-term effects of BFR exercise’s impact on the exercise pressor reflex is still insufficient.
Overall, the risk associated with BFRT appears to be less than that associated with traditional high-load resistance exercise. The results of this review similarly suggest the same conclusion, underscoring that BFR training is not only a safe exercise method for cardiovascular patients but also can act positively in hypertensive patients by reducing blood pressure. However, long-term studies on its effects on the cardiovascular system are needed. The optimal duration and intensity of pressure cuff–induced skeletal muscle blood flow restriction to provide BFR exercise properly and safely, especially in cardiovascular patients, needs to be evaluated with better and well-designed studies.
Cezar et al.[22] and Kambič et al.[23] showed low-intensity resistance exercise with BFR low-load exercise to be safe for cardiovascular patients and reduce blood pressure. Similarly, Madarame et al.[25] suggested no significant changes in markers of hemostasis and inflammation in patients with ischemic heart disease after low-load BFR resistance training, supporting that BFR exercise could be a safe training method for those patients.
Barili et al.[29] and Yasushi et al.[26] reported that aerobic exercise combined with BFR training has positive results in a hypertensive population of patients with chronic heart failure in terms of cardiorespiratory function and improvement of exercise capacity.
Furthermore, both the studies of Ishizaka et al.[24] and Fukuda et al.[21], which were recorded via EMG in cardiovascular patients, reported significant muscle activation after low-load exercises combined with BFR, underscoring the strengthening and hypertrophic effects of exercise on skeletal muscles. Ogawa et al.[27] showed that low-intensity resistance exercise with limited blood flow increases muscle strength and mass in cardiovascular patients who have undergone surgery. Nakajima et al.[28] showed that muscle strength and endurance in cardiovascular patients improved after a three-month low-intensity BFR program, while at the same line Groennebaek et al.[31], underlined that a six week blood flow restriction low load exercise program improved functional capacity, self-reported quality of life and stimulating increases in skeletal muscle mitochondrial respiratory function and ribosomal biogenesis in patients with congestive heart failure, and showed that blood flow restriction low load exercise could be an innovative method at the rehabilitation process in such a patients group.
Although BFR exercise appears to have positive benefits on skeletal muscle function, it is important to recognize possible contraindications that should be considered with respect to vascular health (e.g. coronary artery disease, unstable hypertension, postsurgical excess swelling, medications known to increase blood clotting risk)[39,40]. Therefore, proper screening prior to BFR exercise is required to reduce the risk of complications[40,41]. Future studies should report and discuss any associated side-effects to improve our understanding with respect to the safety of BFR exercise method[37].
Conclusions
This review aimed to evaluate the effects of mild-intensity blood flow restriction exercise in patients with cardiac diseases. Unfortunately, very few studies are available in this area, and most are of moderate quality. From these studies, current evidence suggests that BFR combined with low-load exercises can improve muscle strength, cardiovascular endurance, and functionality in patients with heart disease without requiring high-intensity training. Future studies are needed to determine appropriate indications for prescriptions in cardiovascular patients by extending the follow-up periods, enrolling larger sample sizes, and using specific BFR exercise protocols for these patients.
Footnotes
Edited by: Jagadish K. Chhetri
References
- 1.World Health Organization. World Health Statistics 2012. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 2.World Health Organization. Global health risks:mortality and burden of disease attributable to selected major risks. World Health Organization; 2009. [Google Scholar]
- 3.Timmis A, Townsend N, Gale CP, et al. European Society of Cardiology:Cardiovascular Disease Statistics 2019 [published correction appears in Eur Heart J 2020 Dec 14;41(47):4507] Eur Heart J. 2020;41(1):12–85. doi: 10.1093/eurheartj/ehz859. [DOI] [PubMed] [Google Scholar]
- 4.Thiriet M. Cardiovascular Disease:An Introduction. Vasculopathies. 2019;8:1–90. [Google Scholar]
- 5.Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult:a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure):developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation:endorsed by the Heart Rhythm Society. Circulation. 2005;112(12):e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 6.McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012:The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787–847. doi: 10.1093/eurheartj/ehs104. [DOI] [PubMed] [Google Scholar]
- 7.Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) [published correction appears in Eur Heart J 2012 Sep;33(17):2126] Eur Heart J. 2012;33(13):1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 8.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2010 (GBD 2010) Results by Cause 1990-2010. Seattle, United States of America: Institute for Health Metrics and Evaluation (IHME); 2012. [Google Scholar]
- 9.Joyner MJ, Green DJ. Exercise protects the cardiovascular system:effects beyond traditional risk factors. J Physiol. 2009;587(Pt 23):5551–5558. doi: 10.1113/jphysiol.2009.179432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green DJ, O'Driscoll G, Joyner MJ, Cable NT. Exercise and cardiovascular risk reduction:time to update the rationale for exercise? J Appl Physiol. 2008;105:766–768. doi: 10.1152/japplphysiol.01028.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas DR. Loss of skeletal muscle mass in aging:examining the relationship of starvation, sarcopenia and cachexia. Clin Nutr. 2007;26(4):389–399. doi: 10.1016/j.clnu.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Bittar ST, Pfeiffer PS, Santos HH, Cirilo-Sousa MS. Effects of blood flow restriction exercises on bone metabolism:a systematic review [published online ahead of print, 2018 Mar 2] Clin Physiol Funct Imaging. 2018 doi: 10.1111/cpf.12512. 10.1111/cpf.12512. [DOI] [PubMed] [Google Scholar]
- 13.Lixandrão ME, Ugrinowitsch C, Berton R, et al. Magnitude of Muscle Strength and Mass Adaptations Between High-Load Resistance Training Versus Low-Load Resistance Training Associated with Blood-Flow Restriction:A Systematic Review and Meta-Analysis. Sports Med. 2018;48(2):361–378. doi: 10.1007/s40279-017-0795-y. [DOI] [PubMed] [Google Scholar]
- 14.Abe T, Sakamaki M, Fujita S, et al. Effects of low-intensity walk training with restricted leg blood flow on muscle strength and aerobic capacity in older adults. J Geriatr Phys Ther. 2010;33(1):34–40. [PubMed] [Google Scholar]
- 15.Loenneke, Jeremy Paul BS, Pujol, Thomas Joseph EdD, CSCS. The Use of Occlusion Training to Produce Muscle Hypertrophy. Strength and Conditioning Journal June. 2009;31(3):77–84. [Google Scholar]
- 16.Williams, Mark A, et al. Resistance exercise in individuals with and without cardiovascular disease:2007 update:a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116(5):572–584. doi: 10.1161/CIRCULATIONAHA.107.185214. [DOI] [PubMed] [Google Scholar]
- 17.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015:elaboration and explanation [published correction appears in BMJ 2016 Jul 21;354:i4086] BMJ. 2015;350:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 18.Higgins, Julian PT, et al., editors. Cochrane handbook for systematic reviews of interventions. John Wiley &Sons. 2019 [Google Scholar]
- 19.Dickersin K, Manheimer E, Wieland S, Robinson KA, Lefebvre C, McDonald S. Development of the Cochrane Collaboration's CENTRAL Register of controlled clinical trials. Eval Health Prof. 2002;25(1):38–64. doi: 10.1177/016327870202500104. [DOI] [PubMed] [Google Scholar]
- 20.Michaleff ZA, Costa LO, Moseley AM, et al. CENTRAL, PEDro, PubMed, and EMBASE are the most comprehensive databases indexing randomized controlled trials of physical therapy interventions. Phys Ther. 2011;91(2):190–197. doi: 10.2522/ptj.20100116. [DOI] [PubMed] [Google Scholar]
- 21.Fukuda T, Yasuda T, Fukumura K, et al. Low-intensity kaatsu resistance exercises using an elastic band enhance muscle activation in patients with cardiovascular diseases. International Journal of KAATSU Training Research. 2013;9(1):1–5. [Google Scholar]
- 22.Cezar MA, De SáCA, Corralo VDS, et al. Effects of exercise training with blood flow restriction on blood pressure in medicated hypertensive patients. Motriz:Revista de Educação Física. 2016;2:9–17. [Google Scholar]
- 23.Kambič T, Novaković M, Tomažin K, et al. Blood Flow Restriction Resistance Exercise Improves Muscle Strength and Hemodynamics, but Not Vascular Function in Coronary Artery Disease Patients:A Pilot Randomized Controlled Trial. Front Physiol. 2019;10:656. doi: 10.3389/fphys.2019.00656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishizaka H, Uematsu A, Mizushima Y, et al. Blood Flow Restriction Increases the Neural Activation of the Knee Extensors During Very Low-Intensity Leg Extension Exercise in Cardiovascular Patients:A Pilot Study. J Clin Med. 2019;8(8):1252. doi: 10.3390/jcm8081252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Madarame H, Kurano M, Fukumura K, et al. Haemostatic and inflammatory responses to blood flow-restricted exercise in patients with ischaemic heart disease:a pilot study. Clin Physiol Funct Imaging. 2013;33(1):11–17. doi: 10.1111/j.1475-097X.2012.01158.x. [DOI] [PubMed] [Google Scholar]
- 26.Tanaka Y, Takarada Y. The impact of aerobic exercise training with vascular occlusion in patients with chronic heart failure. ESC Heart Fail. 2018;5(4):586–591. doi: 10.1002/ehf2.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogawa H, Nakajima T, Shibasaki I, et al. Low-Intensity Resistance Training with Moderate Blood Flow Restriction Appears Safe and Increases Skeletal Muscle Strength and Size in Cardiovascular Surgery Patients:A Pilot Study. J Clin Med. 2021;10(3):547. doi: 10.3390/jcm10030547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakajima T, Kurano M, Sakagami F, Iida H, Fukumura K, Fukuda T, et al. Effects of low-intensity KAATSU resistance training on skeletal muscle size/strength and endurance capacity in patients with ischemic heart disease. International journal of KAATSU training research. 2010;6(1):1–7. [Google Scholar]
- 29.Barili A, Corralo VDS, Cardoso AM, et al. Acute responses of hemodynamic and oxidative stress parameters to aerobic exercise with blood flow restriction in hypertensive elderly women. Mol Biol Rep. 2018;45(5):1099–1109. doi: 10.1007/s11033-018-4261-1. [DOI] [PubMed] [Google Scholar]
- 30.Kambic T, Novakovic M, Tomazin K, et al. Hemodynamic and hemostatic response to blood flow restriction resistance exercise in coronary artery disease:a pilot randomized controlled trial. J. Cardiovasc. Nurs. 2021;36:507–516. doi: 10.1097/JCN.0000000000000699. [DOI] [PubMed] [Google Scholar]
- 31.Groennebaek Thomas, et al. Effect of blood flow restricted resistance exercise and remote ischemic conditioning on functional capacity and myocellular adaptations in patients with heart failure. Circulation:Heart Failure. 2019;12(12):e006427. doi: 10.1161/CIRCHEARTFAILURE.119.006427. [DOI] [PubMed] [Google Scholar]
- 32.Wise FM, Patrick JM. Resistance exercise in cardiac rehabilitation. Clin Rehabil. 2011;25(12):1059–1065. doi: 10.1177/0269215511423408. [DOI] [PubMed] [Google Scholar]
- 33.Loenneke JP, Wilson JM, Marín PJ, Zourdos MC, Bemben MG. Low intensity blood flow restriction training:a meta-analysis. Eur J Appl Physiol. 2012;112(5):1849–1859. doi: 10.1007/s00421-011-2167-x. [DOI] [PubMed] [Google Scholar]
- 34.Centner C, Wiegel P, Gollhofer A, König D. Effects of Blood Flow Restriction Training on Muscular Strength and Hypertrophy in Older Individuals:A Systematic Review and Meta-Analysis [published correction appears in Sports Med 2018 Nov 9] Sports Med. 2019;49(1):95–108. doi: 10.1007/s40279-018-0994-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Takarada Y, Takazawa H, Ishii N. Applications of vascular occlusion diminish disuse atrophy of knee extensor muscles. Med Sci Sports Exerc. 2000;32(12):2035–2039. doi: 10.1097/00005768-200012000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Nakajima T, Kurano M, Iida H, Takano H, Oonuma H, Morita T, et al. Use and safety of KAATSU training:results of a national survey. International journal of KAATSU training research. 2006;2(1):5–13. [Google Scholar]
- 37.Rolnick N, de Sousa Neto IV, da Fonseca EF, Neves RVP, Rosa TDS, Nascimento DDC. Potential implications of blood flow restriction exercise on patients with chronic kidney disease:a brief review. J Exerc Rehabil. 2022;18(2):81–95. doi: 10.12965/jer.2244082.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular Disease in Chronic Kidney Disease:Pathophysiological Insights and Therapeutic Options. Circulation. 2021;143(11):1157–1172. doi: 10.1161/CIRCULATIONAHA.120.050686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nascimento DDC, Rolnick N, Neto IVS, Severin R, Beal FLR. A Useful Blood Flow Restriction Training Risk Stratification for Exercise and rehabilitation. Front Physiol. 2022;13:808622. doi: 10.3389/fphys.2022.808622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.da Cunha Nascimento D, Schoenfeld BJ, Prestes J. Potential Implications of Blood Flow Restriction Exercise on Vascular Health:A Brief Review. Sports Med. 2020;50(1):73–81. doi: 10.1007/s40279-019-01196-5. [DOI] [PubMed] [Google Scholar]
- 41.Kacin A, Rosenblatt B, Žargi TG, Biswas A. Safety considerations with blood flow restricted resistance training. Annales Kinesiologiae. 2015;6(1):3–26. [Google Scholar]


