Abstract
A Large pedunculated neurofibrolipoma involving the hypopharynx is a very rare entity. Patient with hypopharyngeal polyp usually presents with progressive dyaphagia, sensation of persistent lump in throat and difficulty in breathing. Regurgitation of the mass into the airway can led to fatal asphyxiation on several occasions and may rarely cause death also if not evaluated and treated timely. Malignant degeneration of these large polyps occurs infrequently. We encountered a case with similar complaints in our outpatient department. After complete clinical examination, radiological investigations and anaesthetic evaluation; patient was taken for elective tracheostomy first and subsequently followed by successful transoral endoscopic excision of hypopharyngeal polypoidal mass. The histopathological examination of mass revealed it to be a neurofibrolipoma.
Keywords: Benign tumours of hypopharynx, Fibrolipomatous hamartoma of nerve, Hypopharyngeal polyp, Lipofibromatosis of nerve, Mesenchymal tumours of pharynx, Neurofibrolipoma
Introduction
Hypopharyngeal polyps are predominantly benign in nature. They causes symptoms due to expansion and compression of the surrounding structures. Benign tumours of Upper Gastrointestinal tract are mostly mesenchymal in origin. The mucosal polyps of digestive tract are usually composed of a combination of fibrous, vascular or adipose tissue covered by intact mucosa. These are usually pedunculated polyps [1]. Neural fibrolipoma also known as fibrolipomatous hamartoma, lipomatosis of a nerve, is characterized by infiltration of the epineurium by adipose and fibrous tissue. The tissue grows between and around nerve bundles thereby causing enlargement of the affected nerve [2]. The median nerve and its digital branches are most commonly affected, followed by the ulnar nerve. It is extremely rare in hypopharynx [3]. The differential diagnosis of Fibrolipomatous Hamartoma of the Nerve arising in the neck is broad and includes benign and malignant spindle cell lesions, such as spindle cell lipoma, perineurioma, and myxoid liposarcoma [4]. Histopathologically neurofibrolipoma differs from other intraneural tumours by its characteristic fibrofatty infiltration around the nerve fascicles and concentric thickening with pseudo-onion bulb-like change in perineurium.. Unlike LFH, neurilemmomas, intraneural lipomas and intraneural ganglia do not intermingle with nerve fascicles [5]. The presenting symptoms can be dysphagia, sensation of lump in throat, regurgitation of food, weight loss and persistent cough etc. Neural fibrolipoma is a benign lesion with no effective therapy. Surgical excision may also cause severe damage of the involved nerve [6]. Resection of these lesions is warranted; it may be approached endoscopically if feasible or surgically through a cervical or thoracotomy approach, depending on the location and surgeon experience. Recurrence is rare. Malignant potential is low [7].
Case Report
A 50-year-old male presented to the outpatient department of otorhinolaryngology, Government medical college, Amritsar in September 2020 with complaint of difficulty in swallowing to both solids and liquids, progressively increased over a period of 1 year, change of voice and occasional difficulty in breathing which gradually progressed over 5 months.
Clinical Finding and Investigation
On physical examination inspiratory stridor was heard and there was no lymphadenopathy or external swelling present over the neck. On rigid 90-degree laryngoscopy, a pedunculated, globular, smooth surfaced pinkish mass was seen behind the epiglottis arising from right pyriform fossa causing indentation of the airway and appeared to be moving with respiration. The left pyriform sinus appeared to be normal. Vocal cords were not visualized. (Fig. 1) Contrast-enhanced computed tomography of the neck revealed a well-defined round to oval soft tissue density lesion in the right pyriform fossa, extending superiorly towards the laryngeal cavity abutting the right aryepiglottic fold crossing the midline, the superior aspect of aryepiglottic fold, anteriorly displacing the epiglottis and posteriorly, it was abutting the posterior pharyngeal wall. There was no infiltration or invasion, bony erosion, or significant enhancement of the surrounding structures like thyroid gland, supraglottis, glottis and infraglottis. (Fig. 2) The clinical symptoms were indicative of benign lesion and imaging findings were suggestive of a fat containing neoplasm in hypopharynx (right pyriform fossa). Based on these findings the differential diagnosis of lipoma, fibro-lipoma or its variants was made.
Fig. 1.
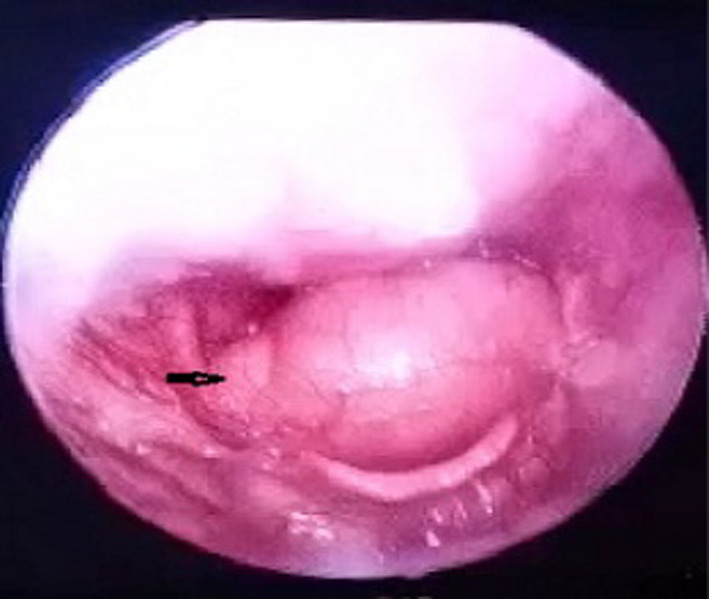
Showing a globular, smooth surfaced pink mass with pedicle (arrow) arising from right side of hypopharynx pushing the epiglottis causing considerable narrowing of the airway on rigid laryngoscopy
Fig. 2.
(A, B) Showing a well-defined, oval hypodense mass lesion (predominantly fat attenuation) in right pharyngeal wall arising from pyriform fossa, extending superiorly in the laryngeal cavity on coronal and sagittal sections of contrast enhanced CT scan respectively
Intervention and Outcome
Tracheostomy was done as first step of management to relieve the respiratory distress as well as for the subsequent excision under general anaesthesia. Once the patient was stabilized, excision biopsy of the mass was planned under general anesthesia through direct laryngoscopy under endoscopic guidance. The lesion during the surgery appeared to be globular, mobile and pedunculated with stalk arising from the right pyriform fossa. The stalk of the mass was carefully dissected off from the mucosa of the pyriform sinus using bipolar electrocautery, taking precaution to preserve the mucosa and avoid damage to the vocal cords and was excised in toto. (Fig. 3) After the removal of mass, hemostasis was achieved and all adjacent structures appeared to be normal. Endoscopic removal of mass made the transoral excision surgery uneventful. The mass excised was rubbery in consistency, approximately 10 cm × 5 cm × 2 cm in size and was sent for histopathological examination.
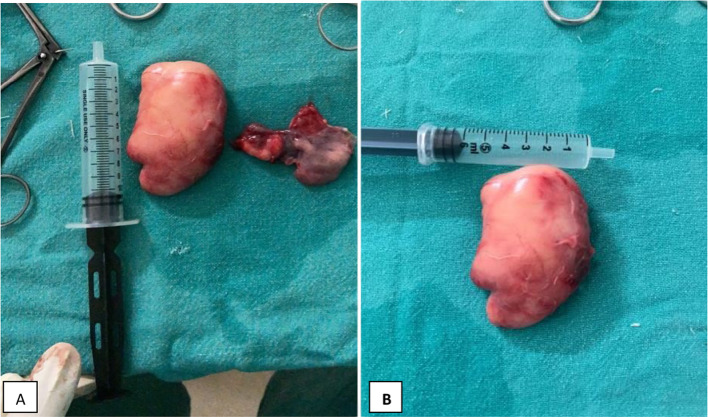
Fig. 3.
(A, B) Images showing approximately 10 cm × 5 cm × 2 cm size of mass excised from pyriform fossa
Histopathology of the mass revealed that bundles of spindle cells with fat spaces, fibro-myxoid areas, blood vessels and nerve bundles were seen, so features were suggestive of neural fibro lipoma. (Fig. 4).
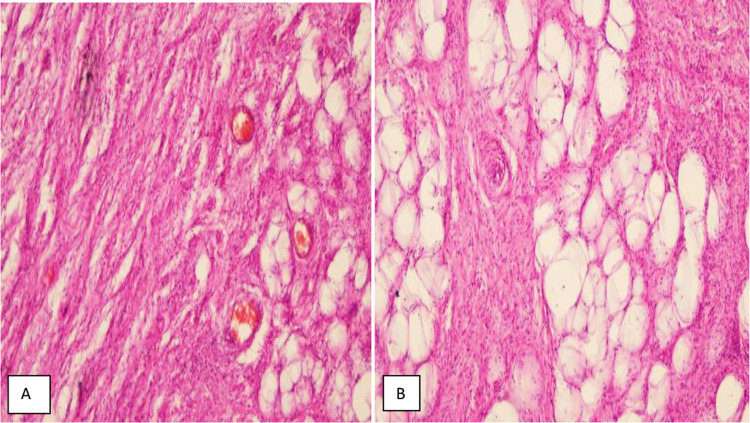
Fig. 4.
(A, B) Photomicrographs of the histopathology specimen (Hematoxylin and eosin; original and 200 × magnification). The lesion is composed of bundles of spindle cells with fat spaces, fibro-myxoid areas, Blood vessels and nerve bundles, features suggestive of neural fibro lipoma
The postoperative period was uneventful and 10 days after the surgery tracheostomy tube was successfully removed. No distress or dysphagia was seen during post-operative period. During post-operative follow up of 6 months there were no signs of any recurrence. (Fig. 5).
Fig. 5.

This is 6 months postoperative image showing no residual lesion or any recurrent lesion
Background
Neuofibrolipoma is one of the very rare entity found in hypopharynx. In previous studies,we have found only one study that was the first one to publish this entity [8].
Rationale
Rationale behind to publish this case report is its very rare presentation of neurofibrolipoma in hypopharynx as a pedunculated mass. Early diagnosis and treatment is also very important to prevent chances of sudden death of patient due to asphyxia.
Discussion
Anatomically hypopharynx is defined as the roughly triangular space extending from the base of the tongue and valleculae to the cricopharyngeus muscle including the corresponding portions of lateral and posterior pharyngeal walls, the pyriform sinuses, and the supraglottic laryngeal structures. Hypopharyngeal or upper GI polyps are benign tumors rarely encountered in clinical practice. Presenting Symptoms of the patients coincides with the size of the polyp. Contrast enhanced computed tomography and Magnetic resonance imaging are the radiological investigations that should be considered of choice [6]. These lesions probably originate as benign submucosal tumors and, with the propulsive movements of swallowing, are pulled with their thin mucosal lining to become pedunculated polyps. The repetitive forces of esophageal peristalsis cause their stalks to elongate slowly over time. They represent approximately 0.03% of all esophageal/hypopharyngeal neoplasms. The majority originate from the upper third of the esophagus, rarely from the hypopharynx, and extremely rarely from the oropharynx [7]. Neurofibrolipoma is a benign neoplasm of nerves, resulting from anomalous growth of fibro-adipose tissue of the nerve sheath; however, the histogenesis of the fibro-fatty tissue is disputed. It may be related to hypertrophy of mature fat and fibroblasts in the epineurium of nerve [8]. In a case study done in 2012 by Kumar, et al., a 12-year-old child was diagnosed with neuro fibrolipoma who had complaints of difficulty in breathing due to obstruction of the airway with the lesion extending into the oral cavity. Lesion in their case was 6.5 cm × 3 cm and was excised by splitting the oropharyngeal mucosa without any complications. It was the first reported case of neuro fibrolipoma in pharynx [8]. An adequate preoperative evaluation to identify the correct origin of the stalk is mandatory for a successful endoscopic or surgical treatment. Due to the potentially disastrous complications, removal of hypopharyngeal polyps is strongly recommended. This can be achieved using a transoral, transcervical, transthoracic, or endoscopic approach, depending on the location and size of the polyp [9]. Mass projecting into the airway in our case could have caused sudden spell of respiratory distress. Therefore, it was only rational and necessary to stabilize the patient with tracheostomy to ensure good and safe ventilation before proceeding with endoscopic procedure. Endoscopic removal appears to be a reasonable alternative to operative exploration if it can be accomplished safely in the hands of an experienced endoscopist. The pedicle should be completely excised/cauterized because incomplete excision may result in recurrence. As per literature the neural deficit can be pre-operative or post-operative if tumor is involving or compressing any nerve [6]. In hypopharynx any nerve from the pharyngeal plexuses may be involved in such lesions. But in our case there was no neural deficit during pre-operative and post-operative period so involvement of any nerve cannot be defined certainly.
Conclusion
Hypopharyngeal polypoidal masses are predominantly benign rare tumors. Neurofibrolipoma of hypopharynx are extremely rare to find. Despite their slow growth, these lesions should be removed because of potentially serious complications such as asphyxia or sudden death. Appropriate treatment should be based on size and site of origin of the lesion. Therefore, it can be concluded that understanding of this lesion and its early diagnosis and excision can be of great help to alleviate the associated morbidity and mortality. Endoscopic removal is a valid tool for excision of the mass with excellent post-operative results.
Funding
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Declarations
Conflicts of interest
The Authors declare that they have no conflicts of interest to declare that are relevant to the content of this article.
Informed consent
Written informed consent for publication of their clinical details was obtained from the patient.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ravinder Singh Nagi, Email: nagiravi@gmail.com.
Rupali, Email: rinkujotsingh799@gmail.com.
Ruchika Bhagat, Email: ruchikabhagat62@gmail.com.
Karan Kumar Sharma, Email: dr.karansharma@yahoo.com.
References
- 1.Liu C, Crawferd JM. The gastrointestinal tract. In: Kumar V, Abbas A, Fausto N, editors. Robbin and Cotran pathologic basis of disease. 7. Philadelphia: Elsevier; 2004. pp. 797–875. [Google Scholar]
- 2.Nielsen GP (2002) Lipomatosis of nerve. World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of Soft Tissue and Bone. In: Fletcher CD, Unni KK, Mertens F, editors. Lyon: IARC Press. pp. 24–5.
- 3.Iqbal B, Kambale T, Mushtaq I. Neurolipoma: a rare entity. J Clin Sci. 2014;11:55–56. doi: 10.4103/1595-9587.146505. [DOI] [Google Scholar]
- 4.Philp L, Naert KA, Ghazarian D. Fibrolipomatous hamartoma of the nerve arising in the neck: a case report with review of the literature and differential diagnosis. Am J Dermatopathol. 2015;37(7):e78–82. doi: 10.1097/DAD.0000000000000129. [DOI] [PubMed] [Google Scholar]
- 5.Razzaghi A, Anastakis DJ. Lipofibromatous hamartoma: review of early diagnosis and treatment. Can J Surg. 2005;48(5):394–399. [PMC free article] [PubMed] [Google Scholar]
- 6.Tokyol C, Aslan A, Hastürk GS, Kacar E, Boyaci MG (2015) Spinal neural fibrolipoma: A case report and review of the literature. Asian J Neurosurg. 10(4):341–3. 10.4103/1793-5482.162727. PMID: 26425172; PMCID: PMC4558819. [DOI] [PMC free article] [PubMed]
- 7.Caceres M, Steeb G, Wilks SM, Garrett HE (2006) Large pedunculated polyps originating in the esophagus and hypopharynx. Ann Thorac Surg 81: 393–396 [PMID: 16368421 DOI: 10.1016/j.athoracsur.2005.05.106] [DOI] [PubMed]
- 8.Kumar N, Mittal MK, Sinha M, Thukral BB. Neural fibrolipoma in pharyngeal mucosal space: a rare occurrence. Indian J Radiol Imaging. 2012;22(4):358. doi: 10.4103/0971-3026.111491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pallabazzer G, Santi S, Biagio S, D'Imporzano S. Difficult polypectomy-giant hypopharyngeal polyp: case report and literature review. World J Gastroenterol. 2013;19(35):5936–5939. doi: 10.3748/wjg.v19.i35.5936. [DOI] [PMC free article] [PubMed] [Google Scholar]