Abstract
Background
People with HIV experiencing homelessness have low rates of viral suppression, driven by sociostructural barriers and traditional care system limitations. Informed by the capability-opportunity-motivation-behavior (COM-B) model and patient preference research, we developed POP-UP, an integrated drop-in (nonappointment-based) HIV clinic with wrap-around services for persons with housing instability and viral nonsuppression in San Francisco.
Methods
We report HIV viral suppression (VS; <200 copies/mL), care engagement, and mortality at 12 months postenrollment. We used logistic regression to determine participant characteristics associated with VS.
Results
We enrolled 112 patients with viral nonsuppression and housing instability: 52% experiencing street-homelessness, 100% with a substance use disorder, and 70% with mental health diagnoses. At 12 months postenrollment, 70% had ≥1 visit each 4-month period, although 59% had a 90-day care gap; 44% had VS, 24% had viral nonsuppression, 23% missing, and 9% died (6 overdose, 2 AIDS-associated, 2 other). No baseline characteristics were associated with VS.
Conclusions
The POP-UP low-barrier HIV care model successfully reached and retained some of our clinic’s highest-risk patients. It was associated with VS improvement from 0% at baseline to 44% at 12 months among people with housing instability. Care gaps and high mortality from overdose remain major challenges to achieving optimal HIV treatment outcomes in this population.
Keywords: HIV, homelessness and unstable housing, care engagement, care model
People with human immunodeficiency virus (PWH) experiencing homelessness have low rates of human immunodeficiency virus (HIV) viral suppression, even among those engaged in care [1, 2]. In San Francisco, unstable housing currently creates the largest disparity in HIV treatment outcomes, with only 20% of persons experiencing homelessness achieving viral suppression in 2020, compared to 71% of housed PWH [3]. Furthermore, increasing levels of housing instability are associated with decreasing levels of HIV viral suppression [4].
Current HIV primary care models are often inadequate for people experiencing homelessness. At the patient level, numerous factors make it difficult to attend appointments at a specified date and time, including competing sustenance needs, phone availability to receive appointment reminders, lack of secure location to store belongings, difficulties navigating insurance, and comorbidities (eg, substance use, mental health, other medical conditions) [5–10]. At a systems level, funding models are built around 20-minute medical visits that are inadequate to address these multiple pressing needs, particularly when patients arrive late or at times when they do not have an appointment. Difficulty attending scheduled visits leads to lower utilization of primary care and greater utilization of urgent care and emergency rooms [1, 11–14].
Low-barrier, comprehensive HIV primary care models that provide drop-in services are a promising strategy for engaging PWH experiencing homelessness in longitudinal HIV care. The Positive-Health Onsite Program for Unstably Housed Populations (POP-UP) HIV primary care model at the Ward 86 clinic in San Francisco is a low-barrier approach designed to address the needs and preferences of this population. We previously reported a 6-month evaluation of POP-UP care outcomes [15]. Here we extend this prior evaluation by evaluating care engagement, HIV viral suppression, and mortality 12 months after POP-UP enrollment.
METHODS
Setting, Design, and Participants
The POP-UP program is based in the Ward 86 HIV clinic at San Francisco General Hospital, San Francisco’s largest public HIV clinic. Ward 86 is a Ryan White-funded clinic that offers HIV primary care through scheduled visits and urgent care services for acute medical issues that cannot wait until the next available primary care appointment. POP-UP was developed to serve the unique needs of patients experiencing homelessness who were accessing Ward 86 for urgent issues, but who were unable to engage with scheduled primary care visits.
Ward 86 patients are eligible for POP-UP if they meet all of the following criteria: (1) experiencing homelessness or unstable housing, (2) off antiretroviral therapy (ART) or current HIV viral load ≥200 copies/mL, (3) missed ≥1 primary care visit in the last year, and (4) ≥2 unscheduled Ward 86 clinic visits in the past year. Eligible patients are identified through referrals from Ward 86, from a San Francisco Department of Public Health linkage team that identifies patients out of care, and through electronic medical record review at a single point in time in November-December 2018. We conducted cohort studies of 2 related populations from POP-UP launch (January 2019) through February 2021: (1) eligible patients referred for POP-UP (eligible cohort) and (2) patients who enrolled in POP-UP (enrolled cohort). The study was approved by the University of California San Francisco Institutional Review Board (IRB); data were collected through medical record review and the IRB determined that individual patient consent was not required.
Description of POP-UP and Theoretical Model
The POP-UP multicomponent care model includes low-barrier primary care services without the need for scheduled appointments, financial incentives for visits and attaining HIV viral suppression, enhanced outreach via peer navigators, and integrated social work and case management services [15]. POP-UP providers prescribe medication assisted treatment for substance use disorders, including buprenorphine-naloxone, and patients can pick up medication directly from clinic, allowing in-clinic buprenorphine-naloxone inductions. We also provide safe consumption kits and naloxone. Methadone treatment is available from a separate methadone clinic in a building adjacent to our clinic.
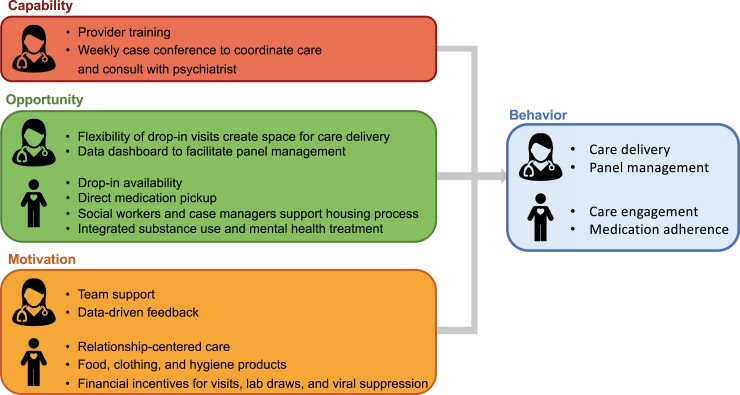
Model components were empirically and theoretically developed to reduce patient- and clinic/provider-level barriers to delivering high-quality HIV primary care for persons experiencing homelessness who have experienced difficulty engaging with traditional care models. To empirically inform model development, we conducted discrete choice experiments to evaluate relative patient preferences for intervention components and refine the intervention over time [16, 17]. Discrete choice experiments are increasingly used in implementation science to identify stated preferences and trade-offs between attributes of an intervention and to enhance stakeholder engagement in intervention design [18]. Relationships with care providers, incentives, and drop-in visit availability were all strongly preferred. Informed by the capability-opportunity-motivation-behavior (COM-B) model for behavior change [19], we also designed additional patient- and provider-level intervention components to facilitate provider care delivery and patient care engagement (Figure 1).
Figure 1.
Theoretical model for patient- and provider-level Positive-Health Onsite Program for Unstably Housed Populations (POP-UP) intervention components.
At the provider level, POP-UP addresses capability through in-service clinical trainings (eg, substance use disorder treatment, management of psychotic symptoms) and weekly case conferences to facilitate care coordination and patient discussion. Case conferences are attended by a psychiatrist, equipping HIV primary care providers with ready access to specialty mental health consultation. POP-UP enhances provider opportunity to deliver care effectively for this patient population by eliminating appointments, allowing more time to spend with patients who might otherwise arrive late for a scheduled visit and may not be seen in a traditional clinic setting. Nurse-led panel management using a data dashboard also enhances opportunities to provide primary care services, follow-up with patients lost to follow-up, and coordinate with other members of the extended care team—a key distinction from urgent care models. Provider motivation is enhanced through team support at weekly case conference, quarterly team support sessions facilitated by a psychologist, and through data-driven feedback via the clinic data dashboard that the team reviews at the weekly case conference.
At the patient level, POP-UP increases opportunity for care engagement via drop-in access to medical care (including integrated substance use and mental health treatment) and drop-in social work/case management services. In addition, patients may directly pick up medications from clinic, removing the extra step of visiting a pharmacy. Patient motivation is enhanced through relationship-centered care facilitated by close relationships with a dedicated nurse, social worker, and small group of clinicians [16, 20]; the use of financial incentives to promote care engagement and attaining viral suppression; and provision of snacks, basic hygiene products, and clothing when needed. Incentives are provided in the form of grocery store gift cards in the amount of $10 for a clinical/social work visit (maximum once/week), $10 for blood draw (if clinically indicated, maximum once/week), $25 for HIV viral load <200 copies/mL (maximum once every 2–3 months).
Measurements and Analysis
Our objective was to evaluate baseline demographic and clinical characteristics associated with POP-UP enrollment among eligible patients referred to the program (eligible cohort) and care engagement and HIV viral suppression after 12 months among patients who enrolled (enrolled cohort). We used chart review to collect baseline demographic information (age, sex assigned at birth, gender identity, self-identified race/ethnicity, and housing status), mental health or a current substance use disorder (restricting to methamphetamine, opioids, cocaine, alcohol; see Supplementary material), housing status, HIV viral load, and CD4 count. We also assessed housing status among patients enrolled in POP-UP at 6 and 12 months postenrollment using chart review from the most recent clinic visit within 3 months of each time point. Our clinic systematically collects self-identified race/ethnicity, sex assigned at birth, and gender identity data through a structured field in the medical record. POP-UP visits systematically assess social determinants of health relevant for our patient population, including housing status, substance use, and mental health. We extracted prospective HIV viral load and clinic visit data from the electronic medical record and changes in housing status from the POP-UP data dashboard. We received notification of all deaths via the county Medical Examiner.
We categorized substance use disorders using a validated hierarchical approach [21, 22]: methamphetamine (± other substances), opioids (± cocaine or alcohol), cocaine (± alcohol), alcohol alone, or none of the above. We used a similar hierarchical approach for mental health diagnoses [21, 22]: psychotic disorder (± other diagnoses), bipolar disorder (±depression/anxiety), depression or anxiety, or none of the above. We classified housing status as street homeless (living on the street, in a vehicle, or in a space not intended for human habitation), temporary (transitional housing, stabilization room, treatment program, couch surfing, shelter, incarceration, or shelter-in place hotel), or permanent (permanent single room occupancy, permanent supportive housing, permanent independent housing) [4]. We used visit and laboratory records to estimate total incentives provided.
Among patients eligible for POP-UP (eligible cohort), our primary outcome was POP-UP enrollment, defined as attendance of ≥1 POP-UP clinic visit. We conducted unadjusted and adjusted logistic regression using a type I error cutoff of P < .1 to assess associations between study factors (demographic and clinical characteristics) and outcomes among referred patients.
Among patients enrolled in POP-UP (enrolled cohort), our primary outcomes were HIV viral suppression and care engagement. HIV viral suppression was defined as viral load <200 copies/mL at 12 months, using the most recent HIV viral load available in months 8–12 postenrollment. We considered those who died or those with missing viral load data during this window to be unsuppressed. In sensitivity analysis, we also report the proportion alive and virally suppressed at 12 months using the last observed HIV viral load. We evaluated care engagement using 2 complementary measures: presence of a 90-day gap between clinical visits and visit constancy [23] (≥1 clinical visit in each 4-month period postenrollment, excluding the initial enrollment visit), with follow-up time for each of these outcomes censored at time of move out of the San Francisco Bay Area or death. We recommend that patients visit POP-UP at least monthly, and more frequently if required by medical acuity or if new medical problems develop. Patients also have the option pick up medications directly from clinic at intervals of weekly, biweekly, or monthly according to patient preference. Patients who are late for medication pick-up or who have not been to clinic in 3 months are considered overdue for a visit and receive outreach by phone call or text message. Thus, these measures assess a minimal threshold for POP-UP care engagement. We evaluated vital status and cause of death using death reports from the county Medical Examiner.
Similar to the enrollment evaluation, we conducted unadjusted and adjusted logistic regression using a type I error cutoff of P < .1 to assess associations between study factors (demographic and clinical characteristics) of enrolled patients and care engagement/viral suppression outcomes. We also used the cumulative incidence function to estimate cumulative incidence of any HIV viral suppression <200 copies/mL during the first 12 months of enrollment, treating death and move out of the San Francisco Bay Area as competing events [24].
RESULTS
Enrollment in POP-UP Among Referred Patients
From January 2019 through February 2021, 185 eligible patients were referred to POP-UP, among whom 112 (61%) enrolled (Table 1). Reasons for nonenrollment included patient preference to remain in traditional primary care (n = 8, 11%) and patient not returning to clinic to offer enrollment (n = 65, 89%).
Table 1.
Demographic Characteristics of Patients Referred (n = 185) and Enrolled (n = 112) in POP-UP Prior to 1 March 2021
| Characteristic | Referred (n = 185) | Enrolled (n = 112) |
|---|---|---|
| Age | ||
| Age, y, median (IQR) | 42 (34–53) | 42 (35–53) |
| Gender | ||
| Cisgender man | 156 (84) | 94 (84) |
| Cisgender woman | 17 (9) | 9 (8) |
| Transgender woman | 10 (5) | 7 (6) |
| Transgender man | 2 (1) | 2 (2) |
| Race | ||
| White | 90 (49) | 53 (47) |
| Black | 55 (30) | 37 (33) |
| Hispanic/Latino/a | 22 (12) | 12 (11) |
| AIAN | 5 (3) | 5 (4) |
| API | 8 (4) | 2 (2) |
| Other | 5 (3) | 3 (3) |
| Housing type | ||
| Street | 78 (42) | 58 (52) |
| Staying with friends | 28 (15) | 15 (13) |
| Transitional | 18 (10) | 15 (13) |
| Shelter | 17 (9) | 13 (12) |
| Treatment | 13 (7) | 4 (4) |
| Shelter-in-place hotel | 10 (5) | 5 (4) |
| Temporary single room occupancy | 6 (3) | 2 (2) |
| Unknown | 15 (8) | 0 (0) |
| Referral source | ||
| Ward 86 clinical team | 106 (57) | 84 (75) |
| External (DPH, jail, other) | 13 (7) | 8 (7) |
| Electronic medical record review | 66 (36) | 20 (18) |
| Any VL <200 copies/mL in 12 mo prior to POP-UP | NA | 34 (30) |
| Baseline CD4 count | ||
| < 200 cells/μL | 64 (35) | 42 (38) |
| ≥ 200 cells/μL | 108 (58) | 70 (62) |
| Missing | 13 (7) | 0 (0) |
| Substance use disordera | ||
| Methamphetamine ± other | 149 (81) | 98 (88) |
| Opioids ± cocaine/alcohol | 10 (5) | 3 (3) |
| Cocaine ± alcohol | 13 (7) | 7 (6) |
| Alcohol | 7 (4) | 4 (4) |
| None | 6 (3) | 0 |
| Mental health diagnosisb | ||
| Psychotic disorder ± other | 34 (18) | 21 (19) |
| Bipolar disorder ± depression/anxiety | 13 (7) | 9 (8) |
| Depressive/anxiety disorder | 71 (38) | 48 (43) |
| None | 67 (36) | 34 (30) |
| Any mental health diagnosis | 118 (64) | 78 (70) |
Data are No. (%) except where indicated.
Abbreviations: AIAN, American Indian or Alaska Native; API, Asian, Hawaiian Naitve, or Other Pacific Islander; DPH, Department of Public Health; IQR, interquartile range; POP-UP, Positive-Health Onsite Program for Unstably Housed Populations; VL, viral load.
Mutually exclusive, hierarchical classification of substance use: methamphetamine (± other substances), opioids (± cocaine or alcohol), cocaine (± alcohol), alcohol alone, or none of the above.
Mutually exclusive, hierarchical classification of mental health diagnoses: psychotic disorder with or without other diagnoses, bipolar disorder (± depression or anxiety), depression or anxiety, or none of the above.
Factors associated with successful enrollment among referred patients included street homelessness (adjusted odds ratio [aOR], 2.20; 95% confidence interval [CI], 1.06–4.57) and presence of a mental health diagnosis (aOR, 2.48; 95% CI, 1.18–5.24). Patients identified by medical record review were much less likely to enroll in POP-UP compared to internal referral (aOR, 0.15; 95% CI, .07–.32; Table 2)
Table 2.
Associations Between Study Characteristics and Enrollment in POP-UP Among Eligible Patients Referred to the Program
| Unadjusted | Adjusted | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Linkage, n linked / total (%) | Odds Ratio | (95% CI) | P Value | Odds Ratio | (95% CI) | P Value |
| Age category, y | .88 | ||||||
| < 40 | 55/90 (61) | ref | |||||
| ≥ 40 | 57/95 (60) | 0.95 | (.53–1.72) | ||||
| Gender | .49 | ||||||
| Cisgender man | 94/156 (60) | ref | |||||
| Cisgender woman | 9/17 (53) | 0.74 | (.27–2.03) | ||||
| Transgender/nonbinary | 9/12 (75) | 1.98 | (.52–7.60) | ||||
| Race | .65 | ||||||
| White | 53/90 (59) | ref | |||||
| Black | 37/55 (67) | 1.44 | (.71–2.90) | ||||
| Hispanic/Latino/a | 12/22 (55) | 0.84 | (.33–2.14) | ||||
| Other | 10/18 (56) | 0.87 | (.31–2.42) | ||||
| Housing type | .03 | .03 | |||||
| Temporary | 54/92 (59) | ref | Ref | ||||
| Unsheltered | 58/78 (74) | 2.04 | (1.06–3.93) | 2.20 | (1.06–4.57) | ||
| Unknown | 0/15 (0) | Omitted | Omitted | ||||
| Baseline CD4 count | .66 | ||||||
| < 200 cells/μL | 43/64 (67) | 1.16 | (.60–2.22) | ||||
| ≥ 200 cells/μL | 69/108 (64) | ref | |||||
| Missing | 0/13 (0) | Omitted | |||||
| Substance use disordera | .17 | ||||||
| Methamphetamine ± other | 112/179 (63) | ref | |||||
| Opioids ± cocaine/alcohol | 3/10 (30) | 0.22 | (.06–.90) | ||||
| Cocaine ± alcohol | 7/13 (54) | 0.61 | (.19–1.90) | ||||
| Alcohol | 4/7 (57) | 0.69 | (.15–3.22) | ||||
| None | 0/6 (0) | … | |||||
| Any mental health diagnosis (vs none) | 78/118 (66) | 1.89 | (1.03–3.49) | .04 | 2.48 | (1.18–5.24) | .02 |
| Mental health diagnosisb | .21 | ||||||
| Psychotic disorder | 21/34 (62) | 1.57 | (.68–3.64) | ||||
| Bipolar disorder | 9/13 (69) | 2.18 | (.61–7.79) | ||||
| Depressive/anxiety disorder | 48/71 (68) | 2.02 | (1.02–4.04) | ||||
| None | 34/67 (51) | ref | |||||
| Referral source | <.0001 | <.0001 | |||||
| Ward 86 clinical team | 84/106 (79) | ref | ref | ||||
| External (DPH, jail, other) | 8/13 (62) | 0.42 | (.12–1.41) | 0.44 | (.12–1.55) | ||
| Electronic medical record review | 20/66 (30) | 0.11 | (.06–.23) | 0.15 | (.07–.32) | ||
Abbreviations: CI, confidence interval; DPH, Department of Public Health; POP-UP, Positive-Health Onsite Program for Unstably Housed Populations; ref, reference.
Mutually exclusive, hierarchical classification of substance use: methamphetamine (± other substances), opioids (± cocaine or alcohol), cocaine (± alcohol), alcohol alone, or none of the above.
Mutually exclusive, hierarchical classification of mental health diagnoses: psychotic disorder with or without other diagnoses, bipolar disorder (± depression or anxiety), depression or anxiety, or none of the above.
Characteristics of Enrolled Patients
Among the 112 patients enrolled in POP-UP prior to 1 March 2021, median age was 42 years (IQR, 35–53 years); 84% were cisgender men, 8% cisgender women, 6% transgender women, 2% transgender men; 47% were white, 33% black, and 10% Hispanic/Latino/a. Over half (52%) were living outdoors at the time of enrollment, 100% had a substance use disorder (methamphetamine, opioids, cocaine, or alcohol), and 70% had a mental health disorder. In the 12 months prior to enrollment, patients attended a median of 1 primary care visit (IQR, 0–1) and 3 drop-in visits (IQR, 2–5) at Ward 86.
Among those living on the street at baseline (n = 58), 53% (n = 31) attained and maintained temporary housing (n = 23; 11 shelter-in-place hotel, 6 transitional housing/treatment program, 3 with friends, 3 shelter) or permanent housing (n = 8; 7 permanent single-room-occupancy, 1 permanent supportive housing) at 12 months. Among those in temporary housing at baseline (n = 54), 78% (n = 42) maintained temporary housing or obtained permanent housing by 12 months and 22% (n = 12) became street homeless. Overall, 66% (n = 74) attained or maintained temporary/permanent housing by 12 months.
Care Engagement and HIV Viral Suppression Among Enrolled Patients
Twelve months following enrollment in POP-UP, 95 (85%) patients remained enrolled in the program, defined as maintaining POP-UP as their assigned primary care provider. Among those unenrolled, 10 died, 3 moved out of state, 3 were transferred to other clinics for behavioral problems, and 1 returned to their previous primary care provider. Seventy percent had ≥1 POP-UP follow-up visit each 4-month period, although 59% had at least 1 gap between clinic visits of ≥90 days. Median POP-UP clinic visits over the first 12 months was 12 per patient (IQR, 7–25). The median value of incentives received was $170 (IQR, $98–$278).
Among 112 enrolled patients, the cumulative incidence of HIV viral suppression was 66% (95% CI, 57%–74%) over the first 12 months (Supplementary Figure 1). At 12 months postenrollment, 49 (44%) were suppressed, 27 (24%) unsuppressed, 26 (23%) had missing viral load data, and 10 (9%) died (6 overdose, 2 AIDS-associated, 1 gastrointestinal bleed, and 1 heart failure; Supplementary Table 1). Reasons for missing viral load data included no visit in prior 4 months (n = 11), clinical visit but no laboratory data (n = 10), moved out of state (n = 2), transferred to another clinic (n = 2), and long-term incarceration and declining care (n = 1). In sensitivity analysis based on the last observed HIV viral load at 12 months postenrollment, 62 (55%) were <200 copies/mL, 40 (36%) were ≥200 copies/mL, and 10 (9%) died.
Unadjusted associations between study factors (baseline demographics, clinical characteristics, and changes in housing status) and 12-month HIV viral suppression, as well as visit constancy, did not reach levels of significance (Table 3 and Supplementary Table 2). Presence of a baseline mental health diagnosis was associated with lower risk of having a ≥90-day gap between clinic visits (53% versus 74%; OR, 0.40; 95% CI, .17–.96; Supplementary Table 3).
Table 3.
Characteristics Associated With HIV Viral Suppression at 12 Months Postenrollment in POP-UP (n = 112)
| Characteristic | VL <200 cells/μL, n / total (%) | Odds Ratio | (95% CI) | P Value |
|---|---|---|---|---|
| Age category, y | .49 | |||
| < 40 | 25/53 (47) | ref | ref | |
| ≥ 40 | 24/59 (41) | 0.77 | (.36–1.62) | |
| Gender | .14 | |||
| Cisgender man | 38/94 (40) | ref | ref | |
| Cisgender woman | 4/9 (44) | 1.18 | (.30–4.68) | |
| Transgender/nonbinary | 7/9 (78) | 5.16 | (1.02–26.2) | |
| Race/ethnicity | .83 | |||
| White | 24/53 (45) | ref | ref | |
| Black | 17/37 (46) | 1.03 | (.44–2.39) | |
| Hispanic/Latinx | 5/12 (42 ) | 0.86 | (.24–3.07) | |
| Other | 3/10 (30) | 0.52 | (.12–2.22) | |
| Housing category | .82 | |||
| Temporary | 23/54 (43) | ref | ref | |
| Unsheltered | 26/58 (45) | 1.10 | (.52–2.31) | |
| Baseline CD4 count | .59 | |||
| < 200 cells/μL | 32/38 (46) | ref | ref | |
| ≥ 200 cells/μL | 17/42 (40) | 0.81 | (.37–1.75) | |
| Substance use disordera | .54 | |||
| Methamphetamine ± other | 41/98 (42) | ref | ref | |
| Opioids ± cocaine/alcohol | 1/3 (33) | 0.70 | (.06–7.93) | |
| Cocaine ± alcohol | 4/7 (57) | 1.85 | (.39–8.73) | |
| Alcohol | 3/4 (75) | 4.17 | (.42–41.5) | |
| Any mental health diagnosis vs none | 36/80 (45) | 1.20 | (.52–2.75) | .67 |
| Mental health diagnosis categoryb | .81 | |||
| Psychotic disorder | 11/21 (52) | 0.83 | (.34–2.02) | |
| Bipolar disorder | 4/9 (44) | 1.01 | (.23–4.45) | |
| Depressive/anxiety disorder | 19/48 (40) | 1.39 | (.47–4.15) | |
| None | 15/34 (44) | ref | ref | |
| Housing change | ||||
| Maintained/improved housing | 34/74 (46) | 1.30 | (.59–2.89) | |
| Worsened/remained homeless | 14/38 (39) | ref | ref |
Abbreviations: CI, confidence interval; POP-UP, Positive-Health Onsite Program for Unstably Housed Populations; ref, reference; VL, viral load.
Mutually exclusive, hierarchical classification of substance use: methamphetamine (± other substances), opioids (± cocaine or alcohol), cocaine (± alcohol), alcohol alone, or none of the above.
Mutually exclusive, hierarchical classification of mental health diagnoses: psychotic disorder with or without other diagnoses, bipolar disorder (± depression or anxiety), depression or anxiety, or none of the above.
DISCUSSION
The POP-UP model at the Ward 86 HIV clinic in San Francisco was purposively designed to address barriers to care engagement for persons experiencing homelessness and was associated with improvement in 12-month HIV viral suppression from 0% to 44%, with 66% achieving viral suppression at least once. This study extends our prior findings that POP-UP achieved HIV viral suppression in 55% of patients over the first 6 months of enrollment [15] and maintained similar levels of viral suppression during the coronavirus disease 2019 (COVID-19) pandemic [25]. Patients maintained high levels of care engagement: over 70% had a visit during each 4-month period of follow-up, despite overlapping barriers of unstable housing, substance use, and mental health conditions.
We attribute success in engaging this hard-to-reach population to the holistic, multicomponent nature of our care model, developed using a theory-informed approach and expressed patient preferences [16, 17]. Two critical, synergistic model components include low-barrier comprehensive medical and social work services without the need for appointments in combination with panel management to proactively identify patients who do not come to clinic and may require additional outreach. Integrated substance and mental health treatment allowed us to address these frequently co-occurring conditions together in the same visit [26]. POP-UP provides low-barrier pharmacologic treatment of substance use disorders, including same-day buprenorphine-naloxone initiation for opioid use disorder, as well as harm reduction counseling and safer use supplies. A psychiatrist is imbedded within our team and available for consultation during weekly case conferences, increasing primary care provider capacity to treat complex psychiatric conditions. We also used financial incentives to motivate care engagement and viral suppression, with incentive amounts that were substantially smaller in value than those used in other incentive studies [27, 28].
While extremely high-risk individuals were able to achieve engagement and viral suppression through POP-UP, treatment outcomes in this population still fall far short of Ending the HIV Epidemic (EHE) targets [29]. First, although POP-UP maintained high levels of care engagement despite a broad array of barriers, over half of patients experienced a ≥90-day gap between clinic visits. While care gaps of this length are expected for stable patients, POP-UP encourages frequent visits to address complex medical and psychosocial issues and provide support. Having a mental health diagnosis reduced the risk of a prolonged gap in care, suggesting that imbedded mental health treatment may have facilitated care engagement, although over half of patients with a mental health diagnosis still had a ≥90-day care gap. Drop-in access and financial incentives also reduce barriers to consistent care engagement, although these interventions were insufficient to avoid long absences from care for many patients.
In addition, many patients were not virally suppressed despite engagement in care. In our cohort, viral nonsuppression was driven entirely by adherence challenges, rather than genotypic resistance. Reasons for adherence difficulties ranged widely and included inability to maintain possession of medications while living on the street, forgetfulness, substance use, mental health, aversion to swallowing pills, low prioritization of HIV treatment, stigma, and denial. Our care model addressed these barriers via a variety of interventions including medication pickup in convenient packaging directly from clinic (medi-sets, bubble packs, etc.), housing referrals, adherence reminders from case managers/care navigators, integrated substance use and mental health care, and relationship-centered care [16, 20].
The high mortality rate in this population is of great concern. Mortality was 9% over 1 year in POP-UP, approximately 5-fold higher than the 2019 crude mortality rate among PWH in San Francisco [3]. Homelessness [30], mental illness [31], and substance use [32] are all associated with increased risk of mortality among PWH, and multimorbidity among these conditions may synergistically increase risk [33]. The majority of deaths in POP-UP were overdoses, either methamphetamine alone or methamphetamine and fentanyl combined. High rates of overdose in POP-UP, and specifically overdose deaths involving both stimulants and opioids, mirror the rising overdose crisis in San Francisco [34] and nationwide [35], particularly among people experiencing homelessness [36] and PWH [37]. Our findings highlighting stimulant use a major risk factor for death is also consistent with prior research among San Francisco homeless and unstably housed women [38]. POP-UP provides evidence-based interventions for opioid use disorder treatment and overdose prevention—although important, these interventions are clearly inadequate for preventing stimulant-related overdoses, which were the most common in this population.
An important consideration is how this type of intensive care model can be sustained and scaled to other jurisdictions. Ryan White funding supports the types of clinical and social services that are included in the POP-UP model (eg, outpatient mental health and substance use treatment, medical case management). The federal government’s commitment to the EHE goals (with funding funneled through the Centers for Disease Control and Prevention, Health Resources and Services Administration, and the National Institutes of Health) will hopefully provide additional funds for these important programs to serve PWH experiencing homelessness. We are planning future costing analysis to quantify the costs required to sustain this care model across clinics, which will aid in justifying further support from EHE initiatives.
This study has several important limitations. Our intervention was not randomized and we cannot directly attribute POP-UP enrollment with improved care outcomes. However, high levels of care engagement following POP-UP enrollment suggest a likely mechanism for observed improvements in HIV viral suppression. Further, one-quarter of patients had missing viral load data at 12 months. We used a conservative approach and assumed that those with missing data were not suppressed, suggesting that suppression may actually be underestimated. Overall, two-thirds attained HIV viral suppression at any point—an improvement compared to 30% who had any suppression in the 12 months prior to enrollment. Although POP-UP offered low-barrier care access, 39% of eligible patients did not enroll—most because they never presented to clinic after they were referred. Enrollment in POP-UP was more successful when facilitated by clinic staff or external partners than when identified via chart review alone, consistent with other studies [39, 40]. Interestingly, patients living on the street and those with a known mental health diagnosis were more likely to link to care in POP-UP. While this may represent confounding by more complete clinical documentation among patients more connected to care, it also suggests the possibility that POP-UP was better able to address barriers to care such as housing status, mental health, and substance use—and less able to address other psychosocial barriers (eg, stigma, denial).
There are a number of additional intervention components that could address persistent suboptimal treatment outcomes. First, out-of-clinic services such as mobile care may help address lack of engagement or gaps in care, particularly for those at highest risk of poor clinical outcomes [41–44]. Second, incorporation of evidence-based interventions for stimulant use, such as contingency management [45, 46], could help reduce the most harmful effects of stimulant use in our population. Finally, greater access to permanent supportive housing is one of the most important needs for our population [47].
CONCLUSIONS
The POP-UP low-barrier, clinic-based HIV primary care model is a promising approach to improving care engagement and HIV viral suppression among PWH with overlapping barriers to care engagement, including homelessness/unstable housing, substance use, and mental health diagnoses. Additional innovations, such out-of-clinic care models and concentrated attention to complications of substance use, are needed to improve HIV care outcomes among this highly vulnerable population.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Disclaimer. Gilead had no role in the interpretation or presentation of these results.
Financial support . This work was supported by Gilead Foundation (grant number IN-US-985-5691 unrestricted investigator-initiated grant to the Ward 86 HIV Program in the Division of HIV, ID and Global Medicine to support implementation and evaluation of the POP-UP program); National Institutes of Health Ending the HIV Epidemic Supplemental Grant (grant number P30 AI027763 to M. G., UCSF-Gladstone Center for AIDS Research); National Institute of Allergy and Infectious Diseases training grant (grant number 5T32AI060530-13 to M. D. H.); and Benioff Homelessness and Housing Initiative (BHHI) UCSF Resource Allocation Program Award (to M. D. H).
Supplement sponsorship. This article appears as part of the supplement “Homelessness and Infectious Diseases: Understanding the Gaps and Defining a Public Health Approach,” sponsored by the Centers for Disease Control and Prevention.
Supplementary Material
Contributor Information
Matthew D Hickey, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Elizabeth Imbert, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Ayesha Appa, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Jan Bing Del Rosario, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Elizabeth Lynch, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
John Friend, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Rodrigo Avila, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Angelo Clemenzi-Allen, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA; Department of Public Health, Jail Health Services, San Francisco, California, USA.
Elise D Riley, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Monica Gandhi, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
Diane V Havlir, Division of HIV, Infectious Diseases, and Global Medicine, Department of Medicine, University of California, San Francisco, California, USA.
References
- 1. Clemenzi-Allen A, Neuhaus J, Geng E, et al. Housing instability results in increased acute care utilization in an urban HIV clinic cohort. Open Forum Infect Dis 2019; 6:ofz148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Doshi RK, Milberg J, Jumento T, Matthews T, Dempsey A, Cheever LW. For many served by the Ryan White HIV/AIDS program, disparities in viral suppression decreased, 2010–14. Health Aff (Millwood) 2017; 36:116–23. [DOI] [PubMed] [Google Scholar]
- 3. Colfax G, Philip S, Enanoria W, Hsu L. HIV epidemiology: annual report, 2020. San Francisco Department of Public Health, 2021. [Google Scholar]
- 4. Clemenzi-Allen A, Geng E, Christopoulos K, et al. Degree of housing instability shows independent ‘dose-response’ with virologic suppression rates among people living with human immunodeficiency virus. Open Forum Infect Dis 2018; 5:ofy035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dombrowski JC, Simoni JM, Katz DA, Golden MR. Barriers to HIV care and treatment among participants in a public health HIV care relinkage program. AIDS Patient Care STDS 2015; 29:279–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holtzman CW, Shea JA, Glanz K, et al. Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen's behavioral model. AIDS Care 2015; 27:817–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yehia BR, Stewart L, Momplaisir F, et al. Barriers and facilitators to patient retention in HIV care. BMC Infect Dis 2015; 15:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Riano NS, Borowsky HM, Arnold EA, et al. HIV testing and counseling at U.S. substance use treatment facilities: A missed opportunity for early identification. Psychiatr Serv 2021; 72:1385–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mangurian C, Cournos F, Schillinger D, et al. Low rates of HIV testing among adults with severe mental illness receiving care in community mental health settings. Psychiatr Serv 2017; 68:443–8. [DOI] [PubMed] [Google Scholar]
- 10. Momenzadeh A, Shumway M, Dong BJ, Dilley J, Nye J, Mangurian C. Patterns of prescribing antiretroviral therapy upon discharge to psychiatry inpatients with HIV/AIDS at a large urban hospital. Ann Pharmacother 2021; 55:452–8. [DOI] [PubMed] [Google Scholar]
- 11. Riley ED, Moore K, Sorensen JL, Tulsky JP, Bangsberg DR, Neilands TB. Basic subsistence needs and overall health among human immunodeficiency virus-infected homeless and unstably housed women. Am J Epidemiol 2011; 174:515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Flentje A, Shumway M, Wong LH, Riley ED. Psychiatric risk in unstably housed sexual minority women: relationship between sexual and racial minority status and human immunodeficiency virus and psychiatric diagnoses. Womens Health Issues 2017; 27:294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tsai AC, Weiser SD, Dilworth SE, Shumway M, Riley ED. Violent victimization, mental health, and service utilization outcomes in a cohort of homeless and unstably housed women living with or at risk of becoming infected with HIV. Am J Epidemiol 2015; 181:817–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Garcia ME, Schillinger D, Vittinghoff E, et al. Nonpsychiatric outpatient care for adults with serious mental illness in California: who is being left behind? Psychiatr Serv 2017; 68:689–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Imbert E, Hickey MD, Clemenzi-Allen A, et al. Evaluation of the POP-UP programme: a multicomponent model of care for people living with HIV with homelessness or unstable housing. AIDS 2021; 35:1241–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Conte M, Eshun-Wilson I, Geng E, et al. Understanding preferences for HIV care among patients experiencing homelessness or unstable housing: a discrete choice experiment. J Acquir Immune Defic Syndr 2020; 85:444–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Imbert E, Hickey MD, Del Rosario JB, et al. Heterogeneous preferences for care engagement among people with HIV experiencing homelessness or unstable housing during the COVID-19 pandemic. J Acquir Immune Defic Syndr 2022; 90:140–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Salloum RG, Shenkman EA, Louviere JJ, Chambers DA. Application of discrete choice experiments to enhance stakeholder engagement as a strategy for advancing implementation: a systematic review. Implement Sci 2017; 12:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wood TJ, Koester KA, Christopoulos KA, Sauceda JA, Neilands TB, Johnson MO. If someone cares about you, you are more apt to come around: improving HIV care engagement by strengthening the patient-provider relationship. Patient Prefer Adherence 2018; 12:919–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dombrowski JC, Ramchandani M, Dhanireddy S, Harrington RD, Moore A, Golden MR. The max clinic: Medical care designed to engage the hardest-to-reach persons living with HIV in Seattle and King County, Washington. AIDS Patient Care STDS 2018; 32:149–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tegger MK, Crane HM, Tapia KA, Uldall KK, Holte SE, Kitahata MM. The effect of mental illness, substance use, and treatment for depression on the initiation of highly active antiretroviral therapy among HIV-infected individuals. AIDS Patient Care STDS 2008; 22:233–43. [DOI] [PubMed] [Google Scholar]
- 23. Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis 2013; 57:1164–71. [DOI] [PubMed] [Google Scholar]
- 24. Satagopan JM, Ben-Porat L, Berwick M, Robson M, Kutler D, Auerbach AD. A note on competing risks in survival data analysis. Br J Cancer 2004; 91:1229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hickey MD, Imbert E, Glidden DV, et al. Viral suppression during COVID-19 among people with HIV experiencing homelessness in a low-barrier clinic-based program. AIDS 2021; 35:517–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Conway FN, Rountree MA, Jones KV. Serving the co-morbid mental health and substance use needs of people with HIV. Community Ment Health J 2021; 57:1328–39. [DOI] [PubMed] [Google Scholar]
- 27. Metsch LR, Feaster DJ, Gooden L, et al. Effect of patient navigation with or without financial incentives on viral suppression among hospitalized patients with HIV infection and substance use: a randomized clinical trial. JAMA 2016; 316:156–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. El-Sadr WM, Donnell D, Beauchamp G, et al. Financial incentives for linkage to care and viral suppression among HIV-positive patients: a randomized clinical trial (HPTN 065). JAMA Intern Med 2017; 177:1083–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA 2019; 321:844–5. [DOI] [PubMed] [Google Scholar]
- 30. Spinelli MA, Hessol NA, Schwarcz S, et al. Homelessness at diagnosis is associated with death among people with HIV in a population-based study of a US city. AIDS 2019; 33:1789–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ebuenyi I, Taylor C, O'Flynn D, Matthew Prina A, Passchier R, Mayston R. The impact of co-morbid severe mental illness and HIV upon mental and physical health and social outcomes: a systematic review. AIDS Care 2018; 30:1586–94. [DOI] [PubMed] [Google Scholar]
- 32. Doshi RK, Byrne M, Levy M, et al. Association of substance use disorders with engagement in care and mortality among a clinical cohort of people with HIV in Washington, DC. AIDS Behav 2021; 25:2289–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jones AA, Gicas KM, Seyedin S, et al. Associations of substance use, psychosis, and mortality among people living in precarious housing or homelessness: a longitudinal, community-based study in Vancouver, Canada. PLoS Med 2020; 17:e1003172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Appa A, Rodda LN, Cawley C, et al. Drug overdose deaths before and after shelter-in-place orders during the COVID-19 pandemic in San Francisco. JAMA Netw Open 2021; 4:e2110452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Imtiaz S, Nafeh F, Russell C, Ali F, Elton-Marshall T, Rehm J. The impact of the novel coronavirus disease (COVID-19) pandemic on drug overdose-related deaths in the United States and Canada: a systematic review of observational studies and analysis of public health surveillance data. Subst Abuse Treat Prev Policy 2021; 16:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cawley C, Kanzaria HK, Zevin B, Doran KM, Kushel M, Raven MC. Mortality among people experiencing homelessness in San Francisco during the COVID-19 pandemic. JAMA Netw Open 2022; 5:e221870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Appa A, Rowe C, Hessol NA, Coffin P. Beyond overdose: drug-related deaths in people with and without HIV in San Francisco, 2007–2018. Open Forum Infect Dis 2020; 7:ofaa565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Riley ED, Cohen J, Shumway M. Overdose fatality and surveillance as a method for understanding mortality trends in homeless populations. JAMA Intern Med 2013; 173:1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dombrowski JC, Hughes JP, Buskin SE, et al. A cluster randomized evaluation of a health department data to care intervention designed to increase engagement in HIV care and antiretroviral use. Sex Transm Dis 2018; 45:361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sachdev DD, Mara E, Hughes AJ, et al. Is a bird in the hand worth 5 in the bush?’: a comparison of 3 data-to-care referral strategies on HIV care continuum outcomes in San Francisco. Open Forum Infect Dis 2020; 7:ofaa369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Aniruddha Hazra MP, Schneider J. Abstract PE16.08 No place like home: engaging HIV and sexual health carethrough a mobile medical unit. 4th HIV Research for Prevention Conference. Vol. 24. Virtual: Wiley, 2021:134. [Google Scholar]
- 42. Ryan Dono MY, Lee R, Bositis A, Bositis C. Implementation of a mobile buprenorphine clinic. 50th Annual Conference of the American Society of Addiction Medicine, ASAM 2019. Orlando, FL, United States. J Addict Med 2019; 13:E9. [Google Scholar]
- 43. Carter J, Zevin B, Lum PJ. Low barrier buprenorphine treatment for persons experiencing homelessness and injecting heroin in San Francisco. Addict Sci Clin Pract 2019; 14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Borne D, Tryon J, Rajabiun S, Fox J, de Groot A, Gunhouse-Vigil K. Mobile multidisciplinary HIV medical care for hard-to-reach individuals experiencing homelessness in San Francisco. Am J Public Health 2018; 108:S528–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Carrico AW, Gόmez W, Jain J, et al. Randomized controlled trial of a positive affect intervention for methamphetamine users. Drug Alcohol Depend 2018; 192:8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, Amass L. Contingency management among homeless, out-of-treatment men who have sex with men. J Subst Abuse Treat 2010; 39:255–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Riley ED, Hickey MD, Imbert E, Clemenzi-Allen AA, Gandhi M. Coronavirus disease 2019 (COVID-19) and HIV spotlight the United States imperative for permanent affordable housing. Clin Infect Dis 2021; 72:2042–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.