Abstract
Operation theatre (OT) time utilisation rates can be improved with an assessment of the procedure time that will result in effective scheduling of cases. Our study is the first of its kind to audit the amount of OT time required for a particular surgery in lip and oral cavity cancers, depending on the various components of this complex procedure. This prospective cross-sectional study, based on an operative room database of 323 OT sessions, was conducted in the Department of Surgical Oncology at a tertiary care centre on lip and oral cancer patients from January 1st, 2019 to December 31st, 2020. Various components of the surgery, like the primary site, operating surgeon, type of neck dissection, bone resection, and reconstructive procedure, were noted. The time of entry and exit of the patient from the OT was noted. Operative time and OT time utilisation rates were calculated. SPSS 21.0 statistical tool; Students ‘T’, ANOVA and Games-Howell tests were applied. In 323 OT sessions, while 303 surgeries were done for primary cases (93.8%), the remaining 20 cases were for recurrent cases (6.2%). Buccal mucosa and the floor of the mouth were the most and least common sites, respectively. The mean OT time was 212.42 ± 73.83 min, the maximum being the primary at alveolus. The mean OT late start time was 70.03 ± 23.41 min and the mean OT runover time was 37.62 ± 43.53 min. The mean time varied significantly with the type of neck dissection, bone resection, and reconstructive surgery done and the operating surgeon. The mean OT time was highest for free flap reconstructive surgery (328.71 ± 62.02 min), but it didn’t vary with its type. Considering only the lip and oral cancer surgeries, the OT time utilisation rate was 57.1%. Assessment and quantification of the operative duration of lip and oral cancer surgeries will help in accurate prediction of surgical duration, better OT list planning, and thus improved OT time utilisation rate. Our research not only provides data on the historical mean of procedures, but it may also encourage other centres to adopt our quantitative approach to OT scheduling.
Keywords: Operating time, Surgical scheduling, Theatre efficiency, Head and neck cancers, Operation theatre utilization, Audit
Introduction
The operating theatre (OT) is a human resource-intensive area equipped with sophisticated, specialized, and costly equipment [1]. They are believed to consume a large part (> 40%) of the hospital’s annual budget [2]. Therefore, they must have a level of productivity that is commensurate with this level of expenditure in a sense similar to that of industrial plants [3]. In order to reduce the cost associated with health care, hospital management often identifies OT as a potential target for cost containment efforts. Efficiency of use of OT time depends on scheduling of cases, allocation of staff, equipment, time required for preparation and induction of anaesthesia, performance of surgery, recovery from anaesthesia, preparation of the OT for the next patient, and other resources [4]. “OT time utilization” is an important tool for the optimal functioning of the OT. “OT time utilization” was defined by Donham and colleagues as the quotient of hours of OT time actually used during elective resource hours and the actual number of elective resource hours available for use [5].
As per the Global Burden of Disease Study, head and neck cancers represent 5.3% of all cancers, and among them, lip and oral cavity (LOC) cancers were the most frequent cancers [6]. In India, among males, LOC cancers rank first both in incidence and mortality rates [7]. Recent advances in the diagnosis and management of oral cancers are not without extra financial burden, leading to the need for out-of-pocket expenditure by patients. A significant demand–supply mismatch is particularly seen in a government hospital setup, where waiting lists of long duration are the norm. This results in a significant delay in initiating treatment, which can be catastrophic as it can result not only in disease upstaging but also render the disease non-operable anymore. The increasing disease burden and resulting economic burden, coupled with poor availability of health services and a high illiteracy rate, necessitate the need for an appropriate allocation of resources by making the treatment pathways more efficient. Therefore, it is imperative on our behalf to maximally utilise the OT time allocated for LOC cancers.
There are cost implications of inefficient OT time scheduling for both patients and the hospital. Delays in surgery increase patient anxiety and cause discomfort due to intake restrictions, while postponement or rescheduling of surgery poses additional costs such as added days in the hospital and days lost from work, both by the patient and their family [8]. Underbooking and/or overbooking of an operation theatre results in inefficient OT time utilisation, OT cancellations, and OT runovers. Data suggests that while a third of the operating list may be underbooked, 10–40% of the booked elective operations may be cancelled before the surgery takes place [9].
Audits of OT time utilisation have been proven to increase the efficiency of OT utilisation [10, 11]. Both prospective [12] and retrospective [13] studies on the analysis of OT time utilisation in the past, have identified various factors that can lead to ineffective OT time utilisation, such as delays in starting the OT, delays in shifting the patient to the OT, non-availability of the anaesthesia procedure room, delays in shifting patients between two cases, and OT run-overs. In order to reduce these deficiencies in OT management, one must be able to determine the time required for a particular surgery depending on the extent of the surgery and various other factors, including the expertise of the operating surgeon. A quantitative approach to operative list scheduling by assessment of the mean operative times for a particular surgery will result not only in the better utilisation of the most valuable resource of an operation theatre, i.e., time, but also prevent overbooking, underbooking, OT cancellations, and OT over-run with a consequent reduction in overtime staff cost. Unfortunately, no studies have attempted to do so to date.
To the best of our knowledge, this is the first study of its kind in which we seek to predict the likely surgical duration of LOC cancers depending on the various components of this complex procedure and use it to improve O.T time utilisation through effective scheduling of cases in the O.T. This will also serve as a reproducible model that can be used for other surgeries and across different countries.
Material and Methods
This prospective study was conducted in the department of surgical oncology at a high-volume cancer care centre, representative of many similar cancer care hospitals across the nation, from January 1st, 2019 to December 31st, 2020. OT data pertaining to all the patients suffering from cancer of the lip and oral cavity were included in the study. The study was a part of the regular departmental audit and approval was obtained from the departmental ethical committee.
During the period of the study, usually 1 operative table was assigned daily to 1 surgery for head and neck cancer. Rarely, two operative tables were given for two cases of head and neck cancer. In that case, it was counted as two OT sessions. Only surgeries done for lip and oral cavity cancers were included in the study. Minor procedures were performed based on the available OT time after the completion of the LOC surgery, but the OT utilisation time for them was not recorded. OT was functional for 6 days a week except for the holidays. The maximum OT time allotted for the scheduled cases was 6 h per OT session.
After detailed pre-anesthetic workup and evaluation, appropriate surgical resection with or without reconstruction was planned. The extent of resection might or might not include neck dissection or bone resection. The various types of neck dissections that were done were: supra omohyoid neck dissection (SOHND), extended SOHND, modified neck dissection (MND), and radical neck dissection (RND). The various types of bone resections done were mandibulectomy, maxillectomy, and bite resection. Mandibulectomy may be marginal, segmental, or hemi-mandibulectomy. Either a partial or total maxillectomy was done. Bite resection includes en bloc resection of a portion of the mandible as well as partial upper alveolectomy, which is commonly performed in cases of RMT tumors.After the resection, either primary closure or reconstructive surgery was done. Reconstructive surgery either consists of locoregional flaps or perforator-based free flaps. The Pectoralis Major Myocutaneous (PMMC), Deltopectoral (DP), Nasolabial (NL), forehead, and platysmal flaps were among the loco-regional flaps used. Radial Forearm Free Flap (RFFF), Fibular Free Flap (FFF), and C (ALT FF) were among the perforator-based free flaps used.
For the scheduled cases, the following observations were made:
OT start time: the time of entry of the patient into the OT.
OT end time: the time of the exit of the patient from the OT.
“OT utilisation time” was the actual duration of the procedure, which was derived from the OT start time and OT end time. Also, “OT late start time” and “OT run-over time” were noted. The “OT late start time” was defined as the time difference between the start of the allotted OT hours and the “OT start time”. “OT run-over time” was defined as the time for which the surgery exceeded 6 hours of the allotted OT time. The “OT time utilisation rate” was defined as the percentage of the allotted time that was actually used for the surgical procedure, after excluding the “OT run-over time”.
[(OT utilisation time-OT run-over time)/Maximum allotted OT time] × 100 = OT time utilisation rate.
The demographic data of the patients, which included name, age, sex, diagnosis, chief operating surgeon, and other team members, was duly noted. Also, to study the effect of the level of expertise of the chief operating surgeon on the surgical duration, the surgeons were classified into 3 categories according to the designation – Surgeon A (Assistant Professor), Surgeon B (Associate Professor), and Surgeon C (Professor). From January 1, 2019 to September 10, 2019, there were no surgical trainees, and after that, they were mainly the first assistants or sometimes operated minute parts of the surgery independently, such as the skin incision, drain placement, fixation, and/or skin closure, which was assumed to have no effect on the OT time utilisation. Lastly, the details of the surgical procedure were noted, which included the type of neck dissection, type of bone resection, and type of reconstruction, if done.
Data Analysis
Data analysis was done using the SPSS Statistical tool and the Students' ‘T’ test was applied. The Anova test was applied to determine if any significant difference was present between different groups. The Games-Howell test was applied to compare and determine the value of the difference among various subgroups within a group, e.g., among various types of loco-regional flaps.
Results
Data was obtained for a total of 323 OT sessions that fulfilled our inclusion criteria during the study period. While 303 surgeries out of 323 were done for primary cases (93.8%), the remaining 20 cases were for recurrent cases (6.2%). Buccal mucosa and the floor of the mouth were the most and least common sites, respectively (Fig. 1).
Fig. 1.
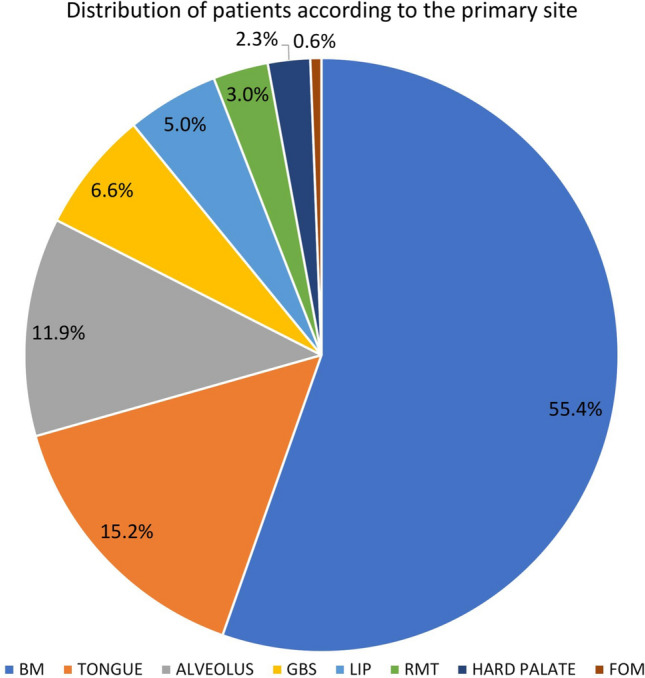
Distribution of patients according to the primary site. BM, Buccal mucosa; GBS, Gingivobuccal sulcus; RMT, Retromolar trigone; FOM, Floor of mouth
The total OT time utilised for surgeries of the lip and oral cavity cancers was 68,613 min (1143.6 h) out of the total available 116,280 min (1938 h). The mean operative time for LOC cancer was 212.42 ± 73.83 min. Leaving 9 OT sessions, all the remaining 314 OT sessions had a delay in starting the operative table of more than 30 min after the scheduled OT start time. The mean OT late start time was 70.03 ± 23.41 min, ranging from as low as 20 min to as high as 145 min. The total OT late start time was 20,658 min, which was 17.77% of the total maximum allotted time. On 51 occasions, the OT ran for more than the stipulated time of 6 h. The mean OT run-over time was 37.62 ± 43.53 min, the range being 5–185 min. The total OT run-over time was 2220 min. After excluding the time for which the OT was overrun, the total and mean “Effective OT utilisation time” was 66,393 min (1106.6 h) and 205.58 ± 64.25 min, respectively. Considering only the LOC cancers, the “Effective OT time utilisation rate” was calculated to be 57.1%.
Table 1 shows the mean OT utilisation time according to the primary site. The difference in the mean OT utilisation time for the primary and recurrent cases was insignificant (213.11 ± 73.69 min vs 202 ± 77.12 min, p = 0.9). The mean OT utilisation time was maximum for the primary tumour at alveolus (255.13 ± 81.98 min) and least for the tongue (158.73 ± 74.32 min), the difference being statistically significant (p < 0.05).
Table 1.
Mean OT utilisation time according to the site of primary
| Site of primary | Mean OT utilisation time (mins) |
|---|---|
| Alveolus | 255.13 ± 81.98 |
| Buccal mucosa | 222.6 ± 64.30 |
| Floor of mouth | 210 ± 35.35 |
| Gingivobuccal sulcus | 238.20 ± 71.01 |
| Hard palate | 159.70 ± 43.53 |
| Lip | 181.33 ± 77 |
| Retromolar trigone | 184.70 ± 35.5 |
| Tongue | 158.73 ± 74.32 |
| Recurrent cases | 202 ± 77.12 |
Table 2 shows the distribution of the mean OT utilisation time according to various surgical variables. The mean OT time utilised per surgery for three categories of chief operating surgeons—A, B, and C—was 200.55 ± 68.97 min, 229.04 ± 82.99 min, and 230.17 ± 62.93 min, respectively. It was noted that the maximum number of cases were operated by surgeon A (n = 190, 58.8%). The differences in the mean OT utilisation time were statistically significant when comparing surgeon A with surgeon B (p = 0.013) or surgeon A with surgeon C (p = 0.029), but statistically insignificant when comparing surgeon B with surgeon C (p = 0.996). One or the other sort of neck dissection was done in 295 patients (91.33%) with a mean OT utilisation time of 216.07 ± 73.36 min, which reduced to 174.03 ± 68.82 min in 28 cases where neck was not addressed. The mean OT utilisation time was highest for MND and least when Ext SOHND was done (234.64 ± 68.92 min v/s 161.78 ± 78.99 min, p = 0.021). It was interesting to note that, though insignificantly, the mean OT utilisation time was higher for SOHND than for Ext SOHND (164.79 ± 56.09 min v/s 161.78 ± 78.99 min, p = 0.99). Similarly, the mean OT utilisation time for RND, which was done in a total of 16 cases (5%), was 191.56 ± 68.86 min, which was insignificantly less than that of MND (234.64 ± 68.92 min, p = 0.112), which was done in 65.3% of patients (n = 211). The mean OT utilisation time was significantly higher in 221 cases (68.4%) undergoing bone resection as compared to 102 cases (31.6%) where bone resection was not done (235.4 ± 94.96 min v/s 162.64 ± 67.3 min, p = 0.001). Mandibulectomy was the most commonly performed bone resection (n = 200, 61.9%) and bite resection was the least commonly performed bone resection (n = 8, 2.5%), with mean OT utilisation times of 238.24 ± 64.43 min and 226.5 ± 29.6 min, respectively. The mean OT utilisation time in cases undergoing maxillectomy was 197.31 ± 78.97 min. On subgroup analysis of the maxillectomy group, the difference in the mean OT utilisation time between partial maxillectomy (n = 9, 69.23%) and total maxillectomy (n = 4, 30.77%) subgroups was insignificant (199.44 ± 94.71 min v/s 192.5 ± 31.22 min, p = 1.000). On subgroup analysis of mandibulectomy group, the findings revealed significant differences only when the segmental mandibulectomy subgroup was compared with others – hemimandibulectomy (p = 0.015), marginal madibulectomy (p = 0.003), bite resection (p = 0.012) and maxillectomy (p = 0.008). There was no significant difference found when comparing all other subgroups among themselves.
Table 2.
Distribution of Mean OT utilisation time according to various surgical variables
| Variable | Mean OT utilisation time (mins) | |||||
|---|---|---|---|---|---|---|
| Surgeon | A (n = 190, 58.8%) | 200.55 ± 68.97 | ||||
| B (n = 94, 29.1%) | 229.04 ± 82.99 | |||||
| C (n = 39, 12.1%) | 230.17 ± 62.93 | |||||
| Neck dissection | Not done (n = 28, 8.7%) | 174.03 ± 68.82 | ||||
| Done (n = 295, 91.33%) | SOHND (n = 54, 16.7%) | 164.79 ± 56.09 | 216.07 ± 73.36 | |||
| Ext SOHND (n = 14, 4.3%) | 161.78 ± 78.99 | |||||
| MND (n = 211, 65.3%) | 234.64 ± 68.92 | |||||
| RND (n = 16, 5.0%) | 191.56 ± 68.86 | |||||
| Bone resection | Not done (n = 102, 31.6%) | 162.64 ± 67.3 | ||||
| Done (n = 221, 68.4%) | Mandibulectomy (n = 200, 61.9%) | Marginal (n = 21, 6.5%) | 214.52 ± 55.24 | 238.24 ± 64.43 | 235.4 ± 94.96 | |
| Segmental (n = 16, 5%) | 296.25 ± 61.41 | |||||
| Hemi (n = 163, 50.5%) | 235.6 ± 62.94 | |||||
| Maxillectomy (n = 13, 4%) | Partial (n = 9, 2.8%) | 199.44 ± 94.71 | 197.31 ± 78.97 | |||
| Total (n = 4, 1.2%) | 192.5 ± 31.22 | |||||
| Bite resection (n = 8, 2.5%) | 226.5 ± 29.6 | |||||
SOHND: Supraomohyoid neck dissection; MND: Modified neck dissection; RND: Radical neck dissection
Table 3 depicts the distribution of mean OT utilisation time based on the type of reconstructive procedure performed. Loco-regional flap reconstruction was the most commonly performed procedure, done in 73.4% of the patients (n = 237). The difference in the mean OT utilisation time between a locoregional and a free flap reconstruction was found to be statistically significant (p < 0.001). While PMMC was the most commonly done loco-regional flap (n = 176, 74.3%), platysmal flap reconstruction was the least commonly done procedure (n = 3, 1.3%). Leaving the estlander flap, there was a significant difference in the mean OT utilisation time between the PMMC flap and all the other loco-regional flaps, namely the nasolabial flap (p < 0.001), the forehead flap (p = 0.032) and the platysmal flap (p = 0.044). There was no statistically significant difference in the mean OT utilisation time among any of the other loco-regional flap subgroups. Out of the total 31 patients undergoing free flap reconstructive procedures, FFF reconstruction was the most commonly performed free flap reconstructive procedure (n = 22, 70.97%). The differences in the mean OT utilisation time between the RFFF and FFF (p = 0.144), RFFF and ALT FF (p = 0.917), and FFF and ALT FF (p = 0.953) were all found to be statistically insignificant.
Table 3.
Distribution of Mean OT utilisation time according to the reconstructive procedure
| Type of reconstructive surgery | Mean OT utilisation time (mins) | ||
|---|---|---|---|
| Not done (n = 55, 17%) | 135.18 ± 43.43 | ||
| Loco-regional flaps (n = 237, 73.4%) | PMMC (n = 176, 54.5%) | 230.10 ± 53.69 | 215.14 ± 57.82 |
| Nasolabial (n = 45, 13.9%) | 175.44 ± 47.75 | ||
| Forehead (n = 8, 2.5%) | 180.62 ± 35.90 | ||
| Platysma (n = 3, 0.9%) | 156.67 ± 18.93 | ||
| Estlander (n = 5, 1.5%) | 136 ± 56.94 | ||
| Free flaps (n = 31, 9.6%) | RFFF (n = 6, 1.9%) | 292.5 ± 46.66 | 328.71 ± 62.02 |
| FFF (n = 22, 6.8%) | 339.77 ± 56.98 | ||
| ALT FF (n = 3, 0.9%) | 320 ± 113.02 | ||
PMMC, Pectoralis Major Myocutaneous; RFFF, Radial Forearm Free Flap; FFF, Fibular Free Flap; ALTFF, Fibular Free Flap
Discussion
An accurate case duration estimate, which is a performance parameter for OT scheduling, is defined as the percentage of cases where patient-in-room duration is within 15 min of the estimated in-room duration [4]. Despite several studies [14, 15] aimed at determining methods to accurately estimate surgical duration, there is still no clear consensus.There are two ways of OT scheduling cases: with a stochastic estimation of procedure duration, or based on measurable data from the team, such as the duration of specific procedures, historical performance (delays), available technology, local structure, and the ability to solve adverse events [16]. In many institutions [9, 17, 18], surgical scheduling is the responsibility of the surgical team and does not adhere to any fixed algorithm. Estimation of operative time by a surgeon is a non-reproducible subjective evaluation that lacks accountability and often results in more frequent unforeseen events [19]. Dexter and Macario showed that a simple average of the past 39 durations of an operation, combined with surgeons’ mean estimates for that operation, yields a good measure of future operating times [20]. At present, there are only a handful of studies [21, 22] aimed at quantitative scheduling of the operative list using the mean surgical duration of the individual surgeries. The same observation regarding the paucity of data on surgical duration was also made by Abouleish et al. [23]. In our study, we seek to objectify the process of O.T. scheduling by planning cases based on objective mean data. While doing so, we also identified some potential areas of further improvement.
While 93.8% of LOC surgeries were performed for primary cancers, 6.2% of those were recurrent ones. This is a considerable figure, keeping in mind the fact that the majority of the recurrent tumours of the lip and oral cavity are inoperable or metastatic at presentation, making them rarely amenable to surgery. Buccal mucosa was the most common site, seen in 55.4% of patients, mainly due to the customary consumption of smokeless tobacco by chewing tobacco and then keeping it in between the buccal mucosa and teeth for a prolonged duration.
There was an insignificant difference between the mean O.T utilisation time for the primary and recurrent cases, despite the additional neck dissection to be done in the primary cases. This extra time for neck dissection in primary cases is balanced by the increased difficulty of operating in recurrent cases, owing to the loss of surgical planes, the presence of dense adhesions, the presence of trismus, etc. The mean O.T time utilisation was highest for the primary site, the alveolus, and lowest for the primary site, the tongue. This is attributable to the fact that the majority of the tongue cancer cases are present at an early stage, where after resection, which itself is not that complex, no reconstruction is needed and the raw area is left open to heal over time. Also, in the case of carcinoma of the alveolus, some sort of bone resection is mandatory, which is then followed by a complex reconstructive surgery, thus requiring more time for surgery. Among other factors, the duration of surgery also depends on the surgeon’s skill [24]. Some studies have demonstrated that the procedure time varies with a particular surgeon or anaesthetist [25, 26]. In our study, surgeon A’s mean operative time was significantly shorter than that of both surgeons B and C. However, it is important to note that approximately 66% of the surgeries were operated by surgeon A, and hence it is believed that frequent exposure and more surgical experience, particularly in head and neck surgeries, might be the reason for this difference. There was no statistically significant difference between the mean O.T time utilisation time of all the 323 surgeries and the 190 surgeries performed by surgeon A. This implies that when the mean duration of all the surgeries is taken into account, variations arising due to the surgeon’s skill should be contemplated.
The mean time required for surgery was the maximum when MND was done and the minimum when SOHND was done. This is elucidated by the simple fact that SOHND is done in early cases and MND is done in advanced cases. Therefore, the more radical a surgery becomes, the more time it requires to perform it. However, contrary to the above mentioned dictum, the surgical duration in RND cases was less, albeit insignificantly, than in MND cases. This is because, in MND, we have to identify and preserve various vital structures, which requires meticulous dissection and extra time to do so. The maximum duration of surgery was seen in cases where segmental mandibulectomy was done. On subgroup analysis, statistically significant differences were seen only when comparing the segmental mandibulectomy group with all others. This was an unexpected finding, but on analysing further, it was found that in 12 of the 16 segmental mandibulectomy cases, reconstruction was done by the free flap tissue transfer method, which is a time-consuming and complex reconstructive procedure. As expected, the mean surgical duration was significantly higher in the free flap reconstruction group when compared to the locoregional flap reconstruction group. However, no significant differences were found among the three types of free flap reconstruction procedures. The mean operative time was significantly higher for the PMMC subgroup when compared to other locoregional flaps except the estlander flaps. The PMMC flap is more exhaustive and technically demanding than other locoregional flaps, and the PMMC flap reconstruction is required in advanced cases where other flaps cannot suffice. Also, the increased operative time in cases where estlander flap reconstruction was done might be due to the estlander flap being the least commonly done flap at our centre, hence the lack of experience demanding more time.
The mean OT utilisation time for the surgery of lip and oral cancer was 212.42 ± 73.83 min (3 h and 32 min). Only 59% of the allotted OT time was utilised for LOC cancers, and the rest was used for other minor surgeries. In their study, Vinukondaiah et al. [27] reported a mean operative time of 10 h and 31 min per OT session, which was 91.5% of the total allotted operative time. Haiart et al. [28] showed an OT utilisation time of 77.1% and reported understaffing as the main reason for underutilization. As per the literature, an OT utilisation rate of 70–80% is realistic, which can also make up for longer than expected operative duration due to intraoperative complications [29, 30]. Though the OT utilisation rate in our study is not the actual utilisation rate, considering the fact that the remaining OT time was used for minor surgeries, the time for which was not taken into account, we do agree that utilising only 59% of the allotted time for head and neck surgeries is unsatisfactory. We firmly believe that scheduling the OT list precisely after predicting the operative time using the operative means from our current study would surely help to improve the OT utilisation rate. In a study comprising 8093 procedures, the operative duration estimation improved by 39 min per procedure when the historical operative means were used to predict the operative time [16]. In a setting where surgical time estimation was done, the OT utilisation rate was found to be as high as 93.8% [31]. It would not be wrong to implicate delayed OT starts as a significant contributor to the underutilization of the operative room. In our study, the total OT late start time constituted approximately 18% of the total allotted time and the mean OT late start time was approximately 70 min, with an OT late start rate of 97.2%, which is an alarming figure and represents a potential target area of insufficiency. Though, not a primary aim of our study, we identified the late transfer of patients from the ward to OT, the unavailability of the anaesthesia procedure room, understaffing, issues with patient fitness, the late arrival of consultant doctors, and technical issues with OT equipment as the main factors. Vinukondaiah et al. [27] reported that 43.6% of the OT lists had delayed starts, and the late transfer of the patients to the OT was the leading cause in 80% of the cases. Similar to our study, several other studies have reported OT late start rates as high as 90–100% [32–34]. Overrunning of the OT also adds to the operating room inefficiency. In our study, in approximately 16% of the OT sessions, the OT list overran, with a mean OT runover time of approximately 38 min. Barr et al. [35] reported a similar OT list runover rate of 21%. Deepti et al. [32] in their study reported a high OT runover rate of 90% and a mean OT runover time of 111.04 min. Delayed OT starts, unexpected intraoperative complications, delays in readiness of operative equipment, delays during recovery from anesthesia, and delays in shifting the patient out of the OT are some of the factors contributing to the OT runover. When Broka et al. used mean operative times in OT list planning [17], they reported a decrease in the OT runover rate from 26 to 12%.Proper communication between the ward and the OT personnel, use of an anaesthesia procedure room, coordinated teamwork, personal accountability, identifying and addressing the avoidable causes, and regular audits of the surgical pathway are the key factors that may not only help to reduce the OT delayed starts and OT runovers but also improve the OT efficiency.
The results of our study will not only help to create a disease-driven paradigm shift in the management of lip and oral cancers but also aid in the cost accounting of the surgery. This factor is gaining importance in the modern era with the introduction of “Payment-By-Results” in the National Health Service [36]. Data from our study will help in precise OT list planning and thus improve the OT utilisation rate. A particular strength of our study is that we have taken into account the total duration of the procedure, as the anaesthesia time and the OT ready time also vary with the complexity of the procedure. Our study does have certain limitations. As ours is a teaching hospital, the trainees were involved in both the anaesthesia and surgical pathways, and it would be better to study the effects of both the trainees on the operative times. Where Eappen et al. [37] reported no effect of anaesthesia residents on the anaesthesia timings, Urman et al. [38] showed that the anaesthesia residents in the OTs result in non-delayed OT starts but increased induction and emergence times. Also, our study is on elective surgeries, and whether the same model can be used for emergency surgeries is also unknown and warrants further studies.
To conclude, our objective model of OT list planning based on mean operative times will help with more efficient OT list planning, improved OT utilisation rates, and decreased OT runover rates. We also came to the conclusion that a regular audit also helps to identify certain potential areas of inefficiency and adequate measures can thus be taken to address the same. The data and results from our study can also act as a template for other surgeries across different countries.
Author contributions
RJ: Concept, Design, Literature search, Writing; PP: Concept, Analysis and/or interpretation; KKL: Analysis and/or interpretation; C: Literature search, Writing; SS: Supervision, Critical review. RGS: Critical review, Supervision.
Funding
No funding was received to assist with the preparation of this manuscript.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Human and animal rights
The research involved human Participants and a well informed consent was taken from each individual. Departmental ethical clearance was obtained. The study was a part of the regular departmental audit.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rohit Jindal, Email: doc_rj24@yahoo.com.
Pinakin Patel, Email: drpinakinp@gmail.com.
Kamal Kishor Lakhera, Email: drkk.bhu@gmail.com.
Chanchal Gulati, Email: chanchal.chanchal1993@gmail.com.
Suresh Singh, Email: drsureshsingh@gmail.com.
Raj Govind Sharma, Email: rajgovindsharma@gmail.com.
References
- 1.Lewis MA, Hall RD, Okolo S, Yoong W. How time flies: a prospective analysis of theatre efficiency during elective gynaecology lists. Gynecol Surg. 2012;9(2):213–217. doi: 10.1007/s10397-011-0696-2. [DOI] [Google Scholar]
- 2.Denton B, Viapiano J, Vogl A. Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Manag Sci. 2007;10:13–24. doi: 10.1007/s10729-006-9005-4. [DOI] [PubMed] [Google Scholar]
- 3.O'Donnell DJ. Theatre utilization analysis. Med J Aust. 1976;2:650–651. doi: 10.5694/j.1326-5377.1976.tb98932.x. [DOI] [PubMed] [Google Scholar]
- 4.Divatia JV, Ranganathan P. Can we improve operating room efficiency? J Postgrad Med. 2015;61(1):1–2. doi: 10.4103/0022-3859.147000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donham RT, Mazzei WJ, Jones RL. Procedural times glossary. Am J Anesthesiol. 1996;23(Suppl):4–12. [Google Scholar]
- 6.Aupérin A. Epidemiology of head and neck cancers: an update. Curr Opin Oncol. 2020;32(3):178–186. doi: 10.1097/CCO.0000000000000629. [DOI] [PubMed] [Google Scholar]
- 7.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 8.Gordon T, Paul S, Lyles A, Fountain J. Surgical unit time utilization review: resource utilization and management implications. J Med Syst. 1988;12(3):169–179. doi: 10.1007/BF00996639. [DOI] [PubMed] [Google Scholar]
- 9.Pandit JJ, Tavare A. Using mean duration and variation of procedure times to plan a list of surgical operations to fit into the scheduled list time. Eur J Anaesthesiol. 2011;28(7):493–501. doi: 10.1097/EJA.0b013e3283446b9c. [DOI] [PubMed] [Google Scholar]
- 10.Saha P, Pinjani A, Al-Shabibi N, Madari S, Ruston J, Magos A. Why we are wasting time in the operating theatre? Int J Health Plann Manage. 2009;24:225–232. doi: 10.1002/hpm.966. [DOI] [PubMed] [Google Scholar]
- 11.Delaney CL, Davis N, Tamblyn P. Audit of the utilization of time in an orthopaedic trauma theatre. ANZ J Surg. 2010;80:217–222. doi: 10.1111/j.1445-2197.2009.05043.x. [DOI] [PubMed] [Google Scholar]
- 12.Talati S, Gupta AK, Kumar A, Malhotra SK, Jain A. An analysis of time utilization and cancellations of scheduled cases in the main operation theater complex of a tertiary care teaching institute of North India. J Postgrad Med. 2015;61(1):3–8. doi: 10.4103/0022-3859.147009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dinesh TA, Nair P, Jha V, et al. Utilization rate of operation theatres—its evaluation and importance. Int J Sci Res. 2018;7(11):1–2. doi: 10.1537/2249555X. [DOI] [Google Scholar]
- 14.Sanjay P, Dodds A, Miller E, Arumugam PJ, Woodward A. Cancelled elective operations: an observational study from a district general hospital. J Health Org Manag. 2007;21(1):54–58. doi: 10.1108/14777260710732268. [DOI] [PubMed] [Google Scholar]
- 15.Silber JH, Rosenbaum PR, Zhang X, Even-Shoshan O. Estimating anesthesia and surgical times from Medicare anesthesia claims. Anesthesiology. 2007;106:346–355. doi: 10.1097/00000542-200702000-00024. [DOI] [PubMed] [Google Scholar]
- 16.Costa ADS Jr Assessment of operative times of multiple surgical specialties in a public university hospital. Einstein (Sao Paulo) 2017;15(2):200–205. doi: 10.1590/S1679-45082017GS3902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Broka SM, Jamart J, Louagie YAG. Scheduling of elective surgical cases within allocated block-times: can the future be drawn from the experience of the past? Acta Chir Belg. 2003;103:90–94. doi: 10.1080/00015458.2003.11679372. [DOI] [PubMed] [Google Scholar]
- 18.Buchanan D. Representing process: the contribution of a re-engineering frame. Int J Oper Prod Manag. 1988;18:1163–1188. doi: 10.1108/01443579810236610. [DOI] [Google Scholar]
- 19.van Eijk RP, van Veen-Berkx E, Kazemier G, Eijkemans MJ. Effect of individual surgeons and anesthesiologists on operating room time. Anesth Analg. 2016;123(2):445–451. doi: 10.1213/ANE.0000000000001430. [DOI] [PubMed] [Google Scholar]
- 20.Dexter F, Macario A. Applications of information systems to operating room scheduling. Anesthesiology. 1996;85:1232–1234. doi: 10.1097/00000542-199612000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Widdison AL. Can we predict when an operating list will finish? Ann R Coll Surg. 1995;77(6 Suppl):304–306. [PubMed] [Google Scholar]
- 22.Kendell J, Wildsmith JAW, Gray IG. Costing anaesthetic practice. An economic comparison of regional and general anaesthesia for varicose vein and inguinal hernia surgery. Anaesthesia. 2000;55:1106–1113. doi: 10.1046/j.1365-2044.2000.01547.x. [DOI] [PubMed] [Google Scholar]
- 23.Abouleish AE, Dexter F, Whitten CW, Zavaleta JR, Prough DS. Quantifying net staffing costs due to longer-than-average surgical case durations. Anesthesiology. 2004;100:403–412. doi: 10.1097/00000542-200402000-00033. [DOI] [PubMed] [Google Scholar]
- 24.Costa AS, Jr, Leão LE, Novais MA, Zucchi P. An assessment of the quality indicators of operative and non-operative times in a public university hospital. Einstein (Sao Paulo) 2015;13(4):594–599. doi: 10.1590/S1679-45082015GS3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stepaniak PS, Heij C, Mannaerts GHH, de Quelerij M, de Vries G. Modeling procedure and surgical times for current procedural terminology-anesthesia-surgeon combinations and evaluation in terms of case-duration prediction and operating room efficiency: a multicenter study. Anesth Analg. 2009;109:1232–1245. doi: 10.1213/ANE.0b013e3181b5de07. [DOI] [PubMed] [Google Scholar]
- 26.Strum DP, Sampson AR, May JH, Vargas LG. Surgeon and type of anesthesia predict variability in surgical procedure times. Anesthesiology. 2000;92:1454–1466. doi: 10.1097/00000542-200005000-00036. [DOI] [PubMed] [Google Scholar]
- 27.Vinukondaiah K, Ananthakrishnan N, Ravishankar M. Audit of operation theatre utilization in general surgery. Natl Med J India. 2000;13:118–121. [PubMed] [Google Scholar]
- 28.Haiart DC, Paul AB, Griffiths JM. An audit of the usage of operating theatre time in a peripheral teaching surgical unit. Postgrad Med J. 1990;66:612–615. doi: 10.1136/pgmj.66.778.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strum DP, Vargas LG, May JH, Bashein G. Surgical suite utilization and capacity planning: a minimal cost analysis model. J Med Syst. 1997;21(5):309–322. doi: 10.1023/a:1022824725691. [DOI] [PubMed] [Google Scholar]
- 30.Faiz O, Tekkis P, McGuire A, Papagrigoriadis S, Rennie J, Leather A. Is theatre utilization a valid performance indicator for NHS operating theatres? BMC Health Serv Res. 2008;8(1):28. doi: 10.1186/1472-6963-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pandit JJ, Carey A. Estimating the duration of common elective operations: implications for operating list management. Anaesthesia. 2006;61:768–776. doi: 10.1111/j.1365-2044.2006.04719.x. [DOI] [PubMed] [Google Scholar]
- 32.Sahran D, Siddharth V, Satpathy S. Are the operation theatres being optimally utilized?—a prospective observational study in a tertiary care public sector hospital. Indian J Surg. 2019;82:407–414. doi: 10.1007/s12262-019-01980-7. [DOI] [Google Scholar]
- 33.Walsh U, Alfhaily F, Gupta R, Vinayagam D, Whitlow B. Theatre sending: how long does it take and what is the cost of late starts? Gynecol Surg. 2010;7(3):307–310. doi: 10.1007/s10397-010-0577-0. [DOI] [Google Scholar]
- 34.Oluwadiya KS, Osinaike BB, Eziyi AK, Oyebamiji EO, Kolawole IK. A theatre time utilization survey in a university teaching hospital from a developing country. J Anesth Clin Res. 2012;3(5):1–4. doi: 10.4172/2155-6148.1000210. [DOI] [Google Scholar]
- 35.Barr A, McNeilly RH, Rogers S. Use of operating theatres. Br Med J (Clin Res Ed) 1982;285(6347):1059–1061. doi: 10.1136/bmj.285.6347.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Audit Commission (2004) Introducing payment by results: getting the balance right for the NHS and taxpayers London: HMSO. https://www.gov.uk/government/publications/audit-commission-annual-report-and-accounts-2012-to-2013
- 37.Eappen S, Flanagan H, Bhattacharyya N. Introduction of anesthesia resident trainees to the operating room does not lead to changes in anesthesia-controlled times for efficiency measures. Anesthesiology. 2004;101:1210–1214. doi: 10.1097/00000542-200411000-00022. [DOI] [PubMed] [Google Scholar]
- 38.Urman RD, Sarin P, Mitani A, Philip B, Eappen S. Presence of anesthesia resident trainees in day surgery unit has mixed effects on operating room efficiency measures. Ochsner J. 2012;12:25–29. [PMC free article] [PubMed] [Google Scholar]


