Abstract
Background:
While some studies suggest that nutritional supplementation may reduce aggressive behavior in children, they have not examined whether its efficacy may be enhanced in conjunction with other treatment approaches. This study tests the hypothesis that a nutritional supplementation of omega-3, multivitamins, and minerals over 3 months, combined with cognitive behavior therapy, will reduce childhood aggression.
Methods:
In this randomized, single-blind, stratified, factorial trial, a high-risk community sample of 290 children aged 11–12 years were randomized into Nutrition only, cognitive behavioral therapy (CBT) only, Nutrition + CBT, and Control groups. The primary outcome measures of child- and parent-reported aggressive and antisocial behavior were collected at 0 months (baseline), 3 months (end of treatment), 6 months (3 months posttreatment), and 12 months (9 months posttreatment). The trial (‘Healthy Brains & Behavior: Understanding and Treating Youth Aggression (HBB)’ was registered at ClinicalTrials.gov at https://clinicaltrials.gov/ct2/show/NCT00842439.
Results:
For child self-reports, children in the Nutrition only group showed reduced externalizing behavior compared to Controls at 3 months. At 6 months, the Nutrition + CBT group scored lower on externalizing behavior compared to both CBT only and Control groups. Findings were more in evidence for an Aggressive-Reactive form of antisocial behavior than for a Callous-Proactive form. Effect sizes were in the small-to-medium range (d = −.33 to −.37). Group differences were not sustained 9 months posttreatment, and no other effects were significant.
Conclusions:
Findings provide some limited support for the efficacy of omega-3, vitamin, and mineral supplementation in reducing aggressive behavior in children, and represent the first evaluation of nutritional supplements in conjunction with CBT.
Keywords: Aggression, omega-3, cognitive behavioral therapy, reactive, callous, nutrition, externalizing
Introduction
There is growing interest in nutritional interventions to attenuate adult psychopathology. Fish consumption is negatively associated with cross-country homicide rates at a level of r = −.63 (Hibbeln, 2001). Experimentally, randomized controlled trial (RCT) studies have shown that omega-3, multivitamin, and mineral supplementation reduce offending in both young adult English prisoners (Gesch, Hammond, Hampson, Eves, & Crowder, 2002) and in Dutch young adult offenders (Zaalberg, Nijman, Bulten, Stroosma, & van der Staak, 2010). Furthermore, an RCT of omega-3, multivitamins, and minerals supplementation reduced aggressive behavior and impulsivity in adult Welshmen (Long & Benton, 2013). Taken together, these cross-cultural adult findings suggest that nutritional supplementation can reduce aggressive and antisocial behavior in adults.
A foundational question concerns whether these initial adult findings on antisocial and aggressive behavior can be developmentally substantiated earlier in life in children. An experimental environmental enrichment at ages 3–5 years that included 2.5 extra portions of fish per week in Mauritius (the African subcontinent), combined with cognitive stimulation and exercise, not only matured brain functioning by 1.1 years at age 11 years but also reduced criminal offending by 34% at age 23 years (Raine, 2013; Raine, Mellingen, Liu, Venables, & Mednick, 2003; Raine et al., 2001). It has also been documented that poor nutritional status in 1,795 Mauritian 3-year-olds predisposes to aggressive and antisocial behavior at ages 8, 11, and 17 years (Liu, Raine, Venables, Dalais, & Mednick, 2004), taking further prior findings from the Netherlands showing that poor prenatal nutrition predisposes to later antisocial personality disorder (Gesch et al., 2002). More recently, an RCT of omega-3 in 200 three-year-old Mauritian children documented a 41.6% reduction in externalizing behavior problems (specifically antisocial and aggressive behavior) in 8–16-year-old community children 6 months after the treatment ended (Raine, Portnoy, Liu, Mahoomed, & Hibbeln, 2015). Overall, prior findings suggest that nutritional supplementation may reduce childhood antisocial and aggressive behavior.
This study attempts to address three core questions. First, can we extend and replicate our findings on African 11-year-old children to show that nutritional supplementation reduces aggressive and antisocial behavior in 11-year-old American children? Second, can nutritional supplementation in combination with a common treatment for antisocial/aggressive behavior – cognitive behavioral therapy (CBT) – be more effective in reducing these child behavior problems? Third, are any beneficial effects more likely to be found for aggression that is reactive and impulsive in nature compared to aggression which is more proactive and planned?
Methods
Trial design
This consisted of a randomized, single-blind, stratified, 4 × 4 factorial, open trial of high-risk children in the community, with equal randomization to the four study groups: CBT only (n = 73), Nutrition only (n = 72), Nutrition + CBT (n = 73), Controls (n = 72). Trial design remained unchanged throughout the study.
Participants
Eligibility criteria.
Full details of participants, design, and methods of recruitment are given elsewhere (Liu et al., 2013; Richmond, Cheney, Soyfer, Kimmel, & Raine, 2013). In brief, participants consisted of children aged 11–12 years, able to speak English, willing to participate in an RCT, residing in the community, and either meeting full or borderline clinical criteria for conduct disorder or oppositional defiant disorder, or scoring 1 SD above the mean on either proactive or reactive scores on the Reactive–Proactive Aggression Questionnaire (Raine et al., 2006). Participants were selected from a larger baseline sample of 454 children. Exclusion criteria consisted of intellectual disability, significant psychiatric and physical illness, extensive use of nutritional supplements within the previous 3 months, and seafood allergy. Written informed consent was obtained from the caregiver, while assent was obtained from the child. Ethics approval was obtained from IRB boards at the University of Pennsylvania and also the Philadelphia Department of Health.
Study setting.
Data collection took place in interview rooms at the University of Pennsylvania from February 2009 to May 2013. The study was registered in ClinicalTrials.gov under the identifier NCT00842439. CBT sessions were conducted in study offices or the participant’s homes.
Nutritional and CBT interventions
Nutritional supplementation.
Nutritional supplementation consisted of omega-3 fatty acids, multivitamins, and calcium. The omega-3 supplement consisted of a daily 200 ml drink (SmartFish Recharge) containing 1,000 mg of omega-3 (300 mg of DHA, 200 mg of EPA, 400 mg of alpha-linolenic acid, and 100 mg of DPA) (see also Appendix S1, available online). This drink was chosen because: (a) it contains an appreciably higher dosage of omega-3 than standard capsules in a relatively small liquid quantity (60.6% of the size of a standard can of cola) suitable for child consumption and (b) the fruit-flavored drink may be better tolerated and result in higher compliance with children than standard capsules. The daily dose of multivitamins consisted of 12 vitamins and seven minerals administered as one chewable tablet (see Appendix S1) together with one fruit-flavored chewable tablet containing calcium (600 mg) and vitamin D (400 micrograms).
CBT.
Full details of the CBT program are given in Appendix S2. In brief, the CBT program was a modification of the Penn Resiliency Program (Gillham, Jaycox, Reivich, Seligman, & Silver, 1990; Jaycox, Reivich, Gillham, & Seligman, 1998), consisting of a manualized, child-caregiver intervention which was delivered in 12 weekly 1-h sessions, supplemented with weekly home exercises. It was adapted from a school-based to a home-based, conjoint, child-caregiver intervention and tailored to enhance cultural relevancy and reading levels. It gave a targeted focus to anger and aggression issues and recognizing and addressing cognitive processes contributing to emotional distress and maladaptive behaviors while building coping, decision-making, and problem-solving skills. The interventionist was a licensed therapist with expertise in CBT and training in the manualized intervention and protocol. The Control group received a list of help resources for their child that they could follow-up on at their discretion.
Treatment duration and administration.
Treatment duration for both nutrition and CBT interventions was 3 months. No changes were made to trial outcomes after treatment commenced. The nutritional supplements were administered by the parents to their children each day at any suitable time.
Primary outcome measures
Reactive–Proactive Aggression Questionnaire (RPQ).
Children completed the self-report RPQ, yielding scales of reactive, proactive, and total aggression (Raine et al., 2006). Reliability and validity have been extensively documented (Baker, Raine, Liu, & Jacobson, 2008; Fossati et al., 2009).
Child Behavior Checklist (CBCL) and Youth Self-Report (YSR).
The CBCL (parent-report) and the YSR (child report) are extensively used psychometric instruments with high reliability/validity in many countries (Achenbach & Rescorla, 2001). It yielded subscale scores for rule-breaking and aggression.
The Antisocial Personality Screening Device (APSD).
The APSD assesses both parent- and child-reported psychopathic traits (Frick, Bodin, & Barry, 2000), yielding three subscales assessing callous-unemotional traits, narcissism, and impulsivity.
Conduct and Oppositional Defiant Disorder Scales (CODDS).
This 23-item parent- and child-report measure is modeled on DSM 5 and assesses the eight oppositional defiant disorder criteria and the 15 conduct disorder criteria (Raine 2009). Each item is assessed on a 3-point scale (never, sometimes, often), with items summated to yield conduct disorder and oppositional defiant disorder scores.
Aggression questionnaire.
The self-report version of the brief Buss–Perry Aggression Questionnaire (Bryant & Smith, 2001) was administered to children, producing subscale scores for physical aggression, verbal aggression, indirect aggression, anger, and hostility.
NIMH-DISC-IV.
The NIMH-DISC-IV is a structured, computer-based diagnostic instrument designed for nonclinicians to diagnose DSM-IV psychiatric disorders in children (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000), including ADHD. Parents were interviewed about their child by research assistants trained on DISC administration. Total symptom counts of oppositional defiant disorder and conduct disorder provided dimensional assessments of both disorders.
To both provide more robust indices of externalizing behavior and to help reduce Type 1 error, all child and parent report scales were separately factor analyzed to produce overarching measures of externalizing behavior using principal component analysis (see Appendix S1).
Sample size
Based on prior findings for externalizing behavior by the first author (Raine et al., 2015), a small-to-medium effect size was anticipated. The final total sample size of 290 would have power of 0.80 to detect a small-to-medium effect size of f = .13, α = .05, critical F (9,858) = 1.89.
Randomization and allocation
Participants were randomized equally into the four treatment groups by the project coordinator. Stratified randomization with blocking within strata was conducted using blocks with strata consisting of age (11 vs. 12), gender (male vs. female), and ethnicity (African American vs. Other). Restricted randomization to group was conducted using a computer-generated list of random numbers generated by SPSS (IBM, Version 22.0., Armonk, NY).
Allocation concealment was maintained by having the intervention allocation conducted separately by the project coordinator who was kept independent of participants and the investigators, and with all research assistants who assessed externalizing behavior blind to group membership.
Adherence to protocol
Adherence to the treatment regimen was assessed by assays of fasting serum omega-6 and omega-3 fats from venous blood drawn by a nurse at both baseline and 3 months (end of treatment). Samples were assayed blinded for treatment condition at the Section of Nutritional Neurosciences, National Institute of Alcohol Abuse and Alcoholism (see Lin, Loewke, Hyun, Leazer, and Hibbeln (2012) for full methodological details).
Blinding
In this single-blind open trial, interviewers were blinded to group assignment.
Statistical methods
An intention-to-treat (ITT) design using all randomly assigned participants was employed for all data analyses. Linear mixed effects modeling (Molenberghs & Verbeke, 2005) was utilized to deal with missing data. In compliance with CONSORT guidelines (Moher, 2010), the analytic plan focused on testing group × time interactions. Intervention group and group × time interaction terms were entered as fixed effects, with outcome measures modeled using maximum likelihood estimation with a first-order autoregressive covariance structure and with homogeneous variances to account for the correlation between time points. The random intercept was included to account for individual differences. Baseline (month 0) antisocial scores, age, ethnicity, social adversity, and IQ were entered as covariates to deal with selective attrition (see below) and to equalize groups on antisocial scores at baseline to facilitate interpretation of posttreatment group differences at 3-, 6-, and 12-month retests, the primary focus of the study. False discovery rate control (Benjamini & Hochberg, 1995) was employed to control for Type I error on group comparisons within each time period. Figures are based on estimated marginal means for posttreatment values after adjusting for baseline covariates.
Results
Demographics and adherence to protocol
Demographics.
No significant group differences were observed at baseline on age, gender, and ethnicity (see Table 1), documenting that stratification procedures were successful.
Table 1.
Baseline demographic, antisocial, and blood omega-3 level data, together with statistical comparisons for dropouts and completers, with standard deviations in parentheses
| Completers | Dropouts | Statistic | P | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 11.40 (.52) | 11.53 (.52) | t = −2.03 | .04 |
| Social adversity | 4.47 (3.97) | 2.32 (2.49) | t = 1.73 | .08 |
| IQ | 90.28 (13.1) | 94.61 (13.35) | t = −2.69 | .008 |
| Sex | ||||
| Male (N) | 94 | 58 | χ2 = 0.05 | .82 |
| Female (N) | 84 | 49 | ||
| Race | ||||
| White (N) | 11 | 18 | χ2 = 7.88 | .005 |
| Minority (N) | 168 | 92 | ||
| Antisocial measures | ||||
| Child report: Externalizing | .27 (.73) | .11 (.75) | t = 1.83 | .07 |
| Child report: Aggressive-Reactive | .28 (.77) | .11 (.80) | t = 1.76 | .08 |
| Child report: Callous-Proactive | .25 (.09) | .86 (.79) | t = 1.56 | .12 |
| Parent report: Externalizing | .56 (.90) | .31 (.84) | t = 2.39 | .02 |
| Omega-3 status | ||||
| Omega-3 at baseline | 19.46 (5.80) | 19.83 (5.21) | t = −.38 | .70 |
Adherence to protocol.
Adherence to the protocol was assessed using blood omega-3 fatty acid levels(see Table 1). A significant group × time interaction was observed, F(3,157) = 10.4, p < .0001. As predicted, groups differed posttreatment (F(1,159) = 14.8, p < .001), but not at baseline (p = .34). Those taking omega-3 showed a significant increase in omega-3 levels from 0 to 3 months (t = 6.2, p < .0001, d = 1.0), whereas those not assigned to omega-3 showed no change across time (p = .20).
Participant flow, attrition, and outcome measures
Participant flow and attrition.
No participant loss was observed on baseline assessment after randomization. Later attrition rates (see Appendix S3) were as follows: 3 months (26.6%), 6 months (27.2%), 12 months (37.9%). While attrition was somewhat lower (by 20.8%) in the Nutrition only group (47.2%) compared to CBT only (61.6%), Nutrition + CBT (58.9%), and Control (58.3%) groups, this difference was not significant (χ2 = 3.58, df = 3, p = .31). As attrition was significantly related to age, ethnicity, IQ, antisocial behavior, together with a trend for social adversity (see Table 2), these variables were entered as covariates in all analyses.
Table 2.
Demographics, baseline externalizing behavior, and omega-3 adherence data together with statistical comparisons for intervention groups. Standard deviations are in parentheses
| Cognitive behavioral therapy (CBT) only | Nutrition only | Nutrition & CBT | Controls | Statistic | p | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age | 11.35 (.48) | 11.42 (.53) | 11.53 (.53) | 11.51 (.53) | F = 1.92 | .13 |
| Social adversity | 4.37 (2.24) | 4.53 (2.49) | 4.46 (2.50) | 3.77 (2.31) | F = 1.53 | .21 |
| IQ | 92.67 (13.86) | 90.72 (13.34) | 92.00 (13.26) | 92.32 (13.07) | F = 0.29 | .83 |
| Sex | ||||||
| Male (N) | 40 | 42 | 36 | 34 | χ2 = 2.29 | .51 |
| Female (N) | 32 | 29 | 34 | 38 | ||
| Race | ||||||
| White (N) | 7 | 7 | 8 | 7 | χ2 = 0.10 | .99 |
| Minority (N) | 66 | 64 | 65 | 65 | ||
| Child report | ||||||
| Externalizing behavior | .19 (.70) | .26 (.71) | .24 (.86) | .15 (.71) | F = 0.29 | .83 |
| Aggressive-Reactive | .18 (.76) | .25 (.73) | .25 (.87) | .19 (.77) | F = 0.17 | .92 |
| Callous-Proactive | .20 (.72) | .25 (.81) | .23 (.99) | .08 (.81) | F = 0.66 | .58 |
| Parent report | ||||||
| Externalizing behavior | .41 (.92) | .42 (.91) | .47 (.80) | .56 (.90) | F = 0.46 | .71 |
| Adherence to supplementation | ||||||
| Omega-3 baseline | 17.46 (2.96) | 16.55 (2.55) | 16.92 (2.42) | 17.69 (4.31) | F = 1.14 | .34 |
| Omega-3 posttreatment | 17.41 (2.54) | 21.80 (6.66) | 20.38 (6.24) | 18.42 (4.98) | F = 5.63 | .001 |
Factor analyses of outcome measures.
Parent and child measures of externalizing behavior were factor analyzed separately to both provide overarching indicators and reduce Type I error. Full details are provided in Appendix S1. Analyses produced overall measures of parent-report and child-report externalizing behavior, and in addition, two subfactors of child-report, ‘Aggressive-Reactive’ and ‘Callous-Proactive’ antisocial behavior.
Treatment effects on child antisocial behavior – child reports
Unadjusted means from mixed effects analyses for child-report and parent-report measures at all four time points are detailed in Table 3. Analyses below are based on the estimated marginal means.
Table 3.
Unadjusted means with 95% confidence intervals (in parentheses) from mixed effects models on child behavior outcomes in the four intervention groups for the four assessment periods
| Child report externalizing | Child report Aggressive-Reactive | Child report Callous-Proactive | Parent report externalizing | |
|---|---|---|---|---|
| Cognitive behavioral therapy (CBT) only intervention group | ||||
| 0 months | .19 (.02, .36) | .18 (−.00, .36) | .20 (.01, .40) | .41 (.22, .60) |
| 3 months | .18 (.00, .37) | .18 (−.01, .38) | .16 (−.05, .37) | .24 (.03, .44) |
| 6 months | .19 (−.01, .38) | .19 (−.02, .39) | .16 (−.06, .38) | .31 (.10, .52) |
| 12 months | .21 (.00, .41) | .21 (−.02, .42) | .22 (−.02, .46) | .12 (−.10, .34) |
| Nutrition only intervention group | ||||
| 0 months | .26 (.08, .43) | .25 (.07, .44) | .26 (.06, .45) | .42 (.22, .61) |
| 3 months | .11 (−.07, .30) | .06 (−.13, .26) | .24 (.03, .44) | .15 (−.05, .36) |
| 6 months | .16 (−.03, .34) | .16 (−.03, .36) | .15 (−.06, .36) | .08 (−.13, .28) |
| 12 months | .04 (−.15, .24) | .06 (−.15, .27) | .01 (−.21, .24) | .05 (−.17, .26) |
| CBT and Nutrition intervention group | ||||
| 0 months | .24 (.07, .41) | .25 (.06, .43) | .23 (.04, .42) | .47 (.27, .66) |
| 3 months | .18 (−.01, .36) | .17 (−.03, .37) | .19 (−.03, .40) | .33 (.13, .54) |
| 6 months | .01 (−.18, .20) | .01 (−.19, .21) | .02 (−.20, .23) | .21 (.00, .41) |
| 12 months | .11 (−.09, .30) | .10 (−.11, .30) | .12 (−.10, .35) | .08 (−.13, .30) |
| Control group - no intervention | ||||
| 0 months | .15 (−.02, .33) | .19 (.00, .37) | .08 (−.12, .27) | .56 (.37, .76) |
| 3 months | .26 (.08, .45) | .34 (.134, .54) | .08 (−.13, .30) | .34 (.13, .55) |
| 6 months | .16 (−.03, .34) | .15 (−.05, .35) | .16 (−.06, .38) | .26 (.06, .47) |
| 12 months | −.01 (−.21, .19) | .00 (−.21, .21) | −.03 (−.25, .20) | .15 (−.06, .36) |
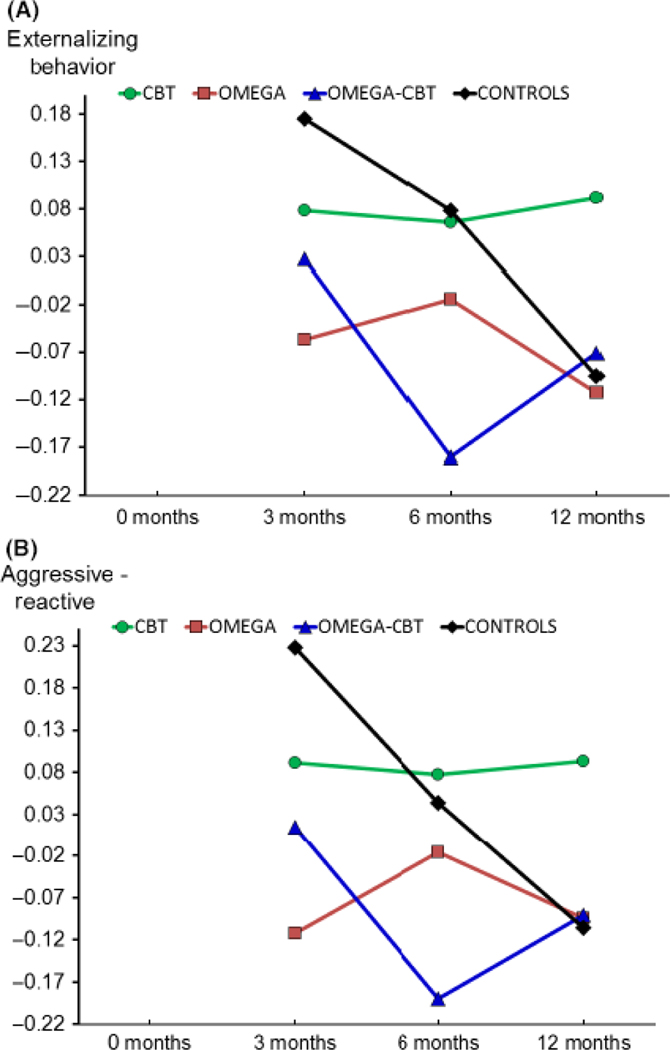
Externalizing behavior.
A significant group × time interaction (p = .037) was observed and is illustrated in Figure 1. At 3 months, the Nutrition only group scored significantly lower than Controls (p = .044, CI = −.003 to −.661, d = −.33). At 6 months, the combined CBT + Nutrition group scored lower than both Controls (p = .023, CI = −.044 to −.700, d = −.37) and the CBT only group (p = .031, CI = −.027 to −.068, d = −.35). At 12 months, the Nutrition only group showed a trend (p .093, CI = −.443 to .034, d = −.28) toward lower scores compared to the CBT only group. No comparisons survived false discovery rate control which corrects for multiple comparisons.
Figure 1.
Illustration from intention-to-treat analyses (all subjects included) of the significant group × time interaction and group differences in (A) child-reported total Externalizing Behavior focusing on group differences after treatment, showing lower scores in the Nutrition only group at 3 months, and in the Nutrition + cognitive behavioral therapy (CBT) group at 6 months, compared to Controls (upper figure), and (B) group differences in child-reported Aggressive-Reactive behavior (lower figure) illustrating the lower scores in the Nutrition only group at 3 months compared to Controls, and in the Nutrition + CBT group at 6 months compared to the CBT only group. Values are posttreatment estimated marginal means with baseline values at 0 months covaried, equating groups at this time point
Aggressive-Reactive.
A significant group × time interaction (p = .024) was observed and is illustrated in Figure 2. At 3 months, the Nutrition only group scored lower than Controls (p = .006, d = −.45, CI = −.118 to −.779), together with a trend for the Nutrition only group to have lower scores compared to the CBT only group (p = .096). Similarly, the combined Nutrition + CBT group showed a trend toward lower scores compared to Controls (p = .085). At 6 months, the combined Nutrition + CBT group showed significantly lower scores compared to the CBT only group (p = .03, d = −.35, CI = −.027 to −.683), with a trend toward lower scores compared to Controls (p = .055). The only comparison that survived false discovery rate control was the Nutrition only group scoring lower than Controls at 3 months.
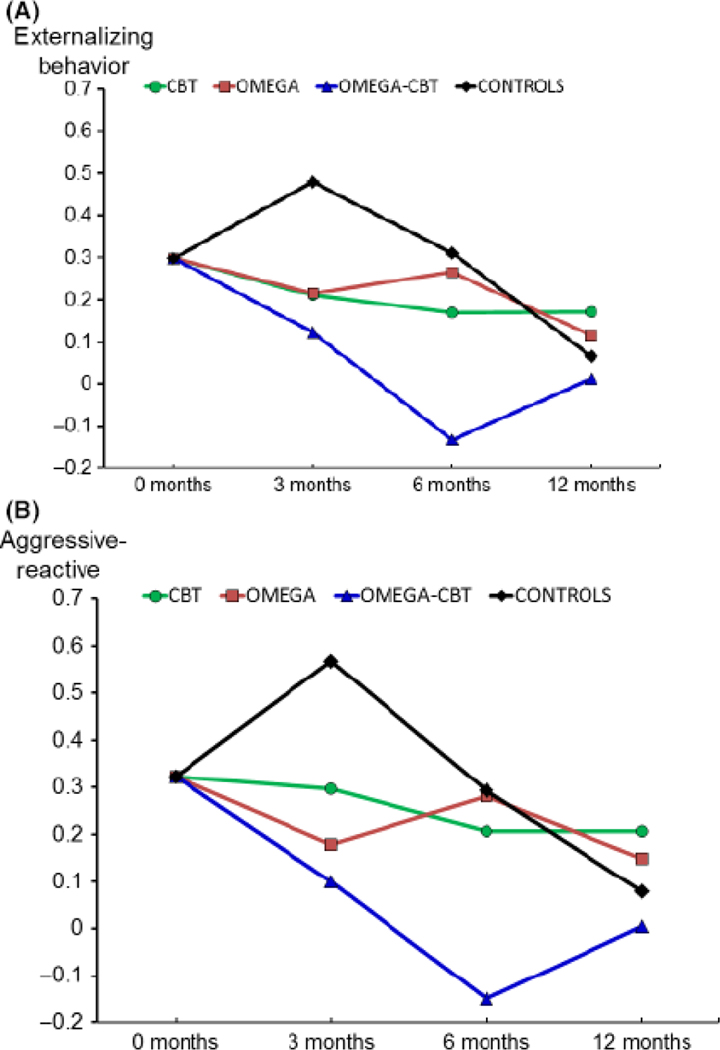
Figure 2.
Illustration from the modified intention-to-treat analyses (only completers included) that replicate the significant group × time interactions from intention-to-treat analyses for (A) child-reported externalizing behavior (upper figure) and (B) child-reported Aggressive-Reactive behavior (lower figure). Values are estimated marginal means with baseline values at 0 months covaried
Callous-Proactive.
The group × time interaction was nonsignificant (p = .11).
Treatment effects on child externalizing behavior – parent reports
The group × time interaction was nonsignificant (p = .40).
Controlling for ADHD, sensitivity analyses, and adverse events
Controlling for ADHD.
Analyses were repeated after adding diagnosis for ADHD as a covariate. The significant group × time interactions were replicated for child self-reported Externalizing Behavior (p = .043) and Aggressive-Reactive dimensions (p = .034).
Sensitivity analyses.
To assess robustness of the ITT design that used mixed effects models, sensitivity analyses were run using a modified intention-to-treat design, where participants lost to follow-up were excluded, with analyses conducted using repeated measures multivariate analysis of variance, using the same covariates as in ITT analyses. The significant group × time interactions were replicated for child self-reported Externalizing Behavior (F = 2.33, df = 6,222, p = .034, η2 = .059) and Aggressive-Reactive dimensions (F = 2.53, df = 6,222, p < .022, η2 = .064). Results are illustrated in Figure 2 and broadly repeat the same pattern as in the ITT analyses, with the strongest group difference being the decline of the Nutrition + CBT group at 6 months.
Adverse events.
No major adverse events were reported. Posttreatment questionnaires indicated that the nutritional supplements were well-tolerated. Minor adverse events are reported in detail in Appendix S4. No participant withdrew due to these minor events.
Discussion
Some limited support was found for the efficacy of nutritional supplementation in reducing childhood aggression. Nutritional supplementation by itself significantly reduced child aggression immediately at the end of treatment compared to Controls. Adding nutritional supplementation to CBT reduced child aggression 3 months posttreatment compared to CBT only and Control groups. Effects were found for child but not parent reports. Positive findings were more in evidence for an impulsive, reactive form of aggression than for Callous-Proactive behavior. Findings were not sustained 9 months posttreatment. Effect sizes were in the small-to-medium range (d = −.33 to −.37). Sensitivity analyses replicated the main findings. Results could not be accounted for by group differences in potential confounds, including ADHD and baseline omega-3 levels. Taken together, findings both provide some evidence for the short-term efficacy of omega-3 in attenuating child behavior problems, but augur for due caution in drawing conclusions on the long-term efficacy in the United States and highlight the further need for both cross-national and within-national research.
Prior studies
While the current findings broadly converge with our prior findings from Mauritius, there are also important differences. In Mauritius, we found that parent (but not child) reports of child externalizing behavior were significantly reduced by omega-3 supplementation (d = −.35) 6 months after treatment termination. In contrast, findings from Philadelphia were significant for child but not for parent reports. Indeed, the only comparison surviving strict false discovery rate control consisted of the Nutrition only group scoring lower than Controls at 3 months on Aggressive-Reactive behavior. This finding provides support for the short-term efficacy of nutritional supplementation in reducing child aggressive behavior, but we were unable to replicate the long-term beneficial effects observed in Mauritius.
There are several important differences between the Mauritius and Philadelphia studies which could help explain differences. These include culture (tropical island in the African subcontinent vs. Philadelphia), ethnicity (Indian and Creoles vs. pre-dominantly African Americans), risk status for aggressive/antisocial behavior (low vs. high), study dropout (low vs. high), and stability of the subject population (high vs. low). Importantly, omega-3 supplementation lasted for 6 months in Mauritius compared to just 3 months in Philadelphia. Future RCTs of omega-3 and other nutritional supplements should assess both cross-country and within-country replicability of findings in larger samples in order to allow firmer conclusions to be drawn.
Placing the current findings in the context of the wider literature, results of prior RCTs on antisocial behavior are mixed. Some find evidence for improved behavior (Gustafsson et al., 2010), while others such as Milte et al. (2012) who assessed oppositional behavior in ADHD children do not (Milte et al., 2012), although this latter study only had 52% power to detect a significant effect. Dosages and durations of omega-3 in RCTs vary widely, ranging from 124 mg/day for 20 weeks (Gesch et al., 2002) to 2,400 mg/day over 6 weeks (Dean, Bor, Adam, Bowling, & Bellgrove, 2014). There appears to be no clear relationship between study outcomes and either duration or dosage. The duration of the current study was comparable to the average of others, although dosage was relatively lower. Whether stronger improvements in behavior can be overserved with longer treatment and increased dosages than those of the current study remains to be seen.
Mechanisms of action
Why might nutritional supplementation alter aggressive behavior, particularly more reactive, impulsive forms of aggression? Prior brain imaging research has documented that reactively aggressive (but not proactively aggressive) adult murderers have reduced prefrontal functioning (Raine et al., 1998). A prior RCT of omega-3 supplementation employing before–after brain imaging documented that 11-year-old children – the same age as in the current study – show posttreatment enhanced functioning of the dorsolateral prefrontal cortex (McNamara et al., 2010). Dorsolateral prefrontal dysfunction is in turn a strongly replicated brain imaging correlate of antisocial behavior (Yang & Raine, 2009). It is conceivable therefore that nutritional supplementation could enhance prefrontal functioning in a way to improve impulsive control and emotion regulation and thus reduce aggressive-reactive behavior.
More broadly, this long-chain fatty acid plays a critical role in brain structure and function, making up approximately 35% of the cell membrane, enhancing neurite outgrowth, and regulating both neurotransmitter functioning and gene expression (McNamara & Carlson, 2006). Because brain imaging research on children and adolescents is increasingly documenting impairment to a number of brain regions outside the prefrontal cortex (Fairchild et al., 2013; Glenn & Yang, 2012; Marsh et al., 2013), and given the role played by omega-3 in cortical maturation (McNamara, Vannest, & Valentine, 2015), nutritional supplementation could to some degree assist in remediating brain risk factors for aggression other than the dorsolateral prefrontal cortex.
Study limitations
As with many RCTs extending beyond the end of treatment, we had significant dropouts that could bias findings. We dealt with this limitation using the ITT approach which is viewed as an important defense against selection bias (White, Horton, & Pocock, 2011). We also employed mixed effects modeling to deal with missing data, documented sensitivity analyses that replicated findings, and controlled for variables associated with attrition. Second, the sample size of 290 is not large, although more than 50% of all registered RCTs have fewer than 70 participants by design (Califf et al., 2012). Third, while adding nutritional supplements to CBT reduced child aggression compared to CBT only and Control groups, these findings were not maintained 6 months posttreatment and the CBT only group did not show improvements. It remains to be seen therefore whether omega-3 supplementation provides added value to CBT interventions for reducing aggression. Fourth, child but not parent reports produced significant effects, conceivably because at this age parents are less cognizant of their child’s behavior with their peers, particularly as many were from single parent families where parental monitoring will be limited (Choy et al., 2015). Because some studies find significant effects for objective measures but not subjective indicators of antisocial behavior (Gesch et al., 2002; Zaalberg et al., 2010), future studies should ideally include objective measures.
Conclusions
Despite study limitations and the small-to-medium effect sizes that were obtained (d = −.33 to −.37), the current study provides some support for considering nutritional supplementation as both an alternative and an adjunct treatment for child externalizing behavior. To our knowledge, this is the very first attempt to assess the efficacy of combining a nutritional intervention with CBT against these same treatments in isolation for any psychiatric or psychological condition.
We recognize that claims that nutritional supplements help reduce psychopathology create controversy and invite significant skepticism (Amminger, Schafer, Schlogelhofer, Klier, & McGorry, 2015). Opinions range from the belief in the toxic effects of the modern diet on behavior and the value of a balanced diet, to strong opposition from some researchers railing against inflated claims of dietary benefits (Sonuga-Barke, 2015). Further replication from methodologically strong studies is required to steer a balanced path that neither dogmatizes nor oversimplifies the message on nutrition and behavior (Sonuga-Barke, 2015).
Supplementary Material
Appendix S1. Multivitamins and factor analyses of antisocial measures.
Appendix S4. Minor adverse events.
Appendix S2. Cognitive behavior therapy interventions.
Appendix S5. CONSORT checklist.
Appendix S3. CONSORT participant flow diagram.
Key points.
There is growing interest in using nutritional supplements, particularly omega-3, to reduce child behaviour problems, but are they effective?
Is combining nutritional supplementation with a standard intervention particularly effective in reducing behavior problems?
This RCT showed that 3 months of omega-3 supplementation produced short-term posttreatment reductions in child-reported externalizing behavior problems.
Combining omega-3 supplementation with CBT reduced child externalizing behavior 3 months posttreatment.
Omega-3 was more effective in reducing an Aggressive-Reactive form of antisocial behavior than a Callous-Proactive form.
Omega-3 supplementation may be considered as an adjunct to more traditional clinical approaches in treating externalizing behavior problems.
Acknowledgements
This project was funded, in part, under a grant from the Pennsylvania Department of Health (SAP# 4100043366). The Department specifically disclaims responsibility for any analyses, interpretations, or conclusions. It was also supported in part by the Clinical & Translational Research Center, Perelman School of Medicine, University of Pennsylvania (grant number UL1-RR-024134), and by the Intramural Research Program of the National Institute on Alcohol Abuse and Alcoholism, Rockville, MD (J.H.). The authors thank the CHOP Pediatric Research Consortium for their help during the recruitment stage. The authors declare that they have no competing or potential conflicts of interest.
Footnotes
Conflict of interest statement: No conflicts declared.
Supporting information
Additional Supporting Information may be found in the online version of this article:
References
- Achenbach TM, & Rescorla L. (2001). Manual for the ASEBA: School-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Amminger GP, Schafer MR, Schlogelhofer R, Klier CM, & McGorry PD (2015). Longer-term outcome in the prevention of psychotic disorders by the Vienna omega-3 study. Nature Communications, 6, 7934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker LA, Raine A, Liu JH, & Jacobson KC (2008). Differential genetic and environmental influences on reactive and proactive aggression in children. Journal of Abnormal Child Psychology, 36, 1265–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, & Hochberg Y. (1995). Controlling the false discovery rate – a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B-Methodological, 57, 289–300. [Google Scholar]
- Bryant FB, & Smith BD (2001). Refining the architecture of aggression: A measurement model for the Buss-Perry aggression questionnaire. Journal of Research in Personality, 35, 138–167. [Google Scholar]
- Califf RM, Zarin DA, Kramer JM, Sherman RE, Aberle LH, & Tasneem A. (2012). Characteristics of clinical trials registered in ClinicalTrials.gov, 2007–2010. JAMA-Journal of the American Medical Association, 307, 1838–1847. [DOI] [PubMed] [Google Scholar]
- Choy O, Raine A, Portnoy J, Rudo-Hutt A, Gao Y, & Soyfer L. (2015). The mediating role of heart rate on the social adversity-antisocial behavior relationship: A social neurocriminology perspective. Journal of Research in Crime and Delinquency, 52, 303–341. [Google Scholar]
- Dean AJ, Bor W, Adam K, Bowling FG, & Bellgrove MA (2014). A randomized, controlled, crossover trial of fish oil treatment for impulsive aggression in children and adolescents with disruptive behavior disorders. Journal of Child and Adolescent Psychopharmacology, 24, 140–148. [DOI] [PubMed] [Google Scholar]
- Fairchild G, Hagan CC, Walsh ND, Passamonti L, Calder AJ, & Goodyer IM (2013). Brain structure abnormalities in adolescent girls with conduct disorder. Journal of Child Psychology and Psychiatry, 54, 86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossati A, Raine A, Borroni S, Bizzozero A, Volpi E, Santalucia I, & Maffei C. (2009). A cross-cultural study of the psychometric properties of the reactive-proactive aggression questionnaire among Italian nonclinical adolescents. Psychological Assessment, 21, 131–135. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Bodin SD, & Barry CT (2000). Psychopathic traits and conduct problems in community and clinic-referred samples of children: Further development of the psychopathy screening device. Psychological Assessment, 12, 382–393. [PubMed] [Google Scholar]
- Gesch CB, Hammond SM, Hampson SE, Eves A, & Crowder MJ (2002). Influence of supplementary vitamins, minerals and essential fatty acids on the antisocial behaviour of young adult prisoners: Randomised, placebo-controlled trial. British Journal of Psychiatry, 181, 22–28. [DOI] [PubMed] [Google Scholar]
- Gillham J, Jaycox L, Reivich K, Seligman J, & Silver T. (1990). The Penn Resiliency Program. Unpublished Manual, University of Pennsylvania, Philadelphia, PA. [Google Scholar]
- Glenn AL, & Yang Y. (2012). The potential role of the striatum in antisocial behavior and psychopathy. Biological Psychiatry, 72, 817–822. [DOI] [PubMed] [Google Scholar]
- Gustafsson PA, Birberg-Thornberg U, Duchen K, Landgren M, Malmberg K, Pelling H, .. . & Karlsson T. (2010). EPA supplementation improves teacher-rated behaviour and oppositional symptoms in children with ADHD. Acta Paediatrica, 99, 1540–1549. [DOI] [PubMed] [Google Scholar]
- Hibbeln JR (2001). Homicide mortality rates and seafood consumption: A cross-national analysis. World Review of Human Nutrition, 88, 41–46. [DOI] [PubMed] [Google Scholar]
- Jaycox L, Reivich K, Gillham J, & Seligman M. (1998). The prevention of depressive symptoms in schoolchildren. Behavioral Research and Therapy, 32, 801–816. [DOI] [PubMed] [Google Scholar]
- Lin YH, Loewke JD, Hyun DY, Leazer J, & Hibbeln JR (2012). Fast transmethylation of serum lipids using microwave irradiation. Lipids, 47, 1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JH, Raine A, Venables PH, Dalais C, & Mednick SA (2004). Malnutrition at age 3 years and externalizing behavior problems at ages 8, 11 and 17 years. American Journal of Psychiatry, 161, 2005–2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JH, Richmond TS, Raine A, Cheney R, Brodkin ES, Gur RC, & Gur RE (2013). The Healthy Brains and Behavior Study: Objectives, design, recruitment, and population coverage. International Journal of Methods in Psychiatric Research, 22, 204–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long SJ, & Benton D. (2013). A double-blind trial of the effect of docosahexaenoic acid and vitamin and mineral supplementation on aggression, impulsivity, and stress. Human Psychopharmacology-Clinical and Experimental, 28, 238–247. [DOI] [PubMed] [Google Scholar]
- Marsh AA, Finger EC, Fowler KA, Adalio CJ, Jurkowitz IT, Schechter JC, .. . & Blair RJR (2013). Empathic responsiveness in amygdala and anterior cingulate cortex in youths with psychopathic traits. Journal of Child Psychology and Psychiatry, 54, 900–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara RK, Able J, Jandacek R, Rider T, Tso P, Eliassen JC, .. . & Adler, C.M. (2010). Docosahexaenoic acid supplementation increases prefrontal cortex activation during sustained attention in healthy boys: A placebo-controlled, dose-ranging, functional magnetic resonance imaging study. American Journal of Clinical Nutrition, 91, 1060–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara RK, & Carlson SE (2006). Role of omega-3 fatty acids in brain development and function: Potential implications for the pathogenesis and prevention of psychopathology. Prostaglandins Leukotrienes and Essential Fatty Acids, 75, 329–349. [DOI] [PubMed] [Google Scholar]
- McNamara RK, Vannest JJ, & Valentine CJ (2015). Role of perinatal long-chain omega-3 fatty acids in cortical circuit maturation: Mechanisms and implications for psychopathology. World Journal of Psychiatry, 5, 15–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milte CM, Parletta N, Buckley JD, Coates AM, Young RM, & Howe PR (2012). Eicosapentaenoic and docosahexaenoic acids, cognition, and behavior in children with attention-deficit/hyperactivity disorder: A randomized controlled trial. Nutrition, 28, 670–677. [DOI] [PubMed] [Google Scholar]
- Moher D. (2010). CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. British Medical Journal, 343, c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molenberghs S, & Verbeke G. (2005). Models for discrete longitudinal data. New York: Springer. [Google Scholar]
- Raine A. (2009). The Conduct and Oppositional Defiant Disorder Scale (CODDS). Unpublished Manuscript, University of Pennsylvania, Philadelphia, PA. [Google Scholar]
- Raine A. (2013). The anatomy of violence: The biological roots of crime. New York, NY: Pantheon Books. [Google Scholar]
- Raine A, Dodge K, Loeber R, Gatzke-Kopp L, Lynam D, Reynolds C, .. . & Liu J. (2006). The reactive-proactive aggression questionnaire: Differential correlates of reactive and proactive aggression in adolescent boys. Aggressive Behavior, 32, 159–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raine A, Mellingen K, Liu JH, Venables P, & Mednick SA (2003). Effects of environmental enrichment at ages 3–5 years on schizotypal personality and antisocial behavior at ages 17 and 23 years. American Journal of Psychiatry, 160, 1627–1635. [DOI] [PubMed] [Google Scholar]
- Raine A, Meloy JR, Bihrle S, Stoddard J, LaCasse L, & Buchsbaum MS (1998). Reduced prefrontal and increased subcortical brain functioning assessed using positron emission tomography in predatory and affective murderers. Behavioral Sciences & the Law, 16, 319–332. [DOI] [PubMed] [Google Scholar]
- Raine A, Portnoy J, Liu JH, Mahoomed T, & Hibbeln JR (2015). Reduction in behavior problems with omega-3 supplementation in children aged 8–16 years: A randomized, double-blind, placebo-controlled, stratified, parallel-group trial. Journal of Child Psychology and Psychiatry, 56, 509–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raine A, Venables PH, Dalais C, Mellingen K, Reynolds C, & Mednick SA (2001). Early educational and health enrichment at age 3–5 years is associated with increased autonomic and central nervous system arousal and orienting at age 11 years: Evidence from the Mauritius Child Health Project. Psychophysiology, 38, 254–266. [PubMed] [Google Scholar]
- Richmond TS, Cheney R, Soyfer L, Kimmel R, & Raine A. (2013). Recruitment of community-residing youth into studies on aggression. Journal of Community Psychology, 41, 425–434. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJ (2015). Editorial: Diet and children’s behaviour problems – disentangling urban myth from clinical reality. Journal of Child Psychology and Psychiatry, 56, 497–499. [DOI] [PubMed] [Google Scholar]
- White I, Horton NJ, & Pocock SJ (2011). Strategy for intention to treat analysis in randomised trials with missing outcome data. British Medical Journal, 342, d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YL, & Raine A. (2009). Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Research: Neuroimaging, 174, 81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaalberg A, Nijman H, Bulten E, Stroosma L, & van der Staak C. (2010). Effects of nutritional supplements on aggression, rule-breaking, and psychopathology among young adult prisoners. Aggressive Behavior, 36, 117–126. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Multivitamins and factor analyses of antisocial measures.
Appendix S4. Minor adverse events.
Appendix S2. Cognitive behavior therapy interventions.
Appendix S5. CONSORT checklist.
Appendix S3. CONSORT participant flow diagram.