Introduction
A vallecular cyst is a mucous retention cyst that forms between the tongue base and the lingual surface of the epiglottis [1]. It presents around 5–10% of all benign laryngeal cysts [2]. Although benign, its significance raises from its location. The vallecula acts as a small valley between the pharynx and larynx, and, if obstructed, it can result in a life-threatening airway obstruction especially in the paediatrics age group [3]. This critical anatomical location makes the surgical access for excision a difficult task. Trans-Oral Laser-Assisted Surgery (TOLS) is one of the surgical modalities for the treatment of vallecular cyst. We hereby present our institutional experience with vallecular cysts and review the available literature.
Materials And Methods
A retrospective study was conducted in the laryngology department of Deenanath Mangeshkar Hospital and Research Centre. The keyword ‘Vallecular Cyst ‘was used to search the diagnosis list and the data search period was from January 2010- January 2020. The medical records numbers of the identified patients were collected. The patients’ records were reviewed, and the collected data includes the demographic details, presenting complaints, recorded pre-operative and post-operative Videolaryngoscopy videos, the surgical notes, and the final histopathology reports. The clinical notes of the follow-up period were also reviewed. For data collection and analysis, Microsoft Excel was used.
Results
1) Demographic Details
20 patients were identified. 13 patients were males, and 7 patients were females. The youngest patient was 2 months old male child, and the eldest patient was 75 years old man. 2 patients were infants and 2 were paediatrics below the age of 10 years and 16 patients were above the age of 18 years.
2) Symptoms and Clinical Examination
Dysphonia and dysphagia were the most common symptoms for the adults’ group. 8 patients reported a triad of dysphonia, dysphagia and globus sensation. On the other hand, snoring was the most reported symptom in paediatrics patients. Interrupted feeds, sleep disturbance with stridor were present in the 2 infants: 2 months old child and 18 months old child.
The video laryngoscopy records were reviewed. In all patients, the vallecular cyst was visible on Videolaryngoscopy examination and hence, the diagnosis of the vallecular cyst was made. 8 patients including all paediatrics age groups had a central vallecular cyst with attachment to the lingual surface of the epiglottis. 6 patients had lateralised vallecular cyst to the left side and 6 patients had lateralised vallecular cyst to the right. In addition, two of the paediatrics patients who had stridor had synchronous grade II laryngomalacia: short aryepiglottic folds with redundant mucosa over the arytenoid falling into the glottis.
3) Surgical Notes
All the patients underwent either trans-oral laser-assisted surgery for vallecular cyst excision or marsupialization combined with cold instruments. The procedures were done in the operating theatre under general anaesthesia. Suspension laryngoscopy was done using Lindholm’s laryngoscope (Picture 1) to access the vallecula under general anaesthesia. The airway was controlled with laser safe endotracheal tube. The intubation process was done as per our centre anaesthesia protocol: fibre-optic guided endotracheal intubation (Picture 2: Laser safe tube with vallecular cyst in the surgical field). Our centre is a tertiary care referral centre that is specialised in difficult airway from both surgical and anaesthesia perspective. In cases where the glottis view was blocked by the cyst, aspiration was done to reduce the pressure on the epiglottis and improve the glottis view. No patient required pre-operative tracheostomy and no patient had intubation related complication after surgery. Laser-friendly endotracheal tube was used in all patients as per standard international laser protocol as contact lasers also carry risk of airway fire. A 0-degree telescope was used to visualise the surgical field. Angio lytic lasers were used: diode laser was used in 12 patients and potassium titanyl phosphate (KTP) laser was used in 8 patients. All the patients underwent aspiration of the content of the cyst for confirmation that the cyst is not of a vascular origin and for microbiology culture before the surgical incision. The laser-assisted cruciate incision for drainage and then excision of the anterior and lateral walls of the cysts is done until the inferior border is flushed with the vallecular mucosa. 7 patients from the diode laser group had documented complete excision of the vallecular cyst including 2 paediatric patients. 1 patient had marsupialization using KTP laser due to embedded cyst with dome shape projected superior wall. The two paediatrics patients who had synchronous laryngomalacia underwent KTP Laser-assisted aryepiglottoplasty. The surgical notes of the remaining 12 patients did not elaborate if marsupialization was done or complete excision.
Picture 1.
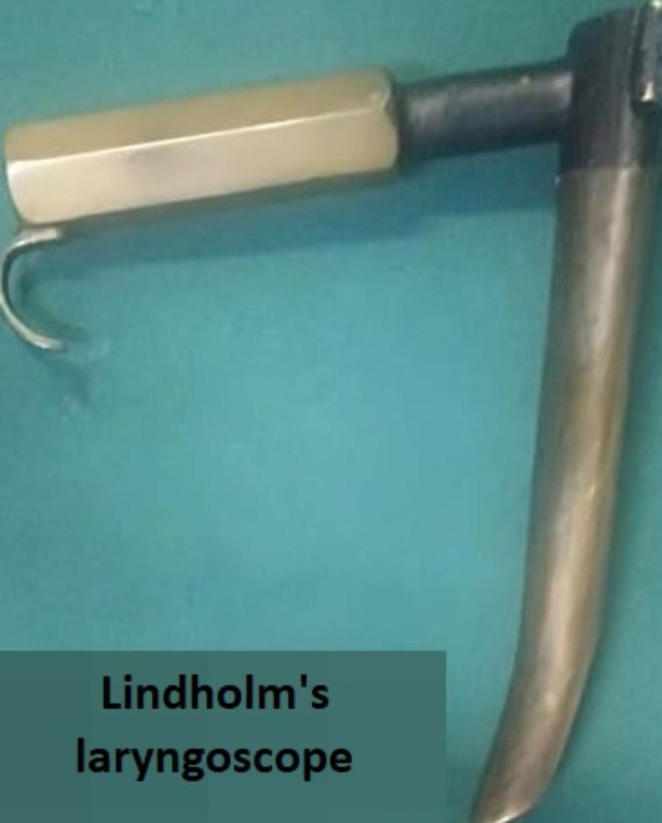
Lindholm?s laryngoscope
Picture 2.
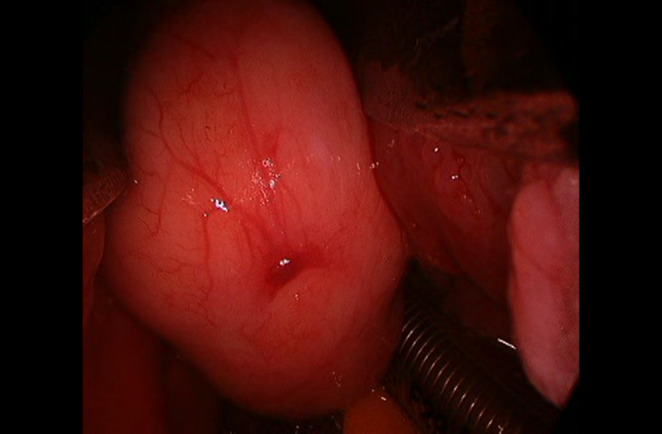
Vallecular cyst in surgical field with laser safety tube and lindholm’s scope in-situ.
4) Microbiology and Histopathology
Histopathologic and microbiologic examination were done for the surgically obtained tissue for all patients. Out of 20 patients, the microbiology of the 2 adults came positive for bacterial growth. 1 patient had positive Pseudomonas Aeruginosa and 1 patient has a positive Morganella Morgagnii. Both patients received post-culture oral antibiotics based on the reported sensitivity. The medical records did not mention if pre-operative infective history was present. The histopathology reports were reviewed as well and Table 1 shows the histopathology types of the obtained cysts.
Table 1.
Types of cysts on final histopathology report per patients
| Cyst Type | Number of patients | Age Group |
|---|---|---|
| Lymph-epithelial/Tonsillar Type | 8 patients | 2 Paediatrics: 6 adults |
| Retention/Ductal Type | 11 Patients | 2 infants: 9 adults |
| MALTOMA | 1 Patient | Adult |
1 out of the 20 patients had an unexpected histopathology report. The patient was a 32-year-old male patient with 5 months history of dysphagia with globus sensation. His video laryngoscopy record showed a centrally located cystic swelling with hypertrophied lingual tonsils. The records did not mention pre-operative neck status if palpable cervical lymph nodes present. Pre-operative computed tomography was done in an outside radiology centre and reported as vallecular cyst. The surgical notes also did not mention any special surgical event. The final histopathology report was MALT Lymphoma (MALTOMA) which was confirmed by immunochemistry study. The patient was referred to medical oncology for further treatment after 3 weeks post-surgery with no further OPD visits.
5) Post-Operative Follow Up
All the patients with the confirmed vallecular cyst (19/20) had 1 year follow up with laryngoscopy surveillance for early detection of recurrence. The video records of the laryngoscopic examination were reviewed. None of the patients developed recurrence 1-year post-surgery.
Discussion
Vallecular cyst is a benign laryngeal cyst that is located between the tongue base and the lingual surface of the epiglottis [4]. It is an uncommon entity and constitutes 5–10% of all benign laryngeal neoplasms [3]. It can be seen in both paediatrics and adult age group, each with different attributed pathogenesis. In the paediatrics population, vallecular cysts are congenital and attributed to a remnant of the embryonic epithelium at the vallecula [5]. On the other hand, in the adult population, the formation of the cyst is thought to be secondary to obstruction of the submucosal minor salivary glands [1]. Due to its location and based on its relative size to the patient’s anatomy, vallecular cyst can present as an incidental mass on laryngoscopic examination or radiological studies, or it can manifest as troublesome globus sensation, difficulty in swallowing and breathing difficulty. In the paediatrics age group, it can present as life-threatening upper airway obstruction, inspiratory stridor, interrupted feeds and cough, failure to thrive and regurgitations. Synchronous laryngomalacia has been reported in the literature[6]. Vallecular cyst has two effects on the supraglottis: (1) large cyst can push the epiglottis posteriorly causing mechanical obstruction of the laryngeal inlet and on the long-term pressure-associated weakness on the epiglottis; (2) the posterior displacement of the epiglottis results in a narrow airway passage that causes increase negative pressure on inspiration and hence induces mucosal oedema, reflux and prolapse of the arytenoid mucosa into the glottis. While it is difficult to identify whether it is primary or secondary, synchronous laryngomalacia management should be tailored to individual cases [7]. Table 2 summarises the reported causes of synchronous laryngomalacia with vallecular cyst. In our study, 2 infants’ patient who had synchronous laryngomalacia underwent cyst excision and supraglottoplasty and had resolution of their symptoms postoperatively.
Table 2.
Summary of the available case reports in the literature on synchronous laryngomalacia
| Author | Patient | Presentation | Laryngomalacia features | Management |
|---|---|---|---|---|
|
Önder et al. (2020) |
1 F 2 months |
Severe inspiratory stridor Failure to thrive |
Posteriorly displaced epiglottis floppy arytenoids | Cyst Excision and supraglottoplasty |
|
Yao et al. (2004) |
1 F 11 weeks |
Stridor failure to thrive |
Posteriorly displaced omega-shaped epiglottis | Cyst Excision |
|
Albert. et al. (2000) |
1 6 weeks |
Stridor Poor feeding |
Omega-shaped epiglottis Collapsing into the glottis on inspiration |
Cyst Excision |
|
WONG et al. (1995) |
2 Patients: 1 month - M 2 months- F |
Patient 1: Choking episodes with stridor Patient 2: interrupted feeding with stridor |
Patinet1: flaccid epiglottis sucked in on inspiration. Patient 2: omega-shaped epiglottis + floppy arytenoids sucked in on inspiration. |
Cyst Excision (both patients did not improve) |
The diagnosis of vallecular cysts is made clinically based on the location of the cyst on laryngoscopy examination and characteristic features of a cyst on CT and MRI[8]. A well-defined low-density lesion in the vallecula is usually suggestive of vallecular cyst when the clinical correlation is made. The differential diagnosis of a vallecular lesion includes lingual thyroid, teratoma and dermoid, out of which, lingual thyroid can have a similar radiological appearance like vallecular cyst. However, the final diagnosis is confirmed by histopathology. In our 10 years of experience, we had one male patient in the 4th decade of life who presented with progressive hoarseness of voice and on strobolaryngoscopy, a non-suspicious cyst was seen in the vallecula. Based on the appearance and location, the diagnosis of vallecular cyst was made. The patient underwent KTP laser-assisted marsupialization. The final histopathology report came as MALTOMA which was not suspected clinically.
Vallecular cyst is a surgical disease. The narrow and deep anatomical location of the vallecula makes the surgical access and instrumentation a challenge. Transoral marsupialization or deroofing are an acceptable treatment modality along with needle aspiration to reduce the size of the cyst in case of acute infection[9]. This procedure can be done using cold instruments, laser, coblation and even radiofrequency. The procedure can be done in office setup under local anaesthesia and theatre under general anaesthesia. Wang et al. reported minor tissue damage and a low recurrence rate in endoscopic-assisted transoral coblation marsupialization in 135 patients of the paediatrics population. Zalvan et al. reported successful improvement in symptoms of vallecular cysts in adults using KTP-laser in-office [8]. However, in his study, Zalvan was unable to send tissue for biopsy in the office-based treatment as the therapeutic channel in the laryngoscope will be loaded with the KTP fiber and the content and the ablated tissue will be removed by suction. This approach might raise a concern of missing a histopathological diagnosis like MALTOMA. In our hands, angiolytic lasers (diode and KTP) are preferred due to better haemostasis control, less collateral thermal injury, less post-operative pain, and faster resumption of routine oral diet.
Histopathology examination is the gold standard diagnostic tool for vallecular cyst[3]. Newman histological classification of intralaryngeal cysts classifies the cysts into three types: epithelial/ductal, tonsillar/lymph-epithelial and oncocytic[10]. This classification reflects the pathogenesis of cysts. While the epithelial and tonsillar are the commonest with good local control, the oncocytic type of intralaryngeal cysts is associated with a high recurrence rate and hence laryngoscope surveillance is recommended for detection of recurrence. This could be attributed to the papillary invagination of the cyst. In our study, none of the patients had an oncocytic cyst and none of our patients had recurrence after 1 year of surgery.
Conclusion
Vallecular cyst is an uncommon benign laryngeal cyst with variable manifestation. The clinical suspicion is made on laryngoscopic examination of a cyst in the vallecula, and CT/MRI can be utilised to narrow the differential diagnosis. Marsupialization with cold instrumentation or laser is an acceptable surgical technique for symptoms relief if complete excision is not feasible. Post-operative follow up is required for early detection of recurrence especially in oncocytic type of cyst.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Li Y, Irace AL, Dombrowski ND, Perez-Atayde AR, Robson CD, Rahbar R (2018 Oct) Vallecular cyst in the pediatric population: evaluation and management. Int J Pediatr Otorhinolaryngol 1:113:198–203 [DOI] [PubMed]
- 2.Lakhkar BN, Rajagopal KV, Shetty L (2003 Apr) Vallecular cyst. Indian J Otolaryngol Head Neck Surg 55(2):130–131 [DOI] [PMC free article] [PubMed]
- 3.Gogia S, Agarwal SK, Agarwal A. Vallecular Cyst in Neonates: Case Series—A clinicosurgical insight.Case Rep Otolaryngol. 2014 Oct28;2014:e764860 [DOI] [PMC free article] [PubMed]
- 4.Large Vallecular Masses ; Differential Diagnosis and Imaging Features [Internet]. [cited 2021 Nov 22]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6034357/ [DOI] [PMC free article] [PubMed]
- 5.Mahajan V, Mathew JL, Singh M, Gupta R, Das A (2008 Oct) Vallecular cyst-revisited. Indian J Pediatr 75(1):1081–1082 [DOI] [PubMed]
- 6.Glibbery N, Bance RR, Jonas N, Bewick J(2021) Synchronous airway lesions in children with severe, progressive and atypical laryngomalacia – experience of a UK tertiary referral centre.Int J Pediatr Otorhinolaryngol. Nov 15;110984. [DOI] [PubMed]
- 7.Ku A (2000 Mar) Vallecular cyst: report of four cases - one with co-existing laryngomalacia. J Laryngol Otol 114(3):224–226 [DOI] [PubMed]
- 8.Zalvan CH, Reilly E. Symptomatic vallecular cysts: diagnosis and management with the KTP laser. Eur Arch Otorhinolaryngol. 2016 Aug 1;273(8):2111–6 [DOI] [PubMed]
- 9.Vijayanand H, Mudhol RS, Patil PH, Maheswaran M (2009 Jun) Innovative surgical management of large vallecular cysts. Indian J Otolaryngol Head Neck Surg 61(2):147–149 [DOI] [PMC free article] [PubMed]
- 10.Wang G, Zhang F, Zhao J, Wang H, Li H, Wang X et al(2020) Minimally invasive procedure for diagnosis and treatment of vallecular cysts in children: review of 156 cases. Eur Arch Otorhinolaryngol. Dec 1;277(12):3407–14 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


