Abstract
Background
Older people are often explicitly or implicitly excluded from research, in particular clinical trials. This means that study findings may not be applicable to them, or that older people may not be offered treatments due to an absence of evidence.
Aims
The aim of this work was to develop recommendations to guide all research relevant to older people.
Methods
A diverse stakeholder group identified barriers and solutions to including older people in research. In parallel, a rapid literature review of published papers was undertaken to identify existing papers on the inclusion of older people in research. The findings were synthesised and mapped onto a socio-ecological model. From the synthesis we identified themes that were developed into initial recommendations that were iteratively refined with the stakeholder group.
Results
A range of individual, interpersonal, organisational, community and policy factors impact on the inclusion of older people in research. A total of 14 recommendations were developed such as removing upper age limits and comorbidity exclusions, involving older people, advocates and health and social care professionals with expertise in ageing in designing the research, and considering flexible or alternative approaches to data collection to maximise opportunities for participation. We also developed four questions that may guide those developing, reviewing and funding research that is inclusive of older people.
Conclusion
Our recommendations provide up to date, practical advice on ways to improve the inclusion of older people in health and care research.
Keywords: inclusion, recommendations, socio-ecological model, older people
Key Points
Individual, interpersonal, organisational, community and policy factors impact on the inclusion of older people in research.
Researchers, reviewers and funders should consider engagement, inclusive study design, adequate resources and communication.
Our 14 recommendations offer practical guidance on ways to improve the inclusion of older people in research.
Introduction
Evidence from health and social care research helps members of the public, patients, practitioners, commissioners and policy makers make decisions about treatment, care and services. However, those recruited into studies, in particular, randomised controlled trials (RCTs), frequently do not represent the population affected by the condition of interest [1, 2]. This impacts people on several levels. Firstly, an inequity in opportunities to participate in and benefit from research. Secondly, arbitrary exclusion (direct or indirect) based on a characteristic such as age is a form of discrimination. Thirdly, study findings may not apply to the breadth of people with a condition, and finally, therapies may not be offered due to absence of evidence or may be ineffective or unsafe. In order to address the lack of representativeness of populations recruited to research studies, the National Institute for Health and Care Research (NIHR) Innovations in Clinical Trials Design and Delivery for the Underserved (INCLUDE) project sought to address the barriers to the inclusion of under-served groups in health and care research [1]. Although there is no single definition for ‘under-served group’, commonly people in such groups have lower rates of inclusion than would be seen in the population of interest, they may engage or respond differently to interventions, or they have a high health and care burden unmatched by the amount of research conducted in that field. Factors to consider in under-served groups include, but are not limited to, demographics (e.g. age, ethnicity, sexual orientation, gender identity), socioeconomic factors (e.g. carers, digitally excluded), health status (e.g. multiple health conditions, hearing impaired) or living circumstances (e.g. care home, homeless).
Heterogeneity is a hallmark of ageing, and older people constitute a broad group, from the robust and healthy through to those with severe frailty and dependency. Older people and those with multiple long terms conditions or frailty are the highest users of health and care resources [3]. Older people are frequently excluded in many areas of healthcare research, through restrictions in upper age limits [4–7], the presence of comorbidities [6, 7] and cognitive impairment [5]. In 2011, McMurdo and colleagues published good practice guidance on improving recruitment of older people to research [8]. They made recommendations on planning and logistic considerations in different settings, recruiting those with impaired capacity and those from ethnic minorities. Nonetheless the problem remains with evidence from a recent review finding that a third of COVID-19 trials had upper age limits that were unjustified, despite COVID-19 disproportionately affecting older people [9].
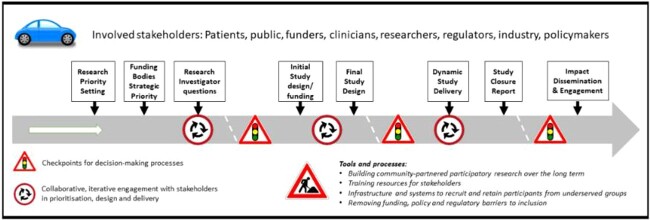
New recommendations on the inclusion of older people in research are needed for several reasons. Firstly, our understanding of under-served groups and how to improve inclusion has evolved in the last decade. For some older people, several factors may impact their inclusion in research and this intersectionality is important (Figure 1). Secondly, the clinical research landscape has evolved with new opportunities and challenges (e.g. digital outcomes, virtual trials) that warrant consideration. Finally, previous recommendations focused on those working in ageing research thus there is an opportunity to refine and extend previous guidance to a broader audience including other specialities.
Figure 1.
Intersectionality of factors that may impact on the inclusion of older people in research.
The aim of our work was to develop system-level principles to guide all research relevant to older people. The objective was to identify factors that impacted the inclusion of older people in research through stakeholder engagement and evidence synthesis. This paper presents the NIHR INCLUDE Older People best practice recommendations.
Developing the INCLUDE older people best practice recommendations
The INCLUDE Older People project began in January 2021 and continued until September 2022. A diverse stakeholder group was established including multi-disciplinary health and care professionals representing geriatrics, general practice, nursing, physiotherapy and psychiatry, charity representatives (Age UK) and those with expertise in health and care research design and delivery (NIHR Clinical Research Network (CRN), Clinical Trials Units, Patient and Public Involvement), and ethics committee membership. The group also included three older people with experience of being involved in research. To maximise their engagement, alongside the stakeholder meetings, one of the academic team met with them separately to discuss key aspects of the work including barriers and solutions to including older people in research and the proposed theory of change model. Whilst the work focused on how to improve participation of older people in research, we also considered principles that may aid retention.
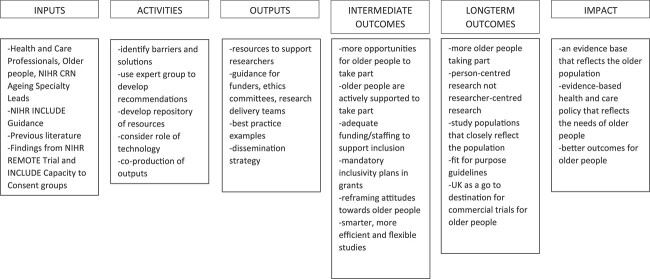
A multi-disciplinary core group (Goodwin, Quinn and Witham) met online in January 2021 and identified key stakeholders needed. The NIHR INCLUDE roadmap (Figure 2) as an initial guide [13] to prompt discussion. Areas for particular focus were non-hospital and non-NHS settings, as well as intersectionality with other under-served groups. This group met throughout the project to synthesise discussions and contributions and to lead development of the recommendations.
-
An initial online stakeholder meeting was held (April 2021). The group discussed and agreed that:
emphasis of recommendations should be on study design and ethics. Regulatory issues would be considered but would not be a primary focus
cross-speciality research that is relevant to older people should be considered, not just ‘ageing’ research
Tools were needed to help researchers or signpost them to existing resources e.g. www.capacityconsent.com or www.trialforge.org
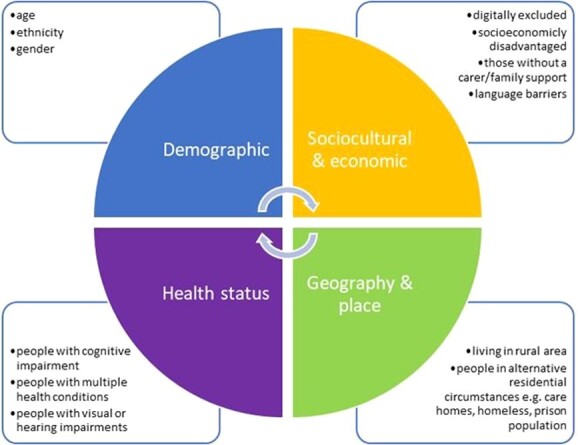
Prior to the next online meeting (June 2021), stakeholders were invited to identify barriers and solutions to including older people in research at key stages of the INCLUDE roadmap [13] and add to a Google Jamboard (real-time digital whiteboard). At the meeting, two parallel groups further discussed factors around inclusion and developed a Theory of Change model (Figure 3) to describe inputs (what was needed), activities (what needed to be done), outputs (what we planned to produce) and outcomes in order to achieve impact. Further suggestions were added in the subsequent months via email or directly onto Jamboard.
In parallel, we conducted a broad rapid scoping search for published English language literature on inclusion of older people in research (March 2022). The aim was to supplement stakeholder activities and provide an overview of relevant literature in this area such as key barriers to including older people in research and potential strategies to improve recruitment and retention. PubMed (Medline), Google Scholar, ScienceDirect and the Age and Ageing journal were searched. We included ‘older adults’, ‘elderly’, ‘recruitment’, ‘retention’, ‘inclusion’ and ‘research’ as search terms using Boolean operators AND and OR.
We conducted the initial synthesis of findings from the literature review with outputs from the stakeholder discussions. Issues relating to the inclusion of older people in research are multi-faceted and complex, thus requiring a systems-level approach. We therefore mapped findings from the review and stakeholder discussions onto a socio-ecological model (SEM) [14]. The SEM (Figure 4) enables mapping of multi-level and interacting factors to help understand how micro, meso and macro-level factors influence the research ecosystem. This approach has been used to better understand recruitment and retention in trials of health interventions [15–17]. From the descriptive synthesis we identified themes that were developed into initial recommendations.
Initial recommendations were presented to the NIHR CRN Ageing National Speciality Group (June 2022) and shared with the stakeholder group (July 2022). Both groups provided feedback and recommendations were revised accordingly.
Revised recommendations were shared with the groups described above (September–October 2022) along with a list of questions to assist researchers, reviewers and funders.
Figure 2.
NIHR INCLUDE Roadmap (reproduced from Witham et al. [13] under CC-BY-4.0 licence).
Figure 3.
Theory of Change for improving the inclusion of older people in research.
Figure 4.
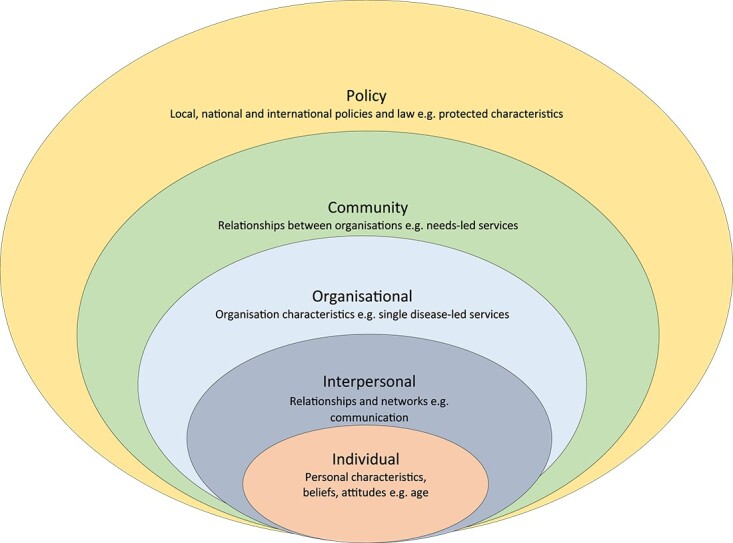
SEM representing the multi-level factors that may impact on the inclusion of older people in research.
Results
A total of 14 recommendations are presented within the SEM and summarised in Table 1. Below we provide rationale for each recommendation with supporting evidence. Examples of good practice and relevant resources are in Appendix 1.
Table 1.
Summary of best practice recommendations for including older people in research.
| SEM Factor | Recommendation |
|---|---|
| 1. Individual factors | 1a. Studies should not have upper age limits in inclusion criteria |
| 1b. Studies should be designed to be inclusive of those with cognitive impairment | |
| 1c. Studies should not have comorbidity exclusions (except where there is an intervention contraindication) | |
| 1d. Use of clear explanations of why research is relevant to older people’s health and wellbeing | |
| 2. Interpersonal factors | 2a. Advocates and peers should be involved in designing research that meets the needs of older people |
| 2b. Health and social care professionals with expertise in ageing should be involved in designing research that meets the needs of older people | |
| 2c. Communication about research should be tailored to the needs of older people | |
| 2d. All older people who meet the eligibility criteria should be offered the opportunity to participate in research | |
| 2e. Consider the involvement of carers or family members and the impact involvement can have on them and the older person | |
| 3. Organisational factors | 3a. Those commissioning, funding and approving research should ensure the inclusion of older people and intersectional factors, such as demographics and health status, have been considered |
| 3b. Those commissioning, funding and approving research should include older people and those with expertise in ageing | |
| 4. Community factors | 4a. Researchers should consider different and flexible approaches to promote accessibility of the research e.g. financial support to attend research centres or offering home visits for data collection |
| 4b. Support, or alternatives should be offered to digital data collection and interventions | |
| 5. Policy factors | 5a. Policymakers should consider the impact of policies on health inequalities in research participation |
Individual factors
Recommendation 1A: Studies should not have upper age limits in inclusion criteria
Some studies still explicitly exclude participants based on chronological age [4, 7]. This approach is ageist and hence a morally indefensible form of discrimination. The heterogeneity of health and function in old age makes chronological age a weak proxy for other factors (e.g. multimorbidity, mobility) that may be more relevant to study design.
Recommendation 1B: Studies should be designed to be inclusive of those with cognitive impairment
Informed consent is a core tenet of research participation. However, blanket exclusion of those with cognitive impairment is discriminatory [18, 19]. The Mental Capacity Act (2005) makes adequate provision for alternative means of participation using consultees [20]. Decisions about capacity to consent need to be taken on an individual basis, and such cut-offs impose a false dichotomy on the concept of capacity for research participation.
Recommendation 1C: Studies should not have comorbidity exclusions (except where there is an intervention contraindication)
Blanket exclusions because of comorbidity not only directly discriminate against participants with multiple conditions but constitute covert age discrimination [7]. Many older people who are the target treatment population for an intervention will have multiple conditions, and excluding such patients risks the production of biassed, unrepresentative research and therefore misleading results. This remains the case even for early phase studies where ‘clean designs’ to minimise heterogeneity may be sought.
Recommendation 1D: Use of clear explanations of why research is relevant to older people’s health and wellbeing
Research should be designed to maximise engagement of the entire population of interest. Some older people may have low interest due to a lack of perceived benefits or relevance of a study to themselves [18].
Some older people may have misconceptions about research, leading to distrust and unwillingness to engage. The issue of trust in health care providers and researchers has been highlighted particularly amongst older people from ethnic minority groups [15]. Engagement with people with varying cultural backgrounds who speak different languages presents further challenges which must be surmounted.
Interpersonal factors
Recommendation 2A: Advocates and peers should be involved in designing research that meets the needs of older people
Personal characteristics may impact on individuals’ perceived and actual ability to take part in research such as general poor health, multiple long-term conditions, fatigue or mobility issues [24, 29, 31]. This means older people may believe they are not able to take part or may have to withdraw from the study. Others may be reluctant to commit to taking part in research due to other priorities e.g. family responsibilities [7, 17].
Recommendation 2B: Health and social care professionals with expertise in ageing should be involved in designing research that meets the needs of older people
Some researchers lack knowledge and understanding of ageing and involving older people in research resulting in inflexible study protocols that don’t accommodate age-related issues [32]. This can result in a general apprehension about recruiting older adults due to a higher likelihood of adverse events and attrition [24, 27].
Recommendation 2C: Communication about research should be tailored to the needs of older people
How research is communicated can have a significant impact on engagement [25, 27, 31]. Some may have difficulty reading and understanding promotional materials to take part in research.
Recommendation 2D: All older people who meet the eligibility criteria should be offered the opportunity to participate in research
Gatekeeping by those involved in recruiting older people can occur based on a misconception that older adults are vulnerable, due to e.g. comorbidities or a lack of mental capacity, and therefore, need to be protected from research [8]. It is important that all those eligible to take part in research be offered the opportunity to make an informed decision themselves. Researchers/clinicians should facilitate access to research and not inhibit it.
Recommendation 2E: Consider the involvement of carers or family members and the impact involvement can have on them and the older person
Lack of support from carers or family members can influence the decision to participate [25–27] and involvement in research can be an additional carer burden. Building a rapport with carers and family members may be important to aid recruitment and retention [8, 26, 33]. For individuals with cognitive impairment, involving carers can aid consent processes, and provide reassurance and encouragement [27, 32, 33].
Organisational factors
Recommendation 3A: Those commissioning, funding or approving research should ensure the inclusion of older people and intersectional factors such as demographics and health status have been considered
Research tends to focus on individual condition processes due to fears that the effects of ageing would impair the ability to report on effects related to a single condition [32]. This focus on single condition at the expense of those living with multiple long-term conditions has resulted in research and guidelines that do not reflect the patients seen in clinical practice.
Recommendation 3B: Those commissioning, funding and approving research should include older people and those with expertise in ageing
Research funders, ethics committees, regulators, sponsors and Research and Development departments may have an overly risk averse approach to involving older people in research that fails to recognise the autonomy of older people [37]. There may also be apprehension to allow inclusion of those who are considered vulnerable. Reviewers and decision makers may lack an understanding of ageing, older people and those living with multiple long-term conditions resulting in ill-informed decision making.
Community factors
Recommendation 4A: Researchers should consider different and flexible approaches to promote accessibility of the research e.g. financial support to attend research centres or offering home visits for data collection
The inaccessibility of research facilities due to the need to travel long distances and/or a lack of available transport are significant barriers to older people taking part in research, especially for those with reduced mobility or fatigue [24, 25, 27] or where costs are prohibitive [25, 27].
Recommendation 4B: Support, or alternatives should be offered for digital data collection and interventions
Whilst there is increasing interest in remote research delivery that may be beneficial for some e.g. those with mobility impairment, caution must be taken not to exacerbate inequalities through digital exclusion [38]. Some may not have access to suitable equipment, or the internet [38]. Older people with equipment may be hesitant due to lack confidence to use it or privacy concerns. Remote trial delivery requires infrastructure and resources [39] and whilst NIHR have an ambition to work towards hybrid and fully remote trials, consideration should be given to those who may be excluded.
Policy factors
Recommendation 5A: Policymakers should consider the impact of policies on health inequalities in research participation
Policy decisions, such as NHS England’s Internet First [40] and Digital First Primary Care [41], are biassed towards those who are digitally enabled. However, older people, and those with disabilities, whose first language is not English, on lower incomes and living in rural areas are considered more likely to be digitally excluded [42]. These types of healthcare directives can lead to unintended consequences and risk worsening of health inequalities,
The following questions may guide those developing, reviewing and funding research that is inclusive of older people:
Engagement: Are representative older people, their family members, advocates and those with experience of working with older people involved in designing the research?
Inclusive study design: Has consideration been given to where the research takes place, how researchers interact with older people and family members and what happens during interactions to maximise the accessibility of research to older people and family members? This may involve piloting study procedures to ensure they are feasible and acceptable.
Resources: Have adequate infrastructure and financial resources been costed into funding applications to maximise participation, minimise withdrawals and ensure recruitment targets are met? There is a need to recognise that studies involving older people and family members may require additional resources, such as staff time and travel to conduct face-to-face recruitment and data collection at the person’s home.
Communication: Have a range of approaches to communicating with older people and family members about research been considered in terms of promoting the study, recruitment, data collection and dissemination.
Discussion
The exclusion of older people in research relevant to their health and care is not a new problem [43, 44]. The aim of our project was to develop best practice recommendations to promote the inclusion of older people in research. These were developed iteratively by identifying barriers and potential solutions in collaboration with a diverse group of stakeholders and from existing evidence. We identified 14 recommendations and four questions for researchers, reviewers and funders to consider: engagement; inclusive study design; adequate resources; communication.
Whilst there are many well established public and patient involvement and engagement (PPIE) groups they tend to be white, middle-class, have background in health or research [45], and are already research active. Older people are the most heterogeneous of any age group [46] with a broad range of intersectional characteristics. Gaining wider perspectives from e.g. communities and community groups would give greater insight into what is important to them and how to overcome some of the perceived barriers. It is a myth that older people and those with complex needs are too risky to include in research. They can and should contribute to identifying important research questions, priority setting, designing studies, participation in studies and disseminating findings [47, 48]. Troya and colleagues evaluated the impact of PPIE in the development of research on self-harm amongst older adults highlighting both the added value PPIE can bring alongside challenges such as support, training and ongoing communication that requires both time and resources [49].
Our findings align with those of the recently developed frameworks for promoting inclusion of people from ethnic minority groups [11, 12] and those with impaired capacity to consent [10, 22]. These frameworks consider four questions that should be asked by those developing RCTs: (i) who should trial apply to; (ii) are these groups likely to respond in different ways; (iii) will intervention make it harder for some to engage and (iv) will the study design make it harder for some to engage? There are some similarities to the key considerations we identified through the literature and stakeholders.
Whilst involving and engaging with older people living with complex needs can be logistically challenging efforts should be made to design research to be more inclusive. For example, a trial of home-based extended rehabilitation for older people living with frailty follow-up data collection is postal with the option for in-person data collection at the person’s home if needed [47]. Whilst having a more person-centred approach to recruitment, data collection and intervention delivery is clearly of benefit to the individual, this will come at a cost, both in staff time and resource [11, 50].
Communication about research needs to take place before, during and after a study. In the USA, the National Institute on Ageing has developed a toolkit and resources to encourage older people to take part in research addressing concerns and worries that older people may have [23]. Researchers need to identify a range of different communication strategies that incorporate people’s preferences, cultural and communication needs. The push towards supporting everyone to be digitally included [41] may create barriers and can threaten some peoples’ autonomy. We must ensure that those that don’t want to or are unable to engage are offered alternatives.
Strengths and limitations of our work
Whilst we conducted a rapid search for existing publications on the inclusion of older people in research, the search strategy may not have been fully comprehensive, and we may have missed relevant studies, which could have been addressed by having broader search terms and by searching the Applied Social Sciences Index and Abstracts database. This said, by integrating the perspectives of a range of key stakeholders involved in research including public representatives, health and care professionals, charity representatives, academics and those involved in reviewing, funding and delivering research, we were able to identify different barriers and solutions that were not apparent in the peer reviewed publications.
Implications for research and practice
Our recommendations are new and simple to understand and provide practical guidance on ways to improve the inclusion of older people in health and care research. We next need to consider how best to implement change, in particular amongst those who are not specialists in conducting research with older people e.g. through the co-development of resources and training, and evaluate its impact on improving inclusion of older people in health and care research.
Conclusion
We have identified a range of factors that impact on the inclusion of older people in research and made recommendations of how these can be addressed in the future to ensure research findings are relevant to them.
Supplementary Material
Acknowledgements
We would like to thank Lesley Gibson, Cath Harris, Jim Harris, Rebecca Maier, Pauline McGlone, Gary Nestor, David Scott, Elizabeth Webb and the NIHR CRN Ageing National Specialty Group for their contributions to this work. This work was supported by the NIHR CRN and the Southwest Peninsula Applied Research Collaboration. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Contributor Information
Victoria A Goodwin, Faculty of Health and Life Sciences, University of Exeter, Exeter, UK.
Mikaela S A Low, School of Medicine, Dentistry & Nursing, University of Glasgow, Glasgow, UK.
Terence J Quinn, School of Cardiovascular and Metabolic Health, University of Glasgow, Glasgow, UK.
Emma J Cockcroft, Faculty of Health and Life Sciences, University of Exeter, Exeter, UK.
Victoria Shepherd, Centre for Trials Research, Cardiff University, Cardiff, UK.
Philip H Evans, Faculty of Health and Life Sciences, University of Exeter, Exeter, UK; National Institute for Health and Care Research, Clinical Research Network, UK.
Emily J Henderson, Ageing and Movement Disorders Research Group, Bristol Medical School, University of Bristol, Bristol, UK.
Farhat Mahmood, Academic Unit for Ageing and Stroke Research, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK.
Mary Ni Lochlainn, National Institute for Health and Care Research, Clinical Research Network, UK; Department of Twin Research and Genetic Epidemiology, Kings College London, London, UK.
Catherine Needham, School for Social Policy, University of Birmingham, Birmingham, UK.
Benjamin R Underwood, Department of Psychiatry, University of Cambridge, Cambridge, UK.
Amit Arora, Elderly Care Department, University Hospitals of North Midlands NHS Trust, Stoke-on-Trent, UK.
Miles D Witham, AGE Research Group, NIHR Newcastle Biomedical Research Centre, Newcastle upon Tyne Hospitals NHS Foundation Trust, Cumbria Northumberland Tyne and Wear NHS Foundation Trust and Newcastle University, Newcastle, UK.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
None.
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.
References
- 1. National Institute for Health and Care Research , Improving Inclusion of under-Served Groups in Clinical Research: Guidance from INCLUDE Project. UK: NIHR, 2020: https://www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435.
- 2. Sheehan KJ, Fitzgerald L, Hatherley Set al. Inequity in rehabilitation interventions after hip fracture: a systematic review. Age Ageing 2019; 48: 489–97. [DOI] [PubMed] [Google Scholar]
- 3. Licchetta M and Stelmach M, Fiscal Sustainability and Public Spending on Health. UK: Office for Budget Responsibility, 2016. https://obr.uk/docs/dlm_uploads/Health-FSAP.pdf.
- 4. Carvalho do Nascimento PR, Ferreira ML, Poitras S, Bilodeau M. Exclusion of older adults from ongoing clinical trials on low back pain: a review of the WHO trial registry database. J Am Geriatr Soc 2019; 67: 603–8. [DOI] [PubMed] [Google Scholar]
- 5. Cruz-Jentoft AJ, Carpena-Ruiz M, Montero-Errasquín B, Sánchez-Castellano C, Sánchez-García E. Exclusion of older adults from ongoing clinical trials about type 2 diabetes mellitus. J Am Geriatr Soc 2013; 61: 734–8. [DOI] [PubMed] [Google Scholar]
- 6. Hamaker ME, Stauder R, Munster BC. Exclusion of older patients from ongoing clinical trials for hematological malignancies: an evaluation of the National Institutes of Health clinical trial registry. Oncologist 2014; 19: 1069–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lockett J, Sauma S, Radziszewska B, Bernard MA. Adequacy of inclusion of older adults in NIH-funded phase III clinical trials. J Am Geriatr Soc 2019; 67: 218–22. [DOI] [PubMed] [Google Scholar]
- 8. McMurdo ME, Roberts H, Parker Set al. Improving recruitment of older people to research through good practice. Age Ageing 2011; 40: 659–65. [DOI] [PubMed] [Google Scholar]
- 9. Richardson SJ, Carroll CB, Close Jet al. Research with older people in a world with COVID-19: identification of current and future priorities, challenges and opportunities. Age Ageing 2020; 49: 901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shepherd V, Hood K, Wood F. Unpacking the ‘black box of horrendousness’: a qualitative exploration of the barriers and facilitators to conducting trials involving adults lacking capacity to consent. Trials 2022; 23: 471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Treweek S, Banister K, Bower Pet al. Developing the INCLUDE ethnicity framework-a tool to help trialists design trials that better reflect the communities they serve. Trials 2021; 22: 337. 10.1186/s13063-021-05276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Trial Forge. The INCLUDE Ethnicity Framework, 2022. https://www.trialforge.org/trial-forge-centre/include/.
- 13. Witham MD, Anderson E, Carroll Cet al. Developing a roadmap to improve trial delivery for under-served groups: results from a UK multi-stakeholder process. Trials 2020; 21: 694. 10.1186/s13063-020-04613-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Green LW, Richard L, Potvin L. Ecological foundations of health promotion. Am J Health Promot 1996; 10: 270–81. [DOI] [PubMed] [Google Scholar]
- 15. Moreno-John G, Gachie A, Fleming CMet al. Ethnic minority older adults participating in clinical research. J Aging Health 2004; 16: 93S–123. [DOI] [PubMed] [Google Scholar]
- 16. Wells AA, Zebrack B. Psychosocial barriers contributing to the under-representation of racial/ethnic minorities in cancer clinical trials. Soc Work Health Care 2008; 46: 1–14. [DOI] [PubMed] [Google Scholar]
- 17. Salihu HM, Wilson RE, King LM, Marty PJ, Whiteman VE. Socio-ecological model as a framework for overcoming barriers and challenges in randomized control trials in minority and underserved communities. Int J MCH AIDS 2015; 3: 85–95. [PMC free article] [PubMed] [Google Scholar]
- 18. Taylor JS, DeMers SM, Vig EK, Borson S. The disappearing subject: exclusion of people with cognitive impairment and dementia from geriatrics research. J Am Geriatr Soc 2012; 60: 413–9. [DOI] [PubMed] [Google Scholar]
- 19. Shepherd V, Wood F, Griffith R, Sheehan M, Hood K. Protection by exclusion? The (lack of) inclusion of adults who lack capacity to consent to research in clinical trials in the UK. Trials 2019; 20: 474. 10.1186/s13063-019-3603-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Department of Health . The Mental Capacity Act. London: HMSO, 2005. [Google Scholar]
- 21. Shepherd, V. and Davies J., Conducting a Randomized Controlled Trial in Care Homes: The Challenges of Recruiting Residents Who Lack Capacity to Consent. 2020: London: SAGE Publications Ltd. 10.4135/9781529726626. [DOI] [Google Scholar]
- 22. Shepherd V. Capacity and Consent to Research, 2022. https://www.capacityconsentresearch.com/.
- 23. National Institute on Aging . Recruiting older adults into research (ROAR). Toolkit 2015; [cited 2022]. https://www.nia.nih.gov/health/recruiting-older-adults-research-roar-toolkit. [Google Scholar]
- 24. Davies K, Collerton JC, Jagger Cet al. Engaging the oldest old in research: lessons from the Newcastle 85+ study. BMC Geriatr 2010; 10: 64. 10.1186/1471-2318-10-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liljas AEM, Walters K, Jovicic Aet al. Strategies to improve engagement of 'hard to reach' older people in research on health promotion: a systematic review. BMC Public Health 2017; 17: 349. 10.1186/s12889-017-4241-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ridda I, MacIntyre CR, Lindley RI, Tan TC. Difficulties in recruiting older people in clinical trials: an examination of barriers and solutions. Vaccine 2010; 28: 901–6. [DOI] [PubMed] [Google Scholar]
- 27. Witham MD, McMurdo MET. How to get older people included in clinical studies. Drugs Aging 2007; 24: 187–96. [DOI] [PubMed] [Google Scholar]
- 28. Bonk J. A road map for the recruitment and retention of older adult participants for longitudinal studies. J Am Geriatr Soc 2010; 58: S303–7. [DOI] [PubMed] [Google Scholar]
- 29. McDougall GJ Jr, Simpson G, Friend ML. Strategies for research recruitment and retention of older adults of racial and ethnic minorities. J Gerontol Nurs 2015; 41: 14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dawson S, Banister K, Biggs Ket al. Trial Forge guidance 3: randomised trials and how to recruit and retain individuals from ethnic minority groups—practical guidance to support better practice. Trials 2022; 23: 672. 10.1186/s13063-022-06553-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Provencher V, Mortenson WB, Tanguay-Garneau L, Bélanger K, Dagenais M. Challenges and strategies pertaining to recruitment and retention of frail elderly in research studies: a systematic review. Arch Gerontol Geriatr 2014; 59: 18–24. [DOI] [PubMed] [Google Scholar]
- 32. Bowling CB, Whitson HE, Johnson TM 2nd. The 5Ts: preliminary development of a framework to support inclusion of older adults in research. J Am Geriatr Soc 2019; 67: 342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mody L, Miller DK, McGloin JMet al. Recruitment and retention of older adults in aging research. J Am Geriatr Soc 2008; 56: 2340–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fudge N, Wolfe CDA, McKevitt C. Involving older people in health research. Age Ageing 2007; 36: 492–500. [DOI] [PubMed] [Google Scholar]
- 35. National Institute for Health and Care Research and NIHR Strategic Framework for Multiple Long-Term Conditions (Multimorbidity) MLTC-M Research. UK: NIHR, 2020: https://www.nihr.ac.uk/documents/research-on-multiple-long-term-conditions-multimorbidity-mltc-m/24639.
- 36. National Institute for Health and Care Research , Equality, Diversity and Inclusion Strategy 2022–2027. UK: NIHR, 2022: https://www.nihr.ac.uk/documents/equality-diversity-and-inclusion-strategy-2022-2027/31295.
- 37. Nurock S. Patients may be less risk averse than committees. BMJ 2005; 330: 471–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Policy@Manchester , On Digital Inequalities: Analysis and Ideas on Addressing Digital Inequalities. 2021, Manchester: University of Manchester: https://policyatmanchester.shorthandstories.com/on-digital-inequalities/. [Google Scholar]
- 39. Government equalities office and equality and Humand rights commission, Equality Act 2010: https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05880-8. [Google Scholar]
- 40. Digital NHS. Internet First Policy, 2020. https://digital.nhs.uk/services/internet-first.
- 41. England NHS. Digital First Primary Care, 2019. https://digital.nhs.uk/about-nhs-digital/corporate-information-anddocuments/digital-inclusion.
- 42. Digital NHS. Digital Inclusion for Health and Social Care. In: 2022; 01/4/22].
- 43. Bartlett C, Doyal L, Ebrahim Set al. The causes and effects of socio-demographic exclusions from clinical trials. Health Technol Assess 2005; 9: iii-iv–x-x1-152. 10.3310/hta9380. [DOI] [PubMed] [Google Scholar]
- 44. Townsley CA, Selby R, Siu LL. Systematic review of barriers to the recruitment of older patients with cancer onto clinical trials. J Clin Oncol 2005; 23: 3112–24. [DOI] [PubMed] [Google Scholar]
- 45. Healthtalk . Patient and Public Involvement in Research. 2017; [11/3/22].https://healthtalk.org/patient-and-public-involvement-research/overview.
- 46. Dannefer D, Sell RR. Age structure, the life course and "aged heterogeneity": prospects for research and theory. Compr Gerontol B 1988; 2: 1–10. [PubMed] [Google Scholar]
- 47. Prescott M, Lilley-Kelly A, Cundill Bet al. Home-based extended rehabilitation for older people (HERO): study protocol for an individually randomised controlled multi-centre trial to determine the clinical and cost-effectiveness of a home-based exercise intervention for older people with frailty as extended rehabilitation following acute illness or injury, including embedded process evaluation. Trials 2021; 22: 783. 10.1186/s13063-021-05778-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Mulrow CD, Gerety MB, Kanten Det al. A randomized trial of physical rehabilitation for very frail nursing home residents. JAMA 1994; 271: 519–24. [PubMed] [Google Scholar]
- 49. Troya MI, Chew-Graham CA, Babatunde O, Bartlam B, Higginbottom A, Dikomitis L. Patient and public involvement and engagement in a doctoral research project exploring self-harm in older adults. Health Expect 2019; 22: 617–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McHenry JC, Insel KC, Einstein GO, Vidrine AN, Koerner KM, Morrow DG. Recruitment of older adults: success may be in the details. Gerontologist 2012; 55: 845–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.