Abstract
There is a scarcity of research on contraceptive decision-making and use among Ethiopian students in higher education institutions. As young college students are more exposed to sexual encounters and premarital sex, it is imperative to look at their contraception decision-making and use. This qualitative study aimed to explore the experiences of young college men and women in sexual relationships regarding the decision-making for contraceptive use at Addis Ababa University, Ethiopia. A Phenomenological qualitative study design was employed for this study. The participants were recruited using purposeful sampling. Twenty eligible study participants [10 female and 10 men] were interviewed face-to-face. To be selected for the study, participants had to be in a relationship for at least 6 months after joining the university, attending a regular program, and were able to offer detailed information about their sexual encounters and contraceptive decision-making and use. Data were analyzed at the same time as data were collected from February 2 through March 15, 2022. Thematic analysis was done for the study, which comprises 3 stages: data reduction, data display, and data conclusion. Both a priori codes (from the query guide) and emerging inductive codes were used in the study. The data analysis from the in-depth interviews revealed 3 overarching themes consistent with the study’s aims, including: types of relationships, level of communication, contraceptive decision-making with a partner, and contraception use. In this study’s analysis, the first emerged theme was the types of relationships, which may be divided into 2 categories: dating/causal and intimate partnerships. Participants described their relationship with their partner as intimate and exciting. According to our data, men and women in intimate relationships reported emotional closeness and connectedness. Mostly they make an open discussion about different things including contraception use and made decisions together, they spent a good time together and have mutual trust. They also mentioned that mostly their discussion involves issues about having a happy future life together. On the contrary, however, participants in the causal relationship claimed that while they now spend time together and enjoy themselves, they lack open communication and trust in their relationship. There is less commitment and accountability, and the majority of them do not have a relationship goal, according to their reports. The second theme that emerged during the analysis of the in-depth interview was the level of communication and decision-making with the partner regarding contraception. Within the theme, there is 2 categories communication with partner and decision-making about contraception use. The study participants felt comfortable discussing their sexuality and contraception use in the current study. Most discussions were believed to be initiated by the male partner, and the majority of the decisions were made jointly, according to our findings. The degree of intimacy with their partner in a relationship, their partner’s desire, and contraceptive-related concerns are all factors that impact contraception use decision-making, according to the study’s findings. The majority of male and female interview participants stated that the length of a relationship was an important consideration when deciding whether or not to use contraception. Participants in stable long-term relationships were more likely to choose protection than those in short-term relationships. The usage of contraception, which encompasses 5 linked categories, emerged as the third theme from the in-depth interview analysis: types of contraception used, concerns and doubts about adverse effects of contraception use, reasons for contraception use, trust between partners determines contraception use, barriers to contraception use. The findings of this study demonstrated that communication and using contraception is a common practice and is accepted as a positive thing on campus, mostly to prevent unexpected pregnancy. The major obstacles to using contraception are believed to be a lack of available contraceptives on campus and cost-related concerns. Most male partner access and bring contraceptives from private drug stores for their girlfriends. The university administration and other interested stakeholders need to pay close attention to efforts to increase the use of contraceptives among high-risk young university women while helping guide actions to involve young men in making contraceptive decisions on campus.
Keywords: Decision-making, contraception use, college students, dating relationships, Ethiopia
What do we already know about this topic?
Premarital sex is prevalent among young college students in Ethiopia.
Unintended pregnancies were common among single female college students in Ethiopia.
How does your research contribute to the field?
According to the findings, utilizing contraception is a popular practice and is viewed favorably on campus, mostly to prevent unplanned pregnancies.
The main barriers to utilizing contraception include reportedly a scarcity of contraceptives on campus and financial considerations
What are your research’s implications for theory, practice, or policy?
Programs to increase accessing contraception use for high-risk young college women should be prioritized, and initiatives to involve young men in using condoms to prevent STIs in a college setting should also be supported.
Introduction
Unintended pregnancies occur more often in adolescents and young girls than in adults, and account for more than 40% of all pregnancies worldwide, with 25% occurring in Africa. 1 In 2019 there were 28% of unwanted pregnancies in Ethiopia. 2 According to the Ethiopian Demographic Health Survey [EDHS] 2016, 13% of women aged 15 to 19 have started having children. 3 Optimal contraceptive uptake and use could avert the burden of unintended pregnancies and abortions by one-third.1,4 In young adults (15-24 years), STI cases account for more than 60% of all cases worldwide). 5 The usage of condoms is a well-recognized method for reducing undesirable health effects, such as STIs and HIV infection. 6
Implementing measures that can promote access to and utilization of STI/HIV and pregnancy prevention techniques is required to reduce the burden of these sexual and reproductive health problems (such as HIV and STI acquisition, and pregnancy complications) among the college student population.
The usage of contraceptives is positively correlated with increased closeness and communication within a partnership. 7 According to studies, young men who exhibit more “couple-like behaviors” with partners before sex and women who feel more comfortable engaging with male partners begin using contraception more frequently.7,8 Making decisions about contraception use is a very contextual process in which women take into account aspects like side effects, personal values, relationship status, and/or preferred prescription types.6,9 Young men also continue to use condoms at a comparatively low rate in sub-Saharan Africa, particularly Ethiopia, which was 20%. 10 The usage of condoms is linked to male authority and dominance in relationships. 8
Although gender inequality in romantic relationships among college students is widely documented, little study has looked at how students’ use of contraceptives, behaviors, and decision-making might both reflect and contribute to inequality. 11 The majority of the current research on collegiate sexual culture, contraception, and reproduction focuses on women, despite calls for more study of men.11,12 The negotiation of contraceptive use and reproductive decision-making, particularly from the perspective of men, is a substantial and under-discussed topic in college students’ sexual life.13,14
Given the unequal burden on young college women and the fact that the female-controlled birth control pill is the most widely used reversible method of contraception in Ethiopia, researchers and laypeople often assume that men are mostly unconcerned in contraceptive decisions and use. This notion has largely remained unsubstantiated since few studies have examined the gendered dynamics of family planning in the setting of colleges. To actively involve young people in the choice and use of contraceptives in academic contexts, evidence is required. This would require a deeper understanding of the sexual and reproductive history of men and women as well as the process of telling one another about these experiences, which quantitative studies might not be able to provide. This qualitative study thus aimed to explore the experiences of young college men and women in sexual relationships regarding the decision-making for contraceptive use at Addis Ababa University, Ethiopia.
Methods
Study Setting
The study was carried out at 2 purposively chosen colleges of Addis Ababa University: the College of Natural and Computational Sciences at Arat Kilo Campus and the College of Health Sciences at Sefere Selam Campus, from February 14 to April 30, 2022.
Study Design, Participants, and Eligibility Criteria
A Phenomenological qualitative study design was employed for this study. The study included 20 eligible participants, with 10 men and 10 women.
The participants were recruited between January 15 to 30, 2022. The participants were recruited using purposeful sampling. Participants had to be in a relationship for at least 6 months after enrolling in the university, be enrolled in a regular undergraduate program, be 18 years and above, and be able to provide rich information about their sexual encounters and decision-making and use of contraceptives to be chosen for the study. The gender officer at the designated campuses addressed participants who met these eligibility requirements, explained the purpose and methods of the study, and invited them to participate in the study. The researcher approached each participant once they had agreed to participate and then followed them for the interview.
Data Collection
Individual face-to-face interviews were performed to get the data. The primary author and one qualified female research assistant conducted the interviews. The research assistant had a strong foundation in qualitative research and was a sociologist. Using an Amharic interview guide, the interview was done in Amharic in the gender office. The interview guide was included as a “Supplemental File 1” The current study explored the perspectives of men and women, including how they use contraception, how they decide whether to use it or not, what influences their decision, and how much communication they have with their partner. The researchers tested the interview guide on 2 women who met the criteria for eligibility. However, the findings were not included in the main study. The interview guide was enriched by the researchers following the pilot study. The interviews were held in the designated gender officer’s room to protect the study participant’s privacy and confidentiality. The research assistant audio-recorded the interviews and made notes with the participants’ explicit consent to preserve the subjects’ original reports of their responses. Upon reaching saturation, which was determined by preliminary data analysis, the interviews were completed with 20 participants.
Data Analysis
The participants’ socio-demographic data were reported using descriptive statistics. The primary author verbatim transcribed the field notes and recorded audio data. Both a priori codes (from the query guide) and emerging inductive codes were used in the study. The principal advisor, Sendo, EG, then reviewed the data that had previously been coded and merged the major and sub-themes. Emerging inductive codes were used in the study. In the thematic data analysis, 3 interrelated stages were involved, namely data reduction, data display, and data conclusion. The thematic approach to analysis involved the construction of textual data, the description of data themes, the coding of the themes, and the interpretation of the structure and content of the themes. Lastly, quotes from the statements of the participants were used to illustrate the study’s main themes.
The Trustworthiness of the Study
Before the main study, a pre-test was completed to assess the interview guide’s validity and reliability and make any necessary corrections. One of the various techniques utilized to ensure the credibility of the report was the employment of the same interview guide throughout the whole study.
An audit trail was used to use as proof of the techniques used in the report. To ensure that the research findings may be applied to situations with a similar context, a full explanation of the study area, methodology, and sample history was provided. Participants received their data back so they could verify and validate their responses, ensuring the accuracy of the results. The researchers’ assertion of a non-biased study design and use of reflexivity increased the veracity of the findings. By using bracketing, the researchers made sure that their opinions and experiences about the subject of the study did not affect the gathering and processing of data. The backgrounds of the researchers had no impact on the methods used to collect and analyze the data. Finally, the study’s reporting complied with all 32 Consolidated criteria for reporting qualitative research. 15
Ethics Approval and Consent to Participate
The School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University’s Research and Ethical Review Committee (IRB) was consulted for approval to proceed with this study ethically. All participants gave their signed written consent to the interviews after receiving full disclosure from the PI. The fact that participation in this study was entirely voluntary was stressed. The identities and other private details of all respondents were also kept confidential.
Research Findings
Characteristics of Participants in the Study
There were a total of 20 participants in the study, including 10 men and 10 women who were undergraduate students. The age range of the entire sample ranged between 19 and 26 years, with a mean age of 22 years. Fourth-year undergraduate students made up half of the participants.
Emerged Themes
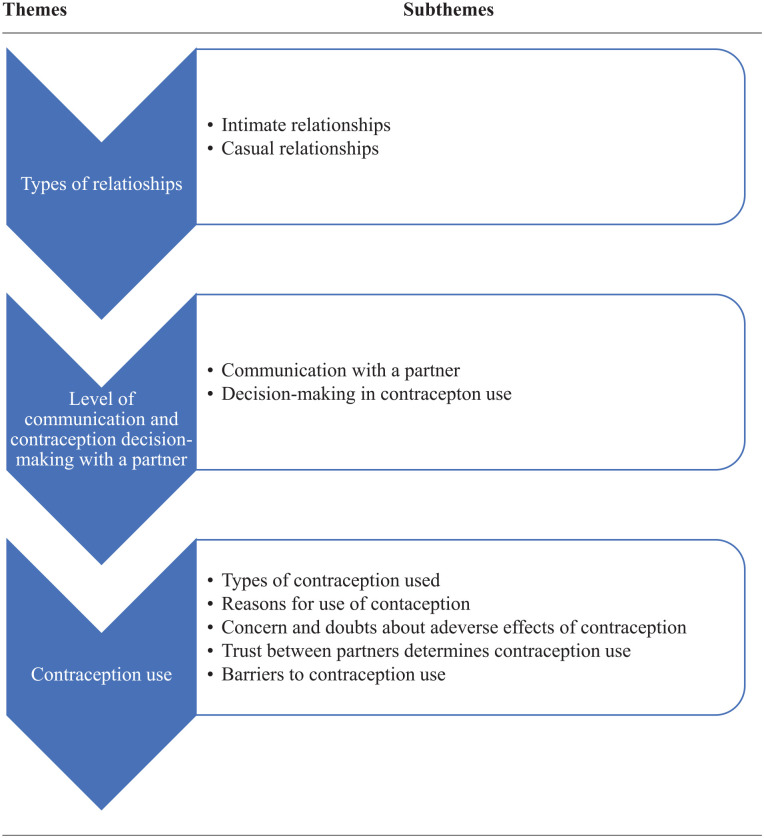
The analysis of the data from the in-depth interviews revealed 3 overarching themes that are consistent with the study’s aims, namely: types of relationships, level of communication, contraceptive decision-making with a partner, and contraception use (Figure 1).
Figure 1.
Schematic presentation of emerged themes and subthemes about contraceptive decision-making among young college students.
Theme 1: Types of Relationships
In this study’s analysis, 2 categories of relationships—intimate relationships and casual dating—made up the first overarching theme.
Intimate Relationships
Participants described their relationship with their partner as intimate and exciting, including emotional closeness and connectedness. Mostly they make an open discussion about different things, including contraception and they made decisions together, spend time together, and have mutual trust. They also mentioned that mostly their discussion involves issues about having a happy future life together. Sample responses include:
“We’ve been together for a year and have had a happy relationship. We spent time watching movies and talking about our future goals, which included getting married and seeing our children.” [Female participant #1, age 21 years]
“We’ve been dating for six months and were having an exciting time together. We spent some time discussing our plans and lives. We intend to have a type of love that would lead to marriage and family formation.” [Female Participant # 2, age 23 years]
Being in a committed relationship helps individuals to discuss contraception openly, voice their opinions freely, including which method they should use or finds most comfortable, and eventually make a decision together. Sample responses include:
“I had been in a relationship for six months and was quite happy with it. Every time we get together, we discuss our future goals to build a fulfilling relationship. We also discuss family planning issues, such as which method we should use or find most comfortable. . . .. I always use a condom properly and have great faith in it. [Male Participant #16, age 20 years]
“It was lovely to be in a committed relationship for ten months. Whenever we get together we discuss family planning issues such as condoms and post-pills. I occasionally buy her post-pills because condoms do not soothe her. We usually make decisions together, but I do give her the option to make her own decisions . . ..” [Male Participant #17, age 20 years]
Casual Relationships
Participants in casual relationships claimed that while they at this moment spend time and enjoy themselves, they lack communication and reciprocal trust in their relationships. Their interactions are unimportant to their relationship, there is less commitment and accountability, and the majority of them do not have a relationship goal, according to their reports. Sample responses include:
“We had been in a good relationship for seven months, but we are no longer together. We spent some time talking about our everyday routines rather than our romantic relationships or future goals. . . We didn’t have any goals in mind, but we both had feelings . . ..” [Female participant #3, age 22.]
“I’ve been a student at this university for four years. I had a lot of girlfriends in the past, even more than five. I have a new girlfriend at the moment” [Male participant #5, age 23 years]
“I had previously been in a relationship for a year, but we are no longer together. We spent more time chatting about class and family than our relationships or plans. . . and we never brought up the subject of contraception. Our sexual relationships then deteriorate, and we become estranged. . .” [Female Participant # 14, age 19 years]
“At the time, I was in a six-month relationship that appeared exciting. We are no longer together, unfortunately. When we initially met, we were just classmates, but after that, we became lovers. It all started because I adored her” [Male participant 18, age 21 years]
Theme 2: Level of Communication and Contraception Decision Making
The second theme that emerged during the analysis of the in-depth interview was the level of communication and decision-making with partners. Within the theme, there is 2 categories communication with partner and decision-making about contraception use.
Communication With Partner
According to our data, men and women in close relationships feel comfortable discussing their sexuality and contraception use. Most discussions were believed to be initiated by the male partner, and the majority of the decisions were made jointly, according to our findings. Sample responses include:
“We spent a long time discussing our sexuality and contraception use. My boyfriend initiates the dialogue, but he values my point of view and is very supportive of me. . ..” [Female participant # 1, age 21 years]
“. . .As long as we are in an intimate relationship, both of us are accountable for making joint decisions concerning contraception use. . .” [Female participant #12, age 19 years] .
Some women, on the other hand, are embarrassed to express their thoughts and initiate conversations about sexuality and contraception. They believe in open communication, yet they are rarely involved in decision-making due to a lack of awareness. As some female partners don’t know where to get the medicines, it’s their boyfriends that go out and buy them post-pills. Some participants stated that discussing health checkups, sexuality, and contraception use must be a pre-request for dating and believes female partner mostly initiate such topics. Contraception is used more often the more this issue is discussed with a partner, regardless of who initiates the talk as long as their position is supported. However, their level of contraceptive knowledge may influence their decision-making. Here are a few instances of responses:
In a sexual relationship, I believe both sides are accountable for contraception use. When it comes to sexuality and contraception, I’m completely naive. But my boyfriend initiates the conversation and tells me a great deal about these subjects. He advises that I use contraception to avoid becoming pregnant so that I can complete my education. . . I’m not sure where I’ll be able to get the drugs. So, he’s the one who goes out and buys my post-pills. . . [Female Participant # 11, age 25 years] .
“Young men and women should discuss their sexuality and use of contraceptives in a relationship. Before we start dating, we need to discuss health checkups and how to start a relationship. . . In a relationship, I believe women often initiate a discussion about sexual matters and contraception use.” [Female participant # 2, age 23 years]
Decision-Making in Contraception Use
The degree of intimacy with their partner in a relationship, their partner’s desire, and contraceptive-related concerns are all factors that impact contraception use decision-making, according to the study’s findings. The majority of male and female interview participants stated that the length of a relationship was an important consideration when deciding whether or not to use contraception. Participants in stable long-term relationships were more likely to choose protection than those in short-term relationships. Sample responses include:
Whether you take contraception or not depends on how close you are to your partner. For instance, “I’ve been dating for 10 months and we want to get married; I’m extremely delighted with it. So, we talk a lot about sexuality and birth control. As long as we are in an intimate relationship, both of us are accountable for making decisions concerning contraception use.” [Female participant # 12, age 19 years] .
“To be honest, I don’t believe most college students, including myself talk about sexuality and contraception in their stable long-term relationships. Most of the time, they don’t talk openly since she may believe she has taken his comfort [boyfriend] for granted. So, I believe the type of relationship influences their decision-making.”. . .. The longer the relationship the better use of contraception. [Female participant #4, age 22 years] .
“We usually make decisions together, but I do give her the option to make her own decisions on some occasions. . ..” As condoms do not bring comfort, I sometimes purchase post-pills for her. [Male Participant # 17, age 20 years]
The frequency of having sex with a partner was also mentioned as a factor to consider while choosing a contraceptive. Sample responses include:
“I’ve been in a relationship for a year and I’m happy to be in a stable condition. He is the one who makes the majority of my contraceptive decisions. Because we have sex so frequently, he buys post-pills for me. . . I admire him and want to marry him, but he doesn’t appear to be ready yet. . ..” [Female participant # 13, age 19 years] .
According to the findings, women also considered themselves as they are more responsible for contraception use so, their point of view should weigh more and be respected due to the reason that most of the time, they are the ones who take the burden and got hurt the most. Sample responses include:
“When we get together, we chat about dating and contraception. Because my point of view is more essential in the decision-making process, I am often the one who makes contraceptive use decisions; I am the one who will be held responsible if a pregnancy arises. . ..” [Female Participant # 1, age 21 years]
“. . ..So, in contraceptive decision-making, I have the final says. Women are more responsible for contraception use in a sexually active relationship. It is their responsibility, as I already indicated if the pregnancy occurs. . . they have a disproportionate share of the blame. . ..” [ Female participant # 2, age 23 years]
Theme 3: Contraception Use
The third theme that emerged from the in-depth interview analysis was contraception use which has 5 categories that are related to it those are types of contraception used, concerns and doubts about adverse effects of contraception use, reasons for contraception use, trust between partners determines contraception use, barriers to contraception use.
Types of Contraceptive Methods used:
According to the study, most college students support contraceptive use and consider it a positive thing to avoid pregnancy. They mostly prefer short-acting contraceptives over the long-term. Most of the students use the post-pill because they assume it is easy to use and reliable. A participant who is 21 years old claimed that condoms are less often used; she uses medications [Post pills] to prevent pregnancy, which her partner purchases for her. Sample responses include:
“College students are the primary users of emergency medications (sometimes known as “post-pills”). My lover routinely buys it from a pharmacy. Condoms were likewise infrequently used by men. . .If a pregnancy occurs; I am the one who will be held accountable. So, I have used it [Pills].” [Female participant # 1, age 21 years]
Meanwhile, a 22-year-old male participant stated that he uses a condom because he feels more at ease with it and that he is not sure if she likes it or not. Sample responses include:
“I feel more comfortable with condoms than I would without them, but I’m not sure how she feels. . ..” [[Male participant # 19, age 22 years].
Even though she thinks implants are safe and effective, one young woman reported that she prefers to use oral contraceptives (OCP). She uses short-acting contraceptives to prevent pregnancy despite having other choices and preferences. Sample responses include:
“Implants are regarded to be both safe and effective. However, I have utilized oral contraceptive pills [OCP] as a short-term strategy though it may be forgotten, placing you at risk of becoming pregnant.” [Female Participant # 2, age 23 years]
Concerns and Doubts About Adverse Effects of Contraception Use
All of the women had previously used emergency contraceptives, but they were worried about the long-term risks of utilizing this method excessively. They also claimed that their boyfriends were the ones who first proposed utilizing emergency contraceptive pills. Sample responses include:
“I am worried about future infertility if I use Postinor too regularly or more than twice per month.” [Female participant # 4, age 21 years]
“One of the reasons why long-term contraceptives are not used is the fear of side effects [infertility].” [Female participant # 1, age 21 years]
“There is a myth that if you utilize contraception, you will never have a child. I am not sure if it is right or wrong. So, I don’t want to use it, but I do take post-pills after having sex with my lover. . ..” [Female participant # 11, age 25 years] .
Reasons for Contraception Use
Most of the young college women who participated in this study gave their justifications for utilizing contraceptive methods; the dread of unintended pregnancy was the most often cited example; they don’t seem to care about other STDs like HIV/AIDS and HPV. Sample responses include:
“Many college students, like me, were concerned about getting pregnant . . .. not sexually transmitted infections. I oppose abortion treatment as a method of family planning. As a result, I prefer to take regular pills. I’ve never taken long-term birth control because I’m afraid of the adverse effects [infertility].” [Female participant #1, age 21 years]
“In a sexually intimate relationship, we are both responsible for contraception use. To assist her finish her education, we need to prevent unwanted pregnancies. Pregnancy is more commonly feared than sexually transmitted diseases. . .” [Male participant # 5, age 23 years]
Trust Between Both Partners Determines Contraception Use
One of the indicators of contraceptive use and decision-making is relationship trust. Having several sexual partners has an impact on contraception use, such as which method to use or whether to consider dual protection. Sample responses include:
“Contraception use is influenced by having several partners. If a person has three or four partners, for example, he may need to use a condom in addition to the pill because having an affair with more people increases the risk of sexually transmitted illnesses. . ..” [Female participant #1, age 21 years]
Some participants asserted that both partners must be committed to their relationship, share equal responsibility, and trust one another before participating in sexual activity and contraception use. Sample responses include:
“Young women and men should consider having a long-term intimacy and trust in a relationship before using family planning methods. . ..” [Female participant #3, age 22 years] .
“The commitment of a partner to the relationship is vital to me. For your future relationship as a partner, you place your trust in someone who is committed to you. For example, if he [boyfriend] is a regular partner, he may be faithful to his girlfriend and supportive of contraception use or barrier method [ex. Condoms” [Female participant # 4, age 21 years]
A 22-year-old male participant claimed to trust his partner, feel deeply responsible for their relationship, and protect his girlfriend from getting pregnant by giving her post-pill medication:
“In a sexual relationship, both men and women are responsible for using contraception. I always get the post-pills and meet her for sex. Yes, we must avoid pregnancy for her to finish her education. . . I trust her very much and I feel she also does. . .” [Male participant # 20, age 22 years]
Barriers to Contraception Use
According to the data, study participants listed a variety of factors as barriers to contraception usage, the most common of which was a shortage of contraception supplies on campus. The study found that the Sidist Kilo campus is the only place where condoms are distributed to boys. Sample responses include:
“The majority of college students want to take contraception to avoid becoming pregnant. But contraception is not available on campus in the student clinic. Most of the time, my boyfriend gets it [Pills] from the drugstore outside.” [Female participant #1, age 21 years]
The only location where condoms are provided to boys is at the Sidist Killo campus. For boys, there are no condoms at our college. Since women are embarrassed to do so, boyfriends purchase pills or condoms from a private pharmacy. [Male participant #5, age 23 years].
The majority of participants [14/20] also stated that the price of contraception is a barrier and that it is more expensive to get it from private pharmacies. Usually, the male partner is the one to buy his female partner’s contraceptive pills. Sample responses include:
“. . .students from low socioeconomic backgrounds cannot afford to purchase contraception from a private drug store. . ..” [Female participant # 4, age 22 years] .
“After two years in this college, I still don’t know where I can get contraceptives; my partner purchases them for me from a private pharmacy. The majority of college students engage in sexual activity, but they lack the funds to purchase condoms and contraceptives, which need to be readily available on campus or in the student clinic” [Female participant # 12, age 19 years].
Discussion
The purpose of this study was to investigate how young college-aged people in sexual relationships felt about the choice to use contraception in Ethiopia. The participants in our survey classified their relationships under the more general categories of casual and committed partnerships while using a variety of notions for sexual relations. The current study discovered that intimate or causal relationships affected Ethiopian college women’s choice to use contraception. The study’s findings indicate that intimate sexual relationships tend to have more open conversations regarding contraception than casual ones, which results in collaborative decision-making. This finding is in line with the previous studies,8,16 which reported that contraception-related conversations are more common in committed relationships than in casual ones, according to a study done in San Francisco and Denver. This result is consistent with a recent study, which found that less communication and decision-making occur between partners in more casual relationships. On the contrary, men and women in close relationships, according to our data, feel comfortable discussing their sexuality and contraception use. Most discussions were believed to be initiated by the male partner, and the majority of the decisions were made jointly, according to our findings.
Our study contributes to our understanding of the reproductive choices made by sexually active adolescents and young adults. According to the study’s findings, factors influencing the decision to use contraception include the degree of intimacy a person has with their partner in a relationship, their partner’s desire, and any concerns about using contraception. For example, most of the young women in our study reported worries about using hormonal contraceptives, especially “post-pills.” The fear that using contraceptives would lead to infertility was the most often cited scenario. This is similar to previous studies,6,9,13 which found that research participants thought about a range of factors when choosing to use contraception, including side effects, personal values, relationship status, and/or preferred medication. Our study’s findings show that choosing whether or not to take contraception is influenced by the length of a relationship. Short-term relationship participants were less likely to choose protection than participants in stable long-term relationships.
The usage of emergency contraceptive pills was the method that all of the women preferred the most out of all the contraceptive methods they had tried, according to a qualitative study from Vietnam, 17 which is in line with the current study, which found that the majority of the college students favorably support the use of contraceptives. However, most of them favor quick-acting contraceptives, such as “post-pills” or emergency drugs, which is consistent with a prior study from Addis Ababa, Ethiopia, 18 which revealed that 12.9% of college-aged women had used emergency contraception, with oral tablets being the most popular form (93.3%). The study also showed that risky sexual behavior is common among the participants. Many college students lack basic knowledge about sexual health, and they often engage in sexual behaviors that put them at risk for unfavorable health effects. 19 Our analysis also showed reasons specific to young people for utilizing contraception. For instance, in the present study, most of the research participants were motivated to use contraceptives to avoid unplanned pregnancy rather than the desire to avoid sexually transmitted diseases (STDs), including HIV. Male participants in our study also stated that wearing condoms during sexual activity was less likely for them to trust their partners. Students will continue to engage in unsafe sexual networks and behaviors if regular condom use remains low, which will accelerate the spread of HIV and STDs. These findings demonstrate a very high risk among college students and call for more strong action to increase awareness and prevent both unintended pregnancies and STDs. Dual contraceptive use is often regarded as a means to reduce these negative health impacts. 6 Undergraduate university students make up a significant population that is exposed to a variety of unsafe behaviors due to their young age. 10 The majority of them are unmarried, young adults who are prone to excitement and the permissive environment of college life, which makes them more likely to engage in high-risk sexual behavior.20,21 These young people who engage in risky behavior—drinking alcohol, smoking cigarettes, or using illegal drugs—have been linked to higher risks of sexual activity, multiple sexual partners, and reduced condom use.10,20,21 Our findings show that there is a high level of sexual risk behavior among this group for the majority of the research sample began engaging in sexual activity before enrolling in college and a significant number of them were sexually active while rarely using condoms. Stakeholders should thus take measures to increase public awareness of sexual and reproductive health issues, such as the use of dual contraception among Ethiopian university students to prevent STDs.
In this study, we looked into what prevents younger college students from using contraception. The barriers to using contraceptives that study participants reported were highlighted in the study were barriers based on the individual and the health care system, which are consistent with the previous studies in Africa.22-24 Individual-based barriers included unawareness about contraception methods, false beliefs about the detrimental effects of contraceptives (including that using contraceptives increased the likelihood of future infertility), and personal financial concerns while the lack of contraceptive supplies in the campus student clinic is the health care problem that is most often mentioned. According to the results, condoms are only given out to boys on one campus. The majority of participants also mentioned that the cost of contraception is a deterrent and that purchasing it from private pharmacies is more expensive. Our study demonstrates that social support from a male partner is a key driver of contraceptive use, which is similar to the earlier study. 25 The cost of the female partner’s birth control pills is often covered by her male partner. Financial barriers, particularly associated with the price of contraceptives and contraceptive services, persisted as a major issue for young individuals seeking to use contraceptives, according to Burke et al. 26 However, this result confronts Castle’s 27 claims that the study’s participants’ perceptions of the affordability of contraceptives functioned as a driving force behind their use of those methods.
Strengths and Limitations of the Study
This study is the first to look at how young college-aged men and women in sexual relationships make decisions for contraception use in Ethiopia to inform future studies. The study is, however, constrained by the small number of participants, some of whom might have found it challenging to share their views and experiences. But the in-depth interviews provide perspectives on their positions through their own words. The participants provided the data on their own accord, which could result in the possibility of social desirability bias. The study was carried out in certain public higher education institutes. The study did not examine college students’ views on contraceptive—decision-making in private higher education institutions.
The reliability of the results was increased in several ways. The questions used in the interviews have been pre-tested before being used. To ensure that the research process was as unbiased as possible, the researchers in this study were self-aware and conscious of their involvement in it. According to the researchers, the study’s opacity is revealed by the detailed descriptions of the sample, data collection techniques, and data processing procedures. Through bracketing, the researchers ensured that their opinions and personal experiences with the subject matter were kept out of the data gathering and analysis.
Conclusion
The research addresses an important gap in knowledge regarding contraceptive decision-making and uses among college students, which is a critical period for shaping future reproductive behavior. The findings of this study also demonstrated that communication and using contraception is a common practice and is accepted as a positive thing on campus, mostly to prevent unexpected pregnancy. The major obstacles to using contraception are believed to be a lack of available contraceptives on campus and cost-related concerns. Most male partner access and bring contraceptives from private drug stores for their girlfriends. Our research also suggests that including men in the decision-making process for contraception use is beneficial, but given the challenges that come with casual relationships, it might call for a strategy that takes into account relationship dynamics and beliefs, condom use for STI prevention, and the capacity to make informed contraceptive decisions.
The university administration and other interested stakeholders need to pay close attention to efforts to increase the use of contraceptives among high-risk young university women while helping guide actions to reinforce young men in making contraceptive decisions on campus. A target population for programs targeted at enhancing joint responsibility for contraception usage may include women at high risk for STDs (high-risk partners) and their partners. Long-term couples should be encouraged to make contraceptive decisions consistently.
Curricula in addition, the university health center should work with the student body to develop family planning education programs and foster a welcoming environment for students to receive family planning services. A setting where young people may communicate openly about topics like sexuality, contraception, and reproductive health may also be made with the help of a reliable online forum as one of the strategies. The student representative council (SRC) should incorporate family planning education into its initiatives and work with the university health services to offer free STI screenings and family planning advice at least once a year. The study recommends that Ethiopia’s public universities consider updating their sexin mixed-method mixed-method mixedmixed-method mixedclude sexuality education and contraception information for non-health disciplines. In this context, a national study is indispensable to better explore the subject and provide information for program and policy decisions.
Supplemental Material
Supplemental material, sj-docx-1-inq-10.1177_00469580231177848 for Contraceptive Decision-Making Among Young College Men and Women in Ethiopia: Results of the Qualitative Study by Nebiyat Lemma, Endalew Gemechu Sendo and Workinesh Sineshaw Abebe in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-2-inq-10.1177_00469580231177848 for Contraceptive Decision-Making Among Young College Men and Women in Ethiopia: Results of the Qualitative Study by Nebiyat Lemma, Endalew Gemechu Sendo and Workinesh Sineshaw Abebe in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
We are indebted to the College of Health Sciences, Addis Ababa University for providing funding for data collection through its Post Graduate Student Grant Scheme. The authors thank the substantial contributions made to the study by the study participants through the sharing of their personal stories voicing voiced and for others. They made it possible for us to learn more.
Footnotes
Authors’ Contributions: The initial research topic and the study design were developed by NL and EGS. The anonymized data was provided by NL. WS and EGS conducted the qualitative analysis. EGS wrote the first draft of the manuscript. All authors contributed to the final data interpretation, revised the first and subsequent drafts critically, and approved the final version of the manuscript.
Presence of Declarations, and Ethics and Consent statements: The School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University’s Research and Ethical Review Committee (IRB) was consulted for approval to proceed with this study ethically. All participants gave their signed written consent to the interviews after receiving full disclosure from the PI. The fact that participation in this study was entirely voluntary was stressed. The identities and other private details of all respondents were also kept confidential.
The author(s) declared no potential conflicts of interest concerning with the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: A small grant for data collection was obtained through grants offered by the Addis Ababa University postgraduate office.
ORCID iD: Endalew Gemechu Sendo  https://orcid.org/0000-0001-7768-0196
https://orcid.org/0000-0001-7768-0196
Data Availability Statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Bain LE, Zweekhorst MBM, de Cock Buning T. Prevalence and determinants of unintended pregnancy in Sub-Saharan Africa: a systematic review. Afr J Reprod Health. 2020;24(2):187-205. [DOI] [PubMed] [Google Scholar]
- 2.Alene M, Yismaw L, Berelie Y, Kassie B, Yeshambel R, Assemie MA. Prevalence and determinants of unintended pregnancy in Ethiopia: A systematic review and meta-analysis of observational studies. PLoS One. 2020;15(4):e0231012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CSA. Ethiopia Demographic and Health Survey. CSA; 2016. [Google Scholar]
- 4.Guttmacher Institute. Contraception and Unintended Pregnancy in Uganda. Guttmacher Institute; 2017. sheet/contraception-and-unintended-pregnancy-Uganda. https://www.guttmacher.org/fact-sheet/contraception-and-unintended-pregnancy-uganda [Google Scholar]
- 5.World Health Organization (WHO). Sexually transmitted infections among adolescents. The need for adequate health services. http://apps.who.int/iris/bitstream/10665/43221/1/9241562889.pdf
- 6.Downey MM, Arteaga S, Villaseñor E, Gomez AM. More than a destination: contraceptive decision making as a journey. Women’s Health Issues. 2017;27(5):539-545. [DOI] [PubMed] [Google Scholar]
- 7.Manlove J, Ryan S, Franzetta K. Contraceptive use patterns across teens’ sexual relationships: the role of relationships, partners, and sexual histories. Demography. 2007;44(3):603-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raine TR, Gard JC, Boyer CB, et al. Contraceptive decision-making in sexual relationships: young men's experiences, attitudes and values. Cult Health Sex. 2010;12(4):373-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arteaga S, Gomez AM. “Is that a method of birth control?” A qualitative exploration of young women’s use of withdrawal. J Sex Res. 2016;53(4-5):626-632. [DOI] [PubMed] [Google Scholar]
- 10.Dingeta T, Oljira L, Assefa N. Patterns of sexual risk behavior among undergraduate university students in Ethiopia: a cross-sectional study. Pan Afr Med J. 2012;12(1):33. [PMC free article] [PubMed] [Google Scholar]
- 11.Almeling R, Waggoner MR. More and less than equal: How men factor in the reproductive equation. Gender Soc. 2013;27(6):821-842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breny JM, Lombardi DC. ‘I don’t want to be that guy walking in the feminine product aisle’: a photovoice exploration of college men’s perceptions of safer sex responsibility. Glob Health Promot. 2019;26(1):6-14. [DOI] [PubMed] [Google Scholar]
- 13.Bearak JM. Casual contraception in casual sex: Life-cycle change in undergraduates’ sexual behavior in hookups. Soc Forces. 2014;93(2):483-513. [Google Scholar]
- 14.Civic D. College students’ reasons for nonuse of condoms within dating relationships. J Sex Marital Ther. 2000;26(1):95-105. [DOI] [PubMed] [Google Scholar]
- 15.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. [DOI] [PubMed] [Google Scholar]
- 16.Landry DJ, Camelo TM. Young unmarried men and women discuss men's role in contraceptive practice. Fam Plann Perspect. 1994;26:222-227. [Google Scholar]
- 17.Lundberg PC. Contraception practices among young unmarried women seeking abortion following unintended pregnancy in Ho Chi Minh City, Vietnam. Cult Health Sex. 2021;23(9):1241-1254. [DOI] [PubMed] [Google Scholar]
- 18.Sendo EG, Fikadu K. Utilization and associated factors of emergency contraception among female college students in Addis Ababa, Ethiopia. Qual Prim Care. 2021;29(1):01-07. [Google Scholar]
- 19.Vaughn JA, Viera AJ. Principles and Practice of College, Health. Springer; 2020. [Google Scholar]
- 20.Sendo EG. The premarital sexual practice among unmarried first-year undergraduate students in Alkan University College in Addis Ababa, Ethiopia. Glob J Med Pub Health. 2014;3(2):1-10. [Google Scholar]
- 21.Young H. Timing of first Sex among college students. Korean J Androl. 2011;29(2):134. [Google Scholar]
- 22.Engelbert Bain L, Amu H, Enowbeyang Tarkang E. Barriers and motivators of contraceptive use among young people in Sub-Saharan Africa: A systematic review of qualitative studies. PloS one. 2021;16(6):e0252745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ochako R, Mbondo M, Aloo S, et al. Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. BMC Public Health. 2015;15(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Otoide VO, Oronsaye F, Okonofua FE. Why Nigerian adolescents seek abortion rather than contraception: evidence from focus-group discussions. Int Fam Plan Perspect. 2001;27:77-81. [Google Scholar]
- 25.Tabane NS, Peu MD. Perceptions of female teenagers in the Tshwane district on the use of contraceptives in South Africa. Curationis. 2015;38(2):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burke E, Kébé F, Flink I, van Reeuwijk M, le May A. A qualitative study to explore the barriers and enablers for young people with disabilities to access sexual and reproductive health services in Senegal. Reprod Health Matters. 2017;25(50):43-54. [DOI] [PubMed] [Google Scholar]
- 27.Castle S. Factors Influencing Young Malians' Reluctance to Use Hormonal Contraceptives. Wiley Online Library; 2003. Citation: Sendo, EG[ as cited in Pubmed] – [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-inq-10.1177_00469580231177848 for Contraceptive Decision-Making Among Young College Men and Women in Ethiopia: Results of the Qualitative Study by Nebiyat Lemma, Endalew Gemechu Sendo and Workinesh Sineshaw Abebe in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-2-inq-10.1177_00469580231177848 for Contraceptive Decision-Making Among Young College Men and Women in Ethiopia: Results of the Qualitative Study by Nebiyat Lemma, Endalew Gemechu Sendo and Workinesh Sineshaw Abebe in INQUIRY: The Journal of Health Care Organization, Provision, and Financing