Abstract
Objective
This work aims to guide clinicians practicing endocrinology in the use of telehealth (synchronous patient-clinician visits conducted over video or telephone) for outpatient care.
Participants
The Endocrine Society convened a 9-member panel of US endocrinologists with expertise in telehealth clinical care, telehealth operations, patient-centered care, health care delivery research, and/or evidence-based medicine.
Evidence
The panel conducted a literature search to identify studies published since 2000 about telehealth in endocrinology. One member extracted a list of factors affecting the quality of endocrine care via telehealth from the extant literature. The panel grouped these factors into 5 domains: clinical, patient, patient-clinician relationship, clinician, and health care setting and technology.
Consensus Process
For each domain, 2 or 3 members drew on existing literature and their expert opinions to draft a section examining the effect of the domain’s component factors on the appropriateness of telehealth use within endocrine practice. Appropriateness was evaluated in the context of the 6 Institute of Medicine aims for health care quality: patient-centeredness, equity, safety, effectiveness, timeliness, and efficiency. The panel held monthly virtual meetings to discuss and revise each domain. Two members wrote the remaining sections and integrated them with the domains to create the full policy perspective, which was reviewed and revised by all members.
Conclusions
Telehealth has become a common care modality within endocrinology. This policy perspective summarizes the factors determining telehealth appropriateness in various patient care scenarios. Strategies to increase the quality of telehealth care are offered. More research is needed to develop a robust evidence base for future guideline development.
Keywords: telehealth, telemedicine, consensus statement, guidelines, endocrinology, virtual care, policy perspective
Telehealth includes many types of medical care delivered remotely using telecommunications technology (1). In this policy perspective (herein referred to as “perspective”) the term telehealth refers to synchronous patient-clinician visits conducted over video or telephone for outpatient care. Endocrinology as a specialty lends itself well to telehealth because the diagnosis and management of many endocrine conditions rely primarily on patient-reported history, laboratory, and/or imaging results rather than physical examination findings. Before the COVID-19 pandemic telehealth was already being used in endocrinology, most frequently for diabetes care (2-4). At the outset of the pandemic, changes in reimbursement models and the recognition of home as an “originating site” of care enabled broader use (5). Endocrinology evolved into one of the subspecialties with the highest shares of visits conducted via telehealth (6), and endocrine and metabolic conditions are now among the most common conditions addressed across all telehealth visits (7). Benefits of telehealth have emerged compared to in-person care across health systems, and include higher visit completion rates (8) and a reduction in patients’ travel burden, with generally high patient (9-11) and clinician satisfaction (12, 13). At the same time, concerns have arisen about the equity, safety, and effectiveness of telehealth in different situations (14-16).
Telehealth will likely remain a common modality for endocrine care after conclusion of the current public health emergency (PHE). Thus, clinicians will need to decide whether it is appropriate to use telehealth outside a PHE for specific types and instances of endocrine care. Few empiric data are available to guide decisions about when to leverage telehealth or in-person encounters for endocrine outpatient care. This perspective aims to provide guidance on that topic by outlining how various domains of care—including clinical factors, patient factors, the patient-clinician relationship, clinician factors, and the health care setting—can influence the use of telehealth within endocrinology, and how this, in turn, can affect the overall quality of care provided. We also offer strategies to support high-quality endocrine care rendered via telehealth. Finally, we identify where future research is needed on quality of telehealth care in endocrinology.
Methods and Guiding Principles
The Endocrine Society convened a panel of 9 US academic endocrinologists with expertise in telehealth clinical care, telehealth operations, patient-centered care, health care delivery research, and/or evidence-based medicine to develop this perspective. As a first step, the panel conducted a literature search to identify literature about telehealth within endocrinology published since 2000. The panel chair (V.G.V.) extracted a list of factors suggested by this literature as potentially affecting the quality of endocrine care via telehealth. Separately, the panel generated a list of factors that based on their experiences may affect the quality of endocrine telehealth care. The chair synthesized the 2 lists and grouped the factors into 5 domains: clinical; patient; patient-clinician relationship; clinician; and health care setting and technology. These groupings were then reviewed and revised by all members. For each domain, 2 or 3 panel members used relevant literature and their experiences to draft a section describing how factors included in that domain affect the appropriateness of telehealth use within endocrinology. When particularly relevant, literature from specialties outside endocrinology was included. Each draft section was reviewed and revised by the group via monthly meetings. Two panel members (V.G.V. and S.S.C.) then wrote the remaining sections and integrated these with the domains to assemble the final draft, which was reviewed and revised by all members.
In evaluating how the domains and their component factors affect the appropriateness of endocrine telehealth care, the panel considered whether a telehealth visit could offer quality of care that was greater or comparable to that of an in-person visit, acknowledging that in some situations the quality of care offered by one visit modality may be superior to the other, while in other situations they may each support high-quality care. The Institute of Medicine (IOM) in 2001 defined high-quality health care as patient centered, equitable, safe, effective, timely, and efficient (17). The panel was guided by these 6 quality aims, further described later.
Where published evidence was available to support the panel's assertions, citations are provided; in all other instances, these assertions represent the expert opinions and perspectives of the panel. Panel members concluded after extensive discussion that no consensus could be reached about designating the value of telehealth or in-person visits for any specific endocrine condition due to the complexity of individual circumstances and the need for clinicians and patients together to weigh the relative importance of competing priorities across domains. Therefore, while this perspective provides guidance about the appropriateness of telehealth use in various scenarios, it does not designate endocrine diagnoses or patient populations that are always or never appropriate to engage via telehealth. We also acknowledge that many endocrine clinicians feel strongly about in-person care at certain intervals, but we do not recommend for or against specific minimum intervals for in-person care given the lack of evidence to support such an assertion and a lack of consensus on this topic.
Patient-centered Care
The IOM defines patient-centered care as “care that is respectful of and responsive to individual patient preferences, needs, and values and ensur(es) that patient values guide all clinical decisions” (17). Interventions to promote patient-centered care can improve clinician and patient satisfaction, encourage high levels of patient participation in care, and improve health outcomes (18, 19). In this perspective we consider the effect of telehealth on patient-centered care in 2 ways. First, we place a high value on patients’ ability to choose their care modality. If the patient prefers one care modality and clinical concerns can be feasibly, adequately, and safely addressed through that care modality, then patient preference should be weighted strongly. This applies equally for patients who prefer telehealth and for patients who prefer in-person care. Second, we consider ways in which telehealth can be a tool to support patients’ specific goals and priorities for their care. For example, telehealth can be used to facilitate supplemental health education or closer contact after medication changes, reduce a patient’s time spent away from work or dependents while receiving their own health care, and/or enable visits that include multiple care team members or key support individuals within the patient’s care encounters. In these ways and others, telehealth can promote patient-centered care.
Health Equity
The Endocrine Society is committed to reducing health disparities by addressing their root causes within our health care system (20). Telehealth has the potential to promote equity by increasing access to care for those facing travel, cost, mobility, mental health, work, or caregiver barriers to in-person visits. Yet emerging data suggest that telehealth visits are often less used or even inaccessible for people who are Black, Asian or other Pacific Islander, American Indian or Alaska Native, Hispanic or Latino, are of older age, have limited English proficiency or low digital or health literacy, or who have fewer socioeconomic resources (14, 21-24). In this perspective we consider how decisions about the modality of endocrinology care may either exacerbate or reduce disparities in health care access and outcomes.
We recognize the powerful influence of social determinants of health on well-being, including economic stability, educational access and quality, neighborhood and built environment, social and community context, and health care access and quality. Many of these conditions appear to present insurmountable barriers to achieving equitable care, but apparent barriers may at times be overcome by clinicians and their clinics adopting strategies that can increase access to care and promote health equity. These are listed among the strategies we propose to support high-quality endocrine telehealth care.
We also acknowledge that system-level changes are essential to ensuring health equity. Although these fall outside the direct influence of individual clinicians, we affirm the central importance of affordable, available broadband internet and mobile devices; websites and technology platforms that are culturally, language-, and literacy-appropriate as well as accessible to those with impaired vision or hearing; availability of patient training for telehealth literacy; and alignment of reimbursement policy with the aim of equity (15, 25). As telehealth becomes a fundamental part of health care delivery, equity concerns need to remain at the forefront of decisions by health care systems and policymakers so that this modality of care promotes the health of all people.
Safety and Effectiveness
The principle of “First, do no harm” guides medical decision-making, along with the imperative to provide care that is evidence based and delivered to all who could benefit. In this perspective we consider circumstances in which safety and effectiveness could be compromised by in-person care (eg, risks of infection, travel accidents, delays in care due to illness or other unforeseen factors) or by telehealth (eg, risks of missing key exam findings, inability to easily escalate to higher acuity care). We also consider how evidence-based practices in endocrinology can be delivered remotely or adapted for telehealth without a reduction in effectiveness, and how a longitudinal care plan involving both telehealth and in-person care can be crafted to optimize the safety and effectiveness of care for each individual patient. It is important to note that telehealth is always preferred if the alternative is no care, such as for patients who are immobile or live in geographic areas without access to endocrine clinicians.
While the volume of telehealth care has increased exponentially in the last 2 years, there are many unanswered questions about clinical outcomes. Where evidence is lacking, we draw on the panel's expert opinions and experiences, and conclude our perspective with a suggested agenda for future research.
Timeliness and Efficiency
The timeliness and efficiency of care inherently affect all other domains of quality including effectiveness, safety, patient-centeredness, and equity. In this perspective we explore ways in which telehealth can reduce harmful delays and wasted effort or resources in the delivery of endocrine care. This includes the use of telehealth to maintain scheduled visits despite mild patient illness, caregiving responsibilities or travel limitations for the patient or clinician; the potential for patients to engage with clinicians and other care team members remotely during times of geographic displacement (eg, college attendance); the use of telehealth to address clinician shortages in specific regions; and the potential to circumnavigate a scarcity of clinical space or staffing by moving from on-site to remote care. We also discuss circumstances in which telehealth care is less likely to be efficient, including situations where essential patient-generated health data (PGHD) cannot be accessed remotely or where in-person measurements or examination findings are likely to be critical to management decisions.
Domains of Care Affecting Appropriateness of Telehealth Use
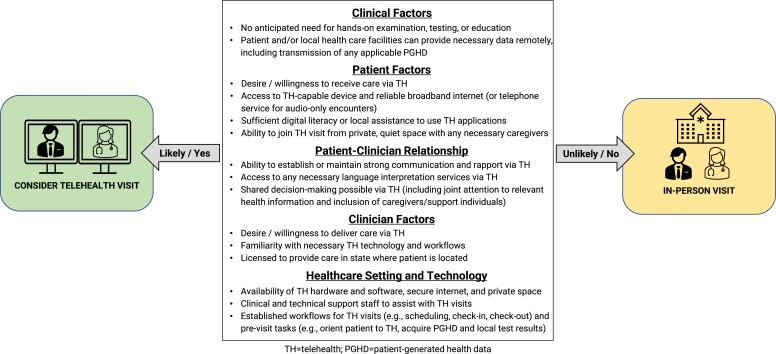
The panel identified 5 domains of care that affect the appropriateness of telehealth use within endocrinology: clinical factors; patient factors; patient-clinician relationship; clinician factors; and healthcare setting and technology. The interactions of these domains with telehealth as a care modality are described next. Circumstances within each domain that support the use of telehealth are summarized in Fig. 1, while Table 1 details strategies that are likely to improve the quality of telehealth care delivered by endocrine clinicians.
Figure 1.
Guide to appropriate use of telehealth visits for endocrine care.
Table 1.
Strategies to support high-quality endocrine care via telehealth
| Use a combination of in-person and telehealth care. |
|---|
| Complete required assessments or testing at sites close to patient's home when possible. |
| Allow multidisciplinary care team members to engage patient via different modalities as appropriate. |
| Mix telehealth and in-person visits as part of a longitudinal care plan via shared decision-making process. |
| Conclude each visit with careful consideration of optimal care modality for next encounter. |
| Anticipate and address patient needs related to telehealth. |
| Establish practice criteria for use of audio-only and video telehealth. |
| Allow patients the flexibility to change modality of scheduled visit if needed. |
| Proactively assess need for language interpretation services before telehealth encounters. |
| Clarify expectations with patient that telehealth will require a private, quiet, safe location for visit. |
| Facilitate previsit outreach by clinic support staff to assist with technology and sharing of pertinent patient-generated health data. |
| Engage caregivers to participate in visits and/or support patient's use of necessary technology. |
| Develop personal best practices and skills specific to telehealth. |
| Ensure private, quiet space from which to deliver care, with adequate and secure broadband access. |
| Strengthen relationships over telehealth through building skills in remote engagement and trust-building. |
| Become familiar with telehealth hardware, software, clinical workflows, and licensing requirements. |
| Develop strong relationships and norms for bidirectional communication with referring clinicians. |
| Participate in telehealth training within endocrinology fellowship programs and professional conferences. |
| Promote health system processes that optimize the telehealth experience and access. |
| Adopt telehealth platforms with advanced features like screen sharing and electronic health record integration, and that support broad access, including availability in multiple languages. |
| Leverage clinical and information technology staff to support telehealth workflows and improve efficiency of virtual care. |
| Advocate for policies that expand access and affordability of telehealth. |
Clinical Factors
Many studies support the clinical effectiveness of telehealth for diabetes management (3, 4, 26-32), but there are currently limited data on the effectiveness of telehealth for other endocrine diagnoses. Endocrinology, in general, is well suited to telehealth since often the physical exam is neither diagnostic nor prognostic, can be completed virtually, or can be replaced by a more sensitive and specific test. For many endocrine conditions such as adrenal disorders, calcium/bone disorders, lipid disorders, and treated hypothyroidism, history and laboratory or imaging assessments drive clinical decision-making. Even conditions that require frequent visits—such as newly initiated insulin therapy (33, 34) or diabetes mellitus treatment in pregnancy (35)—can be appropriately managed via telehealth with remote access to PGHD.
When in-person assessments are needed—such as a hands-on physical exam, anthropometric measurement, clinical procedure, dynamic laboratory testing, or medication administration—adaptations can sometimes be made to enable completion of these elements via telehealth. For example, collecting vital signs or conducting certain endocrine function assessments (such as adrenocorticotropin stimulation tests) may be accomplished at a primary care or satellite clinic local to the patient, with results then communicated to the endocrine clinician. In multidisciplinary care settings, some team members may be present in person while others join the visit virtually. For example, initiation of insulin therapy can use a multidisciplinary approach to patient education with some team members providing hands-on training and others operating via telehealth (33, 34). However, in-person visits may be preferred by patients and clinicians regardless of clinical need when extensive counseling, guidance, and support is needed, such as discussing a poor prognosis, complex endocrine condition, sensitive health topics, or initial treatment decisions related to endocrine malignancies (36).
A mix of in-person and telehealth encounters over time for a given patient can work well in certain clinical situations. Some patients may benefit from frequent telehealth visits to assist with health-related behavior change punctuated by less frequent in-person visits to address sensitive health topics, access a higher volume of health-related data (eg, laboratory testing and device downloads), or perform critical screening examinations (eg, foot exam to assess for diabetic neuropathy). New patients may need an initial in-person visit if the clinician feels that the physical examination will change either the diagnosis or management strategy (eg, concern for precocious puberty), with subsequent care delivered via telehealth once the correct diagnosis has been established. Alternatively, some new patients may be seen initially by telehealth to expedite the intake to endocrine care and capture more information than provided in referral documents, and the clinician can subsequently decide on what time frame in-person care is needed for a more comprehensive examination. At each telehealth visit, clinicians should incorporate information from the history, available test results, and findings from virtual examination, patient self-examination, and/or the referring provider’s examination to decide if an in-person examination is needed.
While several examples are presented here of diagnoses that may be amenable to appropriate care via telehealth, clinical considerations must be weighed for each patient in the context of other domains to guide optimal decision-making about the modality of care. There are not yet data to indicate an optimal frequency of in-person visits, but some clinicians and patients may prefer in-person visits at least once a year if possible. We recommend clinicians carefully consider what modality is most appropriate for the next encounter at each visit in light of that patient’s current and anticipated clinical needs.
Patient Factors
Many patients face substantial barriers to accessing in-person care. Geographic distance from the clinic, transportation limitations, and work and family obligations can affect a patient’s ability to present for in-person care at recommended intervals. In such circumstances, fully in-person care is not likely to be feasible, effective, or patient-centered, and telehealth is an appealing option.
Telehealth visits can allow additional caregivers to participate from different locations, which may benefit pediatric and geriatric populations. Likewise, telehealth can enable patients with caregiving responsibilities to engage in their medical care while supervising dependents in the home environment. Gender-diverse patients may face limited access to gender-affirming care and perceived stigma in their local health care settings, making telehealth an appealing alternative. Patients with severe anxiety, agoraphobia, or other underlying mental health needs may find care easier to access without the stress of an in-person visit. Telehealth can alleviate these barriers for individuals who are otherwise at heightened risk of foregoing endocrine care altogether. It may also facilitate the continuation of care for established patients during economic, social, or health crises that would otherwise lead to gaps in contact with their clinicians.
However, patient-related factors may decrease the likelihood of a successful telehealth visit in some circumstances. Video telehealth is not an option for patients without reliable internet access, or among those without an adequate video-capable device. Telephone visits can be considered in these cases if suitable care can be provided with an audio-only connection or if it is the only option for care. Data from the COVID-19 pandemic indicate that telephone visits accounted for the majority of telehealth care at many safety-net primary care clinics during 2020, and thus provided a critical lifeline for many patient populations (37, 38). The potential benefits of telephone encounters include ease-of-use both for patient and clinician, reduced rate of no-shows for scheduled appointments (39), and diminished effect of the digital divide on access to care. On the other hand, limitations of audio-only care include difficulties sharing and jointly reviewing PGHD to facilitate shared decision-making, potential lessening of the patient-clinician connection in the absence of both visual and tactile interaction, and reduced reimbursement for practices under the most common current payment structures.
Some telehealth tasks require a moderate to high degree of health and digital literacy and the adoption of new health-related routines that are not required for in-person care. Patients should be able to navigate the necessary video application(s) and may need to perform a limited self-examination, manually upload data, or share data to the cloud. Having clinic staff reach out before the visit to test and troubleshoot technology as part of a virtual rooming process can help patients overcome challenges to these tasks (40). For patients who prefer telehealth but have low digital literacy, engaging a trusted family member or friend to be present during the visit can also be helpful.
Patient-Clinician Relationship
The patient-clinician relationship has 2 components—emotional care and cognitive care (41). Emotional care includes mutual trust, empathy, respect, and warmth (42), while cognitive care includes data gathering, patient education, and expectation management.
Emotional care can be facilitated or impeded by telehealth, depending on the circumstances (43). Some data from prepandemic studies suggest that patients and clinicians prefer the first consultation to be in person (44, 45), which may in part reflect the challenges of building a new personal connection through virtual interaction. For some patients, the hands-on physical exam is an expectation that increases confidence and satisfaction with their care (46). However, the preferences of patients and clinicians may change in the postpandemic era where telehealth has become more common, and the related experience and skill sets of both cohorts have increased.
Telehealth visits may affect the capacity for private conversation between the patient and clinician. Some patients will be more amenable to discussing sensitive topics (eg, mental health, personal relationships) from the comfort of their homes. In other cases, confidential discussion will be more difficult over telehealth if the patient is not in a private area or feels uncomfortable confiding in the clinician at a distance. Other patients may not want the clinician to witness their home environments or may choose to participate for other reasons from an alternative setting that is not ideal for a private discussion. For these reasons, clinicians should consider how telehealth or in-person interaction is likely to affect emotional care during future encounters, and guide the choice of care modality accordingly. Telehealth encounters will also be of higher quality if expectations are set in advance that the patient's environment should have limited distractions and provide a private, quiet area where they feel comfortable discussing health concerns.
Cognitive care may also be affected by the choice of care modality. Technical hurdles related to digital literacy and internet connectivity can impede effective communication during telehealth encounters. On the other hand, shared decision-making can sometimes be better facilitated during telehealth visits by the inclusion of key caregivers or support individuals who could not attend in person. Telehealth can at times reduce the ability for joint observation of relevant health information in the patient’s medical chart—particularly during audio-only encounters or video encounters without the ability to screen share. However, telehealth can improve patients’ ability to easily access their home medications for clarification of doses and discussion of medication-related home routines. In addition, telehealth visits (47) and applications used to access and visualize PGHD (48) have been shown to improve patient engagement in care, particularly for people living with diabetes.
Several aspects of the patient-clinician relationship such as trust, nonverbal communication, and shared language can affect both emotional and cognitive dimensions of care, and their interaction with telehealth should be considered. The perceived level of trust between patient and clinician has been shown to influence patient decisions about use of telehealth (43, 49). Telehealth, with the camera focused on the patient’s face, may offer less opportunity for reading patients’ body language and picking up on nonverbal cues. Finally, a language barrier between the clinician and patient may or may not compromise the quality of telehealth care depending on the availability of remote interpretation services. These examples highlight the bidirectional nature of interactions between care modality and the therapeutic patient-clinician alliance, which can both influence and be influenced by use of telehealth encounters.
Clinician Factors
Most endocrine clinicians, including trainees, have now received real-world telehealth experience in the post-COVID era. However, a minority of endocrinologists have received formal training in telehealth (50). Therefore, clinicians’ digital literacy, experience level, and skills in the telehealth arena are likely to vary widely. This variation may greatly affect the quality of the patient visit. Clinicians should receive an orientation to the telehealth processes as implemented at their practices, and may require test visits and/or a temporarily lower visit frequency while learning new telehealth technologies or workflows (51). Going forward, provision of formal training in key telehealth skills as part of continuing medical education would be beneficial, covering topics such as techniques for remote patient engagement (25), remote data analysis, integrated team care via telehealth, and guiding patient self-examination by video or telephone (52).
Clinicians’ physical surroundings and personal circumstances may affect the feasibility of telehealth visits. Although clinicians can engage in telehealth from a variety of settings (including the home), they must ensure the selected setting offers sufficient internet bandwidth to support uninterrupted encounters and a physically private space to facilitate confidential interaction with patients. In addition, clinicians should be aware of any applicable licensing restrictions if they are providing telehealth to patients across state lines. If these conditions are met, however, telehealth may provide flexibility and benefits to the clinician as well as the patient. At a broader level, allowing clinicians to work remotely when they cannot provide care in person may also help to address challenges to timely endocrine care that stem from current shortages and uneven geographic distribution of the endocrinology workforce (53, 54). Given that one major factor limiting the delivery of high-quality endocrine care to all who could benefit is a lack of endocrine clinicians, this type of flexibility should be supported.
Another clinician factor that may affect the feasibility of telehealth is the endocrine clinician's relationship with the referring clinician. If the referring clinician is well known to the endocrine clinician and able to provide a thorough and reliable physical exam, this may enable many diagnoses that would otherwise require an in-person visit for subspecialist examination (eg, hyperthyroidism, precocious puberty) to be managed safely and effectively via telehealth. However, in cases where examination findings are of particular importance to the diagnosis and treatment course, endocrinologists should guard against premature cognitive closure based on limited or third-party physical examination and may consider in these circumstances whether an in-person visit is needed before or after the initial telehealth interaction.
Health Care Setting and Technology
The infrastructure required for high-quality telehealth care includes essential hardware and software, a reliable and secure internet connection, private space, appropriately trained clinical staff in adequate numbers, clearly defined clinical workflows, and the availability of technical support staff.
Necessary hardware for telehealth includes a computer, mobile device, or telepresence room with internet connectivity, camera, microphone/speaker capabilities, and headphones in some circumstances to protect patient privacy. Practices may use proprietary telehealth software or nonmedical videoconferencing platforms that are HIPAA (Health Insurance Portability and Accountability Act) compliant. When choosing a telehealth platform, practices should consider the relative ease of use by patients, which may be influenced by compatibility with various mobile device operating systems, availability of interpreting services and/or user interfaces in non-English languages, capacity to connect more than 2 parties (for inclusion of caregivers, support individuals, and interpreters), and ability to grant access with limited need for preestablished user accounts. Platforms with features like screen sharing can improve the quality of telehealth care by enabling joint attention to PGHD and test/imaging results for the purposes of shared decision-making. Given the hardware and software interfaces required for successful telehealth and the variable digital literacy of clinicians and patients, a technical support team should be available at all times to provide assistance. Interpreters may also be needed for technical support if electronic medical record and video applications are not provided in languages other than English.
Integrating telehealth into traditional outpatient workflows presents several challenges. Practices with care team members working from different locations must ensure the clinician can contact these individuals to join the patient encounter when appropriate. Before the visit, support staff should be available to help patients access telehealth technology and share any required PGHD. Special considerations exist for individuals with diabetes who may have glucose meter, continuous glucose monitoring, insulin pump, and/or self-reported health data (eg, exercise, diet) available on their mobile or medical devices. To enable remote review of these data, we recommend the use of secure, internet-based diabetes data platforms that allow for passive data upload and easy access by the clinician. When this is not possible, the patient should be instructed on how to upload devices actively at home or—if they live a considerable distance from the clinic and lack the necessary hardware or software at home—connect with a local clinic to help in this process.
Clinical support staff such as medical assistants should ideally be involved in virtually rooming patients before telehealth visits, as this step has been shown to improve telehealth visit completion rates, particularly among demographic groups at higher risk for noncompletion (55). Staff can connect with patients by video or telephone to collect updated contact information and self-reported vital signs from the patient, activate interpretation services to join the visit if needed, notify the patient if the clinician is running behind, prepare necessary prescription refill requests, and assist with scheduling the next visit during virtual checkout (40).
Research Agenda
As the use of telehealth has expanded dramatically since the COVID-19 pandemic and now persists broadly within endocrinology, additional research is needed to identify evidence-based practices and validate the perceived benefits and limitations of this care modality in various clinical scenarios. Research outcomes of major interest include short-term and long-term clinical outcomes, user satisfaction and other patient-reported outcomes, cost and cost-effectiveness, components of successful implementation, and effect on population-level disparities both in access and outcomes. Particular attention should be paid to evaluating the effect of telehealth interventions on health equity measures among historically marginalized linguistic, socioeconomic, rural/urban, racial/ethnic, and gender identity groups.
The panel acknowledges that the quality of endocrine care is likely to vary greatly within a given care modality (telehealth or in-person) and that the benefits of many in-person care practices have not been rigorously demonstrated. However, because in-person care is the historical standard within endocrinology the onus will often fall on researchers to demonstrate noninferiority of telehealth in comparison to in-person care.
Telehealth researchers should carefully consider study design, statistical approaches, and outcomes of interest to maximize the utility of research findings. For example, a study designed to evaluate the efficacy of telehealth vs usual in-person care in achieving a commonly applied clinical outcome may have a negative primary result but achieve other important outcomes (eg, improved access, equity, efficiency, or cost) that are critical to overall care quality. Depending on the outcome(s) of interest and telehealth intervention(s) included in a given study, either a superiority or a noninferiority design may be appropriate. For example, studies aiming to evaluate whether telehealth can deliver equivalent outcomes to in-person interaction for a particular type of care may use a noninferiority design, whereas studies aiming to assess the utility of a new or supplemental type of care delivered via telehealth would employ a traditional design to assess superiority of the new intervention. Carefully planned quasi-experimental designs may also be used to mitigate the concerns about selection bias that often arise in observational studies comparing outcomes of telehealth vs in-person care.
In the process of developing this perspective, the panel identified specific areas in need of future investigation within the 5 identified domains of care.
Clinical Factors
The potential risks and benefits of telehealth to patient safety and health outcomes must be evaluated in various settings. The contribution of in-person physical examinations to diagnostic accuracy and treatment outcomes for specific endocrine conditions should be assessed. The role of the virtual physical examination, including self-reported vital signs by patients or structured physical examination by local providers, should be evaluated for feasibility and accuracy as a potential adjunct to telehealth visits by specialists. The potential for delays or missed diagnoses should be compared for telehealth vs in-person visits. Research is also needed on the optimal frequency of in-person visits for patients seen by telehealth.
Patient Factors
Future research should assess the effect of telehealth visits on provision of patient-centered care, evaluating the patient experience of care (including engagement, self-efficacy, and alignment of care with patient values and preferences) via telehealth vs in-person encounters across a broad range of patient populations. In addition, research is sorely needed on interventions that aim to close the digital divide and facilitate telehealth-based care for populations with limited digital literacy. Finally, researchers must carefully evaluate how increased provision of telehealth affects access to care across patient populations, and whether any consequent changes in the availability of in-person care lead to new or worsening health disparities (56).
Patient-Clinician Relationship
It is yet unknown how the patient-clinician relationship may be affected over time by telehealth-driven care in comparison to in-person care. Standard measures of the patient-clinician relationship should be identified and used to study this outcome of interest. Research is also needed to evaluate the relative benefits and limitations of audio-only care as compared to video or in-person care specifically for building and maintaining a therapeutic patient-clinician relationship and facilitating shared decision-making.
Clinician Factors
The positive and negative effects of telehealth on the clinician workforce must be fully evaluated. This includes the formal assessment of professional satisfaction and burnout in care models that are entirely telehealth, hybrid models, and full in-person models. Ideally, outcomes in this domain would inform initiatives to develop care models that are responsive to clinician as well as patient needs, and to promote maximum flexibility by enabling cross-state licensure for clinicians and allied professionals who care for endocrine conditions.
Healthcare Setting and Technology
Health systems would benefit from research to guide ongoing and future investment in telehealth. Priority should be given to the development and evaluation of 1) new hardware and software that improves the accessibility and efficacy of telehealth encounters across all patient populations, 2) structured clinical workflows for telehealth encounters that improve efficiency and satisfaction for clinicians, and 3) standardized approaches for delivering team-based care over telehealth. The effect of video quality on the sensitivity and specificity of the remote physical examination—particularly via laptop or front-facing mobile device cameras and using limited data upload rates—should also be explored. Finally, cost and cost-effectiveness analyses are needed, and should consider the perspectives of the patient, clinician, and health care system.
Discussion
Endocrinology practices rapidly adopted telehealth during the COVID-19 pandemic to preserve access to care while reducing risks of patient and clinician exposure to the virus and addressing practical and economic barriers to in-person visits. At the outset of the pandemic, changes in reimbursement models enabled explosive growth in telehealth use across the United States (57, 58), with the Centers for Medicare & Medicaid Services recognizing the patient home as a place of service and removing prior stipulations that telehealth could be provided only in a health care facility, in rural/health professional shortage areas, to established patients, and using HIPAA-compliant video platforms (5). More than 2 years after the declaration of the PHE, telehealth remains a frequent and, in some instances, exclusive modality for endocrine care. Yet clinicians lack guidance on the risks, benefits, and overall appropriateness of telehealth for ongoing use in their practices. This perspective attempts to meet that need by addressing how the use of telehealth is likely to affect quality of endocrine care in the context of various care domains and through the lens of the IOM’s 6 aims of high-quality care.
Currently there are insufficient data to provide evidence-based guidance that is absolutely in favor of or against the use of telehealth in specific endocrine diagnoses or patient populations. Instead, the panel relied on our professional experiences and judgment in addition to the small but growing body of literature regarding best practices within telehealth. We outline the circumstances under which telehealth could be used to deliver high-quality endocrine care, understanding that clinicians will need to draw on their own judgment to decide how and when these circumstances apply to their individual patients and practices. We also describe strategies that may render telehealth more successful for patients, clinicians, and health systems.
Moving forward, endocrine care is likely to involve a hybrid of in-person and telehealth visits, and thus the decision to use telehealth for any given patient will not be made at a single time point but rather considered in a longitudinal context. Our panel therefore encourages clinicians to formulate individualized care plans together with their patients by discussing expectations for the role of telehealth in each patient's care and each clinician’s practice over time. These care plans should be revisited at each encounter and adapted based on changes in other domains such as patient factors (eg, geographic relocation, new technology use) and clinical factors (eg, new issue requiring physical examination or in-person discussion such as insulin pump training). In addition, clinical practices should allow flexibility in visit modality when possible to accommodate unplanned changes in the physical and social environment. If new circumstances arise for the patient (eg, illness, transportation barriers, or technology access), altering the planned visit modality from in-person to telehealth, video to audio, or vice versa may be the best way to facilitate the continuation of care and better health outcomes.
There are several potential limitations of this perspective. The panel included academic endocrinologists from various US geographic areas and training backgrounds, but we acknowledge that this perspective may not reflect or apply to every clinical setting. Health system factors and clinician and patient circumstances described in this perspective may differ in countries outside the United States, although we anticipate that the domains we highlight for consideration will be broadly relevant. The dichotomy of in-person vs telehealth care is not applicable for geographic areas with no available endocrinologists, where telehealth is the only option for specialty consults without extensive travel. In addition, the panel recognizes that current and future endocrine care includes other types of telehealth that were not addressed in this document, such as asynchronous patient-clinician secure messaging, remote monitoring of PGHD, clinic-to-clinic synchronous telehealth encounters, asynchronous e-consults between clinicians, as well as other ways to extend specialist expertise including ECHO (Extension for Community Healthcare Outcomes) models (59, 60). Each of these forms of care may be appropriately and effectively used within endocrinology. However, they were outside the scope of the present paper.
While this perspective focuses on clinical decision-making, the authors and the Endocrine Society appreciate that decisions about the use of telehealth cannot be discussed in isolation from pertinent health care and government policies. The use of telehealth cannot overcome the limitations of a shortage in the endocrine workforce, and continued efforts to increase clinician recruitment to the field are needed. Given the many ways we detail how telehealth can promote high-quality care and improve health equity for people with endocrine conditions, we support changes that will increase the accessibility and potential benefits of telehealth for all patients. Specifically, we encourage innovations that will promote the following changes: universal access to broadband internet service and audio-video devices; diabetes technology that supports real-time, passive sharing of data; improved training for and usability of telehealth platforms for individuals with non–English-language preferences and/or limited digital literacy; unanimous coverage of telehealth services by medical insurance carriers; and either national licensing agreements or redefinition of site-of-care as the clinician location to facilitate telehealth across state borders. Payment models should provide similar incentives for in-person and telehealth care, so that provider reimbursement does not become a factor in determining whether patients have access to either care modality. Finally, we espouse the need for ongoing research that explores processes and outcomes associated with high-quality endocrine care via telehealth across a variety of conditions and practice settings. Accomplishing this research will require financial and philosophical support from funding organizations and professional societies, and will provide the foundation for future evidence-based guidelines for telehealth use.
Acknowledgment
The authors thank Rob Goldsmith, director, Advocacy and Policy, the Endocrine Society, for his assistance with organizing and facilitating panel logistics and meetings.
Abbreviations
- HIPAA
Health Insurance Portability and Accountability Act
- IOM
Institute of Medicine
- PGHD
patient-generated health data
- PHE
public health emergency
Contributor Information
Varsha G Vimalananda, Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, Massachusetts 01730, USA; Section of Endocrinology, Diabetes, Nutrition & Weight Management, Department of Medicine, Boston University School of Medicine, Boston, Massachusetts, USA.
Juan P Brito, Knowledge and Evaluation Research (KER) Unit, Mayo Clinic, Rochester, Minnesota, USA; Division of Endocrinology, Diabetes, Metabolism, and Nutrition, Department of Internal Medicine, Mayo Clinic, Rochester, Minnesota, USA.
Leslie A Eiland, Division of Diabetes, Endocrinology & Metabolism, Department of Internal Medicine, University of Nebraska Medical Center, Omaha, Nebraska, USA.
Rayhan A Lal, Division of Endocrinology, Department of Medicine, Stanford University, Stanford, California, USA; Division of Endocrinology, Department of Pediatrics, Stanford University, Stanford, California, USA; Stanford Diabetes Research Center, Stanford University, Stanford, California, USA.
Spyridoula Maraka, Knowledge and Evaluation Research (KER) Unit, Mayo Clinic, Rochester, Minnesota, USA; Division of Endocrinology and Metabolism, Department of Medicine, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA; Section of Endocrinology, Central Arkansas Veterans Healthcare System, Little Rock, Arkansas, USA.
Marie E McDonnell, Division of Endocrinology, Diabetes and Hypertension, Department of Medicine, Brigham and Women's Hospital, Boston, Massachusetts, USA; Harvard Medical School, Boston, Massachusetts, USA.
Radhika R Narla, Division of Metabolism, Endocrinology and Nutrition, Department of Medicine, University of Washington, Seattle, Washington, USA; VA Puget Sound Health Care System, Seattle, Washington, USA.
Mara Y Roth, Division of Metabolism, Endocrinology and Nutrition, Department of Medicine, University of Washington, Seattle, Washington, USA.
Stephanie S Crossen, Division of Endocrinology, Department of Pediatrics, University of California Davis School of Medicine, Sacramento, California, USA; Center for Health and Technology, University of California Davis Health, Sacramento, California, USA.
Financial Support
V.G.V. receives support from the United States Department of Veterans Affairs Health Services Research & Development Service of the VA Office of Research and Development through Award No. IK2 HX-002137-01 and from resources at the VA Bedford Healthcare System. J.P.B. receives support from the National Cancer Institute of the National Institutes of Health (NIH) through Award No. R37CA272473. L.A.E. has participated in paid advisory boards for Provention Bio, Roche, and Cecelia Health. R.A.L. has consulted for Abbott Diabetes Care, Biolinq, Capillary Biomedical, Deep Valley Labs, Morgan Stanley, Gluroo, and Tidepool. S.M. receives support from the Arkansas Biosciences Institute, the major research component of the Arkansas Tobacco Settlement Proceeds Act of 2000, and from the United States Department of Veterans Affairs Health Services Research & Development Service of the VA Office of Research and Development through Award No. 1I21HX003268-01A1. M.E.M. has consulted for Everly Health, and research funding from Lilly, Inc. was paid to her institution. S.S.C. receives support from the National Institute for Diabetes and Digestive and Kidney Diseases, NIH, through Award No. K23DK125671. The views presented here do not necessarily represent the views of the Department of Veterans Affairs, the NIH, or the United States government.
Disclosures
The authors have nothing to disclose.
References
- 1. Health Resources & Services Administration . What is telehealth? Department of health and human services. Accessed June 6, 2022. https://telehealth.hhs.gov/patients/understanding-telehealth/#what-does-telehealth-mean
- 2. McDonnell ME. Telemedicine in complex diabetes management. Curr Diab Rep. 2018;18(7):42. [DOI] [PubMed] [Google Scholar]
- 3. Su D, Zhou J, Kelley MS, et al. Does telemedicine improve treatment outcomes for diabetes? A meta-analysis of results from 55 randomized controlled trials. Diabetes Res Clin Pract. 2016;116:136–148. [DOI] [PubMed] [Google Scholar]
- 4. Tchero H, Kangambega P, Briatte C, Brunet-Houdard S, Retali GR, Rusch E. Clinical effectiveness of telemedicine in diabetes mellitus: a meta-analysis of 42 randomized controlled trials. Telemed J E Health. 2019;25(7):569–583. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Medicare & Medicaid Services . Medicare telemedicine health care provider fact sheet. Accessed June 21, 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 6. Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res. 2020;22(12):e24087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood). 2021;40(2):349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Haynes SC, Marcin JP, Dayal P, Tancredi DJ, Crossen S. Impact of telemedicine on visit attendance for paediatric patients receiving endocrinology specialty care. J Telemed Telecare. Published online November 23, 2020. doi: 10.1177/1357633X20972911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crossen SS, Romero CC, Loomba LA, Glaser NS. Patient perspectives on use of video telemedicine for type 1 diabetes care in the United States during the COVID-19 pandemic. Endocrines. 2021;2(4):449–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sim R, Lee SWH. Patient preference and satisfaction with the use of telemedicine for glycemic control in patients with type 2 diabetes: a review. Patient Prefer Adherence. 2021;15:283–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ramaswamy A, Yu M, Drangsholt S, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22(9):e20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Andrews E, Berghofer K, Long J, Prescott A, Caboral-Stevens M. Satisfaction with the use of telehealth during COVID-19: an integrative review. Int J Nurs Stud Adv. 2020;2:100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Saiyed S, Nguyen A, Singh R. Physician perspective and key satisfaction indicators with rapid telehealth adoption during the coronavirus disease 2019 pandemic. Telemed J E Health. 2021;27(11):1225–1234. [DOI] [PubMed] [Google Scholar]
- 14. Haynes SC, Kompala T, Neinstein A, Rosenthal J, Crossen S. Disparities in telemedicine use for subspecialty diabetes care during COVID-19 shelter-in-place orders. J Diabetes Sci Technol. 2021;15(5):986–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barbosa W, Zhou K, Waddell E, Myers T, Dorsey ER. Improving access to care: telemedicine across medical domains. Annu Rev Public Health. 2021;42:463–481. [DOI] [PubMed] [Google Scholar]
- 16. Ye S, Kronish I, Fleck E, et al. Telemedicine expansion during the COVID-19 pandemic and the potential for technology-driven disparities. J Gen Intern Med. 2021;36(1):256–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Institute of Medicine Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001. [PubMed] [Google Scholar]
- 18. Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70(4):351–379. [DOI] [PubMed] [Google Scholar]
- 20. Dhaliwal R, Pereira RI, Diaz-Thomas AM, Powe CE, Yanes Cardozo LL, Joseph JJ. Eradicating racism: an endocrine society policy perspective. J Clin Endocrinol Metab. 2022;107(5):1205–1215. [DOI] [PubMed] [Google Scholar]
- 21. Adepoju OE, Chae M, Ojinnaka CO, Shetty S, Angelocci T. Utilization gaps during the COVID-19 pandemic: racial and ethnic disparities in telemedicine uptake in federally qualified health center clinics. J Gen Intern Med. 2022;37(5):1191–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Eberly LA, Kallan MJ, Julien HM. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med. 2020;180(10):1386–1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rovner BW, Casten RJ, Chang AM, Hollander JE, Rising K. Mistrust, neighborhood deprivation, and telehealth use in African Americans with diabetes. Popul Health Manag. 2021;24(6):699–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gray DM II, Joseph JJ, Olayiwola JN. Strategies for digital care of vulnerable patients in a COVID-19 world—keeping in touch. JAMA Health Forum. 2020;1(6):e200734. [DOI] [PubMed] [Google Scholar]
- 26. Faruque LI, Wiebe N, Ehteshami-Afshar A, et al. ; Alberta Kidney Disease Network. Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. CMAJ. 2017;189(9):E341–E364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;2015(9):CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Greenwood DA, Blozis SA, Young HM, Nesbitt TS, Quinn CC. Overcoming clinical inertia: a randomized clinical trial of a telehealth remote monitoring intervention using paired glucose testing in adults with type 2 diabetes. J Med Internet Res. 2015;17(7):e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shea S, Weinstock RS, Teresi JA, et al. ; IDEATel Consortium. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16(4):446–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wood CL, Clements SA, McFann K, Slover R, Thomas JF, Wadwa RP. Use of telemedicine to improve adherence to American Diabetes Association Standards in pediatric type 1 diabetes. Diabetes Technol Ther. 2016;18(1):7–14. [DOI] [PubMed] [Google Scholar]
- 31. Zhai YK, Zhu WJ, Cai YL, Sun DX, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore). 2014;93(28):e312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Eberle C, Stichling S. Clinical improvements by telemedicine interventions managing type 1 and type 2 diabetes: systematic meta-review. J Med Internet Res. 2021;23(2):e23244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Peters AL, Garg SK. The silver lining to COVID-19: avoiding diabetic ketoacidosis admissions with telehealth. Diabetes Technol Ther. 2020;22(6):449–453. [DOI] [PubMed] [Google Scholar]
- 34. Shawar RS, Cymbaluk AL, Bell JJ, et al. Isolation and education during a pandemic: novel telehealth approach to family education for a child with new-onset type 1 diabetes and concomitant COVID-19. Clin Diabetes. 2021;39(1):124–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ming WK, Mackillop LH, Farmer AJ, et al. Telemedicine technologies for diabetes in pregnancy: a systematic review and meta-analysis. J Med Internet Res. 2016;18(11):e290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zon RT, Kennedy EB, Adelson K, et al. Telehealth in oncology: ASCO standards and practice recommendations. JCO Oncol Pract. 2021;17(9):546–564. [DOI] [PubMed] [Google Scholar]
- 37. Chang JE, Lindenfeld Z, Albert SL, et al. Telephone vs. video visits during COVID-19: safety-net provider perspectives. J Am Board Fam Med. 2021;34(6):1103–1114. [DOI] [PubMed] [Google Scholar]
- 38. Uscher-Pines L, Sousa J, Jones M, et al. Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA. 2021;325(11):1106–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Muppavarapu K, Saeed SA, Jones K, Hurd O, Haley V. Study of impact of telehealth use on clinic “no show” rates at an academic practice. Psychiatr Q. 2022;93(2):689–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gomez T, Bholat MA, Campos B, Tarn DM. Implementing virtual patient rooming during telemedicine visits. In: de Pablos PO, Chui KT, Lytras MD, eds. Digital Innovation for Healthcare in COVID-19 Pandemic: Strategies and Solutions. Information Technologies in Healthcare Industry: Academic Press; 2022:67–74. [Google Scholar]
- 41. Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet. 2001;357(9258):757–762. [DOI] [PubMed] [Google Scholar]
- 42. Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995;40(7):903–918. [DOI] [PubMed] [Google Scholar]
- 43. Yee V, Bajaj SS, Stanford FC. Paradox of telemedicine: building or neglecting trust and equity. Lancet Digit Health. 2022;4(7):e480–e481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Auret K, Pikora T, Pola M. Specialist haematology consultation services in regional western Australia: evaluating a model combining telehealth and onsite clinics. Intern Med J. 2022;52(3):451–457. [DOI] [PubMed] [Google Scholar]
- 45. Sturesson L, Groth K. Clinicians’ selection criteria for video visits in outpatient care: qualitative study. J Med Internet Res. 2018;20(11):e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zemencuk JK, Hayward RA, Skarupski KA, Katz SJ. Patients’ desires and expectations for medical care: a challenge to improving patient satisfaction. Am J Med Qual. 1999;14(1):21–27. [DOI] [PubMed] [Google Scholar]
- 47. Reid MW, Krishnan S, Berget C, et al. CoYoT1 clinic: home telemedicine increases young adult engagement in diabetes care. Diabetes Technol Ther. 2018;20(5):370–379. [DOI] [PubMed] [Google Scholar]
- 48. Wong JC, Izadi Z, Schroeder S, et al. A pilot study of use of a software platform for the collection, integration, and visualization of diabetes device data by health care providers in a multidisciplinary pediatric setting. Diabetes Technol Ther. 2018;20(12):806–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bailey JE, Gurgol C, Pan E, et al. Early patient-centered outcomes research experience with the use of telehealth to address disparities: scoping review. J Med Internet Res. 2021;23(12):e28503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Madduri S, Chowdhary PT, Reddy SS. Telehealth adoption among endocrinologists during the COVID-19 pandemic. Endocr Pract. 2020;26(8):846–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Crossen S, Raymond J, Neinstein A. Top 10 tips for successfully implementing a diabetes telehealth program. Diabetes Technol Ther. 2020;22(12):920–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Tewksbury C, Deleener ME, Dumon KR, Williams NN. Practical considerations of developing and conducting a successful telehealth practice in response to COVID-19. Nutr Clin Pract. 2021;36(4):769–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Allen DB, Aye T, Boney CM, et al. Sustaining the pediatric endocrinology workforce: recommendations from the Pediatric Endocrine Society Workforce Task Force. J Pediatr. 2020;233:4–7. [DOI] [PubMed] [Google Scholar]
- 54. Vigersky RA, Fish L, Hogan P, et al. The clinical endocrinology workforce: current status and future projections of supply and demand. J Clin Endocrinol Metab. 2014;99(9):3112–3121. [DOI] [PubMed] [Google Scholar]
- 55. Lieu TA, Warton EM, Levan C, et al. Association of medical assistant-supported virtual rooming with successful video visit connections. JAMA Intern Med. 2022;182(6):680–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Haynes SC, Kompala T, Tancredi DJ, Neinstein AB, Crossen SS. Factors associated with discontinuation of subspecialty diabetes care during the COVID-19 pandemic: a multisite retrospective cohort study. Diabetes Care. 2022;45(2):e34–e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Cantor JH, McBain RK, Pera MF, Bravata DM, Whaley CM. Who is (and is not) receiving telemedicine care during the COVID-19 pandemic. Am J Prev Med. 2021;61(3):434–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Demeke HB, Merali S, Marks S, et al. Trends in use of telehealth among health centers during the COVID-19 pandemic—United States, June 26-November 6, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(7):240–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bouchonville MF, Paul MM, Billings J, Kirk JB, Arora S. Taking telemedicine to the next level in diabetes population management: a review of the Endo ECHO model. Curr Diab Rep. 2016;16(10):96. [DOI] [PubMed] [Google Scholar]
- 60. Lewiecki EM, Rochelle R, Bouchonville MF II, Chafey DH, Olenginski TP, Arora S. Leveraging scarce resources with bone health TeleECHO to improve the care of osteoporosis. J Endocr Soc. 2017;1(12):1428–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]