Abstract
The diagnosis and management of hidradenitis suppurativa (HS) varies greatly between providers, often resulting in gaps in care including diagnostic delays and poor outcomes. As dermatologists strive to improve HS management, understanding patient perspectives is key. This study aims to characterize existing gaps in HS care as understood through patients’ experiences. This study recruited adult patients with a diagnosis of HS seen at dermatology practices affiliated with Northwestern University. Data were collected through participant surveys and three semi-structured focus groups. Focus group meetings were transcribed verbatim and data were abstracted into themes using conventional content analysis. Six final themes were abstracted after review of 20 pages of transcribed conversation. Four themes centered on improved medical management of HS (access to care, disease-modifying therapies, symptom treatment, prevention of treatment-related adverse events). Two themes centered on supportive care (mental health support, specialized daily wear products). Limitations of this study include single-center recruitment and recall bias introduced by the focus group format. This study identifies six unmet needs for patients with HS and highlights the efficacy of a virtual format for research, conversation, and possibly clinical engagement. Moreover, multiple themes underscore the need for further collaboration across specialties in managing HS.
Keywords: Hidradenitis supprativa, Unmet needs, Gaps in care, Interdisciplinary care
Introduction
Hidradenitis suppurativa (HS) is an inflammatory disorder characterized by recurrent suppurative and painful nodules involving apocrine gland-bearing skin [1]. With an estimated prevalence of 0.05–4.1% HS is associated with tremendous impact on quality of life [2]. Despite the North American and British practice guidelines to stage and treat HS, clinical approach varies among providers [3, 4]. This heterogeneity results in gaps in care manifesting as diagnostic delays, limited treatment access, and unnecessarily poor outcomes [5].
As the dermatologic community strives to improve HS management, understanding patient perspectives is key. While previous studies have utilized standardized questionnaires to survey patients, qualitative analyses have been limited. Thus, the objective of this study is to explore patients’ experiences with HS to characterize existing gaps in care.
Methods
Study design
Data for this study were collected through three institutional review board-approved, semi-structured focus groups comprised of patients with a diagnosis of HS. Focus groups are qualitative research tools useful in providing in-depth information that cannot be obtained in quantitative surveys [6]. Groups are comprised of participants with shared experiences and themes are derived from transcripts of synergistic conversation. To increase validity, three to four focus groups are conducted on the same topic [6].
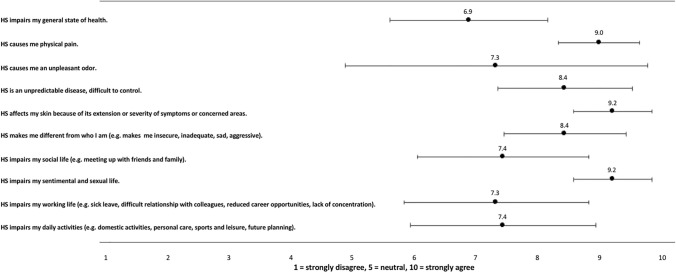
All patients 18 years or older with a diagnosis of HS seen at dermatology practices affiliated with the Northwestern University Department of Dermatology were eligible for participation. Participants were recruited by outreach phone calls and randomly assigned to virtual focus groups on March 31, April 16, and April 30, 2020. Before participating in the focus group, participants independently completed a modified version of the HIDRAdisk questionnaire, a tool validated to rapidly assess HS burden (Fig. 1) [7]. Due to the COVID-19 pandemic, focus groups were held virtually using videoconferencing software, a format validated as non-inferior to in-person focus groups and useful in engaging underrepresented demographics [8]. Participants were given the option to participate anonymously, and focus groups were facilitated by two dermatology residents (P.K.G. and M.A.S.) and one medical student (S.A.C.). A semi-structured series of eight open-ended questions were asked during each session, centered on diagnosis of HS, management options, and patients’ greatest challenges with controlling their disease. Conversation was largely driven by participant-chosen topics, with facilitator guidance to ensure homogeneity between groups.
Fig. 1.
Results of modified HIDRAdisk Questionnairea. aThis figure illustrates average responses and 95% confidence intervals corresponding to each question in the HIDRAdisk questionnaire. Questions are listed on the y-axis and patients can rate each statement on scale of 1–10 indicating degree of agreement or disagreement. N = 9
Data analysis
Verbatim transcripts of the interviews were assessed using “conventional content analysis”—a qualitative data analysis strategy [9, 10]. Three of the authors (P.K.G., M.A.S., and S.A.C.) read through each transcript and identified codes reflective of more than one key thought. Codes were then clustered into themes and compared between reviewers [9]. Themes had to meet the following criteria to be selected: (1) correlates to a minimum of two unique responses and (2) is mentioned in at least two focus groups. Initial themes were selected and two attending dermatologists (C.V.N and K.L.) independently read each transcript and marked statements correlating to the potential themes. Interrater reliability was calculated, and discrepancies were resolved with discussion. Relative importance was determined by frequency of occurrence of theme. Survey data was averaged and corresponding 95% confidence intervals were calculated.
Informed consent of study participants
Participants were provided written informed consent via email and consent forms were collected and reviewed before the start of each focus group. This study was approved by the Northwestern University Institutional Review Board.
Results
Participants
Nine adult patients participated in the study, forming three focus groups of three participants each. Seven (78%) participants were female and the largest contributing age group was 30–39 years of age. Participants predominantly had Hurley stage II and III disease (Table 1).
Table 1.
Participant demographics
| Variables | Number (%) (N = 9) |
|---|---|
| Age | |
| 20–29 | 2 (22%) |
| 30–39 | 6 (67%) |
| 40–49 | 1 (11%) |
| Sex | |
| Female | 7 (78%) |
| Male | 2 (22%) |
| Hurley stage | |
| I | 1 (11%) |
| II | 4 (44%) |
| III | 4 (44%) |
Theme identification and relative importance
The three focus groups resulted in 20 pages of transcribed conversation total, from which 29 codes were abstracted and clustered into seven initial themes. On review by two attending dermatologists, 129 unique statements were ascertained, and interrater reliability was 100% on five of seven themes. The two additional themes had significantly overlapping content, and after discussion, were consolidated into one theme. The final six themes all had corresponding statements in three of three focus groups. The least and most frequently mentioned themes corresponded to seven and 34 unique statements, respectively.
The following themes were identified (Table 2):
Table 2.
Unmet needs in the care of patients with hidradenitis suppurativa
| Domain | Unmet need | |
|---|---|---|
| 1. | Access to reliable healthcare solutions |
Educate dermatologic and primary care providers about hidradenitis suppurativa to expand provider base Create multidisciplinary clinics Develop acute care dermatologic resources to avoid emergency department usage Lower costs to care Improve online resources (medical tools, social media resources) |
| 2. | Better therapeutic options |
Develop novel, validated medications to treat disease Develop novel, validated surgical options |
| 3. | Symptom management | Develop options for managing chronic and acute pain |
| 4. | Prevention of treatment-related adverse effects |
Create strategies to mitigate medication tachyphylaxis Design improved infection prevention strategies |
| 5. | Psychiatric care | Supply easily accessible mental health resources for patients (therapy options, interdisciplinary clinics with psychiatry, support groups) |
| 6. | Specialized products | Design undergarments, clothing, and wound-healing products (dressings, bandages) specialized in the care of hidradenitis suppurativa patients |
Themes are listed in the order of descending relative importance, assigned by frequency of occurrence
Access to reliable healthcare solutions
When asked about finding information about HS, participants overwhelmingly relied on their dermatologists. Multiple participants stated, “I’ve always relied on my doctor”. Participants did not feel online and social media resources compared to the knowledge of their healthcare providers (“literature online is a dead end,” and “I feel that on social media, there isn’t a complete picture”). However, both quality of and access to knowledgeable dermatologists was a source of frustration. For example, one participant stated, “not all [dermatologists] are equal,” and another shared, “it feels difficult to find people who know how to treat this or even who know much about it.” These challenges often arose in the context of diagnostic delays, and one participant shared it took 3 years for her to be diagnosed with HS.
In addition to dermatologists, participants also sought solutions from surgeons, pain specialists, and notably, emergency medicine providers. Participants sometimes managed flares by going to urgent care, and shared, “I’ll have them cut it open and drain it, like spot treatment, but it’s not a great solution.” Lastly, patients shared that lack of insurance coverage and high healthcare costs were barriers to seeking care.
Better therapeutic options
Participants expressed a need for improved treatment options. Participants felt medical therapies for refractory disease were scarce; one participant shared, “the air gets pretty thin in terms of solutions once the disease has progressed,” and another stated, “I’m on antibiotics, finasteride, Humira, a special wash for the shower, a lotion for after the shower, and nothing works”. Tachyphylaxis of medical treatments was an additional concern (“no matter how things work for a while, they always stop working.”). Participants were uncertain of effectiveness of surgical excision and felt significant hesitation about the healing process. “I don’t heal particularly well [from surgery],” and, “the open wounds are a lot,” were two statements corresponding to hesitation in pursuing surgical therapies.
Symptom management
Patients pointed to pain and odor when asked what is most challenging about controlling their disease. During flares, participants experienced, “absolute intense pain that occupies every moment of the day,” with little respite. Further, the pain significantly limited activity. One participant shared, “during my last flare, I couldn’t walk straight or sit down for 2 weeks,” while others echoed having to avoid social gatherings, work, and exercise.
Participants reported trying non-steroidal anti-inflammatories, acetaminophen, opiates, and medical marijuana to manage pain, but were frustrated due to the absence of sustainable and effective solutions. One participant regularly saw a chronic pain specialist.
Likewise, multiple participants identified odor as the biggest gap in care for patients with HS. One participant shared, “if I can get rid of the smell, that would be good. I can do most of it, it’s just the smell that can be really overwhelming.” Similar to severe pain, the odor associated with acute flares also caused significant social and physical activity limitation.
Prevention of treatment-related adverse effects
Most participants had utilized multiple therapeutic options to control their HS—antibiotics, hormonal therapy, immunomodulatory agents, and procedural interventions were discussed specifically. All treatment categories were associated with significant adverse effects, limiting usage despite efficacy and fostering hesitancy to trial additional therapies. One participant shared, “the side effects of what you’re prescribed long-term ends up being worse than the disease they’re trying to fix,” while discussing recurrent yeast infections and nausea secondary to spironolactone and antibiotic dual therapy. Others mentioned antibiotic allergies, and multiple participants mentioned infectious complications from surgical interventions. One patient on an immunomodulatory agent shared, “my primary concern […] is being immunocompromised in the time of coronavirus”.
Psychiatric care
HS significantly impacted participants’ mental health. Participants felt frustrated, isolated, and that poor mental health worsened their disease (“there is an emotional side of this that spirals into ‘how do I deal with this”). Accessing supportive resources (therapists, psychiatrists) was challenging due to lack of specialists and insurance barriers. While some participants found help (“my husband is a big support for me”, and, “I actually have a counselor”), others shared, “it’s not something I really talk to other people about,” and did not seek any mental health support. Others’ inability to understand (“a lot of employers say ‘You don’t look sick’”) and embarrassment were two reasons participants did not seek external support.
Specialized products
Participants noted clothing, bandages, and toiletries could significantly exacerbate their disease. Non-irritating cleansers were preferred for showering, cotton was preferred for undergarments, and specific dressings were identified to promote wound healing without friction or irritation. Participants discovered these specialized products through trial and error.
Survey data
In the ten question HIDRAdisk questionnaire, on average participants agreed with all ten statements (Fig. 1). The top three statements that participants most strongly agreed with included: “HS causes me physical pain”, “HS affects my skin because of its extension or severity of symptoms or concerned areas”, and “HS impairs my sentimental and sexual life”. Participants most variably responded to the statement, “HS causes me an unpleasant odor,” suggesting lack of homogeneity on this topic. Final scores on the HIDRAdisk questionnaire ranged from a low of 59 to a high of 100, validated to correspond to impact on quality of life from a scale of zero to 100 [7].
Discussion
Recent literature has demonstrated an eruption of HS research and clinical guidelines; however, to the authors’ knowledge, few studies exist analyzing the patient experience in an unstructured format [11]. In this study, participants inductively generated six themes, four of which centered on improved medical management of HS (access to care, disease-modifying therapies, symptom treatment, prevention of treatment-related adverse events) and two of which centered on supportive care (mental health support, specialized daily wear products). These themes are listed in Table 2 in the order of descending relative importance.
The most frequently occurring theme was limited access to healthcare solutions, due to (1) financial barriers and (2) scarce knowledgeable providers. The economic burden of HS is estimated to be $6,632 higher than an average patient over a 3-year period [12]. In addition, patients with HS are more likely to be unemployed or on disability and thus have unreliable access to health insurance and increased out-of-pocket costs [13]. These realities underscore the importance of lowering costs to treat HS holistically. However, even when patients can access healthcare, the care received is often subpar. Misdiagnosis of HS is well-established in the literature and improving both medical and layperson informational resources may bridge this gap [2, 14]. Further, educating non-dermatologic physicians about initial diagnosis and treatment would expand access to care in dermatologically underserved communities, as studies show 40–70% of patients first present to general practitioners [15]. Likewise, multidisciplinary clinics can ensure convenience for patients, including specialties such as surgery, pain, psychiatry, and nutrition [16]. Finally, this study demonstrates a need for “acute care dermatology”. HS patients are known to have high ED utilization for flares, but emergency procedures such as deroofing or incision and drainage have poor and unsustainable outcomes [12, 17]. Further, ED visits have been shown to result in prescription of ineffective antibiotics and narcotic pain medications [18]. Thus, creating specialized urgent clinics or appointments can help expand access to high-quality care.
Two themes centered upon a need for improved therapeutic options. Participants were frustrated with limited medical and surgical treatments, both due to (1) lack of long-term effectiveness and (2) significant adverse effects. While a review of current HS treatments is beyond the scope of this article, recent literature has combined anecdotal evidence and clinical trials to aggregate treatment data, potentially helping to enhance innovation [17]. For surgical treatment options, participants were most frustrated with poor, slow wound healing and infectious complications. While a variety of surgical options exist in the treatment of HS, only wide excision for Hurley stage II or III disease is validated to be curative, but involves higher post-operative morbidity [17]. Standardizing surgical treatments and improving wound care practices with the goal of reducing morbidity may help expand safe surgical solutions [15].
Pain, both chronic and acute, was the third most frequently mentioned theme in this study. Participants had unremitting daily pain and found limited relief with medications and intralesional steroid injections. In a review of ED visits, approximately 40% of HS patients reported severe pain, often requiring management with opioid pain medications; an option lamented as unsafe and unsustainable amongst patients in this study [18]. Despite pain correlating with quality of life in patients with HS, limited provider training on pain management in the dermatologic community and ineffective treatments have led to uncontrolled pain being commonplace [19]. A comprehensive psychological, pharmacological, and alternative approach to pain management has been suggested by clinical guidelines, and additional collaboration across specialties (pain specialists, anesthesiology) is paramount [19].
Lacking psychiatric support was another theme—the high incidence of depression and anxiety associated with HS is well-known [20]. The importance of recognition and treatment of these psychiatric comorbidities has been emphasized in the literature, but still lacks implementation. The creation of multidisciplinary clinics with integrated psychologic support could improve patient outcomes and destigmatize seeking mental health support [15, 16]. In addition, beyond medical treatment of depression and anxiety, patients with subclinical mental health challenges could greatly benefit from therapeutic support groups, as created in this study. At the conclusion of focus groups, most participants appreciated connecting with others undergoing similar challenges, particularly on a virtual platform [21].
As the final theme, participants unanimously identified a lack of specialized clothing and wound healing products as a source of frustration. Participants largely found optimal fabrics and wound dressings through trial and error. Avoiding mechanical stress and minimizing sweat and bacterial colonization have been identified as goals in selecting specialized products for patients; however, a centralized database of preferred products remains nonexistent [22]. Thus, improving informational guides with data on patient-preferred products could be of utility.
Lastly, this study presents a unique perspective due to utilization of a virtual interface. Participants responded positively to the flexibility of videoconferencing and appreciated the opportunity to engage with optional anonymity (web camera disabled) [21]. The convenience of participating without having to leave home was lauded as an inability to travel long distances or work in-person is a hallmark of HS [21, 23]. During the COVID-19 pandemic, multiple experts underscored the importance of virtual outpatient care, particularly for patients with dermatologic diseases requiring frequent healthcare utilization [24]. This study pushes this notion a step further by demonstrating utility in virtual support groups to augment patient care. Most participants indicated interest in continuing the virtual conversations amongst themselves to trade ideas and build community. While not the initial intent of this study, such statements suggest therapeutic utility of virtual support groups as well.
Overall, this study has identified six unmet needs for patients with HS and highlighted the efficacy of a virtual format for research, conversation, and possibly clinical engagement. While the dermatologic community is at the forefront of treating HS, the broad range of themes encompassed in this article underscores the need for further teamwork and innovation.
Limitations
Generalizability of this data is limited by the single-center recruitment of participants; however, this was mitigated by 33% of participants reporting narratives of care from non-Northwestern medical providers. In addition, focus groups, by design, require a small sample size and risk both selection and recall bias.
Author contributions
All authors contributed equally to the production of this manuscript.
Funding
None.
Data availability
Not applicable.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nguyen TV, Damiani G, Orenstein LAV, Hamzavi I, Jemec GB. Hidradenitis suppurativa: an update on epidemiology, phenotypes, diagnosis, pathogenesis, comorbidities and quality of life. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16677. [DOI] [PubMed] [Google Scholar]
- 2.Saunte DML, Jemec GBE. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA. 2017;318(20):2019–2032. doi: 10.1001/jama.2017.16691. [DOI] [PubMed] [Google Scholar]
- 3.Ingram JR, Collier F, Brown D, et al. British Association of Dermatologists guidelines for the management of hidradenitis suppurativa (acne inversa) 2018. Br J Dermatol. 2019;180(5):1009–1017. doi: 10.1111/bjd.17537. [DOI] [PubMed] [Google Scholar]
- 4.Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81(1):76–90. doi: 10.1016/j.jaad.2019.02.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garg A, Neuren E, Cha D, et al. Evaluating patients' unmet needs in hidradenitis suppurativa: results from the Global Survey of Impact and Healthcare Needs (VOICE) project. J Am Acad Dermatol. 2020;82(2):366–376. doi: 10.1016/j.jaad.2019.06.1301. [DOI] [PubMed] [Google Scholar]
- 6.Wong LP. Focus group discussion: a tool for health and medical research. Singap Med J. 2008;49(3):256–260. [PubMed] [Google Scholar]
- 7.Peris K, Lo Schiavo A, Fabbrocini G, et al. HIDRAdisk: validation of an innovative visual tool to assess the burden of hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2019;33(4):766–773. doi: 10.1111/jdv.15425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rupert DJ, Poehlman JA, Hayes JJ, Ray SE, Moultrie RR. Virtual versus in-person focus groups: comparison of costs, recruitment, and participant logistics. J Med Internet Res. 2017;19(3):80. doi: 10.2196/jmir.6980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 10.Raskind IG, Shelton RC, Comeau DL, Cooper HLF, Griffith DM, Kegler MC. A review of qualitative data analysis practices in health education and health behavior research. Health Educ Behav. 2019;46(1):32–39. doi: 10.1177/1090198118795019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Savage KT, Gonzalez Brant E, Flood KS, Salian P, Porter ML, Kimball AB. Publication trends in hidradenitis suppurativa from 2008 to 2018. J Eur Acad Dermatol Venereol. 2020;34(9):1885–1889. doi: 10.1111/jdv.16213. [DOI] [PubMed] [Google Scholar]
- 12.Kirby JS, Miller JJ, Adams DR, Leslie D. Health care utilization patterns and costs for patients with hidradenitis suppurativa. JAMA Dermatol. 2014;150(9):937–944. doi: 10.1001/jamadermatol.2014.691. [DOI] [PubMed] [Google Scholar]
- 13.Zouboulis CC. The socioeconomic burden of hidradenitis suppurativa/acne inversa. Br J Dermatol. 2019;181(1):7–8. doi: 10.1111/bjd.17396. [DOI] [PubMed] [Google Scholar]
- 14.Lee EY, Alhusayen R, Lansang P, Shear N, Yeung J. What is hidradenitis suppurativa? Can Fam Physician. 2017;63(2):114–120. [PMC free article] [PubMed] [Google Scholar]
- 15.Collier EK, Hsiao JL, Shi VY, Naik HB. Comprehensive approach to managing hidradenitis suppurativa patients. Int J Dermatol. 2020;59(6):744–747. doi: 10.1111/ijd.14870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Timila Touhouche A, Chaput B, Marie Rouquet R, et al. Integrated multidisciplinary approach to hidradenitis suppurativa in clinical practice. Int J Womens Dermatol. 2020;6(3):164–168. doi: 10.1016/j.ijwd.2020.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldburg SR, Strober BE, Payette MJ. Hidradenitis suppurativa: current and emerging treatments. J Am Acad Dermatol. 2020;82(5):1061–1082. doi: 10.1016/j.jaad.2019.08.089. [DOI] [PubMed] [Google Scholar]
- 18.Taylor MT, Orenstein LAV, Barbieri JS. Pain severity and management of hidradenitis suppurativa at US emergency department visits. JAMA Dermatol. 2021;157(1):115–117. doi: 10.1001/jamadermatol.2020.4494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Savage KT, Singh V, Patel ZS, et al. Pain management in hidradenitis suppurativa and a proposed treatment algorithm. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Machado MO, Stergiopoulos V, Maes M, et al. Depression and anxiety in adults with hidradenitis suppurativa: a systematic review and meta-analysis. JAMA Dermatol. 2019;155(8):939–945. doi: 10.1001/jamadermatol.2019.0759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stout M. The role of virtual support groups for patients with hidradenitis suppurativa during the COVID-19 pandemic. Int J Womens Dermatol. 2020;6(3):154–155. doi: 10.1016/j.ijwd.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loh TY, Hendricks AJ, Hsiao JL, Shi VY. Undergarment and fabric selection in the management of hidradenitis suppurativa. Dermatology. 2021;237(1):119–124. doi: 10.1159/000501611. [DOI] [PubMed] [Google Scholar]
- 23.Mac Mahon J, Kirthi S, Byrne N, O'Grady C, Tobin AM. An update on health-related quality of life and patient-reported outcomes in hidradenitis suppurativa. Patient Relat Outcome Meas. 2020;11:21–26. doi: 10.2147/PROM.S174299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shah M, Naik HB, Alhusayen R. Hidradenitis suppurativa: the importance of virtual outpatient care during COVID-19 pandemic. J Am Acad Dermatol. 2020;83(1):e81–e82. doi: 10.1016/j.jaad.2020.04.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.