Abstract
We present a case of a 26-year-old right-hand-dominant male stage manager who underwent open reduction internal fixation of right open both-bone forearm fractures at the age of 13. The patient presented 13 years and 8 months later with proximal hardware migration, soft tissue erosion, and subsequent hardware exposure. The patient underwent hardware removal with resolution of pain and improvement in range of motion. To the best of our knowledge, this complication has not been published before.
Keywords: distal radius, fracture/dislocation, diagnosis, pediatric, pain, open fractures, trauma, wound management
Introduction
Distal radius fractures are the most common type of pediatric forearm fracture, frequently occurring during the metaphyseal growth phase that coincides with puberty. These fractures typically involve the metaphysis, followed in prevalence by the physis.1-3
Pediatric distal radius fractures are typically managed with closed reduction and immobilization to avoid the long-term sequela of surgical intervention. Casting allows for bony union and remodeling, which is maximized near the physis. As in adults, grossly displaced, rotated, or irreducible fractures require operative intervention, via either percutaneous pinning or internal fixation.4,5
Although internal fixation provides the most stable reduction, placement of internal hardware carries unique risks in the pediatric population. Soft tissue dissection and plating can lead to physeal arrest, which can result in radius bone shortening, ulnocarpal impaction, triangulofibrous cartilage complex dysfunction, and pathology at the distal radioulnar joint.6,7 A second, separate concern is that pediatric patients are not fixed in their bone-muscle relationship. As such, bony hardware can displace relative to the overlying soft tissue, theoretically leading to hardware malposition and soft tissue erosion.
Case Report
In this report, we present a 26-year-old right-hand-dominant male stage manager who underwent open reduction internal fixation of right open both-bone forearm fractures at the age of 13, subsequently found to have proximal hardware migration, soft tissue erosion, and associated hardware exposure upon re-presentation 13 years and 8 months later.
The patient initially presented to our emergency department as a 13-year-old right-hand-dominant man with open right distal radius and ulna fractures following skateboarding injury. Medical history was notable for closed right both-bone fractures at the age of 12 years, managed nonoperatively with immobilization. The patient reported baseline limitations in supination and pronation.
In the emergency department following the injury at age 13, physical examination was notable for a 1-cm laceration over the volar forearm and obvious angular deformity of the radius and ulna bones at the forearm level. Radiography demonstrated right distal radius and ulna shaft fractures with apex volar angulation (Figure 1). Given the open nature of his injury, he was taken urgently to the operating room for washout, debridement, and open reduction internal fixation of both fractures. The radius was fixated with a stainless steel Synthes distal radius plate with six 3.5 mm screws (Figure 2). A combination of cortical screws and locking screws was used. Only one screw was placed distally in the most distal row of the radius internal fixation plate, which was positioned proximal to the physis. The patient tolerated the procedure well without complication and was discharged home on postoperative day 2 in a long-arm posterior splint.
Figure 1.

Postinjury radiographs at 13 years demonstrated right both-bone forearm fractures.
Figure 2.
Intraoperative fluoroscopy demonstrated appropriate reduction and hardware placement.
After this index operation, the patient was followed for 2 months in our pediatric hand surgery clinic before being lost to follow-up. At his last postoperative visit, radiographs demonstrated good hardware position (Figure 3), although he had limited range of motion at the wrist.
Figure 3.

Radiographs at 2 months postoperatively demonstrated good hardware position.
Four years later, the patient presented to the clinic with wrist pain. Radiographs demonstrated proximal migration of the distal radius plate with radial protrusion off the diaphysis of the bone (Figure 4). Hardware was prominent on physical examination, but there was no evidence of infection or soft tissue compromise. Aged 17 at that time, the patient deferred hardware removal.
Figure 4.
Radiographs at 4 years postoperatively (17 years old) demonstrated proximal hardware migration.
Twelve years after his index operation, the patient presented to our emergency department with serous drainage from a volar sinus tract just radial to his surgical incision. He was prescribed antibiotics with plans for hardware removal, but was again lost to follow-up.
He next presented to our clinic 18 months later, at age 26, with worsening pain in his right forearm. Physical examination was notable for dry eschar just radial to the original incisional scar with underlying palpable hardware. He had no neurovascular concerns or weakness, but supination was limited to 45°. Radiographs demonstrated proximal migration of the retained internal fixation hardware relative to its original location, but stable proximal hardware position compared with his more recent prior films (Figure 5). There was, however, increased prominence of the most radial border of the distal portion of the internal fixation plate, magnified by the proximal migration of the plate onto a narrower portion of the radius bone, now with impending hardware exposure radially at this site of hardware prominence. Given his increased pain and impending hardware exposure, the patient elected for operative exploration, sinus tract excision, and hardware removal.
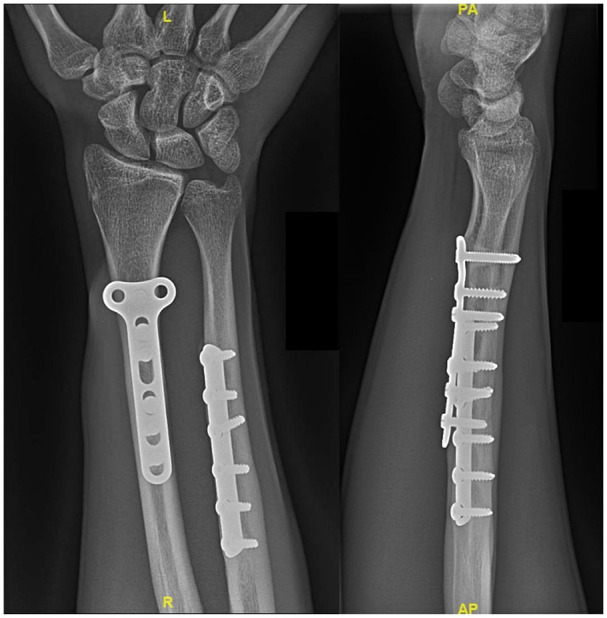
Figure 5.

Radiographs at 13 years and 8 months postoperatively (26 years old) demonstrated stable proximal hardware migration and soft tissue paucity.
In the operating room, preoperative debridement of the eschar revealed exposed hardware through an area of ulceration and erosion with sinus tract formation (Figure 6). An incision was designed to incorporate the patient’s prior surgical scar, allowing for removal of all scarred soft tissue. The radius was exposed via the standard modified Henry’s approach, with careful dissection and release of scar tissue from the prior surgical procedure. The Synthes plate was identified and noted to have considerable bony incorporation. Areas where bone had grown over the plate were removed with a combination of osteotome and rongeur. All 6 screws were identified and removed, followed by removal of the internal fixation plate (Figure 7). The wound was copiously irrigated. The previously identified sinus tract was excised, including a second parallel elliptical incision just radial to the larger primary incision. The pronator quadratus was repaired, the skin was closed in a standard manner, and a resting volar splint was placed with the wrist in neutral position. The patient tolerated the procedure without complication and was discharged home.
Figure 6.
Preoperative examination at age 26 years demonstrated sinus tract with exposed hardware.
Figure 7.
Intraoperative examination revealed proximal migration of hardware with significant bony incorporation. All hardware was successfully removed.
Postoperatively, the patient was followed in our adult hand surgery clinic. He demonstrated appropriate wound healing, decreased wrist and forearm pain, and good finger and wrist range of motion. Given his improvement after surgery, no further imaging or workup was deemed necessary.
Discussion
Pediatric forearm fractures are the most common upper extremity fractures in children and adolescents. 1 Although ideally managed with closed reduction and immobilization, operative intervention is indicated for irreducible or unstable fracture patterns. 5 Open reduction internal fixation carries unique risks in the pediatric population, including the potential for damage to the growth plate during plating.6,7 Although less frequently discussed, skeletally immature patients are also at risk of plate migration with bony growth. This is because, when possible, hardware is placed proximal to the physis to avoid physeal injury and subsequent growth disturbance. As a result, continued bone growth distal to the plate can cause proximal migration of the hardware. In areas of soft tissue paucity, this can result in soft tissue erosion and hardware exposure.
In this report, we present the unusual case of a patient who underwent open reduction internal fixation of a right open both-bone forearm fracture at 13 years. As the patient skeletally matured and as the distal physis produced a progressive increase in radius length, the plate effectively migrated proximally, such that the distal aspect of the plate had poor soft tissue coverage with subsequent pressure necrosis through the overlying skin. The patient re-presented to our clinic with significant pain and exposed hardware 13 years and 8 months after his index operation. The patient was taken to the operating room for hardware removal, with resolution of his symptoms and improved range of motion at his follow-up.
This case is notable in its duration of long-term follow-up after open reduction internal fixation of a pediatric both-bone fracture. Likely, growth of the bone at the metaphysis, which far exceeds that at the diaphysis, effectively pushed the plate proximally, causing proximal bone and plate migration relative to the overlying soft tissue. Heterotopic growth of the bone around the plate with subsequent relative motion of the plate caused the internal fixation hardware to become adherent to the bone, preventing any flexibility in the plate and worsening pressure on the skin.
This case reminds us to consider implant choice and plate placement critically when performing internal fixation in children and adolescents. Although long-term outcomes of such children are not fully predictable, it is imperative that surgeons preoperatively counsel patients and their parents about the possibility of plate migration due to normal bony growth, with subsequent potential need for hardware removal. Alternatively, surgeons may consider use of absorbable plating systems or other fixation methods such as percutaneous pinning in appropriate patients to avoid these long-term sequelae.
Conclusion
In this report, we present the long-term follow-up of a 26-year-old right-hand-dominant male stage manager who underwent open reduction internal fixation of right open both-bone forearm fractures at the age of 13. The patient re-presented 13 years and 8 months later with proximal hardware migration due to interval bony growth with resultant skin ulceration, pain, and hardware exposure. The patient required washout and hardware removal, with resolution of his symptoms. To the best of our knowledge, this complication has not been reported after plate fixation in pediatric patients and should be discussed in the shared decision-making process with the patient and their family.
Footnotes
Authors’ Note: Haley Bunting is now affiliated to Austin Plastic & Reconstructive Surgery, Texas, USA.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Statement of Informed Consent: All patients were informed of possible participation in any experimental treatment in this study and agreed to participate.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Disclosures: All authors have no financial interests including products, devices, or drugs associated with this manuscript. There are no commercial associations that might pose or create a conflict of interest with information presented in this submitted manuscript such as consultancies, stock ownership, or patent licensing arrangements. All sources of funds supporting the completion of this manuscript are under the auspices of the University of California, Los Angeles.
ORCID iDs: Meaghan L. Barr  https://orcid.org/0000-0002-8718-1574
https://orcid.org/0000-0002-8718-1574
Nirbhay S. Jain  https://orcid.org/0000-0002-2377-1364
https://orcid.org/0000-0002-2377-1364
References
- 1.Landin LA.Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl. 1983;202:1-109. http://www.ncbi.nlm.nih.gov/pubmed/6574687. Accessed September 28, 2022. [PubMed] [Google Scholar]
- 2.Bailey DA, Wedge JH, McCulloch RG, et al. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am. 1989;71(8):1225-1231. http://www.ncbi.nlm.nih.gov/pubmed/2777851. Accessed September 28, 2022. [PubMed] [Google Scholar]
- 3.Rodríguez-Merchán EC.Pediatric fractures of the forearm. Clin Orthop Relat Res. 2005;432:65-72. doi: 10.1097/01.blo.0000156480.76450.04. [DOI] [PubMed] [Google Scholar]
- 4.Noonan KJ, Price CT.Forearm and distal radius fractures in children. J Am Acad Orthop Surg. 1998;6(3):146-156. doi: 10.5435/00124635-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Pace JL.Pediatric and adolescent forearm fractures. J Am Acad Orthop Surg. 2016;24(11):780-788. doi: 10.5435/JAAOS-D-15-00151. [DOI] [PubMed] [Google Scholar]
- 6.Abzug JM, Little K, Kozin SH.Physeal arrest of the distal radius. J Am Acad Orthop Surg. 2014;22(6):381-389. doi: 10.5435/JAAOS-22-06-381. [DOI] [PubMed] [Google Scholar]
- 7.Singh V, Garg V, Parikh SN.Management of physeal fractures: a review article. Indian J Orthop. 2021;55(3):525-538. doi: 10.1007/s43465-020-00338-6. [DOI] [PMC free article] [PubMed] [Google Scholar]





