Abstract

Animal experiments have shown that injectable collagen scaffold with human umbilical cord-derived mesenchymal stem cells can promote recovery from spinal cord injury. To investigate whether injectable collagen scaffold with human umbilical cord-derived mesenchymal stem cells can be used to treat spontaneous intracerebral hemorrhage, this non-randomized phase I clinical trial recruited patients who met the inclusion criteria and did not meet the exclusion criteria of spontaneous intracerebral hemorrhage treated in the Characteristic Medical Center of Chinese People’s Armed Police Force from May 2016 to December 2020. Patients were divided into three groups according to the clinical situation and patient benefit: control (n = 18), human umbilical cord-derived mesenchymal stem cells (n = 4), and combination (n = 8). The control group did not receive any transplantation. The human umbilical cord-derived mesenchymal stem cells group received human umbilical cord-derived mesenchymal stem cell transplantation. The combination group received injectable collagen scaffold with human umbilical cord-derived mesenchymal stem cells. Patients who received injectable collagen scaffold with human umbilical cord-derived mesenchymal stem cells had more remarkable improvements in activities of daily living and cognitive function and smaller foci of intracerebral hemorrhage-related encephalomalacia. Severe adverse events associated with cell transplantation were not observed. Injectable collagen scaffold with human umbilical cord-derived mesenchymal stem cells appears to have great potential treating spontaneous intracerebral hemorrhage.
Key Words: clinical trial, collagen scaffold, efficacy, human umbilical cord-derived mesenchymal stem cells, human, safe, neurological recovery, spontaneous intracerebral hemorrhage, transplantation
Introduction
Spontaneous intracerebral hemorrhage (ICH) leads to permanent impairment of sensation, movement, speech, and cognition (Hallevi et al., 2009). ICH not only affects quality of life, but also imposes a financial burden on affected patients, their families, and society (Hesami et al., 2015). Although current ICH therapeutic strategies such as neurotrophic factors, surgery, and rehabilitation can extend patient lifespan, treatments that promote neurological recovery are not available (Law et al., 2017; Cao et al., 2020). The primary brain injury caused by ICH is mechanical injury (Li et al., 2021). Additional secondary injury is caused by altered calcium homeostasis, blood cytotoxicity, neurotransmitter excitotoxicity, and inflammation (Qureshi et al., 2003; Aronowski and Zhao, 2011; Yip et al., 2021). The treatment of ICH is challenging because of the complexity of central nervous system pathophysiological processes and the difficulties with neural regeneration. However, transplantation of biomaterial scaffolds combined with stem cells provides a new potential method for regaining neural function after ICH.
Human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) have several advantages over other stem cell types for treating ICH (Nakano and Fujimiya, 2021). They are less controversial than embryonic stem cells and can be readily acquired and used without concern for immunological rejection. Furthermore, hUC-MSCs exhibit rapid self-renewal characteristics (Bonaventura et al., 2020). MSC transplantation is safe and feasible and associated with low risk of malignant transformation (Karussis et al., 2010; Tsai et al., 2018; Bydon et al., 2020; Yang et al., 2020). After spinal cord injury, transplantation of hUC-MSCs can inhibit astrogliosis and microglial activation, secrete trophic factors, modulate the inflammatory response at the site of injury, and promote neural growth (Park et al., 2012b; Urdzíková et al., 2014; Zhou et al., 2015; Wang et al., 2016). Collagen scaffold (CS) can guide nerve growth along its fibers, connect the gaps of severely injured spinal cords, rebuild the microenvironment at the site of injury, and inhibit scar formation (Lin et al., 2006; Stokols and Tuszynski, 2006; Li et al., 2013; Liu et al., 2021). It also acts as a delivery carrier for trophic factors or stem cells to promote neural regeneration (Zhang et al., 2016). Because the pathological mechanisms of ICH are extremely complex, a single therapeutic approach is unlikely to achieve satisfactory outcomes. Previous studies in animal spinal cord injury models have shown that CS combined with hUC-MSCs can reduce the lesion area, guide orderly regeneration of nerve fibers, and promote remarkable neurological recovery (Li et al., 2017; Wang et al., 2018). Therefore, this approach has promise for treatment of ICH. However, no relevant clinical studies have been conducted. This study aimed to assess the safety and efficacy of transplantation of injectable CS combined with hUC-MSCs in patients with ICH.
Methods
CS preparation
The CS was prepared from bovine aponeurosis (Wanlifa, Beijing, China) as previously reported (Lin et al., 2006; Xiao et al., 2016). Briefly, fresh white aponeuroses were repeatedly rinsed with cold distilled water. The adjunctive tissues, including connective tissue, fat and residual muscles were resected. Then, the samples were repeatedly rinsed and freeze-dried. Standard CS was established at 4°C until use. Biological safety of the CS was evaluated by the National Institutes for Food and Drug Control according to Chinese criteria for medical devices (Xiao et al., 2018).
Isolation, culture, and identification of hUC-MSCs
hUC-MSCs were obtained from healthy newborn umbilical cord. Human umbilical cord research was approved by the Ethics Committee of the Characteristic Medical Center of People’s Armed Police Forces (approval No. 2017-0008; July 20, 2017). Written informed consent was obtained from the newborns’ parents. hUC-MSCs were isolated, cultured, and identified using previously reported methods (Tu et al., 2012; Zhao et al., 2017). Briefly, the blood vessels and amnion were resected from the umbilical cord. The remaining Wharton’s jelly was sliced into tissue pieces (1–2 cm2) and digested with collagenase (Solarbio Science & Technology Co., Ltd., Beijing, China) and 0.25% trypsin (Solarbio Science & Technology Co., Ltd.). Then, the undigested tissue was separated using a 100-μm filter. Cell suspension was seeded in Dulbecco’s modified Eagle’s medium/F12 (Thermo Fisher Scientific Co., Ltd., Shanghai, China) containing 20% fetal bovine serum (MRC Biotechnology Co., Ltd., Changzhou, China), 2 mM glutamine (Sigma-Aldrich, St. Louis, MO, USA), and 100 U penicillin (Solarbio Science & Technology Co., Ltd.) and streptomycin (Solarbio Science& Technology Co., Ltd.). hUC-MSCs were cultured in a cell incubator at 37°C and 5% CO2. The medium was replaced every 3 to 4 days. hUC-MSCs were passaged when they attained 80% confluence. The cell number for transplantation was 1 × 107 cells/2 mL. The morphology of the cells was observed under an inverted fluorescence microscope (Leica DMI3000 B, Wetzlar, Germany). Cells were identified using flow cytometry (Beckman Cytomics™ FC 500, Brea, CA, USA) with antibodies against CD105, CD73, CD90, and human leukocyte antigen-antigen D (all from Abcam, Cambridge, UK). hUC-MSCs were also identified by immunofluorescence staining (CD73, CD90, and CD105; Abcam). Cells (1 × 106) were washed in phosphate buffered saline and incubated for 20 minutes at room temperature. Primary antibodies labeled with fluorescein isothiocyanate were used. Mouse isotype antibody was used as control (Tu et al., 2012). Expanded MSCs needed to meet the following conditions for transplantation: 1) ≥ 95% of expanded MSCs were positive for CD73, CD90, and CD105; and 2) < 3% were positive for HLA-DR. MSCs used for transplantation needed to express key MSCs markers (CD73, CD90, and CD105) without expressing the hematopoietic marker HLA-DR (Zhao et al., 2017).
Clinical trial section
Patient selection
The clinical prospective controlled trial protocol was approved by the Ethics Committee of the Characteristic Medical Center of People’s Armed Police Forces (approval No. 2017-0008; July 20, 2017) and conducted according to the principles of the Declaration of Helsinki. Informed consent was obtained from all participants. Our reporting follows the guidelines of the Transparent Reporting of Evaluations with Nonrandomized Designs statement (Des Jarlais et al., 2004).
Inclusion criteria were as follows: 1) male or female, age 35 to 75 years; 2) surgery performed > 6 hours after symptom onset; 3) Glasgow Coma Scale (GCS) score 4–14 (Gladstone et al., 2019); and 4) computed tomography (CT) diagnosis of spontaneous ICH (hematoma volume, 20–40 mL). Patients with severe heart failure, severe lung disease, uremia, cirrhosis, end-stage cancer, coagulation disorders, stroke sequelae, and those who experienced asphyxia, cardiac arrest, or cardiopulmonary resuscitation before hospitalization were excluded. We also excluded pregnant or lactating women. Potential patients were assessed for study participation and the legal authorized person of the patient provided informed consent for clinical trial participation.
Thirty-four patients who met criteria were recruited between May 2016 and December 2020. Four were lost to follow-up (one in the control group, one in the hUC-MSCs group, and two in the combination group). Therefore, 30 patients were included for analysis. These patients were divided into three groups according to the clinical situation and patient benefit: control (n = 18), hUC-MSCs (n = 4), and combination (n = 8). In the hUC-MSCs group, 1 × 107 hUC-MSCs were transplanted into the hematoma cavity. In the combination group, injectable CS with hUC-MSCs was implanted into the hematoma cavity. In the control group, all patients received conventional treatment. All patients in all groups received the same surgical intervention. The study flow chart is shown in Figure 1.
Figure 1.

Study flow chart.
CS: Collagen scaffold; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells.
Surgical procedure and transplantation of hUC-MSCs or CS with hUC-MSCs
The patients underwent general anesthesia with endotracheal intubation. All surgical procedures were performed by the same experienced neurosurgeon. After stereotactic intracranial hematoma localization, a drainage tube was inserted (Figure 2A and B). Patients were monitored in the neurological intensive care unit (ICU) after surgery. The drainage tube was kept in place for 1 to 2 days until adequate drainage of the hematoma. Daily drainage volume was recorded. Before drainage tube removal, 2 mL of injectable gelatinous CS with 1 × 107/mL hUC-MSCs were transplanted into the hematoma cavity (Figure 2C and D) (Xiao et al., 2018). The syringe for loading hUC-MSCs was a conventional 2 mL syringe, which was diluted with 3 to 8 mL of normal saline after injection. Postoperative vital signs, complete blood count, blood electrolytes, blood glucose, hepatorenal function, coagulation function, and blood-gas analysis were monitored and recorded every 4 hours after admission for 7 days after surgery.
Figure 2.

Transplantation procedure.
(A) The intracranial hematoma was localized using stereotaxis. (B) A tube was inserted for hematoma drainage. (C) 1 × 107 hUC-MSCs were added to the CS. (D) The CS with 1 × 107 hUC-MSCs were transplanted into the hematoma cavity before the drainage tube was removed. CS: Collagen scaffold; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells.
Rehabilitation program and nutritional measures
All patients experienced multisystem rehabilitation and exercise training to maximize recovery of muscle strength and sensation function. Each patient received a diet high in protein and fiber and low in carbohydrates and fat.
Neuroelectrophysiology studies
Somatosensory evoked potentials (SEPs) and electroencephalography (EEG) were performed before surgery and 1, 3, 6, 12, 18, and 24 months after. SEPs were performed using the Viking Quest system (Nicolet Biomedical, Madison, WI, USA). EEG was performed using the EEG-1200C (Nihon Kohden, Tomioka, Japan); scalp electrodes were placed using the International 10–20 system. Electrophysiological studies were made by the same neurologist.
For SEP studies of the upper extremities, electrodes were positioned at the wrist to stimulate the median nerve. Recording electrodes were placed on the contralateral C3’-Fz and Cz’-Fz, respectively. The stimulating intensity was enough to cause a visual contraction of the targeted muscles (time, 200 μs; intensity, 35–50 mA). SEP latency and amplitude were recorded.
EEG parameters were as follows: time constant, 0.3 seconds; and high frequency filter, 70 Hz. The criteria for abnormal EEG were as follows: (1) Mild abnormality-waveforms were mostly α or β activity with low to medium amplitude, scattered irregular θ activity in the medium amplitude; (2) moderate abnormality-waveforms were mostly irregular θ activity in the medium amplitude, α or β activity was weakened, and a small amount of δ activity appeared; and (3) marked abnormality-waveforms were mostly polymorphic δ activity or irregular θ activity with medium to high amplitude, α or β activity was obviously weakened, and occasional sharp and spinous waves.
Head CT
Head CT was performed before surgery and 1, 4, 7 days and 1, 3, 6, 12, 18, and 24 months post-surgery. Scans were performed using a 64-slice Magnetom Verio scanner (Siemens, Munich, Germany) with 5 mm slices. Hematoma volume on CT was determined using the Coniglobus formula. CT scans were performed by the same radiologist. CT results were determined by another radiologist.
Clinical assessments and postoperative follow-up
At 1, 3, 6, 12, 18, and 24 months post-surgery, clinical scores were recorded for the following scales: orientation, myodynamia, and walking ability (Table 1); visual analog scale (VAS) for neuropathic pain (Chang et al., 2021); Barthel index (a measure of activities of daily living); mini-mental state examination (MMSE); and the Brunnstrom scale (Staszewski et al., 2022). Patients were permitted to take analgesic medications according to their conditions. Clinical assessments were performed by the same neurologist to eliminate interrater variability.
Table 1.
Evaluation Form of orientation force, muscle force and walking ability
| Item | Scoring criteria | Score |
|---|---|---|
| Orientation force | 0 = Three items are normal 1 = Two items are normal 2 = One item is normal 3 = Loss of all directional forces |
|
| Muscle strength of affected hand | 0 = Normal 1 = Weakened 2 = The fingertip cannot touch the palm 3 = Completely paralyzed |
|
| Muscle strength of affected limb | 0 = No movement 1 = Stimulate limb flexion 2 = Stimulate limb translation 3 = Lift up, unable to resist gravity 4 = Lift up, able to resist gravity |
|
| Walking ability | 0 = Independent walking 1 = Walk independently, need to help 2 = Sitting alone without support 3 = Bed or wheelchair |
Length of stay
Length of hospitalization and length of time in the ICU were recorded.
Adverse events
Complications and adverse reactions were recorded and handled in a timely manner.
Statistical analysis
Statistical analyses were performed using SPSS software version 15.0 (IBM Corp., Armonk, NY, USA). Data are presented as means ± standard deviation. P < 0.05 was considered significant. Categorical data were compared between groups using the chi-square test. Continuous data were compared using the Mann-Whitney U test. Multiple-group comparisons of time after ICH and GCS score were performed using one-way analysis of variance.
Results
Patient characteristics
Patient characteristics are summarized in Figure 3. Age, sex, time after ICH, hematoma volume, and GCS score did not significantly differ between groups.
Figure 3.

Patient characteristics.
Gender (A), age (B), time after ICH (C), hematoma volume (D), and GCS score (E) did not significantly differ between the groups (P > 0.05). Data are expressed as the mean ± SD and were compared using the chi-square test (A), Mann-Whitney U test (B, D), or one-way analysis of variance (C, E). GCS: Glasgow coma score; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells; ICH: intracerebral hemorrhage.
Orientation, myodynamia, and walking ability
Orientation, myodynamia, and walking ability scores according to group over time are shown in Figure 4A. Group scores did not significantly differ at any time point. At 24 months, the mean score was lower in the combination group than the control and hUC-MSCs groups; however, the difference was not significant.
Figure 4.

Functional outcome scores in the three experimental groups over time.
(A) Orientation, myodynamia, and walking scores. (B) Barthel index scores. (C) Brunnstrom scores. (D) VAS scores. (E) MMSE scores. Data are presented as means ± SD (control group: n = 18; hUC-MSCs group: n = 4; combination group: n = 8). * P < 0.05, **P < 0.01, vs. control group (Mann-Whitney U test). ADL: Activities of daily life; CS: collagen scaffold; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells; ICH: intracerebral hemorrhage; MMSE: Mini-mental State Examination; VAS: Visual Analog Scale.
Barthel index
Barthel index scores according to group over time are shown in Figure 4B. At 24 months, the mean score was significantly higher in the combination group than the control group (P < 0.05).
Brunnstrom scale
Brunnstrom scale scores according to group over time are shown in Figure 4C. Scores did not significantly differ at any time point.
VAS score
VAS pain scale scores according to group over time are shown in Figure 4D. Mean score was significantly lower in the combination group than the control group at 1 month (P < 0.01). Mean scores at other time points did not significantly differ between the groups.
MMSE scale
MMSE scores according to group over time are shown in Figure 4E. At 18 and 24 months, mean score was significantly higher in the combination group than the control group (P < 0.05). These results suggest that transplantation with CS and hUC-MSCs improved cognitive function.
SEPs
Compared with the levels in the control group, SEP amplitude was higher and latency was shorter in the combination group at 24 months (Figure 5). These results suggest that transplantation of CS and hUC-MSCs accelerated recovery of locomotor function.
Figure 5.

Representative SEP tracings.
SEP tracings in the (A) control, (B) hUC-MSCs, and (C) combination groups. SEP amplitude was highest and latency was shortest in the combination group. CS: Collagen scaffold; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells; ICH: intracerebral hemorrhage; SEP: somatosensory evoked potential.
EEG
At 24 months, EEG detection showed occasional slow wave, α or β activity and θ activity in the control, hUC-MSCs and combination groups, but no spikes or sharp waves, or spike and wave discharges. The proportion of patients with α or β activity and θ activity in hUC-MSCs group and combination group was significantly higher than that in control group (P < 0.05; Figure 6). These findings suggest that transplantation of CS and hUC-MSCs did not increase the risk of epilepsy.
Figure 6.

Comparison of the proportion of ICH patients with frequent α or β activities and θ active EEG among the three groups.
*P < 0.05, vs. control group (Chi-square test). EEG: Electroencephalogram; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells; ICH: intracerebral hemorrhage.
CT findings
In the control and hUC-MSCs groups, the post-ICH foci of encephalomalacia did not change much over follow-up (Figure 7A–J). Hematoma volume before surgery in the three groups is shown in Figure 3D. In contrast, the post-ICH foci of encephalomalacia in the combination group decreased in size or disappeared (Figure 7K–O). No sign of tumorigenesis was found at the implantation site. These results suggest that transplantation of CS and hUC-MSCs accelerated central nervous system regeneration.
Figure 7.
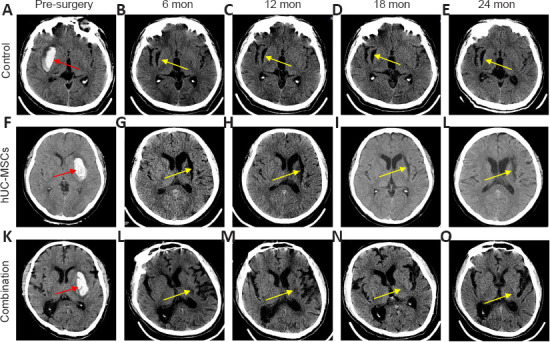
Computerized tomography (CT) imaging before and after surgery in the three groups.
(A–E) In the control group, CT showed a cystic cavity in the right basal ganglia that did not improve during follow-up. (F–J) In the hUC-MSCs group, CT exhibited a cystic cavity in the left basal ganglia that persisted throughout follow-up. (K–O) In the combination group, CT showed a gradual decrease in cystic cavity size from 6 months to 18 months; disappearance was noted at 24 months. Red arrows indicate hemorrhagic foci. Yellow arrows indicate cystic cavities. CS: Collagen scaffold; CT: computerized tomography; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells; ICH: intracerebral hemorrhage.
Safety
Adverse events are shown in Table 2. Seizure, coagulation complications, intracranial infection, and cardiovascular complications did not occur. Nine patients experienced pneumonia. No adverse events were considered transplantation-related. Intracranial rebleeding, deep vein thrombosis, and pneumonia occurred in the control and hUC-MSCs groups. Length of hospitalization and length of ICU stay did not significantly differ between the combination group and the control group or hUC-MSCs group (Figure 8A and B).
Table 2.
Adverse events in control, hUC-MSCs and combination groups
| Adverse events | Control group n = 18) | hUC-MSCs group (n = 4) | Combination group (n = 8) |
|---|---|---|---|
| Seizures | 0 | 0 | 0 |
| Intracranial rebleeding | 0 | 1 | 0 |
| Intracranial infection | 0 | 0 | 0 |
| Pneumonia | 6 | 1 | 2 |
| Complications of coagulation and bleeding | 0 | 0 | 0 |
| Deep vein thrombosis | 0 | 1 | 0 |
| Cardiovascular complications | 0 | 0 | 0 |
hUC-MSCs: Human umbilical cord-derived mesenchymal stem cells.
Figure 8.

Length of hospital stay and NICU stay according to group.
(A) Length of hospital stay did not significantly differ between the combination group and the control group or hUC-MSCs group. (B) Length of NICU stay did not significantly differ between the combination group and the control group or hUC-MSCs group. Data are presented as means ± standard deviation (control group: n = 18; hUC-MSCs group: n = 4; combination group: n = 8) and were analyzed using the Mann-Whitney U test. CS: Collagen scaffold; hUC-MSCs: human umbilical cord-derived mesenchymal stem cells; ICH: intracerebral hemorrhage; NICU: neurological intensive care unit.
Discussion
ICH can be neurologically devastating and can impose an economic burden on families and society. However, there is currently no effective treatment (Rouanet et al., 2017; Qian et al., 2021). In our study, transplantation of CS and hUC-MSCs resulted in higher Barthel index, VAS, and MMSE scores; increased frequency of α, β, and θ waves on EEG, and smaller foci of encephalomalacia on CT. No serious adverse reactions such as seizure, intracranial infection, myocardial infarction, or tumor were observed over 24 months of follow-up. These findings suggest that transplantation of CS and hUC-MSCs is safe and effective for treating patients with ICH.
Transplantation of CS and hUC-MSCs did not increase the length of hospital stay. However, several mild adverse events occurred, including pneumonia and urinary tract infection, which resolved after antibiotic administration. In the hUC-MSCs group, one patient developed deep venous thrombosis. These adverse events are unlikely to be directly related to transplantation.
Various types of biomaterial have been explored for brain injury repair in animal models, including chitosan, hyaluronic acid, and fibrous protein (Jiang et al., 2021). Collagen has been considered a suitable biomaterial because of its accessibility, biocompatibility, biodegradability and low immunogenicity (Rezvani Ghomi et al., 2021). Recent clinical trials examining transplantation of CS have demonstrated its safety (Xiao et al., 2016, 2018; Zhao et al., 2017). Similarly, transplantation of hUC-MSCs to treat ICH has been a recent area of focus. In our study, severe adverse events such as tumorigenesis and infection were not associated with transplantation. Zahra et al. (2020) reported that hUC-MSC transplantation is safe in patients with ICH. Larocca et al. (2017) reported that image-guided percutaneous intralesional administration of hUC-MSCs is safe in patients with spinal cord injury. The safety of hUC-MSC transplantation is primarily owed to advances in cellular harvesting, isolation, culturing and evaluation. To more thoroughly evaluate adverse events, studies with follow-up longer than 2 years are needed.
Activities of daily living were improved after implantation of CS with MSCs. Compared with the control group, ADL scores for getting dressed and moving significantly increased in the combination group at 24 months, which indicated that the treatment improved self-care ability. Barthel index scores were higher in the combination group than the control group, suggesting a positive effect on activities of daily living. Surprisingly, some patients showed improvement in Barthel index score without improvement in Brunnstrom scale score. This was likely related to long-term training. Long-term follow-up will be intriguing.
Electrophysiological examinations are useful for evaluating sensory function after ICH. They can provide a quantitative assessment of reticular circuitry changes and assist with comprehending restoration mechanisms, such as myelinization and synaptization (Lu et al., 2012; van Gorp et al., 2013; Rosenzweig et al., 2018). The mechanism of an intervention used for promoting recovery of neurological function may be embodied in changes in electrical signals. In our study, EEG examination 24 months after transplantation found that patients in the hUC-MSCs and combination groups showed greater α or β activities and θ activity compared with the control group; however, all patients were free of epileptic waves such as spike wave and spike slow wave. Alpha and β are medium and high frequency activities that represent processing of different information and are a sign of sensorimotor activity. Beta activity in particular is the main component of the excitation mechanism while θ is related to mental work (Müller-Putz, 2020).The increased frequency of these waveforms indicated that CS and hUC-MSCs transplantation increased the electrical activity of the brain. It may be that CS and hUC-MSCs transplantation promoted the remodeling of neural pathways or neural repair and regeneration. SEPs recovered 2 years after transplantation. Furthermore, some patients in the combination group showed positive changes in upper extremity SEPs. SEP amplitude was higher and latency was shorter in the combination group, suggesting that transplantation of CS combined with hUC-MSCs improves conductivity repair in ICH (Lu et al., 2012). Electrophysiological improvement after implantation may be attributed to several mechanisms including remyelination, reconnection of damaged nerve fibers, and/or new neural circuitry activity (Curt and Dietz, 1999; Xie and Boakye, 2008).
In addition to motor and sensory function, assessment of cognitive function is required to fully evaluate neurological recovery after ICH. Cognitive dysfunction is common after ICH and may be severe (Scopelliti et al., 2022). Furthermore, it responds poorly to conventional treatment. We observed that MMSE scores were significantly higher in the combination group than the control group. Similarly, Yip et al. (2021) reported mild improvement in cognitive function after hUC-MSC transplantation. Transplantation appears to be beneficial for improving cognitive function.
As stem cells secrete prostaglandins and cytokines, they can trigger nociceptors, regulate the expression of sensory neuron genes, and activate aberrant changes in central nervous system networks that lead to neuropathic pain, spasticity, or dystonia (Hofstetter et al., 2005; Macias et al., 2006). Furthermore, several studies have reported that stem cell transplantation increases the risk of neuropathic pain (Hofstetter et al., 2005). In our study, patients who underwent transplantation of CS with hUC-MSCs reported lower VAS pain scores 1 month after surgery than those in the other two groups. Furthermore, pain scores in these patients did not significantly increase later in the study period. Therefore, transplantation of CS with hUC-MSCs did not seem to increase neuropathic pain.
In our study, patients in the combination group showed a reduction or disappearance in the foci of ICH-related encephalomalacia. However, these foci persisted in the control and hUC-MSC group patients. Chen et al. (2013) reported CT results after hUC-MSC therapy in stroke patients that are similar to ours. The reduction or disappearance of the foci of encephalomalacia may reflect axonal regeneration. At present, brain injury researchers are focusing on diffusion tensor imaging (Douglas et al., 2018). Diffusion tensor tractography, which intuitively describes the distribution of white matter fiber bundles, can quantitatively evaluate white matter tracts by measuring diffusion of water molecules and accurately predict neurological recovery (Cho and Jang, 2021). Use of diffusion tensor tractography may increase the reliability of our results.
Cell delivery for transplantation in the central nervous system can be performed via intravenous, intrathecal, and intramedullary injections. Intravenous delivery is easiest but has unsatisfactory results because the transplanted cells must penetrate the blood-brain barrier (Pal et al., 2009; Mäkelä et al., 2015). Intrathecal injection is more conducive (Bakshi et al., 2004; Paul et al., 2009) but has several disadvantages. First, a large number of stem cells is required. Second, intramedullary or subarachnoid adhesions may block stem cells from migrating to the target. Third, therapeutic stem cell homing effects may not occur in ICH (McColgan et al., 2011; Saberi et al., 2011; Park et al., 2012a). Although many studies have reported the use of intramedullary injection for transplantation (Saberi et al., 2011; Park et al., 2012b; Jiang et al., 2013; Larocca et al., 2017), this strategy did not achieve significant effects in ICH patients. Cerebral edema, ischemia, free radical production, necrosis, and hemorrhage occur in the area of brain injury in these patients. Hematoma that cannot be removed impedes neural regeneration (Lukovic et al., 2015). Surgical hematoma removal is a direct approach for eliminating the impediment. We speculate that surgical removal potentially affects neurological improvement by improving the hematoma microenvironment.
In conclusion, our study has some encouraging results, which indicate that transplantation of hUC-MSCs and CS is safe and effective in ICH patients. However, it has several limitations, especially the number of patients. Initially, patients were included and excluded in strict accordance with the experimental protocol. However, some patients withdrew from the trial for various reasons. Considering experimental preciseness, it was difficult to recruit new volunteers because the trial’s uncertainty and the COVID-19 pandemic. We will make further improvements in future studies. We hope that this trial can provide the basis for a new method of ICH treatment in the future and that future studies will take the shortcomings of this trial into account, so as to obtain more complete and useful experimental results.
Acknowledgments:
We thank Professor Sai Zhang (Yantai Zhenghai Biotechnology Co., Ltd.) for financial assistance, and thank to the team of Professor Jian-Wu Dai (Institute of Genetics and Developmental Biology, Chinese Academy of Sciences) for technical support.
Footnotes
Author contributions: Study design: XYL, WSD, XYC; trial implementation: XYL, WSD, ZQW, ZCL, SLC, ZS, QZ, JL, XYC; trial: XYL, WSD, ZQW; material contribution and equipment coordination: JL, XYC; manuscript writing: XYL, WSD. All authors approved the final version of the manuscript.
Conflicts of interest: The authors declare no competing interests.
Data availability statement: No additional data are available.
Open peer reviewer: Nemil N. Bhatt, The University of Texas Medical Branch at Galveston, USA.
P-Reviewer: Bhatt NN; C-Editor: Zhao M; S-Editors: Yu J, Li CH; L-Editors: Wetzel M, Song LP; T-Editor: Jia Y
Contributor Information
Jin Liang, Email: liangjin1975@126.com.
Xu-Yi Chen, Email: chenxuyi1979@126.com.
References
- 1.Aronowski J, Zhao X. Molecular pathophysiology of cerebral hemorrhage:secondary brain injury. Stroke. 2011;42:1781–1786. doi: 10.1161/STROKEAHA.110.596718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakshi A, Hunter C, Swanger S, Lepore A, Fischer I. Minimally invasive delivery of stem cells for spinal cord injury:advantages of the lumbar puncture technique. J Neurosurg Spine. 2004;1:330–337. doi: 10.3171/spi.2004.1.3.0330. [DOI] [PubMed] [Google Scholar]
- 3.Bonaventura G, Incontro S, Iemmolo R, La Cognata V, Barbagallo I, Costanzo E, Barcellona ML, Pellitteri R, Cavallaro S. Dental mesenchymal stem cells and neuro-regeneration:a focus on spinal cord injury. Cell Tissue Res. 2020;379:421–428. doi: 10.1007/s00441-019-03109-4. [DOI] [PubMed] [Google Scholar]
- 4.Bydon M, Dietz AB, Goncalves S, Moinuddin FM, Alvi MA, Goyal A, Yolcu Y, Hunt CL, Garlanger KL, Del Fabro AS, Reeves RK, Terzic A, Windebank AJ, Qu W. CELLTOP clinical trial:first report from a phase 1 trial of autologous adipose tissue-derived mesenchymal stem cells in the treatment of paralysis due to traumatic spinal cord injury. Mayo Clin Proc. 2020;95:406–414. doi: 10.1016/j.mayocp.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Cao Y, Yu S, Zhang Q, Yu T, Liu Y, Sun Z, Zhao M, Wang W, Zhao JZ. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders:executive summary and 2019 update of clinical management of intracerebral haemorrhage. Stroke Vasc Neurol. 2020;5:396–402. doi: 10.1136/svn-2020-000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang WH, Tu LW, Pei YC, Chen CK, Wang SH, Wong AM. Comparison of the effects between lasers applied to myofascial trigger points and to classical acupoints for patients with cervical myofascial pain syndrome. Biomed J. 2021;44:739–747. doi: 10.1016/j.bj.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen L, Xi H, Huang H, Zhang F, Liu Y, Chen D, Xiao J. Multiple cell transplantation based on an intraparenchymal approach for patients with chronic phase stroke. Cell Transplant 22 Suppl. 2013;1:S83–91. doi: 10.3727/096368913X672154. [DOI] [PubMed] [Google Scholar]
- 8.Cho MJ, Jang SH. Delayed development of aphasia related to degeneration of the arcuate fasciculus in the dominant hemisphere nine years after the onset in a patient with intracerebral hemorrhage:a case report. BMC Neurol. 2021;21:166. doi: 10.1186/s12883-021-02199-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curt A, Dietz V. Electrophysiological recordings in patients with spinal cord injury:significance for predicting outcome. Spinal Cord. 1999;37:157–165. doi: 10.1038/sj.sc.3100809. [DOI] [PubMed] [Google Scholar]
- 10.Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions:the TREND statement. Am J Public Health. 2004;94:361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gladstone DJ, Aviv RI, Demchuk AM, Hill MD, Thorpe KE, Khoury JC, Sucharew HJ, Al-Ajlan F, Butcher K, Dowlatshahi D, Gubitz G, De Masi S, Hall J, Gregg D, Mamdani M, Shamy M, Swartz RH, Del Campo CM, Cucchiara B, Panagos P, et al. Effect of recombinant activated coagulation factor vii on hemorrhage expansion among patients with spot sign-positive acute intracerebral hemorrhage:The SPOTLIGHT and STOP-IT randomized clinical trials. JAMA Neurol. 2019;76:1493–1501. doi: 10.1001/jamaneurol.2019.2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hallevi H, Dar NS, Barreto AD, Morales MM, Martin-Schild S, Abraham AT, Walker KC, Gonzales NR, Illoh K, Grotta JC, Savitz SI. The IVH score:a novel tool for estimating intraventricular hemorrhage volume:clinical and research implications. Crit Care Med. 2009;37:969–974, e1. doi: 10.1097/CCM.0b013e318198683a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hesami O, Kasmaei HD, Matini F, Assarzadegan F, Mansouri B, Jabbehdari S. Relationship between intracerebral hemorrhage and diabetes mellitus:a case-control study. Journal of clinical and diagnostic research :JCDR. 2015;9:OC08–10. doi: 10.7860/JCDR/2015/12226.3741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hofstetter CP, Holmström NA, Lilja JA, Schweinhardt P, Hao J, Spenger C, Wiesenfeld-Hallin Z, Kurpad SN, Frisén J, Olson L. Allodynia limits the usefulness of intraspinal neural stem cell grafts;directed differentiation improves outcome. Nat Neurosci. 2005;8:346–353. doi: 10.1038/nn1405. [DOI] [PubMed] [Google Scholar]
- 15.Jiang J, Dai C, Liu X, Dai L, Li R, Ma K, Xu H, Zhao F, Zhang Z, He T, Niu X, Chen X, Zhang S. Implantation of regenerative complexes in traumatic brain injury canine models enhances the reconstruction of neural networks and motor function recovery. Theranostics. 2021;11:768–788. doi: 10.7150/thno.50540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jiang PC, Xiong WP, Wang G, Ma C, Yao WQ, Kendell SF, Mehling BM, Yuan XH, Wu DC. A clinical trial report of autologous bone marrow-derived mesenchymal stem cell transplantation in patients with spinal cord injury. Exp Ther Med. 2013;6:140–146. doi: 10.3892/etm.2013.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karussis D, Karageorgiou C, Vaknin-Dembinsky A, Gowda-Kurkalli B, Gomori JM, Kassis I, Bulte JW, Petrou P, Ben-Hur T, Abramsky O, Slavin S. Safety and immunological effects of mesenchymal stem cell transplantation in patients with multiple sclerosis and amyotrophic lateral sclerosis. Arch Neurol. 2010;67:1187–1194. doi: 10.1001/archneurol.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larocca TF, Macêdo CT, Souza BSF, Andrade-Souza YM, Villarreal CF, Matos AC, Silva DN, da Silva KN, de Souza C, Paixão DDS, Bezerra MDR, Alves RL, Soares MBP, Dos Santos RR. Image-guided percutaneous intralesional administration of mesenchymal stromal cells in subjects with chronic complete spinal cord injury:a pilot study. Cytotherapy. 2017;19:1189–1196. doi: 10.1016/j.jcyt.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Law ZK, Appleton JP, Bath PM, Sprigg N. Management of acute intracerebral haemorrhage - an update. Clin Med (Lond) 2017;17:166–172. doi: 10.7861/clinmedicine.17-2-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li L, Poon MTC, Samarasekera NE, Perry LA, Moullaali TJ, Rodrigues MA, Loan JJM, Stephen J, Lerpiniere C, Tuna MA, Gutnikov SA, Kuker W, Silver LE, Al-Shahi Salman R, Rothwell PM. Risks of recurrent stroke and all serious vascular events after spontaneous intracerebral haemorrhage:pooled analyses of two population-based studies. Lancet Neurol. 2021;20:437–447. doi: 10.1016/S1474-4422(21)00075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li X, Xiao Z, Han J, Chen L, Xiao H, Ma F, Hou X, Li X, Sun J, Ding W, Zhao Y, Chen B, Dai J. Promotion of neuronal differentiation of neural progenitor cells by using EGFR antibody functionalized collagen scaffolds for spinal cord injury repair. Biomaterials. 2013;34:5107–5116. doi: 10.1016/j.biomaterials.2013.03.062. [DOI] [PubMed] [Google Scholar]
- 22.Li X, Tan J, Xiao Z, Zhao Y, Han S, Liu D, Yin W, Li J, Li J, Wanggou S, Chen B, Ren C, Jiang X, Dai J. Transplantation of hUC-MSCs seeded collagen scaffolds reduces scar formation and promotes functional recovery in canines with chronic spinal cord injury. Sci Rep. 2017;7:43559. doi: 10.1038/srep43559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin H, Chen B, Wang B, Zhao Y, Sun W, Dai J. Novel nerve guidance material prepared from bovine aponeurosis. J Biomed Mater Res A. 2006;79:591–598. doi: 10.1002/jbm.a.30862. [DOI] [PubMed] [Google Scholar]
- 24.Liu S, Xie YY, Wang LD, Tai CX, Chen D, Mu D, Cui YY, Wang B. A multi-channel collagen scaffold loaded with neural stem cells for the repair of spinal cord injury. Neural Regen Res. 2021;16:2284–2292. doi: 10.4103/1673-5374.310698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu P, Wang Y, Graham L, McHale K, Gao M, Wu D, Brock J, Blesch A, Rosenzweig ES, Havton LA, Zheng B, Conner JM, Marsala M, Tuszynski MH. Long-distance growth and connectivity of neural stem cells after severe spinal cord injury. Cell. 2012;150:1264–1273. doi: 10.1016/j.cell.2012.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lukovic D, Stojkovic M, Moreno-Manzano V, Jendelova P, Sykova E, Bhattacharya SS, Erceg S. Concise review:reactive astrocytes and stem cells in spinal cord injury:good guys or bad guys? Stem Cells. 2015;33:1036–1041. doi: 10.1002/stem.1959. [DOI] [PubMed] [Google Scholar]
- 27.Macias MY, Syring MB, Pizzi MA, Crowe MJ, Alexanian AR, Kurpad SN. Pain with no gain:allodynia following neural stem cell transplantation in spinal cord injury. Exp Neurol. 2006;201:335–348. doi: 10.1016/j.expneurol.2006.04.035. [DOI] [PubMed] [Google Scholar]
- 28.Mäkelä T, Takalo R, Arvola O, Haapanen H, Yannopoulos F, Blanco R, Ahvenjärvi L, Kiviluoma K, Kerkelä E, Nystedt J, Juvonen T, Lehenkari P. Safety and biodistribution study of bone marrow-derived mesenchymal stromal cells and mononuclear cells and the impact of the administration route in an intact porcine model. Cytotherapy. 2015;17:392–402. doi: 10.1016/j.jcyt.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 29.McColgan P, Sharma P, Bentley P. Stem cell tracking in human trials:a meta-regression. Stem Cell Rev Rep. 2011;7:1031–1040. doi: 10.1007/s12015-011-9260-8. [DOI] [PubMed] [Google Scholar]
- 30.Nakano M, Fujimiya M. Potential effects of mesenchymal stem cell derived extracellular vesicles and exosomal miRNAs in neurological disorders. Neural Regen Res. 2021;16:2359–2366. doi: 10.4103/1673-5374.313026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pal R, Venkataramana NK, Bansal A, Balaraju S, Jan M, Chandra R, Dixit A, Rauthan A, Murgod U, Totey S. Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia:a pilot clinical study. Cytotherapy. 2009;11:897–911. doi: 10.3109/14653240903253857. [DOI] [PubMed] [Google Scholar]
- 32.Park JH, Kim DY, Sung IY, Choi GH, Jeon MH, Kim KK, Jeon SR. Long-term results of spinal cord injury therapy using mesenchymal stem cells derived from bone marrow in humans. Neurosurgery. 2012a;70:1238–1247. doi: 10.1227/NEU.0b013e31824387f9. discussion 1247. [DOI] [PubMed] [Google Scholar]
- 33.Park SI, Lim JY, Jeong CH, Kim SM, Jun JA, Jeun SS, Oh WI. Human umbilical cord blood-derived mesenchymal stem cell therapy promotes functional recovery of contused rat spinal cord through enhancement of endogenous cell proliferation and oligogenesis. J Biomed Biotechnol. 2012b;2012:362473. doi: 10.1155/2012/362473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paul C, Samdani AF, Betz RR, Fischer I, Neuhuber B. Grafting of human bone marrow stromal cells into spinal cord injury:a comparison of delivery methods. Spine (Phila Pa 1976) 2009;34:328–334. doi: 10.1097/BRS.0b013e31819403ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qian X, Lan S, Zhang X. Effects of mild hypothermia therapy combined with minimally invasive debridement in patients with hypertensive intracranial hemorrhage:a randomized controlled study. Am J Transl Res. 2021;13:7997–8003. [PMC free article] [PubMed] [Google Scholar]
- 36.Qureshi AI, Ali Z, Suri MF, Shuaib A, Baker G, Todd K, Guterman LR, Hopkins LN. Extracellular glutamate and other amino acids in experimental intracerebral hemorrhage:an in vivo microdialysis study. Crit Care Med. 2003;31:1482–1489. doi: 10.1097/01.CCM.0000063047.63862.99. [DOI] [PubMed] [Google Scholar]
- 37.Rosenzweig ES, Brock JH, Lu P, Kumamaru H, Salegio EA, Kadoya K, Weber JL, Liang JJ, Moseanko R, Hawbecker S, Huie JR, Havton LA, Nout-Lomas YS, Ferguson AR, Beattie MS, Bresnahan JC, Tuszynski MH. Restorative effects of human neural stem cell grafts on the primate spinal cord. Nat Med. 2018;24:484–490. doi: 10.1038/nm.4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rouanet C, Reges D, Rocha E, Gagliardi V, Silva GS. Traumatic spinal cord injury:current concepts and treatment update. Arq Neuropsiquiatr. 2017;75:387–393. doi: 10.1590/0004-282X20170048. [DOI] [PubMed] [Google Scholar]
- 39.Saberi H, Firouzi M, Habibi Z, Moshayedi P, Aghayan HR, Arjmand B, Hosseini K, Razavi HE, Yekaninejad MS. Safety of intramedullary Schwann cell transplantation for postrehabilitation spinal cord injuries:2-year follow-up of 33 cases. J Neurosurg Spine. 2011;15:515–525. doi: 10.3171/2011.6.SPINE10917. [DOI] [PubMed] [Google Scholar]
- 40.Scopelliti G, Casolla B, Boulouis G, Kuchcinski G, Moulin S, Leys D, Henon H, Cordonnier C, Pasi M. Long-term neuropsychiatric symptoms in spontaneous intracerebral haemorrhage survivors. J Neurol Neurosurg Psychiatry. 2022;93:232–237. doi: 10.1136/jnnp-2021-327557. [DOI] [PubMed] [Google Scholar]
- 41.Staszewski J, St?pień A, Piusińska-Macoch R, D?biec A, Gniadek-Olejniczak K, Frankowska E, Maliborski A, Chadaide Z, Balo D, Król B, Namias R, Harston G, Mróz J, Piasecki P. Efficacy of cerebrolysin treatment as an add-on therapy to mechanical thrombectomy in patients with acute ischemic stroke due to large vessel occlusion:study protocol for a prospective, open label, single-center study with 12 months of follow-up. Front Neurol. 2022;13:910697. doi: 10.3389/fneur.2022.910697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stokols S, Tuszynski MH. Freeze-dried agarose scaffolds with uniaxial channels stimulate and guide linear axonal growth following spinal cord injury. Biomaterials. 2006;27:443–451. doi: 10.1016/j.biomaterials.2005.06.039. [DOI] [PubMed] [Google Scholar]
- 43.Tsai MJ, Liou DY, Lin YR, Weng CF, Huang MC, Huang WC, Tseng FW, Cheng H. Attenuating spinal cord injury by conditioned medium from bone marrow mesenchymal stem cells. J Clin Med. 2018;8:23. doi: 10.3390/jcm8010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tu Y, Chen C, Sun HT, Cheng SX, Liu XZ, Qu Y, Li XH, Zhang S. Combination of temperature-sensitive stem cells and mild hypothermia:a new potential therapy for severe traumatic brain injury. J Neurotrauma. 2012;29:2393–2403. doi: 10.1089/neu.2012.2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Urdzíková LM, Růžička J, LaBagnara M, Kárová K, Kubinová Š, Jiráková K, Murali R, Syková E, Jhanwar-Uniyal M, Jendelová P. Human mesenchymal stem cells modulate inflammatory cytokines after spinal cord injury in rat. Int J Mol Sci. 2014;15:11275–11293. doi: 10.3390/ijms150711275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Gorp S, Leerink M, Kakinohana O, Platoshyn O, Santucci C, Galik J, Joosten EA, Hruska-Plochan M, Goldberg D, Marsala S, Johe K, Ciacci JD, Marsala M. Amelioration of motor/sensory dysfunction and spasticity in a rat model of acute lumbar spinal cord injury by human neural stem cell transplantation. Stem Cell Res Ther. 2013;4:57. doi: 10.1186/scrt209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang GH, Liu Y, Wu XB, Lu Y, Liu J, Qin YR, Li T, Duan HF. Neuroprotective effects of human umbilical cord-derived mesenchymal stromal cells combined with nimodipine against radiation-induced brain injury through inhibition of apoptosis. Cytotherapy. 2016;18:53–64. doi: 10.1016/j.jcyt.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 48.Wang N, Xiao Z, Zhao Y, Wang B, Li X, Li J, Dai J. Collagen scaffold combined with human umbilical cord-derived mesenchymal stem cells promote functional recovery after scar resection in rats with chronic spinal cord injury. J Tissue Eng Regen Med. 2018;12:e1154–e1163. doi: 10.1002/term.2450. [DOI] [PubMed] [Google Scholar]
- 49.Xiao Z, Tang F, Zhao Y, Han G, Yin N, Li X, Chen B, Han S, Jiang X, Yun C, Zhao C, Cheng S, Zhang S, Dai J. Significant improvement of acute complete spinal cord injury patients diagnosed by a combined criteria implanted with neuroregen scaffolds and mesenchymal stem cells. Cell Transplant. 2018;27:907–915. doi: 10.1177/0963689718766279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xiao Z, Tang F, Tang J, Yang H, Zhao Y, Chen B, Han S, Wang N, Li X, Cheng S, Han G, Zhao C, Yang X, Chen Y, Shi Q, Hou S, Zhang S, Dai J. One-year clinical study of NeuroRegen scaffold implantation following scar resection in complete chronic spinal cord injury patients. Sci China Life Sci. 2016;59:647–655. doi: 10.1007/s11427-016-5080-z. [DOI] [PubMed] [Google Scholar]
- 51.Xie J, Boakye M. Electrophysiological outcomes after spinal cord injury. Neurosurg Focus. 2008;25:E11. doi: 10.3171/FOC.2008.25.11.E11. [DOI] [PubMed] [Google Scholar]
- 52.Yang Y, Ye G, Zhang YL, He HW, Yu BQ, Hong YM, You W, Li X. Transfer of mitochondria from mesenchymal stem cells derived from induced pluripotent stem cells attenuates hypoxia-ischemia-induced mitochondrial dysfunction in PC12 cells. Neural Regen Res. 2020;15:464–472. doi: 10.4103/1673-5374.266058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yip HK, Lin KC, Sung PH, Chiang JY, Yin TC, Wu RW, Chen KH. Umbilical cord-derived MSC and hyperbaric oxygen therapy effectively protected the brain in rat after acute intracerebral haemorrhage. J Cell Mol Med. 2021;25:5640–5654. doi: 10.1111/jcmm.16577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zahra K, Turnbull MT, Zubair AC, Siegel JL, Venegas-Borsellino CP, Tawk RG, Freeman WD. A Combined Approach to Intracerebral Hemorrhage:Intravenous Mesenchymal Stem Cell Therapy with Minimally Invasive Hematoma Evacuation. J Stroke Cerebrovasc Dis. 2020;29:104931. doi: 10.1016/j.jstrokecerebrovasdis.2020.104931. [DOI] [PubMed] [Google Scholar]
- 55.Zhang J, Lu X, Feng G, Gu Z, Sun Y, Bao G, Xu G, Lu Y, Chen J, Xu L, Feng X, Cui Z. Chitosan scaffolds induce human dental pulp stem cells to neural differentiation:potential roles for spinal cord injury therapy. Cell Tissue Res. 2016;366:129–142. doi: 10.1007/s00441-016-2402-1. [DOI] [PubMed] [Google Scholar]
- 56.Zhao Y, Tang F, Xiao Z, Han G, Wang N, Yin N, Chen B, Jiang X, Yun C, Han W, Zhao C, Cheng S, Zhang S, Dai J. Clinical study of neuroregen scaffold combined with human mesenchymal stem cells for the repair of chronic complete spinal cord injury. Cell Transplant. 2017;26:891–900. doi: 10.3727/096368917X695038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhou X, Gu J, Gu Y, He M, Bi Y, Chen J, Li T. Human umbilical cord-derived mesenchymal stem cells improve learning and memory function in hypoxic-ischemic brain-damaged rats via an il-8-mediated secretion mechanism rather than differentiation pattern induction. Cell Physiol Biochem. 2015;35:2383–2401. doi: 10.1159/000374040. [DOI] [PubMed] [Google Scholar]


