Abstract
Background
Currently, little is known regarding the optimal technique for the abdominal phase of RAMIE. The aim of this study was to investigate the outcome of robot-assisted minimally invasive esophagectomy (RAMIE) in both the abdominal and thoracic phase (full RAMIE) compared to laparoscopy during the abdominal phase (hybrid laparoscopic RAMIE).
Methods
This retrospective propensity-score matched analysis of the International Upper Gastrointestinal International Robotic Association (UGIRA) database included 807 RAMIE procedures with intrathoracic anastomosis between 2017 and 2021 from 23 centers.
Results
After propensity-score matching, 296 hybrid laparoscopic RAMIE patients were compared to 296 full RAMIE patients. Both groups were equal regarding intraoperative blood loss (median 200 ml versus 197 ml, p = 0.6967), operational time (mean 430.3 min versus 417.7 min, p = 0.1032), conversion rate during abdominal phase (2.4% versus 1.7%, p = 0.560), radical resection (R0) rate (95.6% versus 96.3%, p = 0.8526) and total lymph node yield (mean 30.4 versus 29.5, p = 0.3834). The hybrid laparoscopic RAMIE group showed higher rates of anastomotic leakage (28.0% versus 16.6%, p = 0.001) and Clavien Dindo grade 3a or higher (45.3% versus 26.0%, p < 0.001). The length of stay on intensive care unit (median 3 days versus 2 days, p = 0.0005) and in-hospital (median 15 days versus 12 days, p < 0.0001) were longer for the hybrid laparoscopic RAMIE group.
Conclusions
Hybrid laparoscopic RAMIE and full RAMIE were oncologically equivalent with a potential decrease of postoperative complications and shorter (intensive care) stay after full RAMIE.
Keywords: Robot-assisted minimally invasive esophagectomy, RAMIE, Hybrid laparoscopic approach, Propensity-score matching, Perioperative outcome, Complications
Oncological esophagectomy is a key component of curative treatment for resectable esophageal cancer and can be performed as a combination of open, laparoscopic/thoracoscopic and robot-assisted surgery [1–3]. Over the years, minimally invasive esophagectomy and especially robot-assisted minimally invasive esophagectomy (RAMIE) have gained in popularity, possibly allowing technical and postoperative advantages [4–8]. To date, research on the added value of a robotic system for esophagectomy has mainly focused on the thoracic phase while the added value of the robotic system during the abdominal phase has rarely been studied [9]. Most surgeons perform the abdominal phase laparoscopically or via laparotomy [10]. Moreover, the decision to be operated via a fully robotic or only partially robotic approach may depend on multiple patient characteristics such as body mass index and comorbidities. A recent review elaborated on the effects of robot assistance during the abdominal phase of RAMIE suggesting its non-inferiority compared to conventional laparoscopic abdominal approaches [11]. However, it remains unclear how the robot-assisted abdominal phase during RAMIE relates to laparoscopy regarding oncological safety and perioperative complications. Therefore, the aim of this study was to compare hybrid laparoscopic RAMIE to full RAMIE for patients with esophageal cancer in an international propensity-score matched cohort study.
Materials and methods
Data were acquired from the prospectively maintained database from the Upper GI International Robotic Association (UGIRA) [12]. The UGIRA group was initiated in 2017 as a worldwide group investigating robotic surgery in upper gastrointestinal cancer and provides data on perioperative care of patients who underwent robotic esophagogastric surgery. Participating centers can provide data for the UGIRA database without a minimum number of robotic procedures. This design was intentionally chosen to also compare the first robot-assisted operations which might be under the influence of a learning curve. The registry consists of 23 participating centers and the UGIRA study group has a central institutional review board approval at the University Medical Center of Utrecht (17/837). For each participating center local ethical approval was either obtained or waived by the local ethical committee. The research proposal was reviewed by the scientific committee of UGIRA and was approved. This paper follows to the STROBE guidelines for observational cohort studies [13].
Patients, procedures and tumor entity
All patients of the UGIRA group who underwent full RAMIE and hybrid laparoscopic RAMIE for esophageal cancer between 2017 and 2021 were included. Full RAMIE consists of both a robot-assisted abdominal phase and a robot-assisted thoracic phase while the hybrid laparoscopic group consists of a laparoscopic abdominal phase and a robot-assisted thoracic phase. In this study, only procedures with curative intention and intrathoracic anastomosis (Ivor-Lewis) were included. One essential inclusion criterion defined adenocarcinoma or squamous cell carcinoma as acceptable tumor entities based on the preoperative histology during primary diagnosis. However, final histopathology could eventually differentiate other tumor entities such as mixed adenoneuroendocrine carcinoma (MANEC), poorly differentiated carcinoma or small cell carcinoma as well (named as other tumor entities).
Outcomes
The primary endpoint was postoperative complications according to Clavien Dindo grade 3a or higher. Secondary endpoints were intraoperative adverse events, in-hospital mortality, postoperative complications, and oncological outcomes including radical resection (R0) rates and lymph node yield. The eighth TNM edition was used for both clinical and pathological TNM stage. The definition of the College of American Pathologists was used for radical resection (i.e., no tumor cells within the resection margins).
Statistical analysis
Data management, missingness imputation and propensity-score matching (PSM) were all realized via Python 3.9 [14] within the integrated development environment of Visual Studio Code (Version 1.59). Patients who underwent full RAMIE were compared to patients who underwent hybrid laparoscopic RAMIE. To account for missing data, case-specific and variable-specific missingness of more than 25% was excluded. Eventually, the overall rate of missing data in the whole dataset was calculated as 2.0% which is widely accepted as a legitimate threshold for imputation. We performed multiple imputations with n = 1000 iterations via Iterative Imputer from Sci–kit learn [15]. After multiple imputation, a propensity-score matching analysis was performed via the Python package pymatch (adapted from the R package Matching [16]) to reduce the effect of known confounders to a minimum. As potential confounders, all variables were utilized which were available before surgery and which were considered as potentially relevant for the decision to either belong to the full RAMIE or hybrid laparoscopic RAMIE group. Through logistic regression, a propensity-score was calculated for each patient based on the selected characteristics displayed in Table 1. Matched study groups were created using nearest-neighbor one-to-one matching without replacement. A threshold of 0.001 was calculated to prevent poor matches after optimizing the threshold and simultaneous maximization of retained proportion according to the overlap of both groups (demonstrated in Fig. 1). After matching, the further comparison between full RAMIE and hybrid laparoscopic RAMIE was performed using Chi2-square tests for binary data, Mann–Whitney U test for ordinal data and student’s t-test for continuous data. A p-value of less than 0.05 was considered as statistically significant. StataSE Version 15.0 (by StataCorp LLC, College Station, TX) was eventually used for final statistical analysis after matching.
Table 1.
Preoperative variables used for propensity-score matching
| Parameter | Before matching | p-value | After matching | p-value |
|---|---|---|---|---|
|
1. Hybrid laparoscopic RAMIE 2. Full RAMIE |
n = 319 n = 488 |
n = 296 n = 296 |
||
|
Age at diagnosis - Hybrid laparoscopic RAMIE - Full RAMIE |
Mean (95%-CI) 64.2 (63.2–65.2) 64.5 (63.6–65.4) |
0.6308 (t-test) |
Mean (95%-CI) 64.5 (63.5–65.5) 64.2 (63.1–65.3) |
0.7593 (t-test) |
|
Gender - Hybrid laparoscopic RAMIE - Full RAMIE |
Female (%) 55 (17.2) 98 (20.1) |
0.314 (χ2-test) |
Female (%) 62 (20.9%) 51 (17.2%) |
0.744 (χ2-test) |
|
Body mass index (in kg/m2) - Hybrid laparoscopic RAMIE - Full RAMIE |
Mean (95%-CI): 26.5 (26.0–27.0) 26.1 (25.7–26.5) |
0.2942 (t-test) |
Mean (95%-CI): 25.7 (25.2–26.1) 26.2 (25.7–26.7) |
0.1213 (t-test) |
|
ASA score - Hybrid laparoscopic RAMIE - ASA 1 - ASA 2 - ASA 3 - ASA 4 - Full RAMIE - ASA 1 - ASA 2 - ASA 3 - ASA 4 |
n (%) 28 (8.8) 207 (64.9) 83 (26.0) 1 (0.3) 29 (5.9) 252 (51.6) 203 (41.6) 4 (0.8%) |
< 0.0001 (U-test) |
n (%) 9 (3.0) 177 (59.8) 108 (36.5) 2 (0.7) 22 (7.4) 175 (59.1) 98 (33.1) 1 (0.3) |
0.1155 (U-test) |
|
cT-status - Hybrid laparoscopic RAMIE - cT1a/b - cT2 - cT3 - cT4a/b - Full RAMIE - cT1a/b - cT2 - cT3 - cT4a/b |
n (%) 46 (9.4) 94 (19.3) 324 (66.4) 24 (4.9) 29 (9.1) 57 (17.9) 227 (71.2) 6 (1.9) |
0.8984 (U-test) |
n (%) 19 (6.4) 58 (19.6) 214 (72.3) 5 (1.7) 26 (8.8) 59 (19.9) 196 (66.2) 15 (5.1) |
0.8383 (U-test) |
|
cN-status - Hybrid laparoscopic RAMIE - cN0 - cN1 - cN2 - cN3 - Full RAMIE - cN0 - cN1 - cN2 - cN3 |
n (%) 99 (31.0) 178 (55.8) 39 (12.2) 3 (0.9) 186 (38.1) 238 (48.8) 53 (10.9% 11 (2.3) |
0.1026 (U-test) |
n (%) 116 (39.2) 142 (48.0) 35 (11.8) 3 (1.0) 106 (35.8) 153 (51.7) 31 (10.5) 6 (2.0) |
0.5870 (U-test) |
|
cMX-status - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 8 (2.5) 9 (1.8) |
0.521 (χ2-test) |
Yes (%) 6 (2.0) 3 (1.0) |
0.314 (χ2-test) |
| Parameter | Before matching | P-value | After matching | P-value |
|---|---|---|---|---|
|
1. Hybrid laparoscopic RAMIE 2. Full RAMIE |
n = 319 n = 488 |
n = 296 n = 296 |
||
|
Year of esophagectomy - Hybrid laparoscopic RAMIE - 2017 - 2018 - 2019 - 2020 - 2021 - Full RAMIE - 2017 - 2018 - 2019 - 2020 - 2021 |
n (%) 51 (16.0) 80 (25.1) 141 (44.2) 37 (11.6) 10 (3.1) 124 (25.4) 155 (31.8) 125 (25.6) 75 (15.4) 9 (1.8) |
0.0006 (U-test) |
n (%) 69 (23.3) 69 (23.3) 124 (41.9) 28 (9.5) 6 (2.0) 68 (23.0) 97 (32.8) 84 (28.4) 43 (14.5) 4 (1.4) |
0.3264 (U-test) |
|
Neoadjuvant therapy - Hybrid laparoscopic RAMIE - No neoadjuvant therapy - Radiochemotherapy - Chemotherapy alone - Other - Full RAMIE - No neoadjuvant therapy - Radiochemotherapy - Chemotherapy alone - Other |
n (%) 35 (11.0) 220 (69.0) 60 (18.8) 4 (1.25) 110 (22.5) 255 (52.3) 115 (23.6) 8 (1.64) |
0.2049 (U-test) |
n (%) 24 (8.1) 219 (74.0) 49 (16.6) 4 (1.4) 61 (20.6) 158 (53.4) 74 (25.0) 3 (1.0) |
0.4625 (U-test) |
|
Cardiological comorbidities - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 94 (26.8) 131 (29.5) |
0.417 (χ2-test) |
Yes (%) 84 (28.4) 77 (26.0) |
0.518 (χ2-test) |
|
Diabetes - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 42 (13.2) 71 (14.5) |
0.580 (χ2-test) |
Yes (%) 45 (15.2) 45 (15.2) |
1.000 (χ2-test) |
|
Neurological comorbidities - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 23 (7.2) 29 (5.9) |
0.473 (χ2-test) |
Yes (%) 17 (5.7) 18 (6.1) |
0.862 (χ2-test) |
|
History of malignant disease - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 16 (5.0) 46 (9.4) |
0.021 (χ2-test) |
Yes (%) 23 (7.8) 23 (7.8) |
1.000 (χ2-test) |
|
Pulmonary comorbidities - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 43 (13.5) 79 (16.2) |
0.294 (χ2-test) |
Yes (%) 46 (15.5) 45 (15.2) |
0.909 (χ2-test) |
|
Vascular comorbidities - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 93 (29.2) 167 (34.2) |
0.132 (χ2-test) |
Yes (%) 96 (32.4) 93 (31.4) |
0.791 (χ2-test) |
|
Other comorbidities - Hybrid laparoscopic RAMIE - Full RAMIE |
Yes (%) 77 (24.1) 143 (29.3) |
0.107 (χ2-test) |
Yes (%) 89 (30.1) 87 (29.4) |
0.857 (χ2-test) |
Significant values (p < 0.05) are given in bold
RAMIE robot-assisted minimally invasive esophagectomy, 95%-CI = 95% confidence interval, ASA American society of anesthesiologists
Fig. 1.
Overlap of data points with propensity-score plotted against data availability (see A). The augmentation of the PSM threshold does not necessarily lead to higher case numbers which is why a threshold of 0.001 was chosen with a retained proportion of > 80% (see B)
Results
Study population
A total of 807 patients underwent Ivor-Lewis esophagectomy and were included for propensity-score matching. Table 1 summarizes all preoperative variables which were used for logistic regression to achieve propensity-score matching. Several parameters such as ASA score (p < 0.0001), year of esophagectomy (p = 0.0002) and history of malignant disease (p = 0.021) were significantly different between groups before matching. Figure 1A shows the overlap of patients in both groups (full RAMIE versus hybrid laparoscopic RAMIE) with their propensity-score plotted on the x-axis. To maximize data similarity, propensity-score matching was eventually performed with an average accuracy of the score of 65.11% based on the selected preoperative variables. In Fig. 1B, the threshold is depicted in relation to the retained proportion of cases. Finally, 296 patients were matched for each group. The last two columns of Table 1 demonstrate the frequency distributions and test statistics of both matched groups with all parameters not showing any significant differences.
Hybrid laparoscopic RAMIE versus full RAMIE
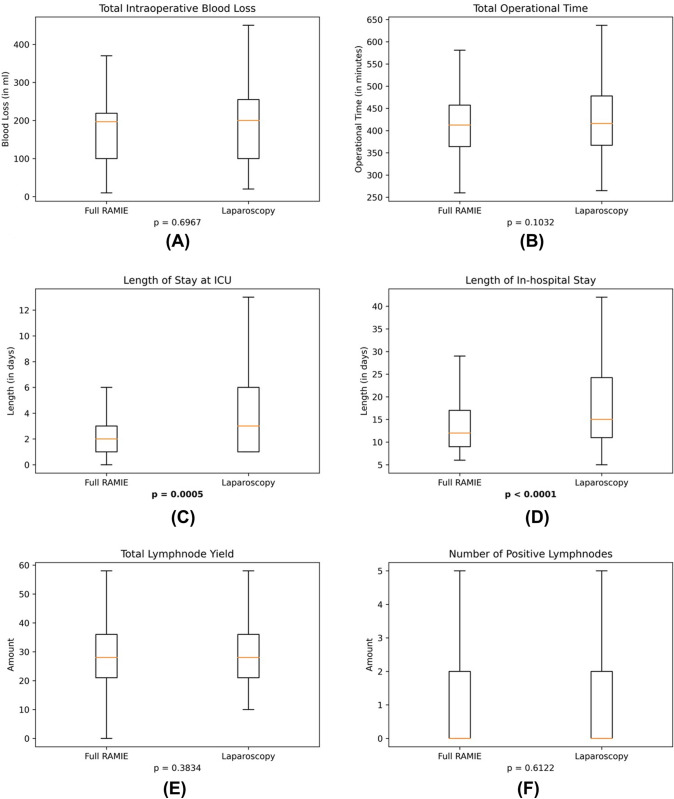
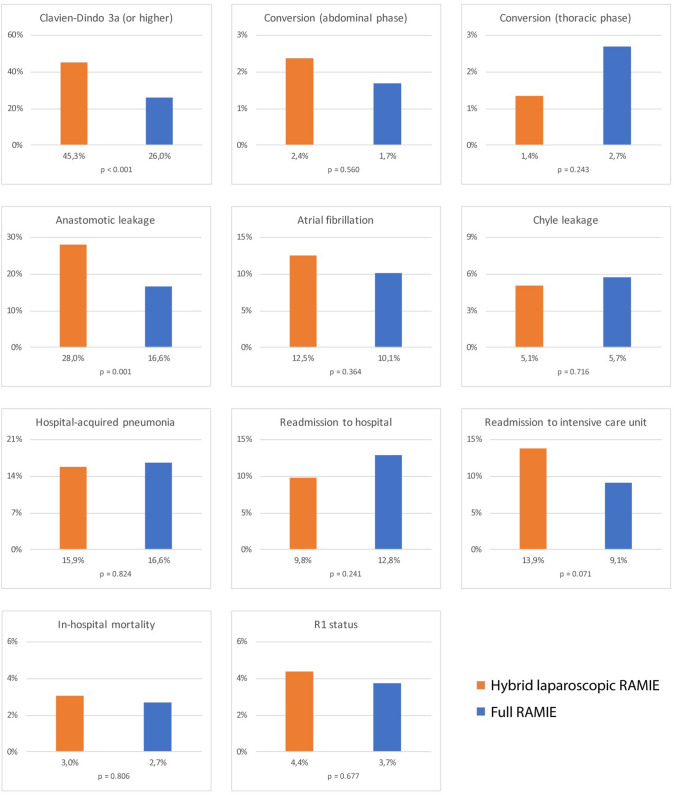
Table 2 demonstrates all outcome variables and test statistics for both full RAMIE and hybrid laparoscopic RAMIE. Figure 2 shows all continuous outcome variables represented as box plots.
Table 2.
Intraoperative and postoperative outcome variables with according test statistics after propensity-score matching of both groups hybrid laparoscopic RAMIE and full RAMIE
| Parameter | Hybrid laparoscopic RAMIE (n = 296) |
Full RAMIE (n = 296) |
p-value |
|---|---|---|---|
|
Intraoperative blood loss (in ml) |
Median (IQR): 200.0 (100.0–260.0) |
Median (IQR): 197.0 (100.0–219.0) |
0.6967 (t-test) |
|
Operational time (in minutes) |
Mean (95%-CI): 430.3 (420.7–439.9) |
Mean (95%-CI): 417.7 (406.0–429.4) |
0.1032 (t-test) |
|
Surgical technique - Circular stapler - Linear stapler - Hand-sewn |
n (%) 139 (47.0) 64 (21.6) 93 (31.4) |
n (%) 173 (58.5) 26 (8.8) 97 (32.8) |
0.0953 (U-test) |
|
Anastomosis type - End-to-side - End-to-end - Side-to-side |
n (%) 217 (73.3) 12 (4.1) 67 (22.6) |
n (%) 212 (71.6) 57 (19.3) 27 (9.1) |
0.5366 (U-test) |
|
Conversion to open surgery During abdominal phase |
Yes (%): 7 (2.4) |
Yes (%): 5 (1.7) |
0.560 (χ2-test) |
|
Conversion to open surgery during thoracic phase |
Yes (%): 4 (1.4) |
Yes (%): 8 (2.7) |
0.243 (χ2-test) |
|
Length of stay ICU (in days) |
Median (IQR): 3 (1–6) |
Median (IQR): 2 (1–3) |
0.0005 (t-test) |
|
Length of in-hospital stay (in days) |
Median (IQR): 15 (11–25) |
Median (IQR): 12 (9–17) |
< 0.0001 (t-test) |
|
Tumor histology - Adenocarcinoma - Squamous cell carcinoma - Others |
n (%) 250 (84.5) 37 (12.5) 9 (3.0) |
n (%) 225 (76) 65 (22.0) 6 (2.0) |
0.0145 (U-test) |
| Total lymph node yield |
Mean (95%-CI): 30.4 (29.0–31.7) |
Mean (95%-CI): 29.5 (28.0–30.9) |
0.3834 (t-test) |
| Positive lymph nodes |
Median (IQR): 0 (0–2) |
Median (IQR): 0 (0–2) |
0.6122 (t-test) |
| R1 status |
Yes (%) 13 (4.4%) |
Yes (%) 11 (3.7%) |
0.677 (χ2-test) |
| Parameter | Hybrid laparoscopic RAMIE (n = 296) |
Full RAMIE (n = 296) |
p-value |
|---|---|---|---|
| Anastomotic leakage |
Yes (%): 83 (28.0) |
Yes (%): 49 (16.6) |
0.001 (χ2-test) |
| Clavien Dindo grade ≥ 3a |
Yes (%): 134 (45.3) |
Yes (%): 77 (26.0) |
< 0.001 (χ2-test) |
|
Highest Clavien Dindo grade - Grade 0 - Grade 1 - Grade 2 - Grade 3a - Grade 3b - Grade 4 - Grade 5 |
n (%) 85 (28.7) 24 (8.11) 53 (17.9) 80 (27.0) 23 (7.8) 22 (7.4) 9 (3.0) |
n (%) 141 (47.6) 24 (8.1) 54 (18.2) 36 (12.2) 23 (7.8) 10 (3.4) 8 (2.7) |
< 0.0001 (U-test) |
| Readmission to ICU |
Yes (%): 41 (17.5) |
Yes (%): 27 (11.2) |
0.071 (χ2-test) |
| Readmission to hospital |
Yes (%): 29 (9.8) |
Yes (%): 38 (13.2) |
0.241 (χ2-test) |
| Hospital-acquired pneumonia |
Yes (%): 47 (15.9) |
Yes (%): 49 (16.6) |
0.824 (χ2-test) |
| Atrial fibrillation |
Yes (%): 37 (12.5) |
Yes (%): 30 (10.1) |
0.364 (χ2-test) |
| Chyle leakage |
Yes (%): 15 (5.1) |
Yes (%): 17 (5.7) |
0.716 (χ2-test) |
| In-hospital mortality |
Yes (%) 9 (3.0) |
Yes (%) 8 (2.7) |
0.806 (χ2-test) |
Significant values (p < 0.05) are given in bold
ICU intensive care unit, IQR interquartile range, 95%-CI 95% confidence interval
Fig. 2.
Box plots for continuous outcome parameters: Significant differences were found for length of stay on ICU (see C, p = 0.0005) and for total length of in-hospital stay (see D, p < 0.0001). Box plots for A total intraoperative blood loss, B total operational time, C length of stay on ICU, D length of in-hospital stay, E total lymphnode yield, F number of positive lymphnodes. ICU intensive care unit
Intraoperative parameters such as blood loss (p = 0.6967) and operational time (p = 0.1032) were not significantly different between both groups. Median intraoperative blood loss was measured as 200 ml for hybrid laparoscopic RAMIE and as 197 ml for full RAMIE. Mean operational time was averaged 430.3 min for hybrid laparoscopic RAMIE compared to 417.7 min for full RAMIE. Significant differences could be found for the length of stay (LOS) on intensive care unit (median LOS of 3 days for hybrid laparoscopic RAMIE versus 2 days for full RAMIE, p = 0.0005) and total in-hospital stay (median LOS of 15 days versus 12 days, p < 0.0001) (Fig. 3)
Fig. 3.
Bar graphs of binary outcome parameters: Significant differences were found for complications according to Clavien Dindo grade 3a or higher (p < 0.001) and anastomotic leakage (p = 0.001). RAMIE robot-assisted minimally invasive esophagectomy
Oncological outcome parameters such as radical resection (R0) rates (95.6% for hybrid laparoscopic RAMIE versus 96.3% for full RAMIE, p = 0.8526) and total lymph node yield (mean 30.4 for hybrid laparoscopic RAMIE versus 29.5 for full RAMIE, p = 0.3834) were comparable between both groups. Likewise, the number of positive lymph nodes in the final histopathology did not differ between both groups (median 0 for both RAMIE groups, p = 0.6122). The conversion rate to open surgery during the abdominal phase was 2.4% in the hybrid laparoscopic RAMIE group compared to 1.7% in the full RAMIE group (p = 0.560). During the thoracic phase open surgery occurred in 1.4% of hybrid laparoscopic RAMIE cases and in 2.7% of full RAMIE cases (p = 0.243).
Postoperative complications with Clavien Dindo grade 3a or higher appeared more frequently in the hybrid laparoscopic RAMIE group (45.3% versus 26.0%, p < 0.001). This is confirmed via the U-test for the most severe Clavien Dindo grade reported for the individual patients (p < 0.0001). The overall postoperative complication rate was also higher in the hybrid laparoscopic RAMIE group (65.2% versus 48.3%, p < 0.001), including specific complications such as anastomotic leakage (28.0% versus 16.6%, p = 0.001). Readmission rates either to intensive care unit (17.5% for hybrid laparoscopic RAMIE versus 11.2% for full RAMIE, p = 0.071) or to hospital (9.8% versus 13.2%, p = 0.241) did not differ significantly between both groups. The rate of hospital-acquired pneumonia after surgery also did not differ between both groups (15.9% for hybrid laparoscopic RAMIE versus 16.6% for full RAMIE, p = 0.824).
Discussion
This propensity-score matched analysis compared hybrid laparoscopic RAMIE to full RAMIE and suggests that full RAMIE may be superior in terms of overall postoperative complications according to Clavien Dindo grade 3a or higher. A significantly lower percentage of anastomotic leakage was observed after full RAMIE as opposed to the hybrid laparoscopic RAMIE group. In addition, the length of in-hospital stay after full RAMIE was significantly shorter than after hybrid laparoscopic RAMIE. Oncological outcomes (such as radical resection rates or lymph node yield) and intraoperative parameters including operation time were equal for both procedures.
To date, only few studies have focused specifically on the abdominal phase by comparing full RAMIE with hybrid laparoscopic RAMIE [17–20]. For instance, a retrospective multicenter study by Grimminger et al. compared 175 full RAMIE procedures to 67 hybrid (either laparoscopic or open laparotomy) RAMIE procedures and demonstrated that full RAMIE was associated with significantly lower postoperative complications including anastomotic leakage and respiratory failure [20]. Since there is not much evidence in the current literature, it is necessary to reflect on potential benefits of the robotic abdominal approach. Thus, shorter operation times after full RAMIE and a more precise dissection and reduction in surgical trauma of the gastric conduit could theoretically lead to less complications such as anastomotic leakage of the esophagogastrostomy [20–22]. On the other hand, financial expenses of a robotic system and its maintenance are often debated. It has been shown that hybrid laparoscopic RAMIE can be performed with comparable costs in comparison to full RAMIE in the setting of a high-volume European medical center [23]. If robotic assistance does truly lead to a decrease in postoperative complications, it is thinkable that costs could be saved on the long run regarding avoidable time and resources during intensive care and postoperative course [24].
Concerning the limitations of this study, it is to state that the retrospective design based on the UGIRA database may not respect standardized operational steps of the participating centers (such as the implementation of a feeding jejunostomy during the abdominal phase). Similarly, the acquisition of data regarding abdominal lymph node yield and operational time during the abdominal phase is heterogeneously available with a significant missingness due to different approaches by the centers. As another important limitation, it is necessary to discuss a potential learning curve effect leading to the concordant result that a robot-assisted abdominal phase might be superior to laparoscopy during RAMIE. It is very likely that a learning curve effect is involved in the hybrid laparoscopic RAMIE group. A robotic system is generally implemented in the thoracic phase at first place, and after completing the learning curve for the thoracic phase the robotic system may also be implemented for the abdominal phase. Hence, it may be possible that the full RAMIE cases included in this analysis were more frequently performed by a team that has more robotic experience. Consequently, it may be possible that the hybrid laparoscopic RAMIE group consists of procedures performed by surgeons who are undergoing the learning curve for RAMIE. According to the current literature, the learning curve for RAMIE is generally completed after 45–70 cases with the possibility of being shortened by following a structured training pathway that involves proctoring, and modular approaches may help to further reduce time to proficiency [25–28]. On the other hand, there is also a learning curve for the robot-assisted abdominal phase, although only few studies have dealt with this question and allegedly found a plateau phase after 14–22 cases [29, 30]. Moreover, the learning curve for non-robotic total MIE has also been reported to be relatively high with 119 cases [31]. The effect of the learning curve may be significant for the results of the presented study since the UGIRA registry holds data from centers that are yet in their learning curve. Anyhow, in order to solely compare the robot-assisted abdominal phase to laparoscopy a cohort without a learning curve effect is needed. In this way, only cases after completion of the learning curve for both the thoracic as well as the abdominal phase could be included in a follow-up study. Finally, the significance of a learning curve effect during the abdominal phase has to be elucidated especially in this setting of two cavity surgery where the thoracic phase is performed robotically in any case.
A strength of this study is the fact that it includes a large and international multicenter cohort representing the real practice of specialized hospitals. The UGIRA study group offers the unique opportunity to conduct comparative studies based on standardized procedures and a rigorous selection of participating medical centers. This study also features a strong methodology with a state-of-the-art statistical implementation for data handling, missingness imputation and propensity-score matching.
The current study showed that the use of a robotic system in the abdominal phase during RAMIE achieves comparably good postoperative outcomes. The study suggests that the implementation of a robotic system during the abdominal phase is safe without compromising histopathological results. In the future, it is inevitable to perform prospective and randomized studies investigating whether full RAMIE is truly superior to hybrid laparoscopic RAMIE regarding complications and long-term expenses.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for this study.
Declarations
Disclosures
Drs. Richard van Hillegersberg, Peter P Grimminger and Jelle P Ruurda are consultants for Medtronic and proctors for Intuitive Surgical. Drs. Daniel Perez and Marc J van Det are proctors for Intuitive Surgical. Dr. Mark I van Berge Henegouwen is consultant for Mylan, Johnson & Johnson, Alesi Surgical, B. Braun, Medtronic, and received unrestricted research grants from Stryker (all fees paid to institution). Dr. Yin-Kai Chao is consultant for Intuitive Surgical and received a research grant from Intuitive Surgical. Drs. Christiane J Bruns and Hans F Fuchs are both consultants for Medtronic and received an educational grant from Intuitive Surgical. Drs. Jin-On Jung, Eline M de Groot, B Feike Kingma, Benjamin Babic, Jens P Hölzen, Jan W Haveman, Philippe Rouanet, Frank Benedix, Hecheng Li, Inderpal Sarkaria, Gijs I van Boxel, Philip Chiu, Jan-Hendrik Egberts, Rubens Sallum, Arul Immanuel, Paul Turner, Donald E Low, Michal Hubka, Paolo Strignano, Matthias Biebl and M Asif Chaudry have no conflicts of interest or financial ties to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jin-On Jung and Eline M. de Groot shared first author.
Richard van Hillegersberg and Hans F. Fuchs shared last author.
References
- 1.Shapiro J, van Lanschot JJB, Hulshof MCCM, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16(9):1090–1098. doi: 10.1016/S1470-2045(15)00040-6. [DOI] [PubMed] [Google Scholar]
- 2.Schröder W, Gisbertz SS, Voeten DM, Gutschow CA, Fuchs HF, van Berge Henegouwen MI. Surgical therapy of esophageal adenocarcinoma–current standards and future perspectives. Cancers (Basel) 2021;13(22):5834. doi: 10.3390/cancers13225834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babic B, Schiffmann LM, Schröder W, Bruns CJ, Fuchs HF. Evidence in minimally invasive oncological surgery of the esophagus. Chirurg. 2021;92(4):299–303. doi: 10.1007/s00104-020-01337-x. [DOI] [PubMed] [Google Scholar]
- 4.Haverkamp L, Seesing MFJ, Ruurda JP, Boone J, van Hillegersberg R. Worldwide trends in surgical techniques in the treatment of esophageal and gastroesophageal junction cancer. Dis Esophagus. 2017;30(1):1–7. doi: 10.1111/dote.12480. [DOI] [PubMed] [Google Scholar]
- 5.Straatman J, Van Der Wielen N, Cuesta MA, et al. Minimally invasive versus open esophageal resection. Ann Surg. 2017;266(2):232–236. doi: 10.1097/SLA.0000000000002171. [DOI] [PubMed] [Google Scholar]
- 6.van der Sluis PC, van der Horst S, May AM, et al. Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer: a randomized controlled trial. Ann Surg. 2019 doi: 10.1097/SLA.0000000000003031. [DOI] [PubMed] [Google Scholar]
- 7.Mariette C, Markar SR, Dabakuyo-Yonli TS, et al. Hybrid minimally invasive esophagectomy for esophageal Cancer. N Engl J Med. 2019;380(2):152–162. doi: 10.1056/NEJMoa1805101. [DOI] [PubMed] [Google Scholar]
- 8.Horgan S, Berger RA, Elli EF, Espat NJ. Robotic-assisted minimally invasive transhiatal esophagectomy. Am Surg. 2003;69(7):624–626. doi: 10.1177/000313480306900716. [DOI] [PubMed] [Google Scholar]
- 9.Na KJ, Park S, Park IK, Kim YT, Kang CH. Outcomes after total robotic esophagectomy for esophageal cancer: a propensity-matched comparison with hybrid robotic esophagectomy. J Thorac Dis. 2019;11(12):5310–5320. doi: 10.21037/jtd.2019.11.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dolan DP, Swanson SJ. The modern approach to esophagectomy—review of the shift towards minimally invasive surgery. Ann Transl Med. 2021;9(10):901–901. doi: 10.21037/ATM.2020.03.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Groot EM, Goense L, Ruurda JP, van Hillegersberg R. State of the art in esophagectomy: robotic assistance in the abdominal phase. Updates Surg. 2021;73(3):823–830. doi: 10.1007/s13304-020-00937-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kingma BF, Grimminger PP, van der Sluis PC, et al. Worldwide techniques and outcomes in robot-assisted minimally invasive esophagectomy (RAMIE) Ann Surg. 2020 doi: 10.1097/sla.0000000000004550. [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 14.Van Rossum G, Drake FL. (2009) Python 3 Reference Manual. Scotts Val CA Creat. Published online
- 15.Pedregosa F, Varoquaux G, Gramfort A, et al. Scikit-learn: machine learning in python. J Mach Learn Res. 2011;12(85):2825–2830. [Google Scholar]
- 16.Sekhon JS. Multivariate and propensity score matching software with automated balance optimization: the matching package for R. J Stat Softw. 2011;42(7):1–52. doi: 10.18637/jss.v042.i07. [DOI] [Google Scholar]
- 17.Deng HY, Luo J, Li SX, et al. Does robot-assisted minimally invasive esophagectomy really have the advantage of lymphadenectomy over video-assisted minimally invasive esophagectomy in treating esophageal squamous cell carcinoma? A propensity score-matched analysis based on short-term. Dis Esophagus. 2019 doi: 10.1093/dote/doy110. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Han Y, Gan Q, et al. Early outcomes of robot-assisted versus thoracoscopic-assisted ivor lewis esophagectomy for esophageal cancer: a propensity score-matched study. Ann Surg Oncol. 2019;26(5):1284–1291. doi: 10.1245/s10434-019-07273-3. [DOI] [PubMed] [Google Scholar]
- 19.Yang Y, Zhang X, Li B, et al. Short- and mid-term outcomes of robotic versus thoraco-laparoscopic McKeown esophagectomy for squamous cell esophageal cancer: a propensity score-matched study. Dis Esophagus. 2020 doi: 10.1093/dote/doz080. [DOI] [PubMed] [Google Scholar]
- 20.Grimminger PP, Staubitz JI, Perez D, et al. Multicenter experience in robot-assisted minimally invasive esophagectomy—a comparison of hybrid and totally robot-assisted techniques. J Gastrointest Surg. 2021;25(10):2463–2469. doi: 10.1007/s11605-021-05044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laméris W, Eshuis WJ, Cuesta MA, Gisbertz SS, van Berge Henegouwen MI. Optimal mobilization of the stomach and the best place in the gastric tube for intrathoracic anastomosis. J Thorac Dis. 2019;11:S743–S749. doi: 10.21037/jtd.2019.01.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang Y, Li B, Yi J, et al. Robot-assisted versus conventional minimally invasive esophagectomy for resectable esophageal squamous cell carcinoma. Ann Surgdoi. 2021 doi: 10.1097/sla.0000000000005023. [DOI] [PubMed] [Google Scholar]
- 23.Urbanski A, Babic B, Schröder W, et al. New techniques and training methods for robot-assisted surgery and cost-benefit analysis of Ivor Lewis esophagectomy. Chirurg. 2021;92(2):97–101. doi: 10.1007/s00104-020-01317-1. [DOI] [PubMed] [Google Scholar]
- 24.Goense L, van Dijk WA, Govaert JA, van Rossum PSN, Ruurda JP, van Hillegersberg R. Hospital costs of complications after esophagectomy for cancer. Eur J Surg Oncol. 2017;43(4):696–702. doi: 10.1016/j.ejso.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 25.van der Sluis PC, Ruurda JP, van der Horst S, Goense L, van Hillegersberg R. Learning curve for robot-assisted minimally invasive thoracoscopic esophagectomy: results from 312 cases. Ann Thorac Surg. 2018;106(1):264–271. doi: 10.1016/j.athoracsur.2018.01.038. [DOI] [PubMed] [Google Scholar]
- 26.Sarkaria IS, Rizk NP, Grosser R, et al. Attaining proficiency in robotic-assisted minimally invasive esophagectomy while maximizing safety during procedure development. Innov Technol Tech Cardiothorac Vasc Surg. 2016;11(4):268–273. doi: 10.1097/IMI.0000000000000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.FeikeKingma B, Hadzijusufovic E, van der Sluis PC, et al. A structured training pathway to implement robot-assisted minimally invasive esophagectomy: the learning curve results from a high-volume center. Dis Esophagus. 2020 doi: 10.1093/dote/doaa047. [DOI] [PubMed] [Google Scholar]
- 28.Fuchs HF, Müller DT, Leers JM, Schröder W, Bruns CJ. Modular step-up approach to robot-assisted transthoracic esophagectomy-experience of a German high volume center. Transl Gastroenterol Hepatol. 2019 doi: 10.21037/tgh.2019.07.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang H, Chen L, Wang Z, et al. The learning curve for robotic Mckeown esophagectomy in patients With esophageal cancer. Ann Thorac Surg. 2018;105(4):1024–1030. doi: 10.1016/j.athoracsur.2017.11.058. [DOI] [PubMed] [Google Scholar]
- 30.Berlth F, Mann C, Uzun E, et al. Technical details of the abdominal part during full robotic-assisted minimally invasive esophagectomy. Dis Esophagus. 2020 doi: 10.1093/dote/doaa084. [DOI] [PubMed] [Google Scholar]
- 31.Van Workum F, Stenstra MHBC, Berkelmans GHK, et al. Learning curve and associated morbidity of minimally invasive esophagectomy: a retrospective multicenter study. Ann Surg. 2019;269(1):88–94. doi: 10.1097/SLA.0000000000002469. [DOI] [PubMed] [Google Scholar]