Abstract
Extraosseous osteosarcoma is a rare malignant soft tissue neoplasm, and extraosseous osteosarcoma of the parotid gland is very rare. It has a very aggressive course, and there are no standardized treatment guidelines. We report the case of a 20 year old male patient who presented with history of right neck swelling since 6 years for which he had undergone right parotid surgery 5 years ago. The final histopathological report indicated that the mass was a pleomorphic adenoma. One year after the first surgery, the patient experienced recurrence of swelling over the operated site, and the size of the swelling has been increasing gradually since then. He was evaluated clinically, and a large mass was noted over the upper aspect of the right upper neck, extending to the occipital and parotid regions. An MRI scan was done which showed a 12 × 10 × 8 cm lesion centred in the right parotid gland, involving paraspinal muscles, C1–C2 vertebrae and extending into the parapharyngeal space. FNAC of the lesion showed features of pleomorphic adenoma. The patient underwent a complete excision of the tumour. The patient’s post-operative period was uneventful. The final histopathological report of the patient was extraosseous osteosarcoma of the parotid gland. The patient was referred for adjuvant radiotherapy. He has been on regular follow-up for the past 6 months and has shown no sign of recurrence. EOS is an extremely rare tumour of the head and neck region which often requires extensive surgical resection with or without adjuvant radiotherapy. It has a high rate of local recurrence and a very low disease free survival. Such patients should be kept on a close follow-up.
Keywords: Extraskeletal osteosarcoma, Extraosseous osteosarcoma, Parotid gland cancer
Introduction
Osteosarcoma is the most common malignancy of bone, commonly seen in extremities. Only 10% cases of osteosarcomas are diagnosed in the head and neck region [1]. Extraosseous osteosarcoma is a separate term used to describe a very rare and aggressive malignant tumour accounting for less than 1% of soft tissue sarcomas and are extremely rare in the head and neck region [2].
Case report
A 20 year old male patient presented to us with a history of right sided parotid swelling for the past 6 years. He had undergone right superficial parotidectomy/enucleation of mass 5 years ago for the same, the complete surgical details were not available with the patient. The final histopathology report was pleomorphic adenoma. One year after the first surgery the patient had recurrence of swelling over the operated site which has been slowly progressing in size and has reached the current size over the past 3 years.
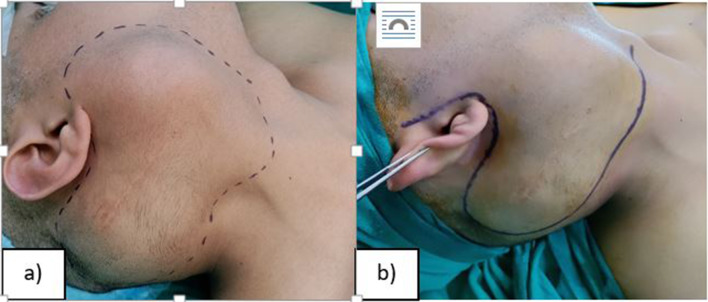
On clinical examination, a large firm mass was identified over the right parotid measuring about 10 × 8 cm extending to upper neck ( levels II–III ) inferiorly, anteriorly upto the anterior border of parotid gland, posteriorly to the occipital region, superiorly upto the level of tragus, intraorally the mass was seen pushing the tonsillar pillars medially (Fig. 1). Facial nerve functions were intact. Fibreoptic laryngoscopy was done which showed a normal study with mobile vocal cords. Gag reflex of the patient was intact. Examination of all cranial nerves was normal.
Fig. 1.
a dotted marker indicating the extent of the mass clinically on lateral view. b surgical incision marking
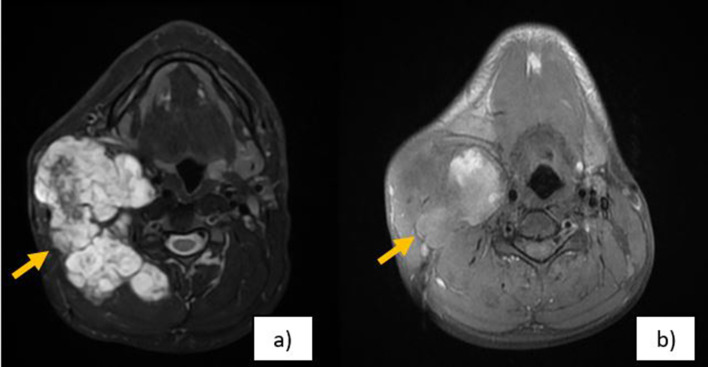
A magnetic resonance imaging (MRI) showed 12 × 10 × 8 cm large heterogeneous mass lesion with central cystic, non enhancing areas centred in the right parotid gland involving both superficial and deep lobes, with extension into masseter space and right parapharyngeal space reaching upto C1–C2 vertebrae levels with possible involvement of the same. Right internal carotid artery was seen draping over the medial part of the lesion and was also displaced medially but with preserved signal flow void. Anteriorly the mass was seen abutting pterygoid muscle, posteriorly seen extending into the posterior triangle and right paraspinal muscles, reaching upto midline (Figs. 2, 3 and 4) and caudally it was reaching just below submandibular gland. An FNAC was performed and the report suggested features of pleomorphic adenoma of right parotid gland.
Fig. 2.
a MRI with contrast axial image. b, c MRI plain axial image. Images showing a right parotid mass involving both superficial and deep lobes with extension to C1–C2 vertebral levels
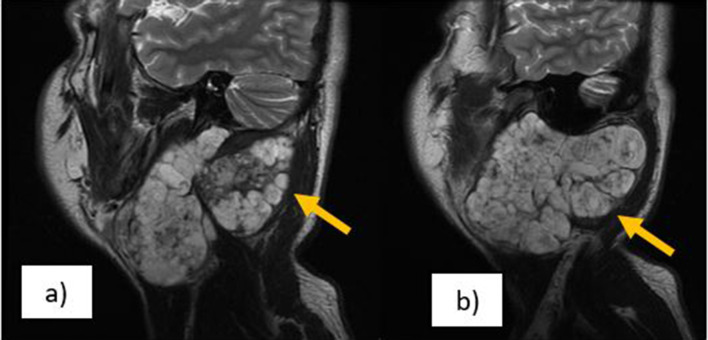
Fig. 3.
a MRI coronal with contrast. b MRI coronal plain. Images showing a right parotid mass involving the Paraspinal muscles, extending to parapharyngeal space
Fig. 4.
a, b MRI sagittal with contrast mass centred in parotid extending to C1–C2 transverse process
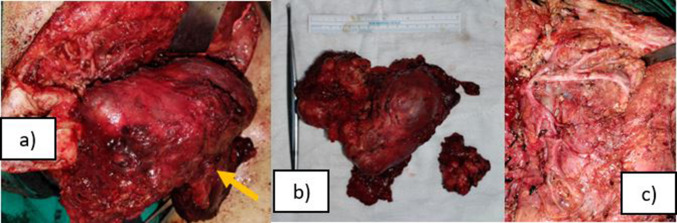
The surgical excision comprised of a total conservative parotidectomy with ligation of external carotid artery and included a wide margin of soft tissue excision which comprised of the muscles of prevertebral, parapharyngeal and retropharyngeal space. Possible lysis was noted over C1–C2 vertebrae levels which was chiselled out after consultation with a spine specialist and excision margins were widened intraoperatively. Facial nerve and all its branches were preserved. (Fig. 5)
Fig. 5.
a large mass visualised partly dissected out with the facial nerve partially seen over the bed. b 10 × 8 cm well encapsulated mass along with a 4 × 5 cm hard lesion removed separately. c Post operative bed showing all branches of facial nerve intact
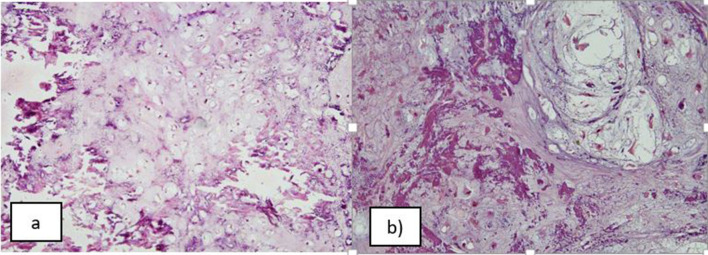
Final histopathological examination showed chondroblastic extraosseous osteosarcoma with osteoid and chondroid matrix arranged in an atypical formation. (Fig. 6) Immunohistochemistry was negative for cytokeratin. The post-operative course was uneventful and patient was referred for radiotherapy. Follow up scans done after 6 months did not indicate any evidence of residual or recurrent disease.
Fig. 6.
a Haematoxylin and eosin stained section, 100x: shows a tumour composed of lobules of chondrocytic cells within lacunae; left half of the image shows presence of osteoid matrix. b Haematoxylin and eosin stained section, 200X: Higher magnification shows chondroid areas containing tumour cells in lacunar spaces that are intimately associated with osteoid matrix (darker pink) present in the left half of the image
Discussion
Extraosseous osteosarcoma of the head and neck region is extremely rare and only 15 cases have been reported in available literature out of which 9 cases were seen arising from the parotid gland (Table 1).
Table 1.
– Reported cases of extraosseous osteosarcoma in head and neck
| Luna- Ortiz et al. [2] | Manning JT et al. [3] | Hatano et al. [4] | Saito et al. [5] | Stimson et al. [6] | Kosec et al. [7] | Adeyemo et al. [8] | Huang EC et al. [9] | Hamamoto et al. [10] | Xin Ge et al. [11] | Zhang et al. [12] | Aslan et al. [13] | Our case | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 74 | 73 | 25 | 17 | 63 | 48 | 46 | 62 | 47 | 51 | 81 | 69 | 20 |
| Gender | Female | Male | Male | Male | 3 male and 1 female | Female | Male | Male | Male | Male | Male | Male | Male |
| Localization | Right submandibular region | Parotid gland | Right mandibular angle | Left submandibular region | Parotid | Right neck | Parotid | Parotid | Parotid gland | Parotid gland | Right neck subcutaneous tissue | Parapharyngeal space | Parotid |
| Tumour diameter (cm) | 12 | 3 | 1.5 | 6.5 | 3–6 | 6 | 16 | 6 | 6 | 4 | 4 | 5 | 12 |
| Follow up | Died within 1 year | Lost to follow up | Disease free – 2 years | Died within 1 year | 3 died of metastatic disease within 2 years, 1 was lost to follow up | Died of metastatic disease after 1 year | Disease free – 4 months | Died due to metastatic disease in 6 months | Died due to metastatic disease in 17 months | Died due to local recurrence and distant metastasis in 13 months | Disease free – 2 years | Disease free – 6 months | Disease free after 6 months |
| Treatment | Surgery and palliative radiotherapy | Surgery | Surgery and chemoradiotherapy | Surgery and chemoradiotherapy | Surgery | Surgery | Surgery and chemoradiotherapy | Surgery and chemoradiotherapy | Surgery and raditherapy | Surgery and chemotherapy | Multiple surgeries with radiotherapy | Surgery and chemotherapy | Surgery and radiotherapy |
The tumour often mimics a reactive lymph node or benign disease as was in the case of our patient. Other differential diagnosis includes myositis ossificans, calcified lymph nodes associated with granulomatous inflammatory disease and pilomatricoma [6]. It has been reported that trauma and radiotherapy are possible inducing agents for extraosseous osteosarcoma [10].
Previous data have shown that FNAC or biopsy cannot produce a reliable diagnosis, with excisional biopsy remaining the gold standard in confirming the diagnosis [14]. Previous reports have also stated that 25% of the cases appeared encapsulated on gross examination, but on histopathologic examination, all of the tumours penetrated their pseudocapsule and infiltrated the adjacent structures [15]. Histological types include osteoblastic, chondroblastic, fibroblastic, osteoclastic, telangiectatic and small cell forms [3].
Existing data on extraosseous osteosarcoma have emphasized the importance of timely surgical intervention with adjuvant radiotherapy [16]. Recent studies have shown that 88% of reported cases have locally advanced disease (Stage III) according to American Joint Committee on Cancer staging system and 50% cases develop recurrence following surgical resection with wide margins [17]. Tumour diameter of more than 5 cm is an independent poor prognostic factor which directly affects the rate of recurrence in extraosseous osteosarcoma [2]. One report does suggest surgery combined with a chemotherapy (doxorubicin, cisplatin, and ifosfamide etc.) regimen was used to treat EOS, thereby giving a higher survival rate [18]. For parotid EOS, nevertheless, postoperative chemoradiotherapy have not shown any benefits in survival rates till date [10].
The 5 year disease specific survival rates range from 25 to 46% mostly because of the invasive local recurrence and pulmonary metastasis occurring in first post-operative year in 60% patients. Chemotherapy treatment has shown very limited success in 13–15% patients [7]. Due to the rarity of EOS in the head and neck region, it is difficult to obtain a sufficient sample size to evaluate clinicopathological characteristics of this disease and devise evidence-based treatment strategies. Further study is therefore warranted, especially with respect to adjuvant treatment.
Conclusion
Extraosseous osteosarcoma is an extremely rare malignancy that encompasses less than 1% of head and neck soft tissue sarcomas. It is difficult to diagnose as it is usually labelled as a benign tumour in its early stages and often requires extensive resection with wide margins. It has a very high rate of local recurrence and very low disease free survival rates.
Acknowledgements
I would like to acknowledge the efforts of the department of robotics and surgical oncology, department of radiology and pathology of BLK—MAX Superspeciality hospital.
Funding
None.
Data Availability
All material submitted in the article are original.
Declarations
Conflict of interest
No potential conflict of interest relevant to this article exist.
Informed Consent
Written and informed consent has been taken from the patient for the procedure and all procedures have been done ethically.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Clark L, Unni KK, Dahlin DC. Osteosarcoma of the jaw. Cancer. 1983;51:2311. doi: 10.1002/1097-0142(19830615)51:12<2311::AID-CNCR2820511224>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 2.Luna-Ortiz K, Ortega-Gutierrez C, Dominguez-Malagon H, et al. Extraosseous osteosarcoma in the neck. Auris Nasus Larynx. 2012;39:333. doi: 10.1016/j.anl.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Manning JT, Raymond AK, Batsakis JG. Extraosseous osteogenic sarcoma of the parotid gland. J Laryngol Otol. 1986;100(2):239–242. doi: 10.1017/S0022215100099059. [DOI] [PubMed] [Google Scholar]
- 4.Hatano H, Morita T, Kobayashi H, et al. Extraskeletal osteosarcoma of the jaw. Skeletal Radiol. 2005;34:171. doi: 10.1007/s00256-004-0797-3. [DOI] [PubMed] [Google Scholar]
- 5.Saito Y, Miyajima C, Nakao K, et al. Highly malignant submandibular extraskeletal osteosarcoma in a young patient. Auris Nasus Larynx. 2008;35:576. doi: 10.1016/j.anl.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Stimson PG, Valenzuela-Espinoza A, Tortoledo ME, et al. Primary osteosarcoma of the parotid gland. Oral Surg Oral Med Oral Pathol. 1989;68:80. doi: 10.1016/0030-4220(89)90119-9. [DOI] [PubMed] [Google Scholar]
- 7.Kosec A, Vucic M, Bedekovic V, Ivkic M. Osteoblastic Extraosseous Osteosarcoma of the Neck. J Oral Maxillofac Surg. 2016;75(3):e1–1.e5. doi: 10.1016/j.joms.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Adeyemo A, Ameye SA. A rare case of extraosseous osteosarcoma of parotid gland. East Central Afr J Surg. 2016;21(2):100–105. [Google Scholar]
- 9.Huang EC, Ghazikhanian V, Qian X. Giant cell-rich osteosarcoma of the parotid gland: an exceptionally rare entity at an unusual site. Diagn Cytopathol. 2016;44(12):1107–1111. doi: 10.1002/dc.23563. [DOI] [PubMed] [Google Scholar]
- 10.Hamamoto T, Kono T, Furuie H, et al. Extraskeletal osteosarcoma in the parotid gland: a case report. Auris Nasus Larynx. 2018;45(3):644–647. doi: 10.1016/j.anl.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Ge X, Wang M, Zhai X, (2022) Extraskeletal Osteosarcoma in the parotid gland a case report and review of literature. Eur J Med Res, DOI: 10.21203/rs.3.rs-1511384/v2
- 12.Zhang JS, Wen G, Liu Y, Wu ZH, Chen GD, Wang H, Zhou TC. Extraskeletal osteosarcoma in right neck subcutaneous tissue: A case report of an extremely rare tumour. Mol Clin Oncol. 2018;9(2):149–154. doi: 10.3892/mco.2018.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aslan M, Samdanci ET. A very rare mass mimicking paraganglioma in the parapharyngeal area: extraskeletal osteosarcoma. Braz J Otorhinolaryngol. 2022;88:279–282. doi: 10.1016/j.bjorl.2020.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nicol KK, Ward WG, Savage PD, et al. Fine-needle aspiration biopsy of skeletal versus extraskeletal osteosarcoma. Cancer. 1998;84:176. doi: 10.1002/(SICI)1097-0142(19980625)84:3<176::AID-CNCR10>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 15.Bane BL, Evans HL, Ro JY, et al. Extraskeletal osteosarcoma. a clinic-pathologic review of 26 cases. Cancer. 1990;65:2762. doi: 10.1002/1097-0142(19900615)65:12<2762::AID-CNCR2820651226>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad SA, Patel SR, Ballo MT, et al. Extraosseous osteosarcoma: response to treatment and long-term outcome. J Clin Oncol. 2002;20:521. doi: 10.1200/JCO.2002.20.2.521. [DOI] [PubMed] [Google Scholar]
- 17.Edge SB, Byrd DR, Compton CC, et al. AJCC Cancer Staging Manual. New York: Springer; 2010. [Google Scholar]
- 18.Longhi A, Bielack SS, Grimer R, et al. Extraskeletal osteosarcoma: a European musculoskeletal oncology society study on 266 patients. Eur J Cancer. 2017;74:9–16. doi: 10.1016/j.ejca.2016.12.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All material submitted in the article are original.