Abstract
Background:
Cannabis policy liberalization has increased cannabis availability for medical or recreational purposes. Up-to-date trends in medical cannabis licensure can inform clinical policy and care.
Objective:
To describe recent trends in medical cannabis licensure in the US.
Design:
Ecological study with repeated measures.
Setting:
State registry data via state reports and data requests on medical cannabis licensure from 2016–2020.
Participants:
Medical cannabis patients (people with medical cannabis licenses) in the US.
Measurements:
Total patient volume, patients per 10,000 of total population, and patient-reported qualifying conditions (i.e., symptoms/conditions qualifying patients for licensure) – including whether these symptoms align with current therapeutic evidence of cannabis/cannabinoid efficacy.
Results:
In 2020, 26 states and Washington DC reported patient numbers, and 19 states reported patient-reported qualifying conditions. Total enrolled patients increased 4.5-fold from 661,990 in 2016 to 2,974,443 in 2020. Patients per 10,000 total population generally increased from 2016–2020, most dramatically in Oklahoma (927.1 patients per 10,000 population). However, enrollment increased in states without recreational legalization (i.e., medical only states), while enrollment decreased in 5/7 with recreational legalization (i.e., recreational states). In 2020, 68.2% of patient-reported qualifying conditions had substantial or conclusive evidence of therapeutic value vs. 84.6% in 2016. Chronic pain was the most common patient-reported qualifying condition in 2020 (60.6%), followed by post-traumatic stress disorder (10.6%) and multiple sclerosis (4.8%).
Limitations:
Missing state data; lack of rationale for discontinuing medical cannabis licensure.
Conclusions:
Enrollment in medical cannabis programs increased 4.5-fold from 2016 to 2020, although enrollment decreased in recreational states. Use for conditions/symptoms without a strong evidence basis increased from 15.4% (2016) to 31.4% (2020). Thoughtful regulatory and clinical strategies are needed to effectively manage this rapidly changing landscape.
INTRODUCTION
Since 1996, access to Cannabis sativa (hereafter cannabis) has expanded rapidly, with 37 states in the US legalizing medical cannabis and 18 legalizing cannabis for adult recreational use. These policies conflict with the federal Controlled Substances Act, which designates cannabis as a Schedule I drug, defined as having no accepted medical use.(1) This policy mismatch generates much medical and legal uncertainty, as legalization efforts have largely increased accessibility while marginally integrating cannabis into medicine.(2) For instance, some qualifying conditions for medical cannabis licensure (e.g., arthritis) do not align with current evidence for therapeutic value,(3) healthcare providers consistently express a lack of knowledge about managing patients using cannabis,(4) and dispensary employees experience minimal medical training.(5) Further, laws variably enforce medicalization of cannabis products, including manufacturing/testing requirements, product labeling, and prescription drug monitoring program tracking.(6) Recreational laws further blur the landscape, as some people use recreational products for medical purposes (e.g., pain).(7) In this context, knowing why people seek medical cannabis and whether this is affected by recreational cannabis laws is critical for developing thoughtful public and medical policy around cannabis.
Analyzing data from US medical cannabis registries through 2016, we showed that chronic pain was the most common reason for medical cannabis licensure (64.5%), followed by multiple sclerosis (14.4%) and nausea/vomiting (6.2%).(3) Since 2016, 14 additional states have legalized medical cannabis and 10 legalized recreational cannabis. Thus, our goal was to provide updated data on national medical cannabis licensure through 2020. We describe trends in total medical cannabis licensure, conditions/symptoms for licensure, and changes in states with and without recreational legislation.
METHODS
As described previously, we collected data from US medical cannabis registries using publicly available reports and data requests from governmental departments overseeing medical cannabis programs. We adopted and expanded upon definitions that we employed previously.(3)
Definitions.
Patients refers to people enrolled in medical cannabis programs. Qualifying conditions are state-recognized medical conditions for which patients may be authorized to obtain cannabis licenses. These conditions vary by state. Patient-reported qualifying conditions are conditions/symptoms reported by patients for their medical cannabis license. Thus, patients can be licensed for ≥1 qualifying conditions, resulting in more patient-reported qualifying conditions listed in state registries than patients. States that had implemented laws legalizing non-medical cannabis use by adults that also had active recreational dispensaries are defined as recreational states, while those with medical cannabis laws alone are defined as medical only states.
We sought registry data as of October 2021 from the District of Columbia (DC) and 35 states with legal medical cannabis: Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Hawaii, Illinois, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Dakota, Utah, Vermont, Virginia, Washington, and West Virginia. Note: We newly obtained 2016 data from Rhode Island and Connecticut, which had been unavailable for our previous report.(3) No data were available from South Dakota, Virginia, Washington, or West Virginia. While we obtained some data from California and Maine, these states have voluntary registries that are unlikely to accurately report patient numbers—exemplified by California reporting only 113,862 licensed cumulative patients from program inception in 1996 through 2021. Data sources are reported in Supplemental Table 1.
As with our previous report, we classified qualifying conditions into categories aligned with the 2017 National Academies of Sciences, Engineering, and Medicine (NASEM) report on the Health Effects of Cannabis and Cannabinoids(1) based on guidance from licensed physician and co-author Avinash Hosanagar (Supplemental Table 2). Chemotherapy-induced nausea and vomiting, chronic pain, and multiple sclerosis-related spasticity were the only conditions/symptoms rated as having substantial or conclusive evidence of efficacy in the NASEM report.
Analysis Plan
Using Microsoft Excel, we first graphed the raw number of patients per state from 2016–2020. We then calculated patient enrollment rates per 10,000 using year-specific estimates for state population from the US Census and compared enrollment per 10,000 population in recreational vs. medical only states. Next, we investigated trends in patient-reported qualifying conditions from 2016–2020 by NASEM category. Lastly, we graphically investigated the distribution of patient-reported qualifying conditions in recreational vs. medical only states in 2020.
IRB Approval
As this study used publicly available data sets that do not include any identifiable information, no institutional review board review was required per University of Michigan policy.
Funding Source:
Dr. Boehnke’s effort on this publication was partially supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number K01DA049219. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of the Funding source
The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
RESULTS
In 2020, DC and 26/35 legal states (75.0%) reported the number of patients in 2020 (Table 1) and 19 (52.8%) reported the number of patient-reported qualifying conditions. However, some states only reported data in certain years (e.g., Louisiana only published 2019 data), did not report complete data (e.g., Rhode Island reported cumulative patient totals but not cumulative patient-reported qualifying conditions), or did not consistently publish reports. For example, New York published biennial reports in 2016 and 2018 but not 2020. Please see data sources in Supplemental Table 2.
Table 1.
Patient numbers by state: 2016–2020
| 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|
| Alaska | 1084 (14.6) | 1053 (14.2) | 621 (8.4) | 404 (5.5) | ND |
| Arizona | 114439 (164.9) | 152979 (217.2) | 186002 (259.9) | 219817 (302) | 295295 (412.9) |
| Arkansas | PI | PI | 5459 (18.1) | 15351 (50.9) | 66638 (221.3) |
| California | VR | VR | VR | VR | VR |
| Colorado | 94577 (170.7) | 93372 (166.4) | 86641 (152.2) | 81610 (141.7) | 85814 (148.6) |
| Connecticut | 15136 (42.3) | 22573 (63.2) | 26641 (74.6) | 36700 (102.9) | 49562 (137.4) |
| Delaware | 1414 (14.9) | 3274 (34.2) | 6060 (62.8) | 11213 (115.2) | 15495 (156.5) |
| District of Columbia (DC) | 4600 (67.1) | 5386 (77.5) | 5836 (83.2) | 5836 (87.3) | 9618 (139.5) |
| Florida | PI | 42724 (20.4) | 167211 (78.7) | 299914 (139.6) | 456594 (212) |
| Hawaii | 15334 (107.4) | 19858 (139.4) | 23746 (167.2) | 27152 (191.8) | 30868 (212.1) |
| Illinois | 7707 (6) | 21800 (17.1) | 39808 (31.3) | 76939 (60.7) | 121775 (95) |
| Louisiana | PI | PI | PI | 4350 (9.4) | PI |
| Maine | VR | VR | VR | VR | VR |
| Maryland | PI | 11489 (19.1) | 51589 (85.5) | 90120 (149.1) | 121994 (197.5) |
| Massachusetts | 33543 (49.2) | 45319 (66.1) | 58920 (85.6) | 60110 (87.2) | 92240 (131.2) |
| Michigan | 218556 (219.6) | 269553 (270.3) | 297515 (298) | 268566 (268.9) | 243372 (241.5) |
| Minnesota | 2806 (5.1) | 8075 (14.5) | 14481 (25.8) | 18249 (32.4) | 28522 (50) |
| Missouri | PI | PI | PI | 22706 (37) | 69397 (112.8) |
| Montana | 7785 (74.8) | 22849 (217.1) | 31186 (294) | 36422 (340.8) | 41638 (384) |
| Nevada | 25358 (86.9) | 23489 (79.1) | 17211 (56.9) | 15839 (51.4) | 13303 (42.8) |
| New Hampshire | 2089 (15.6) | 3493 (25.9) | 6480 (47.9) | 8302 (61.1) | 10688 (77.6) |
| New Jersey | 12154 (13.7) | 16937 (19.1) | 44000 (49.5) | 63062 (71) | 81111 (87.3) |
| New Mexico | 29046 (138.9) | 46645 (223) | 67574 (322.9) | 80257 (382.8) | 104655 (494.2) |
| New York | 4998 (2.5) | 57960 (29.6) | 98101 (50.2) | 111358 (57.2) | 133362 (66) |
| North Dakota | PI | PI | PI | 707 (9.3) | 3233 (41.5) |
| Ohio | PI | PI | 3575 (3.1) | 78376 (67.1) | 176387 (149.5) |
| Oklahoma | PI | PI | 30786 (78.1) | 238869 (603.7) | 367053 (927.1) |
| Oregon | 68032 (166.3) | 50400 (121.6) | 31251 (74.7) | 24801 (58.8) | 22603 (53.3) |
| Pennsylvania | PI | 10532 (8.2) | 100027 (78.1) | 243433 (190.2) | 297317 (228.7) |
| Rhode Island | 16418 (155.4) | 18533 (175.6) | 16963 (160.3) | 16218 (153.1) | 19803 (180.5) |
| South Dakota | PI | PI | PI | PI | PI |
| Utah | PI | PI | PI | PI | 16096 (49.2) |
| Vermont | 3332 (53.4) | 5313 (85.1) | ND | ND | ND |
| Virginia | PI | PI | PI | PI | PI |
| Washington State | ND | ND | ND | ND | ND |
| West Virginia | PI | PI | PI | PI | PI |
| Total patients | 678408 | 953606 | 1417684 | 2157005 | 2974433 |
| # states with data/number of states and DC with medical cannabis laws | 20/30 (66.7%) | 23/31 (74.2%) | 26/34 (76.5%) | 28/34 (82.3%) | 27/36 (75.0%) |
Values are total patient number, with patients per 10,000 total population in parentheses. ND: No data available from active program. PI: Program inactive, resulting in no data. VR: Voluntary Registry, resulting in no reliable data. Patient number increased nearly 4.5-fold between 2016 and 2020.
Total patient number increased approximately 4.5-fold in the study period: 678,408 in 2016 to 2,974,433 in 2020 (Table 1). The patients per 10,000 total population generally increased during this period (Figure 1), most dramatically in Oklahoma (78.1/10,000 in 2018 to 927.1/10,000 in 2020). States implementing laws after 2016 accounted for 52.9% of patients in 2020 (Supplemental Figure 1). While all medical only states except Rhode Island consistently increased enrollment during this time, five of the seven recreational states had decreasing enrollment (Figure 1).
Figure 1.
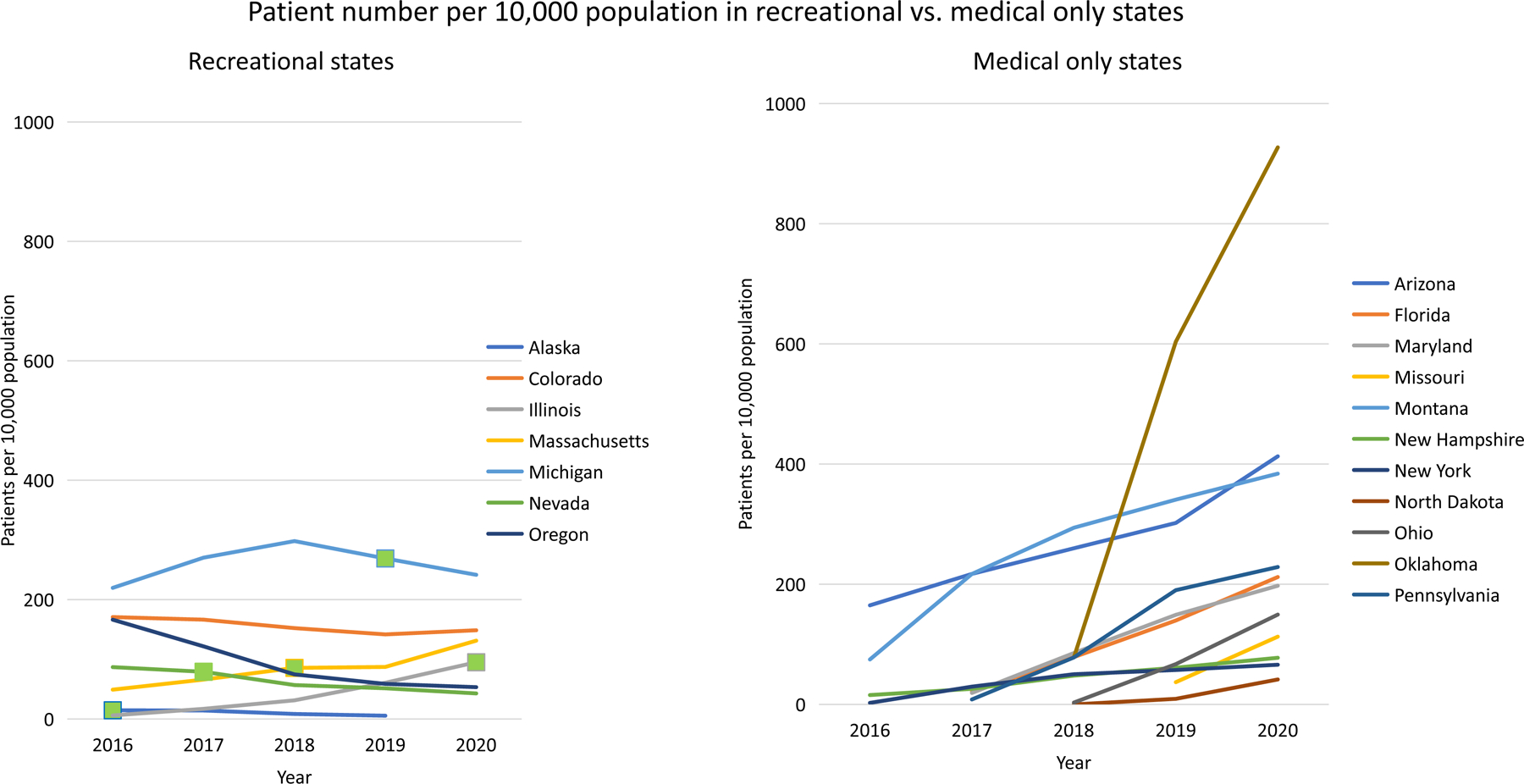
The frame on the left shows population-level trends in adult-use states, with the green square indicates when adult-use dispensaries became active. The frame on the right shows a sampling of n=11 medical only states that highlight the range of population-level values. Years recreational cannabis laws were passed: Alaska (2015), Colorado (2012), Illinois (2019), Massachusetts (2018), Michigan (2018), Nevada (2016), Oregon (2014). Years recreational cannabis dispensaries became active prior to study period: Colorado (2014), Oregon (2015).
Among states with patient-reported qualifying condition data, chronic pain increased from 484,386 in 2016 to 1,119,668 in 2020, accounting for 60.6% of all patient-reported qualifying conditions in 2020 (Figure 2). Post-traumatic stress disorder (PTSD) was the second most common patient-reported qualifying condition in 2020, increasing from 27,447 in 2016 to 195,984 in 2020 (10.6% of total). Notably, the percentage of conditions for which cannabis has substantial or conclusive evidence of therapeutic value decreased from 84.6% in 2016 to 68.2% in 2020 (Figure 3). Conditions in the “other” category increased considerably as well, partially due to contributions from vague categories such as “chronic or debilitating disease or condition”, “psychiatric conditions”, or “other” (17,492, 11,914, and 48,485 patient-reported qualifying conditions, respectively, in 2020). Medical only and recreational states had different distributions of patient-reported qualifying conditions (Figure 4). Chronic pain and PTSD were more common in medical only states (62.3% vs. 57.7%, 13.3% vs. 5.9%, respectively), whereas recreational states had higher percentages of multiple sclerosis (9.3% vs. 2.3%), arthritis (8.3% vs. 0.9%), and chemotherapy-induced nausea and vomiting (5.6% vs 1.2%).
Figure 2.
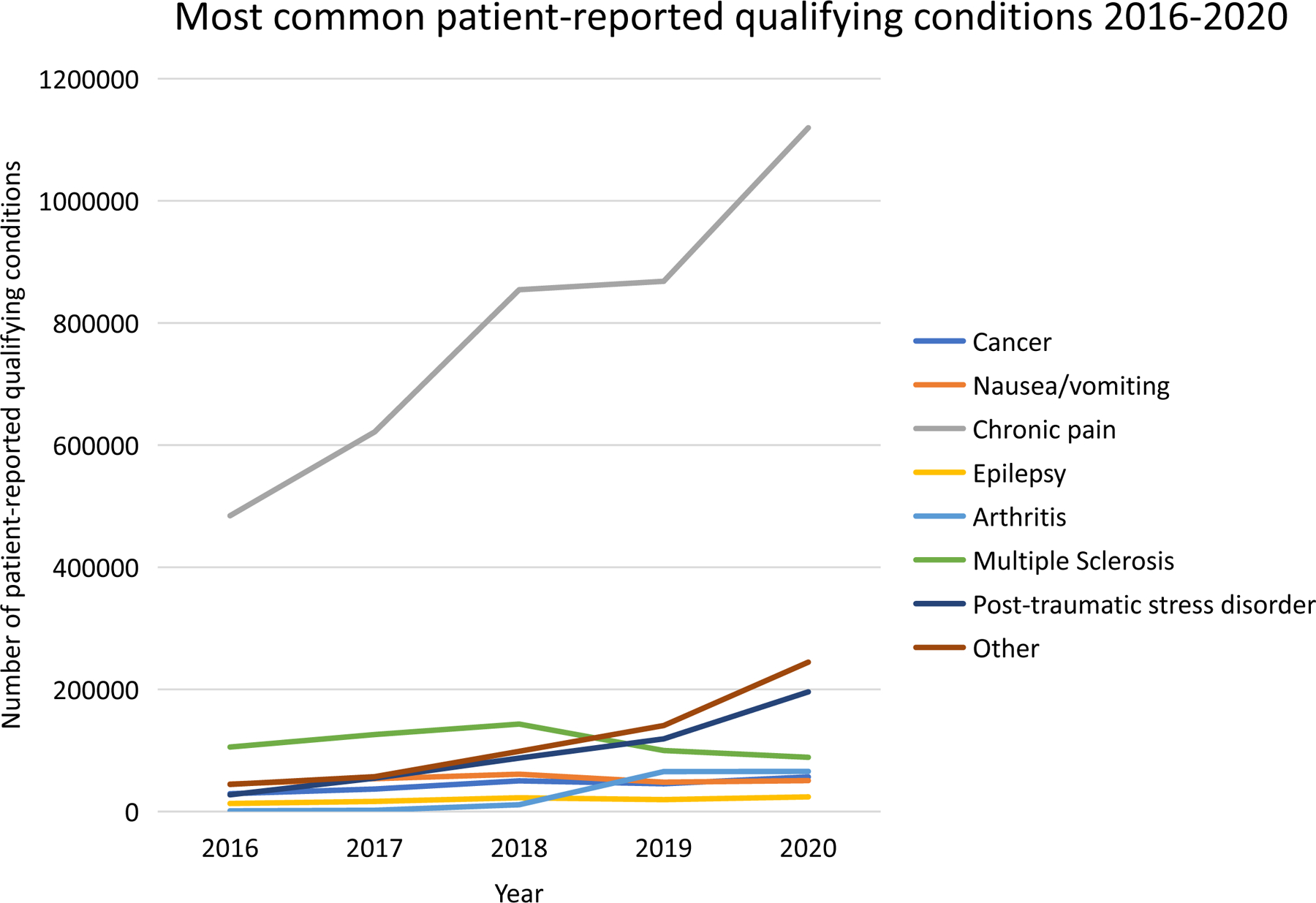
Chronic pain was the most common reason patient-reported qualifying condition, accounting for more licenses than all other conditions combined. Patients could report ≥1 qualifying condition or symptom. Significant contributors to the “Other” category include: vague categories such as “chronic or debilitating disease or condition”, “Psychiatric conditions”, “multiple conditions”, or “other” in state reports. The years for which each state contributed data are as follows:
2016: AZ, CO, DE, HI, IL, MI, MN, MT, NV, NH, NJ, NM, NY, OR, RI.
2017: AZ, CO, DE, HI, IL, MI, MN, MT, NV, NH, NJ, NM, OR, RI.
2018: AR, AZ, CO, DE, HI, IL, MD, MI, MN, MT, NV, NH, NM, NY, OR, RI.
2019: AR, AZ, CO, DE, HI, IL, MD, MI, MN, MO, MT, NV, NH, NM, ND, OH, OR, RI.
2020: AR, AZ, CO, DE, HI, IL, MD, MI, MN, MO, MT, NV, NH, NM, ND, OH, OR, RI, UT.
Figure 3.
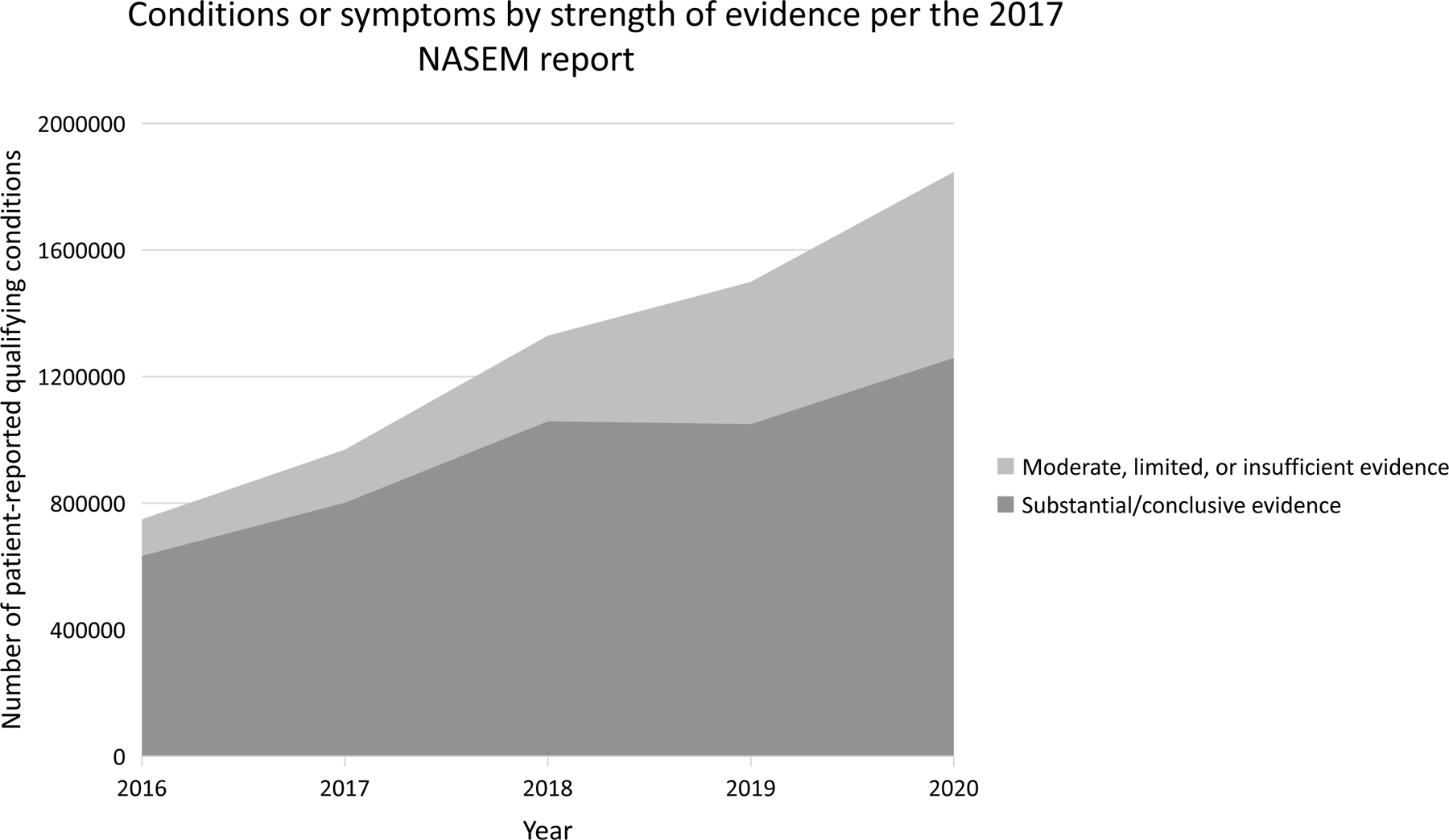
The percentage of patient-reported qualifying conditions with substantial or conclusive evidence decreased from 84.6% in 2016 to 68.2% in 2020. Patients could report ≥1 qualifying condition or symptom. The years for which each state contributed data are below.
2016: AZ, CO, DE, HI, IL, MI, MN, MT, NV, NH, NJ, NM, NY, OR, RI.
2017: AZ, CO, DE, HI, IL, MI, MN, MT, NV, NH, NJ, NM, OR, RI.
2018: AR, AZ, CO, DE, HI, IL, MD, MI, MN, MT, NV, NH, NM, NY, OR, RI.
2019: AR, AZ, CO, DE, HI, IL, MD, MI, MN, MO, MT, NV, NH, NM, ND, OH, OR, RI.
2020: AR, AZ, CO, DE, HI, IL, MD, MI, MN, MO, MT, NV, NH, NM, ND, OH, OR, RI, UT.
Figure 4.
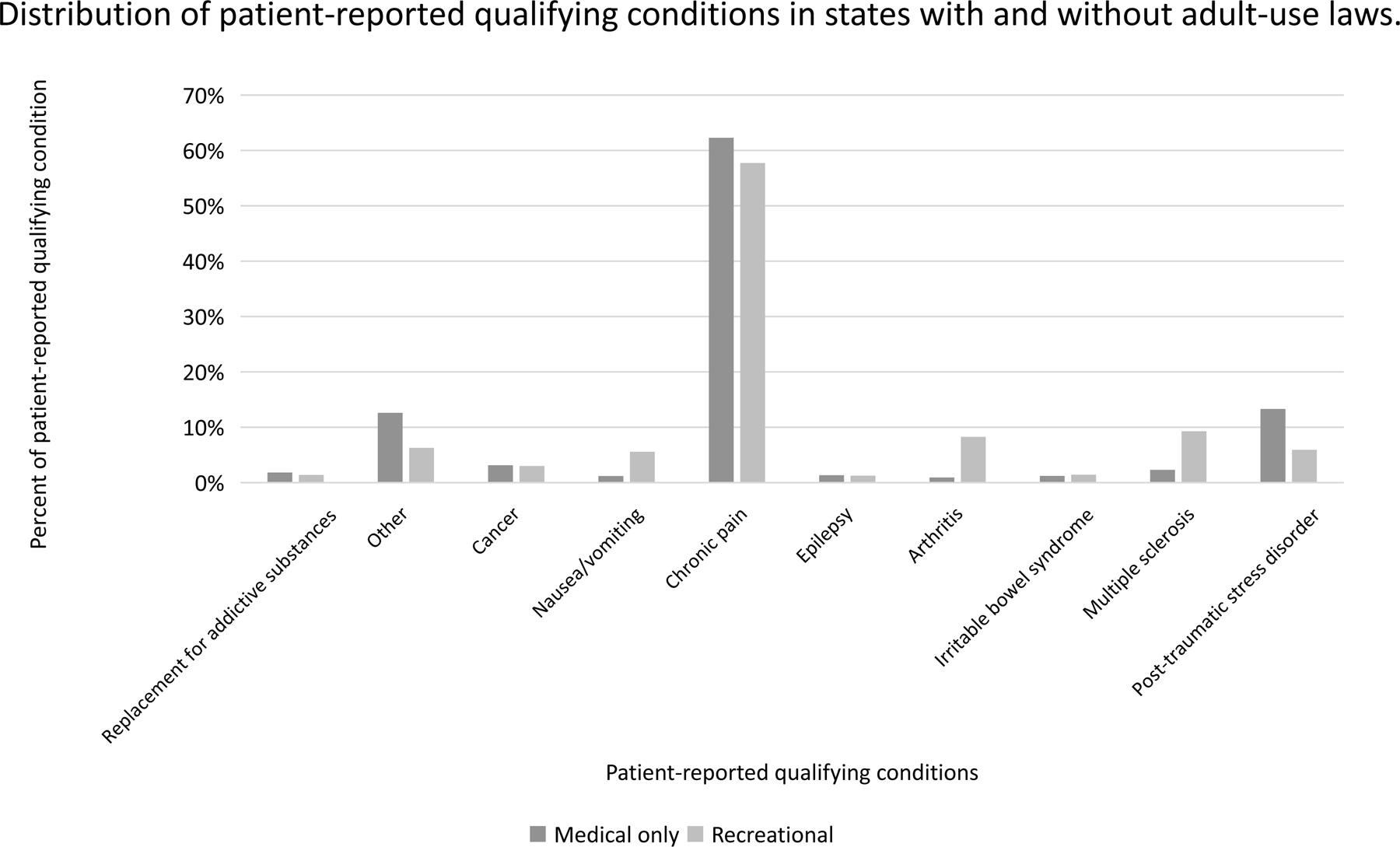
Recreational states had a lower percentage of licenses for chronic pain (57.2% vs. 62.3%) and PTSD (5.9% vs. 13.3%) than medical only states, but a higher proportion of licenses for multiple sclerosis, arthritis, and nausea/vomiting. Patients could report ≥1 qualifying condition or symptom for licensure. Significant contributors to the “Other” category include: vague categories such as “chronic or debilitating disease or condition”, “Psychiatric conditions”, “multiple conditions”, or “other” in state reports. Recreational states: CO, IL, MI, NV, OR. Medical-only states: AR, AZ, DE, HI, MD, MN, MO, MT, NH, NM, ND, OH, RI, UT
DISCUSSION
Medical cannabis licensure continues to accelerate, from 678,408 patients in 2016 to over 2.9 million in 2020. This increase was driven by new medical cannabis laws (35 states and Washington DC had enacted laws by 2020 vs. 23 and Washington DC in 2016) and increasing enrollment in many existing programs, including expanding licensure for new qualifying conditions, such as chronic pain in Illinois. Programs that opened since 2016 had the fastest growing number of patients. While previous studies have showed that the degree of medicalization of cannabis laws is associated with proportionately fewer patients,(8) these trends are becoming less clear, demonstrated by the high degree of medicalization in Florida, Pennsylvania, and Ohio.(6)
Overall, population-level enrollment in medical cannabis programs varied considerably, ranging from 0.05% in Alaska to 9.3% in Oklahoma. Enrollment patterns represent a fruitful area for future research, and are potentially influenced by time since legislation implementation, demographics, permissiveness of state laws,(9) and recreational cannabis laws—as demonstrated by decreasing medical enrollment in 5/7 recreational states. This could be due to patients opting out because they no longer need a license to provide legal cover for recreational use, inconvenience and/or licensing fees, or because they are using recreational products medically.(7) Rapid growth of patients also likely reflects increasing acceptance of cannabis, demonstrated by a 2021 national Pew poll reporting that >90% of Americans agreed that cannabis should be legal for medical purposes.(10) Most medical cannabis markets were also designated as “essential” during the COVID-19 pandemic, enhancing access through telemedicine visits, at-home delivery, or curbside pickup.(11)
Patient-reported qualifying conditions without a substantial or conclusive evidence basis increased from 15.4% (2016) to 31.4% (2020). Increasing licensure for PTSD (limited evidence, 10.6% of conditions in 2020) contributed to this trend, as does poor data quality, since growing, vague categories including “other” or “psychiatric conditions” have no evidence of efficacy. PTSD licensure trends may be influenced by the COVID-19 pandemic, which substantially impacted mental health(12) and is associated with increased cannabis use–especially among people with mental health conditions.(13, 14) The most common patient-reported qualifying condition remained chronic pain: 64.5% in 2016 and 60.6% in 2020. This finding is unsurprising given the high prevalence of chronic pain,(15) and that it is a common co-morbidity with many qualifying conditions (e.g., cancer). Lastly, poor outcomes with pain medications,(16, 17) including opioids,(18) have led some patients to seek alternatives.(19) Indeed, observational reports suggest that some substitute cannabis for pain medications due to fewer negative side effects and better symptom management.(19–21) These factors likely contributed to legislative updates allowing cannabis in place of opioids or other habit-forming medications.
In 2020, recreational states had a different distribution of patient-reported qualifying conditions than medical only states, largely driven by arthritis, multiple sclerosis, and PTSD. While our descriptive analyses cannot determine causality, this finding could be related to underlying population characteristics or to characteristics of legislation—such as the highly specific qualifying conditions in Illinois.
Implications
Combined with growing scientific and public acceptance of cannabis’s therapeutic properties, our results highlight the value of aligned federal and state cannabis regulation.(22) The federal Schedule I designation is inconsistent with accepted therapeutic uses of cannabis and cannabinoids,(1) and legal consequences of cannabis’ criminalization disproportionately impact black and brown communities.(22, 23) Well-crafted federal regulation could improve patchwork state policies,(6) enforce adequate labeling and potency testing, clarify blurred lines between medical and recreational use, and ensure appropriate training for dispensary employees and healthcare professionals.(24) Finally, progress in cannabis therapeutics would be aided through real-world data on health outcomes—a process already ongoing in Florida(25) and Minnesota.(26)
Limitations
First, the data provided in state reports are of inconsistent quality and some data are missing, including data from California—the most populous state. Reports also do not provide data on products used (e.g., cannabinoid content, dose, administration route) or patient demographics by qualifying condition, both of are important areas for future research. Second, we have no data explaining why patients no longer obtain licenses after recreational laws are implemented, which could be due to other population-level factors. Third, we do not know primary reasons for use as many patients reported use of cannabis for multiple conditions or symptoms. Fourth, classifying medical conditions into NASEM categories may be problematic because: 1) these categories are broad; 2) the NASEM report assessed therapeutic value using a limited evidence base with predominantly delta-9-tetrahydrocannabinol products that different greatly from those on the medical cannabis market, many of which contain cannabidiol, and; 3) evidence for therapeutic value is changing rapidly (e.g., cannabidiol for Dravet Syndrome).(27)
Conclusions
Among states with available data, medical cannabis licensure has increased dramatically since 2016, from 678,408 to 2,974,433 patients in 2020. However, licensure decreased in 5/7 recreational states. Use for conditions/symptoms without a substantial evidence basis increased from 15.4% (2016) to 31.4% (2020). While chronic pain remains the most common patient-reported qualifying condition (60.6%), this finding should be interpreted with caution given the broad nature of this category and the heterogeneity of chronic pain. Coherent U.S. cannabis policy would enhance research efforts to guide appropriate medical cannabis use.
Supplementary Material
Funding Source:
Dr. Boehnke’s effort on this publication was partially supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number K01DA049219 (KFB). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Registration: N/A
Data Availability Statement:
Protocol: not available
Computer Code: All graphs were created in Excel, so there was no code used.
Data: Available to interested readers. Please contact Dr. Kevin Boehnke at kboehnke@med.umich.edu.
References
- 1.National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington (DC); 2017. [PubMed] [Google Scholar]
- 2.Haffajee RL, MacCoun RJ, Mello MM. Behind Schedule - Reconciling Federal and State Marijuana Policy. N Engl J Med 2018;379(6):501–4. [DOI] [PubMed] [Google Scholar]
- 3.Boehnke KF, Gangopadhyay S, Clauw DJ, Haffajee RL. Qualifying Conditions Of Medical Cannabis License Holders In The United States. Health Aff (Millwood) 2019;38(2):295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ronne ST, Rosenbaek F, Pedersen LB, Waldorff FB, Nielsen JB, Riisgaard H, et al. Physicians’ experiences, attitudes, and beliefs towards medical cannabis: a systematic literature review. BMC Fam Pract 2021;22(1):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merlin JS, Althouse A, Feldman R, Arnsten JH, Bulls HW, Liebschutz JM, et al. Analysis of State Cannabis Laws and Dispensary Staff Recommendations to Adults Purchasing Medical Cannabis. JAMA Netw Open 2021;4(9):e2124511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richard EL, Althouse AD, Arnsten JH, Bulls HW, Kansagara D, Kerbag MN, et al. How medical are states’ medical cannabis policies?: Proposing a standardized scale. Int J Drug Policy 2021;94:103202. [DOI] [PubMed] [Google Scholar]
- 7.Bachhuber M, Arnsten JH, Wurm G. Use of Cannabis to Relieve Pain and Promote Sleep by Customers at an Adult Use Dispensary. J Psychoactive Drugs 2019;51(5):400–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams AR, Olfson M, Kim JH, Martins SS, Kleber HD. Older, Less Regulated Medical Marijuana Programs Have Much Greater Enrollment Rates Than Newer ‘Medicalized’ Programs. Health Aff (Millwood) 2016;35(3):480–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okey SA, Castro SA, Waddell JT, Jones CB, Blake AJ, O’Rourke HP, et al. Are recreational cannabis laws associated with declining medical cannabis program enrollment in the U.S.? An analysis of cardholder enrollment and demographic characteristics from 2013 to 2020. Int J Drug Policy 2021;100:103531. [DOI] [PubMed] [Google Scholar]
- 10.Green TV 2021;Pages. Accessed at Pew Research Center at https://www.pewresearch.org/fact-tank/2021/04/16/americans-overwhelmingly-say-marijuana-should-be-legal-for-recreational-or-medical-use/ on 11-16-2021.
- 11.Sacirbey O 2021;Pages. Accessed at MjBizDaily at https://mjbizdaily.com/how-essential-transformed-the-us-marijuana-industry-amid-the-covid-19-pandemic/ on 11-16-2021.
- 12.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet 2020;395(10227):912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boehnke KF, McAfee J, Ackerman JM, Kruger DJ. Medication and substance use increases among people using cannabis medically during the COVID-19 pandemic. Int J Drug Policy 2021;92:103053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vidot DC, Islam JY, Marlene C-R, Harrell MB, Rao DR, Chavez JV, et al. The COVID-19 cannabis health study: Results from an epidemiologic assessment of adults who use cannabis for medicinal reasons in the United States. J Addict Dis 2021;39(1):26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high-impact chronic pain among US adults, 2019. In: Prevention CfDCa, ed; 2020. [PubMed] [Google Scholar]
- 16.Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 2015;14(2):162–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hauser W, Walitt B, Fitzcharles MA, Sommer C. Review of pharmacological therapies in fibromyalgia syndrome. Arthritis Res Ther 2014;16(1):201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA 2016;315(15):1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boehnke KF, Scott JR, Litinas E, Sisley S, Williams DA, Clauw DJ. Pills to Pot: Observational Analyses of Cannabis Substitution Among Medical Cannabis Users With Chronic Pain. J Pain 2019;20(7):830–41. [DOI] [PubMed] [Google Scholar]
- 20.Boehnke KF, Gagnier JJ, Matallana L, Williams DA. Substituting Cannabidiol for Opioids and Pain Medications Among Individuals With Fibromyalgia: A Large Online Survey. J Pain 2021;22(11):1418–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lucas P, Baron EP, Jikomes N. Medical cannabis patterns of use and substitution for opioids & other pharmaceutical drugs, alcohol, tobacco, and illicit substances; results from a cross-sectional survey of authorized patients. Harm Reduct J 2019;16(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haffajee R, Mauri A. Cannabis Liberalization In The US: The Policy Landscape. Health Affairs Health Policy Brief 2021. [Google Scholar]
- 23.Earp BD, Lewis J, Hart CL, with B, Allied Professionals for Drug Policy R. Racial Justice Requires Ending the War on Drugs. Am J Bioeth 2021;21(4):4–19. [DOI] [PubMed] [Google Scholar]
- 24.Shover CL, Humphreys K. Six policy lessons relevant to cannabis legalization. Am J Drug Alcohol Abuse 2019;45(6):698–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown JD, Costales B, van Boemmel-Wegmann S, Goodin AJ, Segal R, Winterstein AG. Characteristics of Older Adults Who Were Early Adopters of Medical Cannabis in the Florida Medical Marijuana Use Registry. J Clin Med 2020;9(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anderson SP, Zylla DM, McGriff DM, Arneson TJ. Impact of Medical Cannabis on Patient-Reported Symptoms for Patients With Cancer Enrolled in Minnesota’s Medical Cannabis Program. J Oncol Pract 2019;15(4):e338–e45. [DOI] [PubMed] [Google Scholar]
- 27.Devinsky O, Cross JH, Laux L, Marsh E, Miller I, Nabbout R, et al. Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome. N Engl J Med 2017;376(21):2011–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


