Abstract
Many poxviruses are significant human and animal pathogens, including viruses that cause smallpox and mpox (formerly monkeypox). Identifying novel and potent antiviral compounds is critical to successful drug development targeting poxviruses. Here we tested two compounds, nucleoside trifluridine, and nucleotide adefovir dipivoxil, for antiviral activities against vaccinia virus (VACV), mpox virus (MPXV), and cowpox virus (CPXV) in physiologically relevant primary human fibroblasts. Both compounds potently inhibited the replication of VACV, CPXV, and MPXV (MA001 2022 isolate) in plaque assays. In our recently developed assay based on a recombinant VACV expressing secreted Gaussia luciferase, they both exhibited high potency in inhibiting VACV replication with EC50s in the low nanomolar range. In addition, both trifluridine and adefovir dipivoxil inhibited VACV DNA replication and downstream viral gene expression. Our results characterized trifluridine and adefovir dipivoxil as strong poxvirus antiviral compounds and further validate the VACV Gaussia luciferase assay as a highly efficient and reliable reporter tool for identifying poxvirus inhibitors. Given that both compounds are FDA-approved drugs, and trifluridine is already used to treat ocular vaccinia, further development of trifluridine and adefovir dipivoxil holds great promise in treating poxvirus infections, including mpox.
Keywords: Mpox (monkeypox) virus, Vaccinia virus, Cowpox virus, Adefovir dipivoxil, Trifluridine, Nucleos(t)ide, Antiviral, Gaussia luciferase reporter
1. Introduction
The family Poxviridae comprises 22 genera with 83 species based on the 2021 International Committee on Taxonomy of Viruses (ICTV) release. These viruses cause a broad range of human and animal diseases. The Orthopoxvirus genus contains 12 known species, including high-consequence human pathogens, such as variola virus that causes smallpox, and mpox (monkeypox) virus (MPXV). Historically, smallpox accounted for the most human deaths among all infectious diseases, claiming an estimated ∼300 million lives in the first 80 years of the 20th century alone. Despite its eradication in 1980 (Theves et al. 2016; WHO 2011), the potential re-emergence of smallpox from unsecured stocks or by a synthetic biology approach remains a major national security concern (Noyce et al. 2018; McCarthy 2014), particularly due to the rapid decline of population immunity after the cessation of smallpox vaccination. The loss of cross-protection by smallpox-induced immunity also increases the danger of other orthopoxvirus infections. Consequently, other orthopoxviruses may emerge to pose significant threats to public health (Yang et al. 2021). This is manifested in the ongoing global mpox outbreak, with over 87,000 reported cases in more than 110 countries (∼30,000 in the USA, from CDC, 2022 Outbreak Cases & Data, by May 09, 2023). The current mpox outbreak also underlines the pandemic potential of MPXV, of which future outbreaks are expected (Yang 2022; Rothenburg et al., 2022). The current outbreak is caused by MPXV clade II, a less severe/less transmissible clade than clade I that is endemic in central Africa (Likos et al., 2005). Other orthopoxviruses may also emerge to infect humans. For example, animals are believed to have transmitted a novel orthopoxvirus that infected four human individuals in Alaska in recent years (Department of Health and Social service, 2020, Department of Health and Social service, 2021; Springer et al., 2017). Such orthopoxviruses may evolve to adapt to human hosts over time and cause more serious concerns.
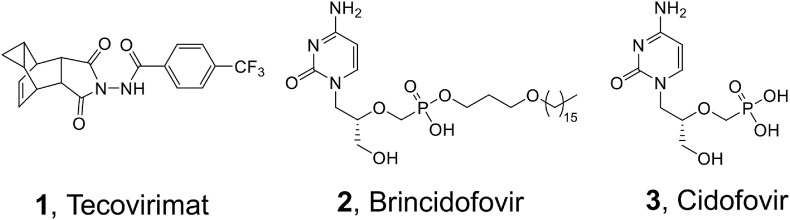
FDA has approved two drugs for strategic stockpiling against smallpox: tecovirimat (Yang et al., 2005b) (1, Fig. 1 ) and brincidofovir (Florescu and Keck 2014) (BCV, 2, Fig. 1), the lipid prodrug of nucleotide analog cidofovir (3, Fig. 1). However, the clinical efficacy of BCV against mpox is not promising (Carvalho 2022; Adler et al., 2022), and the clinical use of cidofovir for treating human cytomegalovirus is associated with severe adverse effects (Lea and Bryson 1996; Vandercam et al., 1999; Friedberg 1997) and drug resistance (Chou et al., 1997; Erice et al., 1997; Lurain and Chou 2010). Tecovirimat inhibits viral release by targeting the viral extracellular envelop protein VP37 (Grosenbach et al., 2018; Duraffour et al., 2015; Yang et al., 2005a). Although tecovirimat has shown promising efficacy in some mpox cases (Desai et al., 2022), clinical efficacy data are still very limited (O'Laughlin et al., 2022; Warner et al., 2022). Importantly, tecovirimat has a low barrier to viral resistance (FDA 2021; Yang et al., 2005a), and resistant mutants are expected after extensive use. In fact, resistance during the current mpox outbreak has been documented in severely immunocompromised patients who received prolonged administration of the drug (Alarcon et al., 2023). Therefore, it is critically important to develop new chemical entities against orthopoxviruses to provide valuable leads for rapid and effective countermeasures against re-emerging smallpox, mpox outbreaks, and other emerging orthopoxviruses. While many antiviral candidates against poxviruses have been identified in the past years (Wang et al., 2023; Siegrist and Sassine 2023), the majority of them have not been further characterized.
Fig. 1.
Structures of FDA-approved smallpox drugs. Tecovirimat (1) inhibits viral release by targeting the envelop protein VP37. Brincidofovir (2) is the prodrug of Cidofovir (3) which targets viral DNA polymerase.
Vaccinia virus (VACV) is the prototype poxvirus and is a closely related surrogate to study highly pathogenic poxviruses (e.g., mpox and variola viruses) due to their >95% genome identity (Hendrickson et al., 2010). We previously developed a VACV-Gaussia luciferase reporter assay and screened a library comprising FDA-approved antiviral drugs and Selleck bioactives (Peng et al., 2020). Of the many hits identified, we have further characterized the antiviral activities of two nucleos(t)ide analogs: trifluridine and adefovir dipivoxil. They significantly inhibited VACV, cowpox virus (CPXV), and MPXV replication in physiologically relevant primary human foreskin fibroblasts (HFFs) without discernible cytotoxicity. Mechanistically, they both target the DNA replication stage of viral infection. Our findings reveal two strong candidates suitable for further development as antivirals against orthopoxviruses.
2. Materials and methods
2.1. Viruses and cells
Primary Human Foreskin Fibroblasts (HFFs) were obtained from Dr. Nicholas Wallace at Kansas State University. HFFs and E6 cells (ATCC-CRL-1586) were cultured in Dulbecco's Minimal Essential Medium (DMEM; Fisher Scientific). BS-C-1 cells (ATCC-CCL26) were cultured in Eagle's Minimum Essential Medium (EMEM). The EMEM or DMEM was supplemented with 10% fetal bovine serum (FBS: VWR), L-glutamine (2 mM, VWR), streptomycin (100 μg/mL, VWR), and penicillin (100 units/mL, VWR). Cells were cultured in an incubator with 5% CO2 at 37 °C.
Vaccinia virus Western Reserve (WR, ATCC VR-1354) strain was propagated and purified by ultracentrifugation onto a sucrose cushion as described previously (Earl et al., 2001). MPXV-WA 2003–044 (Weiner et al., 2019), an MPXV-MA001 2022 isolate (GenBank: ON563414.3), CPXV (strain Brighton Red) were utilized in this study. Recombinant VACV expressing Gaussia luciferase under VACV early, intermediate, or late promoter vEGluc, vIGluc, and vLGluc were described previously (Pant et al. 2019). Preparation and infection of VACV and MPXV were carried out as described previously (Cotter et al., 2017; Hughes et al., 2017).
2.2. Titration of VACV, cowpox virus (CPXV) and MPXV by plaque assay
Titration of VACV, CPXV, and MPXV by plaque assay was carried out as described previously (Cotter et al., 2017). BS-C-1 (for VACV and CPXV) and E6 (for MPXV) cells were cultured in 6- or 12-well plates, infected with diluted virus samples, and incubated in culture medium (VACV and CPXV, EMEM, 2.5% FBS; MPXV, DMEM, 2% FBS) and 0.5–1% methylcellulose for 48 h–96 h. Cells were stained with 0.1% crystal violet for 15 min, followed by washing with water, and the number of plaques was counted. For MPXV, the staining solution contained >12% formalin.
2.3. Chemicals
Cytarabine (AraC) was purchased from Sigma-Aldrich. Brincidofovir (BCV), trifluridine, and adefovir dipivoxil were purchased from TargetMol.
2.4. Cell viability assay
Cell viability was measured by trypan blue staining or MTT assay. For the trypan blue staining assay, cells were cultured in the presence of DMSO or a specific compound at a desired concentration. Cells were then examined using trypan-blue exclusion as described elsewhere (Cao et al., 2017). The MTT [3-(4,5-dimethylthiazol-2-yl)-2,5 diphenyl tetrazolium bromide] assay was performed using an MTT assay kit (Cayman Chemical). Cells in 96-well plates were treated with DMSO or desired chemical inhibitors at different concentrations and incubated for the designated time. Ten μL of MTT reagent were added to each well and cells were incubated for 3 h. A 100 μL crystal resolving solution was added to each well and absorbance at 570 nm was measured using the citation 5 imaging reader (UV light) (Biotek) for each well after 18 h of incubation at 37 °C.
2.5. Determination of half maximal effective concentration (EC50)
HFFs were cultured in 96-well plates. The cells were infected with vLGluc at a multiplicity of infection (MOI) of 0.01 in the presence of DMSO or specific compound at a series of concentrations. Gluc activities were measured at 24 hpi. The EC50 was calculated using the following equation: log (inhibitor) vs. normalized response – variable slope in GraphPad Prism software (version 9.5.0).
2.6. Luciferase assay
Gaussia luciferase activities in culture medium were measured using a Pierce Gaussia Luciferase Flash Assay Kit (Thermo Scientific) using a GloMax Luminometer (Promega) according to the manufacturer's instructions.
Firefly luciferase activities for MPXV experiments were measured using an ENSPIRE plate reader (PerkinElmer, Waltham, MA) using the Luciferase Assay System (Promega, Madison, WI, United States) according to the manufacturer's instructions.
2.7. Quantitative real-time PCR
Total DNA was extracted using EZNA Blood DNA Kit. Relative viral DNA levels were quantified by CFX96 real-time PCR instrument (Bio-Rad, Hercules, CA) using All-in-oneTM 2 × qPCR mix (GeneCopoeia) with specific VACV primers against the C11 gene. 18 S rRNA gene primers were used as the internal reference.
2.8. Statistical analysis
All data were represented as the means of at least three independent experiments. Student's T-test was used to assess for significant difference between the two means with P ≤ 0.05.
3. Results
3.1. Trifluridine and adefovir dipivoxil potently inhibit VACV and CPXV replication in primary HFFs
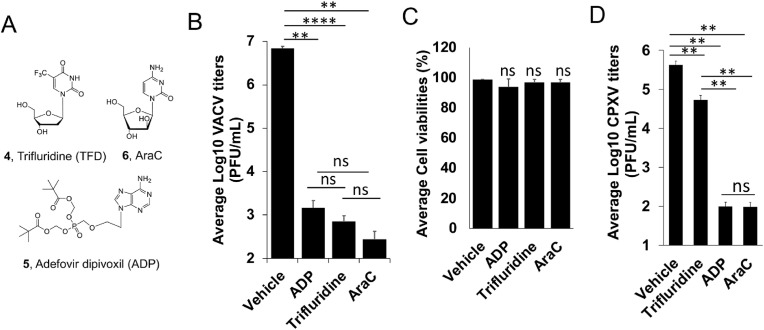
We have previously screened focused compound libraries for VACV inhibitors using a reporter VACV expressing Gaussia luciferase (Gluc) (vLGluc) in transformed HeLa cells, and have identified a number of strong hits (Peng et al., 2020), including several nucleos(t)ide analogs. To further confirm the antiviral effects of trifluridine (4, Fig. 2 A) and adefovir dipivoxil (5, Fig. 2A), we tested their effects on VACV replication in primary HFFs by plaque assay, the gold standard method of infectious viral yield measurement. It is worth noting that dermal fibroblasts are physiologically relevant to orthopoxvirus infection as they are among the major cell types in poxvirus infection and dissemination (Lum et al., 2022). Under a multiplicity of infection (MOI) of 0.01 and 48 h infection incubation time, trifluridine and adefovir dipivoxil strongly suppressed VACV yield by ∼9500- and 4500-fold, respectively, at 10 μM (Fig. 2B), without reducing the viability of HFFs (Fig. 2C). As a positive control, cytarabine (AraC, 6, Fig. 2A), a well-studied compound that blocks poxvirus genome replication, also strongly suppressed VACV replication in HFFs by 24,000-fold (Fig. 2B and C). Trifluridine and adefovir dipivoxil also significantly suppressed CPXV replication at 10 μM in HFFs (Fig. 2D).
Fig. 2.
Inhibition of VACV and CPXV replication by trifluridine and Adefovir dipivoxil (ADP) by plaque assay. (A) Structures of trifluridine (TFD, 4), adefovir dipivoxil (ADP, 5), and AraC (6). (B) HFFs were infected with VACV at an MOI of 0.01 and treated with indicated compounds at 10 μM for 48 h. Viral yields were titrated using a plaque assay using BS-C-1 cells. (C) HFF cell viability was measured 48 h after the cells were treated with indicated compounds at 10 μM. (D) HFFs were infected with CPXV at an MOI of 0.01 and treated with indicated compounds at 10 μM for 48 h. Viral yields were titrated using a plaque assay using BS-C-1 cells. The plotted values represent the means of at least three repeats. Error bars represent standard deviation. **0.001<p ≤ 0.01; ****0.00001<p ≤ 0.0001; ns, not significant.
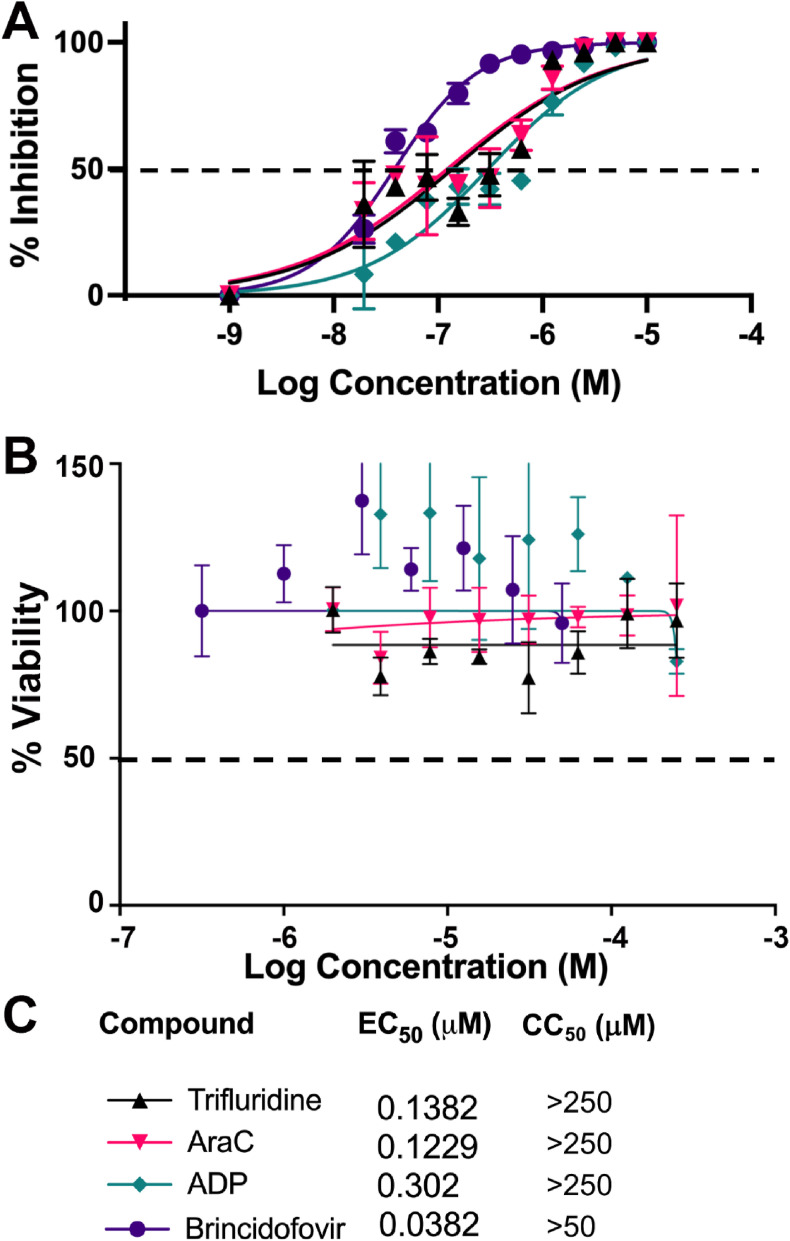
We next determined the half-maximal effective concentration (EC50) of trifluridine and adefovir dipivoxil in inhibiting VACV replication in HFFs using the vLGluc. The vLGluc is a recombinant VACV expressing Gluc under a viral late promoter used in our initial screening of VACV inhibitors (Peng et al., 2020; Pant et al. 2019). We first evaluated if this assay is suitable for measuring VACV inhibitor's EC50 using BCV (Chan-Tack et al., 2021). With an MOI of 0.01 and 24 h infection incubation time, the EC50 of BCV was determined to be ∼38 nM in HFFs (Fig. 3 A and C), which is similar to reported values (Lanier et al., 2010; JW Huggins et al., 2002), suggesting that vLGluc is suitable for EC50 measurement. Using the same MOI and incubation time, we determined the EC50s of trifluridine (EC50 = 138 nM) and adefovir dipivoxil (EC50 = 302 nM) (Fig. 3A and C). The EC50 of AraC was also determined (EC50 = 123 nM) (Fig. 3A). Remarkably, both trifluridine and adefovir dipivoxil, as well as the positive control compounds BCV and AraC, caused no significant cytotoxicity in HFFs at high concentrations (CC50 > 250 μM for trifluridine, AraC, and adefovir dipivoxil, CC50 > 50 μM for BCV) as measured in an MTT assay (Fig. 3B and C).
Fig. 3.
Measurement of EC50 and CC50 of indicated compounds in HFFs. (A) HFFs were infected with vLGluc at an MOI of 0.01 and treated with indicated individual compounds at a series of concentrations (or vehicle DMSO) for 24 h. Gluc activities were measured to determine the EC50. (B) HFFs cell viability was determined by an MTT assay after incubation with indicated compounds at a series of concentrations for 24 h. (C) EC50 and CC50 of the compounds in A and B are shown. The plotted values represent the means of at least three repeats. Error bars represent standard deviation.
Together, the above results established that trifluridine and adefovir dipivoxil inhibit VACV with EC50s at low nM and low cytotoxic effects in HFFs. Our results also further validated the Gluc expressing reporter VACV (vLGluc) as a valuable tool in poxvirus inhibitor identification and characterization.
3.2. Trifluridine and adefovir dipivoxil inhibit VACV genome replication
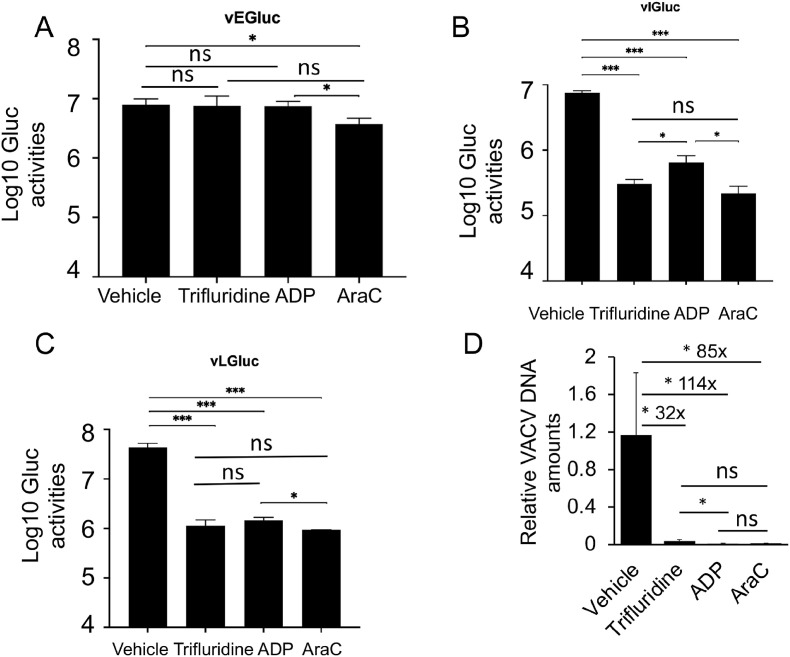
Poxvirus replication is divided into the following steps: entry, early gene expression, uncoating, DNA replication, intermediate gene expression, late gene expression, and post-gene expression events such as viral morphogenesis, assembly, and spreading (Moss, 2013). Nucleos(t)ide analogs, e.g., trifluridine and adefovir dipivoxil, presumably inhibit VACV replication at the DNA replication stage. Subsequently, the post-DNA replication gene expression should also be affected due to the excessive need for RNA synthesis. To test this hypothesis, we first used recombinant VACVs with stage-specific Gluc reporter genes. In addition to the VACV encoding Gluc under the late F17R promoter (vLGluc), two other recombinant VACVs were also used: in one, the Gluc gene is under the control of the VACV early C11R (vEGluc) promoter, and in the other, it is under the control of the G8R intermediate (vIGluc) promoter (Pant et al. 2019). The C11R, G8R, and F17R genes are well-characterized, exclusively early, intermediate, and late VACV genes, respectively, and their promoters can be used to effectively distinguish stages of VACV gene expression (Yang et al. 2010, 2011). Neither trifluridine nor adefovir dipivoxil affected the Gluc expression under the VACV early C11R promoter (Fig. 4 A), while they both strongly inhibited Gluc expression under intermediate G8R and late F17R promoters (Fig. 4B and C). The trends were similar to the AraC treatment (Fig. 4A–C).
Fig. 4.
Trifluridine and adefovir dipivoxil (ADP) suppress VACV DNA replication and post-replicative gene expression but not early gene expression. (A–C) HFFs were infected with vEGluc (A), vIGluc (B), and vLGluc (C) at an MOI of 2 and treated with indicated compounds at 10 μM, respectively, or vehicle DMSO. Gluc activities were measured at 4 h (vEGluc), 8 h (vIGluc), and 8 h (vLGluc), respectively. (D) HFFs were infected with VACV at an MOI of 2 in the presence of Indicated compounds at 10 μM for 8 h. Relative amounts of Viral DNA were determined by real-time PCR using VACV-specific primers. The plotted values represent the means of at least three repeats. Error bars represent standard deviation. *0.01<p ≤ 0.05; ***0.0001<p ≤ 0.001; ns, not significant. DMSO was used as the vehicle for the compounds.
As poxvirus intermediate and late gene expression depend on viral genomic DNA replication, we examined VACV DNA levels in the presence or absence of individual compounds. We found that trifluridine, adefovir dipivoxil, and the positive control AraC strongly reduced viral DNA levels by 32- to 114-fold (Fig. 4D), respectively. Together, these results confirmed that trifluridine and adefovir dipivoxil function to restrict VACV DNA synthesis.
3.3. Trifluridine and adefovir dipivoxil significantly inhibit MPXV replication in primary HFFs
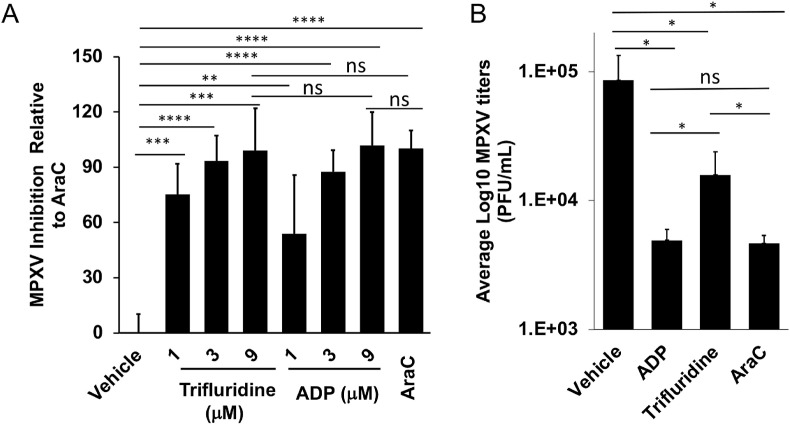
We used two methods to examine the effects of trifluridine and adefovir dipivoxil on MPXV replication. In one method, we used a WA strain MPXV-USA-2003-044 expressing firefly luciferase (Fluc) under a viral early/late promoter (luc + MPXV) gene as the reporter. We observed that trifluridine and adefovir dipivoxil strongly inhibited MPXV replication with similar potency to AraC (Fig. 5 A). We also tested the inhibitory effects on an MPXV-MA001 2022 isolate by plaque assay and found that both trifluridine and adefovir dipivoxil significantly suppressed MPXV replication (Fig. 5B).
Fig. 5.
Inhibition of MPXV replication by trifluridine and Adefovir dipivoxil (ADP). (A) HFFs were infected with MPXV-WA-2003-Fluc (luc + MPXV) under an early/late promoter (MOI = 0.01) and treated with indicated compounds at the indicated concentration for 24 h. Firefly luciferase activities were measured. The inhibition by AraC was normalized to 100. (B) MPXV-MA001 2022 isolate was added to cells at an MOI of 2 for 1 h. The virus was removed, cells were washed with PBS, and trifluridine or adefovir dipivoxil was added at 10 μM. Cells were harvested 24 h post-infection. AraC treatment was used as the positive control. Viral yields were titrated using a plaque assay on E6 cells. The plotted values represent the means of at least three repeats. Error bars represent standard deviation. *p ≤ 0.05; **0.001<p ≤ 0.01; ***0.0001<p ≤ 0.001; ****0.00001<p ≤ 0.0001; ns, not significant. DMSO was used as the vehicle for the compounds.
4. Discussion
Nucleos(t)ide analogs represent a main class of antiviral drugs (De Clercq and Li 2016; Jordheim et al., 2013), as exemplified by various herpesvirus inhibitors (Sadowski et al., 2021), a large panel of nucleos(t)ide reverse transcriptase inhibitors against HIV (Holec et al., 2017), hepatitis B virus (HBV) (Tavakolpour et al., 2018), hepatitis C virus (HCV) inhibitors (Sofia et al., 2017), and recently, SARS-CoV-2 (Beigel et al., 2020; Yu and Chang 2022; Xie et al., 2021; Zhang et al., 2021). Mechanistically, most nucleoside analogs act as chain terminators. Per this mechanism, the analogs are intracellularly converted to the active triphosphate (TP) form via monophosphate (MP) and diphosphate (DP) intermediates by the host or virally-encoded kinases. The TPs then compete against endogenous nucleoside triphosphates (NTPs) for incorporation by the viral polymerase. Once incorporated, these analogs act as chain terminators to stall viral genome replication. In cases where the intracellular conversion into MP, which is typically the rate-limiting step of nucleoside drug bioactivation, is inefficient, the MP is chemically installed to bypass kinase functions, constituting a mechanistically distinct nucleotide drug family. The FDA-approved smallpox drug BCV is a prodrug of the nucleotide drug cidofovir, which belongs to the acyclic nucleoside phosphonate (ANP) (De Clercq and Holy 2005) sub-class. Important antiviral drugs of this sub-class also include the reverse transcriptase inhibitors tenofovir (Naesens et al., 1998; Lyseng-Williamson et al. 2005), for treating HIV and HBV, and adefovir (Naesens et al., 1997; Dando and Plosker 2003), an HBV drug, typically administered in an ester prodrug form to overcome the low cell permeability. The two drugs characterized in this study, trifluridine, and adefovir dipivoxil, represent these two pharmacologically distinct classes of nucleos(t)ide drugs.
As an antiviral drug, trifluridine has long been approved for topically treating herpes simplex virus (HSV) infection of the eyes (keratoconjunctivitis) (Carmine et al., 1982). Interestingly, trifluridine has also been used to treat eye infections of VACV in humans and has been tested in rabbits for VACV keratitis (Parkhurst et al. 1976; Altmann et al., 2011), and mpox during the 2022 outbreak (Perzia et al., 2023). In addition, trifluridine is approved as a systemic drug to treat colorectal and gastric cancers. However, since trifluridine is highly labile toward degradation by thymidine phosphorylase (TP), it is used along with a TP inhibitor tipiracil in a combination setting for systemic cancer treatment (Burness and Duggan 2016). We report here its low nM potency inhibiting VACV infection in HFFs, and strong antiviral effect on MPXV replication.
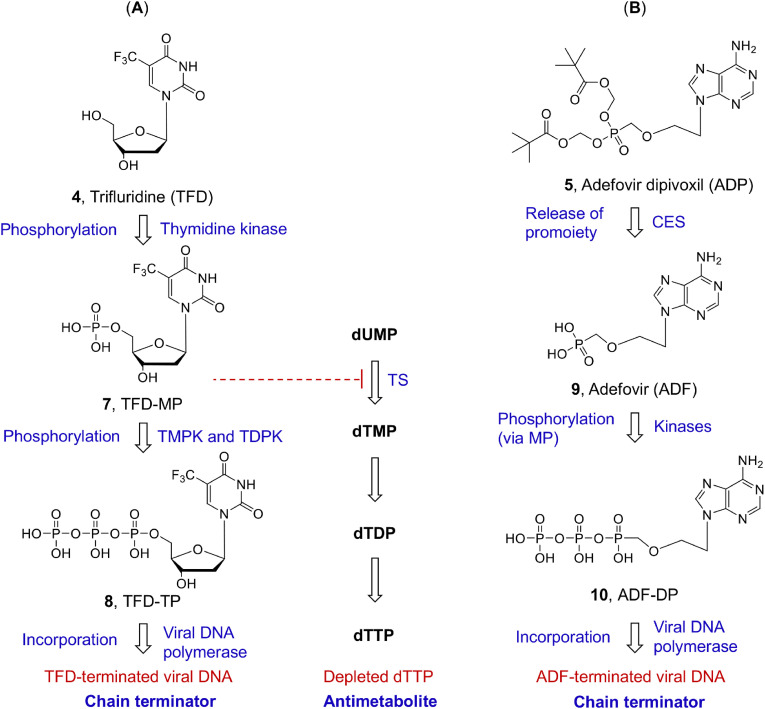
Mechanistically, trifluridine can act as a chain terminator or antimetabolite (Fig. 6 A), both requiring the intracellular conversion to trifluridine-MP (TFD-TP) (7, Fig. 6A) by thymidine kinase (TK). Under the chain termination mechanism, TFD-MP is further phosphorylated to TFD-TP (8, Fig. 6A) by thymidine monophosphate kinase (TMPK) and thymidine diphosphate kinase (TDPK). As a thymidine analog, TP (8, Fig. 6A) competes against the endogenous dTTP for incorporation by the viral DNA polymerase, leading to the termination of viral DNA. It is noteworthy that orthopoxviruses encode both TK and TMPK required for phosphorylating synthetic nucleoside analogs (Paoletti and Moss 1972; Kit et al. 1963; Moss, 2013), with substrate specificity partially overlapping with that of cellular kinases (Topalis et al., 2005; Caillat et al., 2008). Multiple lines of evidence suggest that in orthopoxvirus-infected cells, C5-modified nucleosides, trifluridine included, are likely phosphorylated by the viral kinases (Prichard et al., 2007). In cancer cells, trifluridine likely inhibits DNA synthesis via dual mechanisms (Fig. 6A): as a chain terminator; and as a dTTP antimetabolite in the form of TFD-MP (Temmink et al., 2007). Cellular dTTP anabolism critically entails the function of thymidylate synthase (TS), which converts dUMP to dTMP (Fig. 6A). TFD-MP inhibits thymidylate synthase and ultimately leads to the depletion of the cellular dTTP pool.
Fig. 6.
Mechanisms of action of nucleoside analog trifluridine (TFD, 4) and nucleotide analog prodrug adefovir dipivoxil (ADP, 5). (A) TFD is intracellularly converted into TFD-MP by cellular or viral thymidine kinase, followed by two additional phosphorylation steps to yield TFD-TP. The incorporation of TFD-TP by viral DNA polymerase terminates viral DNA (chain terminator). Alternatively, TFD-MP inhibits thymidylate synthase (TS) to stall the conversion of dUMP to dTMP, ultimately depleting the cellular dTTP pool (antimetabolite); (B) Ester prodrug ADP is intracellularly converted into adefovir first under the action of carboxylesterase (CES). The subsequent successive phosphorylation produces the active ADF-DP. When incorporated, ADF-DP terminates the viral DNA (chain terminator).
The other drug studied herein, adefovir dipivoxil (Dando and Plosker 2003), is a prodrug of ANP adefovir for HBV treatment. Upon cellular uptake, adefovir dipivoxil is cleaved by a cellular carboxylesterase (CES) to release the ester promoiety and generate Adefovir (9, Fig. 6B). This is followed by two successive phosphorylation by AMP kinase to produce the active adefovir-DP (Naesens et al., 1997) (10, Fig. 6B). By competing against cellular dATP, adefovir-DP is incorporated by the viral DNA polymerase, and subsequently causes an obligate chain termination. While adefovir dipivoxil was a hit from previous antiviral screening against poxviruses (Peng et al., 2020; Kern 2003), it has not been used to treat poxvirus infection in humans.
Against VACV and MPXV replication in HFFs, both trifluridine and adefovir dipivoxil showed potent inhibition of VACV with EC50s in the nM range without discernible cytotoxicity (CC50 > 250 μM). Interestingly, it has been reported that trifluridine is quite toxic when given systemically due to its effect on cellular DNA synthesis (Lee and Chu 2017). The lack of cytotoxicity in cultured HFFs observed suggests that further characterizations with additional cell lines and possibly in vivo testing are needed to better understand the toxic effects of the compound. Nonetheless, these results validate both drugs as viable candidates for further investigation as potential anti-MPXV and other orthopoxvirus drugs. The successful repurposing of adefovir dipivoxil will add to the already approved BCV to further enhance ANP prodrugs as an important drug class for treating poxvirus infections. In addition, nucleoside analog trifluridine as a poxvirus drug candidate will introduce a mechanistically distinct drug class and expand the options for synergistic combination therapies with ANPs or tecovirimat.
In this study, we also validated the utility of the Gluc expression VACV under a late promoter F17R (vLGluc) by measuring Gluc activities in the media to determine EC50 of compounds in poxvirus drug research. Because Gluc is secreted into the medium (Tannous and Teng 2011), this assay is a rapid, non-disruptive, and highly simplified VACV replication reporter with an exceptionally high Signal-to-Basal ratio (Peng et al., 2020). This reporter VACV is suitable for high-throughput screening, as shown in our previous study (Peng et al., 2020), which will facilitate our future antiviral research against poxviruses.
5. Conclusion
In summary, we characterized the antiviral profiles of nucleoside analog trifluridine and acyclic nucleoside phosphonate adefovir dipivoxil against VACV, CPXV, and MPXV in primary fibroblasts. Further testing in animal models will determine their in vivo anti-MPXV and other orthopoxvirus potential. Chemical modification of the compounds may also improve their potency, pharmacokinetic (PK), and safety profiles.
Funding sources
ZY was supported in part by grants from the National Institutes of Health (R01AI143709).
PSS is supported in part by grants from the Biomedical Advanced Research and Development Authority, and the Center for Disease Control and Prevention intramural research funding.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the funding agencies.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We thank Nicholas Wallace (Kansas State University) for providing HFFs. We thank Bernard Moss for providing VACV.
Glossary
- VACV
vaccinia virus
- MPXV
mpox (monkeypox) virus
- CPXV
cowpox virus
- HBV
hepatitis B virus
- HCV
hepatitis C virus
- AraC
cytarabine
- BCV
brincidofovir
- ADP
adefovir dipivoxil
- ADF
adefovir
- TFD
trifluridine
- TMPK
thymidine monophosphate kinase
- TDPK
thymidine diphosphate kinase
- TK
thymidine kinase
- ANP
acyclic nucleoside phosphonate
- NTP
nucleoside triphosphate
- Gluc
Gaussia luciferase
- EC50
half maximal effective concentration
- CC50
50% cytotoxic concentration
Data availability
Data will be made available on request.
References
- Adler H., Gould S., Hine P., Snell L.B., Wong W., Houlihan C.F., Osborne J.C., Rampling T., Beadsworth M.B., Duncan C.J., Dunning J., Fletcher T.E., Hunter E.R., Jacobs M., Khoo S.H., Newsholme W., Porter D., Porter R.J., Ratcliffe L., Schmid M.L., Semple M.G., Tunbridge A.J., Wingfield T., Price N.M., England High Consequence Infectious Diseases Network N.H.S. 'Clinical features and management of human monkeypox: a retrospective observational study in the UK'. Lancet Infect. Dis. 2022;22:1153–1162. doi: 10.1016/S1473-3099(22)00228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alarcon J., Kim M., Terashita D., Davar K., Garrigues J.M., Guccione J.P., Evans M.G., Hemarajata P., Wald-Dickler N., Holtom P., Garcia Tome R., Anyanwu L., Shah N.K., Miller M., Smith T., Matheny A., Davidson W., Hutson C.L., Lucas J., Ukpo O.C., Green N.M., Balter S.E. An mpox-related death in the United States. N. Engl. J. Med. 2023;388:1246–1247. doi: 10.1056/NEJMc2214921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altmann S., Brandt C.R., Murphy C.J., Patnaikuni R., Takla T., Toomey M., Nesbit B., McIntyre K., Covert J., Dubielzig R., Leatherberry G., Adkins E., Kodihalli S. 'Evaluation of therapeutic interventions for vaccinia virus keratitis'. J. Infect. Dis. 2011;203:683–690. doi: 10.1093/infdis/jiq103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beigel J.H., Tomashek K.M., Dodd L.E., Mehta A.K., Zingman B.S., Kalil A.C., Hohmann E., Chu H.Y., Luetkemeyer A., Kline S., Lopez de Castilla D., Finberg R.W., Dierberg K., Tapson V., Hsieh L., Patterson T.F., Paredes R., Sweeney D.A., Short W.R., Touloumi G., Lye D.C., Ohmagari N., Oh M.D., Ruiz-Palacios G.M., Benfield T., Fatkenheuer G., Kortepeter M.G., Atmar R.L., Creech C.B., Lundgren J., Babiker A.G., Pett S., Neaton J.D., Burgess T.H., Bonnett T., Green M., Makowski M., Osinusi A., Nayak S., Lane H.C., Actt- Study Group Members 'Remdesivir for the treatment of covid-19 - final report'. N. Engl. J. Med. 2020;383:1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burness Celeste B., Duggan Sean T. 'Trifluridine/Tipiracil: a review in metastatic colorectal cancer'. Drugs. 2016;76:1393–1402. doi: 10.1007/s40265-016-0633-9. [DOI] [PubMed] [Google Scholar]
- Caillat C., Topalis D., Agrofoglio L.A., Pochet S., Balzarini J., Deville-Bonne D., Meyer P. 'Crystal structure of poxvirus thymidylate kinase: an unexpected dimerization has implications for antiviral therapy'. Proc. Natl. Acad. Sci. U. S. A. 2008;105:16900–16905. doi: 10.1073/pnas.0804525105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao S., Realegeno S., Pant A., Satheshkumar P.S., Yang Z. 'Suppression of poxvirus replication by resveratrol'. Front. Microbiol. 2017;8:2196. doi: 10.3389/fmicb.2017.02196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmine A.A., Brogden R.N., Heel R.C., Speight T.M., Avery G.S. 'Trifluridine: a review of its antiviral activity and therapeutic use in the topical treatment of viral eye infections'. Drugs. 1982;23:329–353. doi: 10.2165/00003495-198223050-00001. [DOI] [PubMed] [Google Scholar]
- Carvalho T. 'The unknown efficacy of tecovirimat against monkeypox'. Nat. Med. 2022;28:2224–2225. doi: 10.1038/d41591-022-00094-0. [DOI] [PubMed] [Google Scholar]
- Chan-Tack K., Harrington P., Bensman T., Choi S.Y., Donaldson E., O'Rear J., McMillan D., Myers L., Seaton M., Ghantous H., Cao Y., Valappil T., Birnkrant D., Struble K. 'Benefit-risk assessment for brincidofovir for the treatment of smallpox: U.S. Food and Drug Administration's Evaluation'. Antivir. Res. 2021;195 doi: 10.1016/j.antiviral.2021.105182. [DOI] [PubMed] [Google Scholar]
- Chou S., Marousek G., Guentzel S., Follansbee S.E., Poscher M.E., Lalezari J.P., Miner R.C., Drew W.L. 'Evolution of mutations conferring multidrug resistance during prophylaxis and therapy for cytomegalovirus disease'. J. Infect. Dis. 1997;176:786–789. doi: 10.1086/517302. [DOI] [PubMed] [Google Scholar]
- Cotter C.A., Earl P.L., Wyatt L.S., Moss B. Preparation of cell cultures and vaccinia virus stocks. Curr Protoc Protein Sci. 2017;89 doi: 10.1002/cpps.34. 5 12 1-5 12 18. [DOI] [PubMed] [Google Scholar]
- Dando Toni M., Plosker Greg L. 'Adefovir dipivoxil'. Drugs. 2003;63:2215–2234. doi: 10.2165/00003495-200363200-00007. [DOI] [PubMed] [Google Scholar]
- De Clercq E., Holy A. 'Acyclic nucleoside phosphonates: a key class of antiviral drugs'. Nat. Rev. Drug Discov. 2005;4:928–940. doi: 10.1038/nrd1877. [DOI] [PubMed] [Google Scholar]
- De Clercq E., Li G. 'Approved antiviral drugs over the past 50 Years'. Clin. Microbiol. Rev. 2016;29:695–747. doi: 10.1128/CMR.00102-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Social service . Second Case of Novel Orthopoxvirus Infection in a Fairbanks-area Resident. State of Alaska Epidemiology Bulletin; 2020. [Google Scholar]
- Department of Health and Social service . Additional Cases of Orthopoxvirus Infection in Fairbanks-area Residents. State of Alaska Epidemiology Bulletin; 2021. [Google Scholar]
- Desai A.N., Thompson G.R., 3rd, Neumeister S.M., Arutyunova A.M., Trigg K., Cohen S.H. 'Compassionate use of tecovirimat for the treatment of monkeypox infection'. JAMA. 2022;328:1348–1350. doi: 10.1001/jama.2022.15336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duraffour S., Lorenzo M.M., Zöller G., Topalis D., Grosenbach D., Hruby D.E., Andrei G., Blasco R., Meyer H., Snoeck R. 'ST-246 is a key antiviral to inhibit the viral F13L phospholipase, one of the essential proteins for orthopoxvirus wrapping'. J. Antimicrob. Chemother. 2015;70:1367–1380. doi: 10.1093/jac/dku545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earl P.L., Cooper N., Wyatt L.S., Moss B., Carroll M.W. 'Preparation of cell cultures and vaccinia virus stocks'. Curr. Protoc. Mol. Biol. 2001 doi: 10.1002/0471142727.mb1616s43. (Chapter 16): Unit16 16. [DOI] [PubMed] [Google Scholar]
- Erice A., Gil-Roda C., Pérez J.L., Balfour H.H., Jr., Sannerud K.J., Hanson M.N., Boivin G., Chou S. 'Antiviral susceptibilities and analysis of UL97 and DNA polymerase sequences of clinical cytomegalovirus isolates from immunocompromised patients'. J. Infect. Dis. 1997;175:1087–1092. doi: 10.1086/516446. [DOI] [PubMed] [Google Scholar]
- FDA . 2021. TPOXX (Tecovirimat) Capsules for Oral Use. [Google Scholar]
- Florescu Diana F., Keck Megan A. 'Development of CMX001 (Brincidofovir) for the treatment of serious diseases or conditions caused by dsDNA viruses'. Expert Rev. Anti-infect. Ther. 2014;12:1171–1178. doi: 10.1586/14787210.2014.948847. [DOI] [PubMed] [Google Scholar]
- Friedberg D.N. 'Hypotony and visual loss with intravenous cidofovir treatment of cytomegalovirus retinitis'. Arch. Ophthalmol. 1997;115:801–802. doi: 10.1001/archopht.1997.01100150803021. [DOI] [PubMed] [Google Scholar]
- Grosenbach D.W., Honeychurch K., Rose E.A., Chinsangaram J., Frimm A., Maiti B., Lovejoy C., Meara I., Long P., Hruby D.E. 'Oral tecovirimat for the treatment of smallpox'. N. Engl. J. Med. 2018;379:44–53. doi: 10.1056/NEJMoa1705688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrickson R.C., Wang C., Hatcher E.L., Lefkowitz E.J. 'Orthopoxvirus genome evolution: the role of gene loss'. Viruses. 2010;2:1933–1967. doi: 10.3390/v2091933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holec A.D., Mandal S., Prathipati P.K., Destache C.J. 'Nucleotide reverse transcriptase inhibitors: a thorough review, present status and future perspective as HIV therapeutics'. Curr. HIV Res. 2017;15:411–421. doi: 10.2174/1570162X15666171120110145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huggins J.W., Baker R.O., Beadle J.R., Hostetler K.Y. 'Orally active ether lipid prodrugs of cidofovir for the treatment of smallpox'. Antivir. Res. 2002;53 [Google Scholar]
- Hughes L., Wilkins K., Goldsmith C.S., Smith S., Hudson P., Patel N., Karem K., Damon I., Li Y., Olson V.A., Satheshkumar P.S. 'A rapid Orthopoxvirus purification protocol suitable for high-containment laboratories'. J. Virol. Methods. 2017;243:68–73. doi: 10.1016/j.jviromet.2017.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordheim L.P., Durantel D., Zoulim F., Dumontet C. Advances in the development of nucleoside and nucleotide analogues for cancer and viral diseases. Nat. Rev. Drug Discov. 2013;12:447–464. doi: 10.1038/nrd4010. [DOI] [PubMed] [Google Scholar]
- Kern E.R. In vitro activity of potential anti-poxvirus agents. Antivir. Res. 2003;57:35–40. doi: 10.1016/S0166-3542(02)00198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kit S., Piekarski L.J., Dubbs D.R. 'Induction of thymidine kinase by vaccinia-infected mouse fibroblasts'. J. Mol. Biol. 1963;6:22–33. doi: 10.1016/s0022-2836(63)80078-9. [DOI] [PubMed] [Google Scholar]
- Lanier R., Trost L., Tippin T., Lampert B., Robertson A., Foster S., Rose M., Painter W., O'Mahony R., Almond M., Painter G. 'Development of CMX001 for the treatment of poxvirus infections'. Viruses. 2010;2:2740–2762. doi: 10.3390/v2122740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lea A.P., Bryson H.M. 'Cidofovir'. Drugs. 1996;52:225–230. doi: 10.2165/00003495-199652020-00006. discussion 31. [DOI] [PubMed] [Google Scholar]
- Lee J.J., Chu E. 'Adherence, dosing, and managing toxicities with trifluridine/tipiracil (TAS-102)'. Clin. Colorectal Cancer. 2017;16:85–92. doi: 10.1016/j.clcc.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Likos A.M., Sammons S.A., Olson V.A., Frace A.M., Li Y., Olsen-Rasmussen M., Davidson W., Galloway R., Khristova M.L., Reynolds M.G., Zhao H., Carroll D.S., Curns A., Formenty P., Esposito J.J., Regnery R.L., Damon I.K. A tale of two clades: monkeypox viruses. J. Gen. Virol. 2005;86:2661–2672. doi: 10.1099/vir.0.81215-0. [DOI] [PubMed] [Google Scholar]
- Lum F.M., Torres-Ruesta A., Tay M.Z., Lin R.T.P., Lye D.C., Renia L., Ng L.F.P. 'Monkeypox: disease epidemiology, host immunity and clinical interventions'. Nat. Rev. Immunol. 2022;22:597–613. doi: 10.1038/s41577-022-00775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurain N.S., Chou S. 'Antiviral drug resistance of human cytomegalovirus'. Clin. Microbiol. Rev. 2010;23:689–712. doi: 10.1128/CMR.00009-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyseng-Williamson, Katherine A., Reynolds Neil A., Plosker Greg L. Tenofovir disoproxil fumarate. Drugs. 2005;65:413–432. doi: 10.2165/00003495-200565030-00006. [DOI] [PubMed] [Google Scholar]
- McCarthy M. 'Smallpox samples are found in FDA storage room in Maryland'. BMJ. 2014;349:g4545. doi: 10.1136/bmj.g4545. [DOI] [PubMed] [Google Scholar]
- Moss B. In: Howley PM Knipe D.M., editor. Vol. 2. 2013. Poxviridae: the Viruses and Their Replication; pp. 2129–2159. (Fields Virology). [Google Scholar]
- Naesens L., Snoeck R., Andrei G., Balzarini J., Neyts J., De Clercq E. 'HPMPC (cidofovir), pmea (adefovir) and related acyclic nucleoside phosphonate analogues: a review of their pharmacology and clinical potential in the treatment of viral infections'. Antivir. Chem. Chemother. 1997;8:1–23. [Google Scholar]
- Naesens L., Bischofberger N., Augustijns P., Annaert P., Van den Mooter G., Arimilli M.N., Kim C.U., De Clercq E. 'Antiretroviral efficacy and pharmacokinetics of oral bis(isopropyloxycarbonyloxymethyl)-9-(2-phosphonylmethoxypropyl)adenine in mice'. Antimicrob. Agents Chemother. 1998;42:1568–1573. doi: 10.1128/aac.42.7.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noyce R.S., Lederman S., Evans D.H. Construction of an infectious horsepox virus vaccine from chemically synthesized DNA fragments. PLoS One. 2018;13 doi: 10.1371/journal.pone.0188453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Laughlin K., Tobolowsky F.A., Elmor R., Overton R., O'Connor S.M., Damon I.K., Petersen B.W., Rao A.K., Chatham-Stephens K., Yu P., Yu Y., Monkeypox Tecovirimat Data Abstraction Team C.D.C. 'Clinical use of tecovirimat (tpoxx) for treatment of monkeypox under an investigational new drug protocol - United States, may-august 2022'. MMWR Morb. Mortal. Wkly. Rep. 2022;71:1190–1195. doi: 10.15585/mmwr.mm7137e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant A., Cao S., Yang Z. 'Asparagine is a critical limiting metabolite for vaccinia virus protein synthesis during glutamine deprivation'. J. Virol. 2019;93 doi: 10.1128/JVI.01834-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paoletti E., Moss B. 'Protein kinase and specific phosphate acceptor proteins associated with vaccinia virus cores'. J. Virol. 1972;10:417–424. doi: 10.1128/jvi.10.3.417-424.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkhurst J.R., Danenberg P.V., Heidelberger C. 'Growth inhibition of cells in cultures and of vaccinia virus infected HeLa cells by derivatives of trifluorothymidine'. Chemotherapy. 1976;22:221–231. doi: 10.1159/000221929. [DOI] [PubMed] [Google Scholar]
- Peng C., Zhou Y., Cao S., Pant A., Campos Guerrero M.L., McDonald P., Roy A., Yang Z. vol. 8. Vaccines; Basel): 2020. ('Identification of Vaccinia Virus Inhibitors and Cellular Functions Necessary for Efficient Viral Replication by Screening Bioactives and FDA-Approved Drugs). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perzia B., Theotoka D., Li K., Moss E., Matesva M., Gill M., Kibe M., Chow J., Green S. 'Treatment of ocular-involving monkeypox virus with topical trifluridine and oral tecovirimat in the 2022 monkeypox virus outbreak'. Am J Ophthalmol Case Rep. 2023;29 doi: 10.1016/j.ajoc.2022.101779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prichard M.N., Keith K.A., Johnson M.P., Harden E.A., McBrayer A., Luo M., Qiu S., Chattopadhyay D., Fan X., Torrence P.F., Kern E.R. 'Selective phosphorylation of antiviral drugs by vaccinia virus thymidine kinase'. Antimicrob. Agents Chemother. 2007;51:1795–1803. doi: 10.1128/AAC.01447-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothenburg S., Yang Z., Beard P., Sawyer S.L., Titanji B., Gonsalves G., Kindrachuk J. 'Monkeypox emergency: urgent questions and perspectives'. Cell. 2022;185:3279–3281. doi: 10.1016/j.cell.2022.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadowski L.A., Upadhyay R., Greeley Z.W., Margulies B.J. 'Current drugs to treat infections with herpes simplex viruses-1 and -2'. Viruses. 2021;13 doi: 10.3390/v13071228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist E.A., Sassine J. 'Antivirals with activity against mpox: a clinically oriented review'. Clin. Infect. Dis. 2023;76:155–164. doi: 10.1093/cid/ciac622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofia M.J., Chang W., Furman P.A., Mosley R.T., Ross B.S. 'Nucleoside, nucleotide, and non-nucleoside inhibitors of hepatitis C virus NS5B RNA-dependent RNA-polymerase (vol 55, pg 2481, 2012)'. J. Med. Chem. 2017;60 doi: 10.1021/jm201384j. 3219-19. [DOI] [PubMed] [Google Scholar]
- Springer Y.P., Hsu C.H., Werle Z.R., Olson L.E., Cooper M.P., Castrodale L.J., Fowler N., McCollum A.M., Goldsmith C.S., Emerson G.L., Wilkins K., Doty J.B., Burgado J., Gao J., Patel N., Mauldin M.R., Reynolds M.G., Satheshkumar P.S., Davidson W., Li Y., McLaughlin J.B. 'Novel orthopoxvirus infection in an Alaska resident'. Clin. Infect. Dis. 2017;64:1737–1741. doi: 10.1093/cid/cix219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tannous B.A., Teng J. 'Secreted blood reporters: insights and applications'. Biotechnol. Adv. 2011;29:997–1003. doi: 10.1016/j.biotechadv.2011.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavakolpour S., Darvishi M., Mirsafaei H.S., Ghasemiadl M. 'Nucleoside/nucleotide analogues in the treatment of chronic hepatitis B infection during pregnancy: a systematic review'. Inf. Disp. 2018;50:95–106. doi: 10.1080/23744235.2017.1384957. [DOI] [PubMed] [Google Scholar]
- Temmink O.H., Emura T., de Bruin M., Fukushima M., Peters G.J. 'Therapeutic potential of the dual-targeted TAS-102 formulation in the treatment of gastrointestinal malignancies'. Cancer Sci. 2007;98:779–789. doi: 10.1111/j.1349-7006.2007.00477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theves C., Crubezy E., Biagini P. 'History of smallpox and its spread in human populations'. Microbiol. Spectr. 2016;4 doi: 10.1128/microbiolspec.PoH-0004-2014. [DOI] [PubMed] [Google Scholar]
- Topalis D., Collinet B., Gasse C., Dugue L., Balzarini J., Pochet S., Deville-Bonne D. 'Substrate specificity of vaccinia virus thymidylate kinase'. FEBS J. 2005;272:6254–6265. doi: 10.1111/j.1742-4658.2005.05006.x. [DOI] [PubMed] [Google Scholar]
- Vandercam B., Moreau M., Goffin E., Marot J.C., Cosyns J.P., Jadoul M. 'Cidofovir-induced end-stage renal failure'. Clin. Infect. Dis. 1999;29:948–949. doi: 10.1086/520475. [DOI] [PubMed] [Google Scholar]
- Wang J., Shahed-Ai-Mahmud M., Chen A., Li K., Tan H., Joyce R. An overview of antivirals against monkeypox virus and other orthopoxviruses. J. Med. Chem. 2023;66:4468–4490. doi: 10.1021/acs.jmedchem.3c00069. [DOI] [PubMed] [Google Scholar]
- Warner B.M., Klassen L., Sloan A., Deschambault Y., Soule G., Banadyga L., Cao J., Strong J.E., Kobasa D., Safronetz D. 'In vitro and in vivo efficacy of tecovirimat against a recently emerged 2022 monkeypox virus isolate'. Sci. Transl. Med. 2022;14 doi: 10.1126/scitranslmed.ade7646. [DOI] [PubMed] [Google Scholar]
- Weiner Z.P., Salzer J.S., LeMasters E., Ellison J.A., Kondas A.V., Morgan C.N., Doty J.B., Martin B.E., Satheshkumar P.S., Olson V.A., Hutson C.L. 'Characterization of Monkeypox virus dissemination in the black-tailed prairie dog (Cynomys ludovicianus) through in vivo bioluminescent imaging'. PLoS One. 2019;14 doi: 10.1371/journal.pone.0222612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2011. Bugs, Drugs and Smoke: Stories from Public Health. [Google Scholar]
- Xie Y., Yin W., Zhang Y., Shang W., Wang Z., Luan X., Tian G., Aisa H.A., Xu Y., Xiao G., Li J., Jiang H., Zhang S., Zhang L., Xu H.E., Shen J. 'Design and development of an oral remdesivir derivative VV116 against SARS-CoV-2'. Cell Res. 2021;31:1212–1214. doi: 10.1038/s41422-021-00570-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z. Monkeypox: a potential global threat? J. Med. Virol. 2022;94:4034–4036. doi: 10.1002/jmv.27884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang G., Pevear D.C., Davies M.H., Collett M.S., Bailey T., Rippen S., Barone L., Burns C., Rhodes G., Tohan S., Huggins J.W., Baker R.O., Buller R.L., Touchette E., Waller K., Schriewer J., Neyts J., DeClercq E., Jones K., Hruby D., Jordan R. 'An orally bioavailable antipoxvirus compound (ST-246) inhibits extracellular virus formation and protects mice from lethal orthopoxvirus Challenge'. J. Virol. 2005;79:13139–13149. doi: 10.1128/JVI.79.20.13139-13149.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Guang, Pevear Daniel C., Davies Marc H., Collett Marc S., Bailey Tom, Rippen Susan, Barone Linda, Burns Chris, Rhodes Gerry, Tohan Sanjeev, Huggins John W., Robert O., Baker, Mark Buller R.L., Touchette Erin, Waller Kem, Schriewer Jill, Neyts Johan, DeClercq Erik, Jones Kevin, Hruby Dennis, Jordan Robert. 'An orally bioavailable antipoxvirus compound (ST-246) inhibits extracellular virus formation and protects mice from lethal orthopoxvirus challenge'. J. Virol. 2005;79:13139–13149. doi: 10.1128/JVI.79.20.13139-13149.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Bruno D.P., Martens C.A., Porcella S.F., Moss B. 'Simultaneous high-resolution analysis of vaccinia virus and host cell transcriptomes by deep RNA sequencing'. Proc. Natl. Acad. Sci. U. S. A. 2010;107:11513–11518. doi: 10.1073/pnas.1006594107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Reynolds S.E., Martens C.A., Bruno D.P., Porcella S.F., Moss B. 'Expression profiling of the intermediate and late stages of poxvirus replication'. J. Virol. 2011;85:9899–9908. doi: 10.1128/JVI.05446-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Zhilong, Gray Mark, Winter Lake. Why do poxviruses still matter? Cell Biosci. 2021;11:96. doi: 10.1186/s13578-021-00610-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B., Chang J. The first Chinese oral anti-COVID-19 drug Azvudine launched. Innovation. 2022;3 doi: 10.1016/j.xinn.2022.100321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J.L., Li Y.H., Wang L.L., Liu H.Q., Lu S.Y., Liu Y., Li K., Liu B., Li S.Y., Shao F.M., Wang K., Sheng N., Li R., Cui J.J., Sun P.C., Ma C.X., Zhu B., Wang Z., Wan Y.H., Yu S.S., Che Y., Wang C.Y., Wang C., Zhang Q., Zhao L.M., Peng X.Z., Cheng Z., Chang J.B., Jiang J.D. 'Azvudine is a thymus-homing anti-SARS-CoV-2 drug effective in treating COVID-19 patients'. Signal Transduct. Targeted Ther. 2021;6:414. doi: 10.1038/s41392-021-00835-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.