Abstract
Background
A growing body of literature shows that psychological distress is not only a major threat to psychological well-being but can also have a significant impact on physical health. In cancer patients, it can negatively affect prognosis and posttreatment recovery processes. Since face-to-face psychological interventions are often inaccessible to cancer patients, researchers have recently been focusing on the effectiveness of eHealth adaptations of well-established approaches. In this context, there has been a call for high-quality randomised controlled trials that would allow for a direct comparison of different approaches, potentially addressing different needs and preferences of patients, and also for more systematic research focusing on how psychological interventions affect not only psychological but also biological markers of stress. Both of these questions are addressed in the present study.
Methods
A randomised controlled trial will be carried out to test and compare the effectiveness of three eight-week eHealth programmes for the mental health support of cancer patients. All programmes will be delivered through the same application for mobile devices MOU MindCare. N = 440 of breast cancer survivors will be recruited at the end of their adjuvant treatment (chemotherapy, radiotherapy, or both) and randomly assigned to one of the three interventions – Mindfulness-Based Cognitive Therapy for Cancer (MBCT-Ca), Positive Psychology (PP), or Autogenic Training (AT) – or the treatment-as-usual (TAU) control group. Psychological and biological markers of stress and adaptive functioning will be assessed at baseline (T0), post-treatment (T1), three-month follow-up (T2), and nine-month follow-up (T3). Primary outcomes will include heart-rate variability and self-report measures of depression, anxiety, perceived stress, general quality of life, and positive mental health. Secondary outcomes will include the levels of serum cortisol and immunomarkers, sleep quality, fatigue, common health symptoms, and several transdiagnostic psychological variables that are expected to be specifically affected by the MBCT-Ca and PP interventions, including dispositional mindfulness, emotion regulation, self-compassion, perceived hope, and gratitude. The data will be analysed using the mixed model repeated measures (MMRM) approach.
Discussion
This trial is unique in comparing three different eHealth interventions for cancer patients based on three well-established approaches to mental health support delivered on the same platform. The study will allow us to examine whether different types of interventions affect different indicators of mental health. In addition, it will provide valuable data regarding the effects of stress-reducing psychological interventions on the biomarkers of stress playing an essential role in cancer recovery processes and general health.
Keywords: Psycho-oncology, e-mental health, Biomarkers of stress, Mindfulness-based intervention, Positive psychology intervention, Autogenic training
Highlights
-
•
A randomised controlled study is conducted to test a new eHealth application for cancer patients
-
•
The study compares three well-established stress-reduction interventions
-
•
Intervention effects on both psychological and biological markers of stress are tested
1. Background
Despite major advances in oncological care, psychological distress and its behavioral symptoms remain a pressing problem in cancer survivors (e.g., Bower, 2008). Recently, the management of the negative impact of cancer on mental health has been moving up in the rank of priority challenges of complex oncological and palliative care, not just for one, but for at least two reasons: Apart from directly affecting the quality of life through reduced psychological well-being, a growing body of literature shows that chronic stress can have a detrimental impact on physical health as well. Short-term effects can take the form of burdensome exacerbated physical symptoms (e.g., Mazor et al., 2019), while the arguably more concerning long-term effects concern the impact of chronic stress on lasting changes in physiology. A recent review by O’Connor et al. (2021) summarises three broad areas in which these effects have been demonstrated. The first involves long-term elevation in blood pressure and heart rate and decreased vagally mediated heart-rate variability (HRV), which has been linked to a worse prognosis in cancer progression (Kloter et al., 2018). The second area involves the effect of chronic stress on cortisol reactivity, specifically elevated cortisol levels with generally flatter diurnal cortisol curves. Both effects have been associated with negative health outcomes, such as a higher risk of cardiovascular problems and diabetes (O’Connor et al., 2021). Cortisol reactivity additionally plays an important part in the third area of documented impact of stress on health, namely dysregulation of the immune system. According to the glucocorticoid resistance hypothesis, the constantly elevated production of cortisol associated with chronic stress leads to a cascade of events that result in persistent inflammation within the organism (Tian et al., 2014), which has been associated with a host of problems, including increased risk of tumour initiation, progression, and metastasis (Antoni and Dhabhar, 2019). The concurrent suppression of cell-mediated immunity, on the other hand, inhibits the detection of pathogens and tumour cells and slows down healing processes (Antoni and Dhabhar, 2019). Both of these effects may result in a worse prognosis for cancer patients, complicate the process of post-treatment regeneration, and increase the incidence of health issues associated with unresolved tissue damage and a weakened immune system. Finding ways to protect the mental health of cancer survivors, therefore, seems to be crucial not only as a means of increasing well-being but potentially also as an essential part of the prevention of relapse and symptom aggravation (Eckerling et al., 2021).
1.1. eHealth psychological interventions for cancer patients
A major barrier to systematic mental health support for cancer survivors is the limited availability of evidence-based face-to-face interventions. eHealth adaptations of such interventions seem to offer a viable alternative with a much higher overall population impact. Apart from being highly accessible, considerably cheaper, and timesaving, online interventions offer additional advantages, such as anonymity and uninterrupted availability, and often do not require any further involvement of a trained mental health professional (Andersson and Titov, 2014). However, while there is some scientific evidence that cancer survivors may benefit from eHealth interventions (e.g., Nissen et al., 2021; Bruggeman Everts et al., 2015), there have also been calls for more rigorous research in this area for the effects to be more reliably established (e.g., Willems et al., 2020).
The latest systematic review and meta-analysis of psychological interventions improving mental well-being (van Agteren et al., 2021), based on the analysis of 419 randomised controlled trials, has revealed that mindfulness-based and multi-component positive psychological interventions demonstrate the greatest efficacy in both clinical and non-clinical populations. A key advantage of both these interventions is that they can be adapted into low-intensity structured programmes suitable for eHealth applications for individual use without the need for professional supervision. The proposed effectiveness mechanisms of mindfulness-based intervention programmes (MBPs) include improved attention regulation, body awareness, emotional awareness, and emotion regulation, change in perspective on the self, and increased self-compassion and self-transcendence (e.g., Tang et al., 2015). Mindfulness and self-compassion are considered to be transtherapeutic and transdiagnostic phenomena that play roles in the development and maintenance of mental health and quality of life (Schanche, 2013). A recent systematic review published by our research group (Matis et al., 2020) has shown that these interventions can be used successfully with cancer patients to reduce stress, anxiety, depression, fatigue, sleep problems and pain, and improve the levels of mindfulness, posttraumatic growth, and some parameters of general health. Compared to MBPs, which are focused on modifying the process of perceiving reality rather than the content, positive psychology interventions (PPIs) are more directional in their goals, teaching people how to perceive reality more positively through cognitive reappraisal. Beneficial effects in reducing stress symptoms (Hendriks et al., 2020) and increasing quality of life and well-being (Casellas-Grau et al., 2014) have been reported for multi-component PPIs; however, despite evidence that PPIs can also be successfully delivered online (Bolier and Abello, 2014), research on the efficacy of eHealth adaptations of such programmes in cancer patients is scarce.
Although MBPs and PPIs differ in the mechanism through which the positive change is supposed to be achieved, they are similar in focusing on the development of specific cognitive skills. In contrast, autogenic training (AT; Schultz and Luthe, 1959), the “golden standard” of psychological relaxation techniques, focuses on attenuating the immediate negative impacts of stress by directly addressing the physical aspect of the stress response. AT is a commonly used technique for relieving stress, tension, anxiety, and related somatic problems (Stetter and Kupper, 2002). Its beneficial effects have also been demonstrated in cancer patients (e.g., Minowa and Koitabashi, 2013). This widely clinically used intervention is commonly delivered as an audio recording, which makes it a good comparative criterion (active control) for evaluating the effectiveness of electronically delivered interventions, especially when testing for the incremental effect of cognitive intervention components compared to the relaxation component, such as in eMBPs.
In a review of psychological interventions for cancer patients, Hulbert-Williams et al. (2018) pointed out several limitations of current effectiveness research. These included, among other things, a lack of multiple-arm studies that would allow comparisons between different interventions, a lack of active control studies, a lack of high-powered studies testing for outcome moderators, and narrow choices of intervention outcomes. In the present research project, we address these limitations by simultaneously testing and comparing the effectiveness of three eHealth psychological intervention programmes based on the three approaches described above, all delivered through a single mobile application – MOU MindCare – using the same design and interface. Comparisons between different interventions are not only helpful in determining whether the individual eHealth programmes might be considered interchangeable when offered to patients with different personal preferences or access options, but they also allow the exploration of potential differences in suitability for different kinds of needs and patients with different baseline characteristics.
1.2. Impact of psychological interventions on psychological and biological markers of stress
While the detrimental impact of chronic stress on long-term physical health outcomes has been increasingly emphasised in scientific literature, still very little is known about how exactly the psycho-neuro-endocrine-immune network is affected by psychological interventions, and, specifically for the area of psycho-oncology, how those mechanisms interact with the cancer treatment and healing processes. Systematic, high-quality research focusing directly on changes in biological markers of stress has been scarce not only with regard to eHealth interventions but with regard to psychological interventions in general. One of the most commonly studied biological marker of stress is the level of cortisol and its regulation. A recent meta-analysis (Koncz et al., 2021) yielded a medium overall effect of meditation interventions on blood cortisol levels. The effect was more substantial for individuals at risk, including cancer patients, which is in line with the logical assumption that interventions help maintain neuro-immuno-humoral balance rather than systematically lowering cortisol levels. More recently, HRV has been gaining prominence as a reliable indicator of autonomic nervous system functioning, including its stress-related changes (Kim et al., 2018). However, due to the lack of high-powered randomised controlled studies, its role as a stress outcome in psychological intervention research could not yet be established (Rådmark et al., 2019). The same is true of the effect of psychological interventions on the functioning of the immune system. While Zhang et al. (2019) recent meta-analysis, focusing exclusively on cancer patients, demonstrated significant effects of various psychological interventions on white blood cell counts and the levels of several types of cytokines, immunomarkers in cancer patients are generally expected to be significantly affected by the type and stage of the disease, treatment and/or recovery, and research focusing on the impact of these factors has been almost completely absent. A notable exception is a recent study by Bower et al. (2022), which demonstrated a strong and long-term effect of the combination of chemotherapy and radiotherapy on inflammatory parameters, while radiotherapy by itself had a much less substantial impact, and no effects were observed for surgery. These findings indicate that treatment type is an important factor when studying the effect of stress reduction interventions on the immune response in cancer patients.
1.3. Aims of the study
The main objective of the presented study is to test the effectiveness of three eHealth psychological intervention programmes – (1) Mindfulness-Based Cognitive Therapy for Cancer (MBCT-Ca), (2) Positive Psychology (PP), and (3) Autogenic Training (AT) – delivered through a single mobile application in breast cancer survivors after adjuvant treatment. This includes the effects of these interventions on the change in multiple outcomes related to adaptive psychological functioning: symptoms of chronic stress, anxiety, and depression, overall quality of life, including physical health symptoms, positive mental health indicators, and biological markers of stress.
In addition, the present study has two secondary objectives. The first one is to compare the effects of the three intervention programmes on specific psychological outcome variables postulated as the driving forces of change in mindfulness-based and positive psychology interventions, i.e., dispositional mindfulness, emotion regulation, self-compassion, hope, and gratitude. The second one is to examine the associations between the psychological and biological markers of stress, with a special emphasis on immunological parameters, while controlling for the type, dosage, and time of completion of the adjuvant treatment (chemotherapy, radiotherapy, or both).
1.4. Hypotheses and research questions
1.4.1. Hypotheses regarding primary outcomes
Breast cancer survivors in all three intervention groups are expected to show a greater reduction in symptoms of depression (H1), anxiety (H2), and perceived stress (H3), and a greater increase in overall quality of life (H4) and heart rate variability (H5) as compared to the treatment-as-usual (TAU; waitlist) control group. In addition, participants in the MBCT-Ca and PP groups will show an increase in positive mental health (H6) and spiritual well-being (H7) compared to TAU. The primary criterion for determining intervention effectiveness will be changes in the outcome variables between the pre-treatment (T0) and post-treatment (T1) assessments; however, it is also expected that significant improvement over the pre-treatment condition will be maintained in the first and second follow-up assessments.
1.4.2. Hypotheses regarding secondary outcomes
Breast cancer survivors in all three intervention groups are expected to show a greater decrease in cortisol levels (H8), fatigue (H9), and common health symptoms (H10), and a greater increase in sleep quality (H11) as compared to TAU. In addition, participants in the MBCT-Ca group will show an increase in dispositional mindfulness (H12) and participants in the PP group will show an increase in gratitude (H13) and perceived hope (H14) compared to TAU. Both MBCT-Ca and PP will show an increase in self-compassion (H15) and a decrease in difficulties in emotion regulation (H16) compared to TAU.
1.4.3. Research questions
RQ1
Which immunomarkers are affected by the MOU MindCare interventions, and how is this change related to the change in other biological and psychological markers of stress?
RQ2
Is there a significant difference in mental and physical health outcomes associated with different types of intervention (i.e., MBCT-Ca, PP, and AT)?
2. Method
2.1. Study design
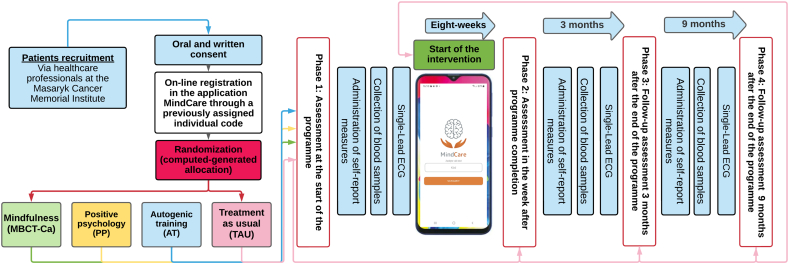
The study is conceptualised as a prospective randomised control trial employing a mixed 4 × 4 design. The design and timeline are outlined in Fig. 1. The study is registered at ClinicalTrials.gov (ID: NCT05406531).
Fig. 1.
Study design.
Participants will be randomly assigned to one of three intervention conditions – Mindfulness-Based Cognitive Therapy for Cancer (MBCT-Ca), Positive Psychology (PP), or Autogenic Training (AT) – or the waitlist/treatment-as-usual control condition (TAU). The 8-week online programme will be administered to each of the treatment groups via the same mobile application MOU MindCare. Assessment measurements will be collected at four time points: (1) pre-treatment assessment at the start of the intervention programme; (2) post-treatment assessment 8–9 weeks after the first assessment (one week within programme completion); (3) first follow-up assessment, three months after post-treatment assessment; (4) second follow-up assessment, nine months after post-treatment assessment. Data collection will involve the collection of blood samples, single‑lead electrocardiography (ECG) in standardised conditions, and online administration of self-report measures.
2.2. Participants and recruitment
2.2.1. Inclusion criteria
Individuals eligible for the study participants are breast cancer patients over the age of 18 at the end of adjuvant treatment (chemotherapy, radiotherapy, or a combination of both) who own a mobile device compatible with the MOU MindCare application and have Internet access.
2.2.2. Exclusion criteria
Contraindications for the tested intervention programmes: diagnosed psychotic disorder; severe depressive episode; panic disorder; bipolar disorder; personality disorder associated with uncontrollable mood changes; post-traumatic stress disorder; suicidal attempts and/or active suicidal ideation; disability pension due to non-specific mental or somatic problems; hospitalisation due to a psychiatric disorder in the past year.
The exclusion criteria will be assessed by the study coordinator (a psychologist or a medical doctor) upon recruitment. A printed list of the criteria will be presented to each potential participant, who will tick “yes” or “no” for the item. If the answer is “yes”, the study coordinator will discuss this verbally with the participant. If it is confirmed that one of more exclusion criteria are met, it will be explained to the participant that the eHealth programme is not suitable for them, and they will be given the contact details of the hospital's clinical psychology department in case they would like help with their mental health care.
2.2.3. Recruitment and participant registration
Eligible participants will be identified and individually invited to participate by their treating oncologist before the end of their adjuvant treatment and subsequently referred to a study coordinator on site. Alternatively, patients can learn about the study through personal recommendations and public advertisements (leaflets, social networks, and video clips screened in the hospital waiting room) and make an appointment with a study coordinator using the contact information provided. The study coordinator will meet each potential participant individually to introduce them to the MOU MindCare application, interventions, and the purpose of the study, including the conditions of study participation. The MOU MindCare eHealth programme will be offered to study participants for free. The patients who will express interest in participating in the study will then be asked to read and sign the consent form and provide their contact information.
The research team will get in touch with each participant before a medical check-up after the completion of their adjuvant treatment (at least 3 months for participants undergoing chemotherapy and 5–6 weeks for participants undergoing radiotherapy). At that point, the participants will receive an email with instructions on downloading and installing the MOU MindCare application and a unique code that will enable them to log into the online research management system administered by the Masaryk Memorial Cancer Institute, which will perform participant randomisation.
2.3. Randomisation
Before the participants sign the informed consent, it will be explained to them that if they are assigned to the control group (TAU/waitlist), the content of the MOU MindCare application will only be made available to them at the end of the study. Random assignment will take place for each participant individually after they complete the first set of self-report measures administered through the online research management system at the time of their first check-up. Block randomisation without stratification (with a block size of n = 4, corresponding to the number of groups) will be performed directly by the electronic system with blocks randomly generated without any involvement of the research team. This will allow the participants to be randomised on a rolling basis while ensuring a balanced group assignment. When the participant submits the completed questionnaire, the system will send an email with another code they will then use to unlock the MOU MindCare application. It can be downloaded at the Google or Apple store. Upon unlocking the application, each participant will learn about which group they were assigned to via a short introductory video with one of the instructors explaining the situation and reminding the participant of the conditions described in detail during recruitment.
The participants will be randomly assigned to one of four groups (MBCT-Ca, PP, AT, or TAU) as described in Section 2.1. and Fig. 1, with equal numbers of participants assigned to each condition, including TAU. Group identifiers will be subsequently converted into numerical codes by an authorised member of the research team responsible for anonymisation and data matching, so that neither the staff members performing the assessment of the biological outcomes nor the researchers performing the data analyses will be aware of the participants' group assignment.
2.4. Procedure
After completing the first set of measures and randomisation, participants in the intervention groups will be allowed to choose the first day of the intervention programme within the next 10 days. Each intervention programme lasts 8 weeks. After completing the programme, participants in the intervention groups will receive a link to the second (post-treatment) questionnaire. The control group will receive the link 8 weeks after logging into the MOU MindCare application. The link to the third questionnaire (first follow-up) will be sent automatically 3 months later, and the link to the fourth questionnaire (second follow-up) 9 months later. Each questionnaire will be available for completion 10 days after the link is sent.
The start of the intervention programme will be scheduled for each participant individually so that their regular appointments with the oncologist are synchronised with data collection points. This measure will minimise the burden on the participants and reduce study dropout, as the participants will not be required to make additional visits to the hospital or provide blood samples additional to those collected for clinical testing during the regular check-ups. Whenever possible, each appointment will be negotiated with the participant and their oncologist so that it takes place within 14 days of the research management system sending an email to the participant with a link to the questionnaire for the corresponding data collection point. During the appointment, peripheral blood samples will be collected, and ECG will be measured in standardised laboratory conditions.
2.5. Ethical issues and data management
The subjects will be informed about all pros and cons of the MOU MindCare programme both orally and in writing. The participant's identity will be strictly protected following the current legislation. The data will be collected by the Masaryk Memorial Cancer Institute and stored on the hospital's protected internal cloud storage system administered by authorised members of the hospital IT staff. All data sets will be matched by authorised members of the research team at the MMCI at the end of the study using participant identifiers, which will be subsequently removed. The final research data set, serving as the basis for data analysis and publication, will contain no information that could reveal the patient's identity.
2.6. Interventions
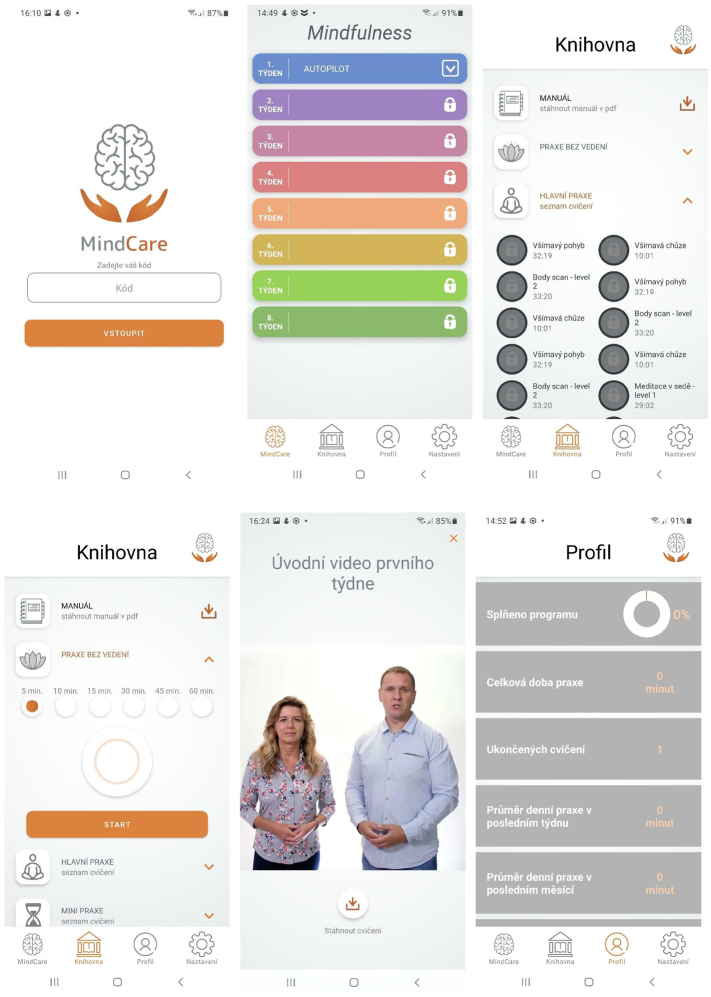
The MOU MindCare application delivers three independent 8-week mental health support programmes combining an asynchronous face-to-face approach, text, audio and video components, and support psychotherapy principles with a unique reminder and an emotional state monitoring system.1 The three programmes are (1) Mindfulness-Based Cognitive Therapy for Cancer (MBCT-Ca; Bartley, 2016), (2) Positive Psychology intervention based on the PERMA model (PP; Seligman, 2011), and (3) the basic level of Autogenic Training (AT; Schultz and Luthe, 1959). The structure and content of each programme are described in Appendix A, Appendix B, Appendix C, respectively.
Within the application, each programme is delivered via a set of short video recordings featuring lecturers providing explanations and instructions for each day's session or task. The videos are unlocked gradually to ensure the programme is timed correctly. Engagement with the programme takes up about 30 min each day. The application also sends notifications three times per day, prompting the user to respond to three simple questions about their current emotional state and providing brief statements of encouragement, reminders, or explanations. Sample screenshots from the application are shown in Fig. 2.
Fig. 2.
Sample screenshots of the MOU MindCare application (in Czech language).
2.7. Outcomes
2.7.1. Primary outcomes
2.7.1.1. Primary biological outcome
Heart rate variability (HRV): In the present study, it was chosen as a primary biological outcome over serum cortisol level because the logistical aspects of the study will not allow the collecting of blood samples at later times of the day when cortisol level fluctuations are minimised. ECG for the computation of HRV parameters will be recorded in standardised laboratory conditions (10 min spontaneous breathing at rest vs. 5 min controlled breathing at rest, with the frequency of six breathing cycles per minute) with the Psychlab data acquisition system with a sampling rate of 1000 Hz. The obtained data will be processed using the Kubios HRV Premium programme. Analysed HRV parameters will include: i) time-domain – mean RR, mean HR, RMSSD, SDNN, pNN50, stress index; ii) frequency-domain – LF power, HF power, and LF/HF ratio; iii) nonlinear – SD1, SD2.
2.7.1.2. Primary psychological outcomes
Perceived Stress Scale (PSS; Cohen et al., 1983) consists of 14 items describing feelings and thoughts the respondent might have experienced over the past month. Responses are indicated on a scale ranging from 0 (“Never”) to 4 (“Very often”), with higher scores indicating higher levels of perceived stress. PSS is extensively used as an outcome in intervention research in cancer patients (e.g., Zainal et al., 2013) and has been recommended for capturing both positive and negative aspects of coping with daily stress (Golden-Kreutz et al., 2004).
Depression Anxiety Stress Scales (DASS-21; Lovibond and Lovibond, 1995; Antony et al., 1998) comprise three 7-item scales assessing the emotional symptoms of depression, anxiety, and stress over the past week. Each item is rated on a scale from 0 (“Did not apply to me at all”) to 3 (“Applied to me very much or most of the time”). A separate score is computed for each scale. The widely used measure of anxiety and depression has demonstrated diagnostic properties comparable or superior to other widely used measures in breast cancer patients (Bener et al., 2016).
Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being (FACIT-Sp; FACIT, 2007) is a widely used measure of health-related quality of life for cancer patients. It is composed of the four scales of the 27-item Functional Assessment of Cancer Therapy – General (FACT-G Version 4; Webster et al., 2003) – Physical Well-Being, Social/Family Well-Being, Emotional Well-Being, and Functional Well-Being – and an additional 12-item Spiritual Well-Being scale (SpWB; Bredle et al., 2011). Each item is rated from 0 (“Not at all”) to 4 (“Very much”). FACT-G and SpWB yield two separate scores, with higher scores indicating higher quality of life.
Positive Mental Health Scale (PMHS; Lukat et al., 2016) is a short measure designed for the assessment of positive mental health (a combination of emotional, psychological, and social aspects of well-being) to expand the definition of mental health and complement measures focusing on symptoms of distress. Its 9 items are rated on a scale from 0 (“Do not agree”) to 3 (“Agree”).
2.7.2. Secondary outcomes
2.7.2.1. Secondary biological outcomes
Immuno-endocrine indicators: Peripheral blood samples will be collected between 9 and 11 a.m. Serum cortisol level will be determined by chemiluminescence-based immunoassay. Flow cytometric immunophenotyping will be used to establish relative and absolute counts of B-lymphocytes (CD19+), T-lymphocytes, T-helper lymphocytes (CD3+ CD4+), including HLA DR, T-cytotoxic lymphocytes (CD3+ CD8+) including HLA DR, NK-cells (CD16+ CD56+), NK-T-like cells (CD3+ CD56+) and monocytes HLA DR/CD14+. Levels of C-reactive protein (CRP) will be determined through turbidimetry. Cytokine levels (IL-1β, IL-2, IL-6, IL-8, IL-12, IFN-γ, TNFα, IL-17, IL-1ra, IL-4, IL-5, IL-10, TGF-β) will be analysed using the Bioplex 200 multiplex system.
2.7.2.2. Secondary psychological outcomes and other measures
Transdiagnostic aspects of adaptive psychological functioning tested as specific outcomes of the MBCT-Ca and PP interventions include dispositional mindfulness, measured by the Five Facet Mindfulness Questionnaire-15 (FFMQ-15; Baer et al., 2008), emotion regulation, measured by the Difficulties in Emotion Regulation Scale Short Form (DERS-SF; Kaufman et al., 2016), self-compassion, measured by the Self-Compassion Scale (SCS; Neff, 2003), gratitude, measured by the Gratitude Questionnaire-Six-Item Form (GQ-6; McCullough et al., 2002), and hope, measured by the Perceived Hope Scale (PHS; Krafft et al., 2019). Short-term stress-related health outcomes will include fatigue, sleep quality, and common somatic symptom severity. A complete list of secondary outcomes and other measures included in the study can be found in the study registration record at ClinicalTrials.gov (ID: NCT05406531).
2.7.3. Adherence and usability measures2
Self-report data on programme adherence and application usability will be collected via the post-treatment (T1) questionnaire, which will contain a set of questions asking about the participant's experience with the application including attractiveness, perceived usefulness, ease of use, and the level of engagement with the application as well as implementation of the presented practices in everyday life.
2.8. Sample size estimation
The target sample size was determined based on both practical and methodological considerations. Using a simulation method introduced by Lakens and Caldwell (2021), we computed the sample size necessary to detect an interaction effect for a 4 × 4 mixed design with 80 % power (at the 5 % significance level). The effect can be described as no change in the outcome variable observed in the control group contrasted with a moderate improvement (Cohen's d = 0.50) in all three intervention groups, which remains stable over time, given that the individual measurements are only weakly correlated (r = 0.25, based on intraindividual day-to-day variation in cortisol levels). The target sample size was thus established at 90 participants per group (N = 360 in total). Considering the study logistics, we expect relatively low drop-out rates of about 20 %, which is why we are aiming at recruiting 110 participants per group, which is near the upper limit of eligible subjects that can be recruited at the MMCI over two years.
2.9. Planned analyses
The researcher performing data analyses will be blinded to the participant group assignment. In the preliminary analysis, descriptive statistics will be computed, and pre-treatment (T0) data will be analysed to examine pre-treatment differences between the groups and the nature of dropout. The effectiveness analyses will be performed using the intention-to-treat (ITT) approach. Change in primary and secondary outcomes will be analysed using the mixed model repeated measures (MMRM) approach, testing the fixed effects of time, group, and their interaction. In the mixed model approach, missing data are treated as missing at random (MAR), and cases with missing data can be analysed directly to yield unbiased estimates provided that all cases with no post-baseline observations (i.e., cases in which there are no outcomes to analyse) are excluded. Therefore, in the analysis of post-treatment outcomes, participants with no post-treatment outcome data will be excluded, and the identified covariates of the missingness (drop-out) will be included in the model to adjust for potential bias. In the analysis of change in the outcome over the first and second follow-up, all participants with at least one post-baseline outcome assessment will be included.
Since we expect some level of variation in the timing of the collection of physiological data due to practical considerations (scheduling and rescheduling of regular check-ups), depending on the level of asynchronisation, a sensitivity analysis might be performed by fitting two separate models for each basic effectiveness analysis, one assuming a repeated-measures design ignoring the temporal misalignment, and the other treating the actual time of the measurement as a continuous covariate within the prediction model. In addition, since the multilevel modelling approach assumes a normal distribution of outcome variables, in case of severe non-normality requiring data transformation, depending on the nature of non-normality, an additional alternative basic effectiveness analysis might be conducted with untransformed data (e.g., robust repeated measure ANOVA with trimmed means) to see if the main results are confirmed. The significance level for the tested effects will be set at 5 %.
Within the MMRM model, the type of received adjuvant treatment (chemotherapy, radiotherapy, or a combination of both) will be entered in the next step as an additional factor and programme adherence and programme timing (i.e., days after completing adjuvant therapy) as covariates. Associations between psychological and biological variables will be computed while taking the measurement time point and the treatment type into account.
3. Discussion
Mental health support has become an essential part of cancer treatment, not only as a means of improving the psychological functioning of cancer patients but also – based on the increasingly emphasised links between long-term psychological stress and physical health – to help reduce barriers to fast and successful recovery and protect cancer survivors from further physical health issues. However, because the vast majority of previous studies regarding the effect of psychological interventions on the biomarkers of stress have been conducted on small samples and each tested a different set of outcomes (often employing different methodological approaches), several authors (e.g., Antoni and Dhabhar, 2019; Rådmark et al., 2019) have reiterated that high-quality RCTs on larger samples are essential in resolving current inconsistencies in research findings. In the area of eHealth interventions, the gap to fill has been even wider.
Our study has several strong points. Most importantly, it allows us to simultaneously test and compare the effectiveness of eHealth versions of three well-established intervention programmes using a single mobile application, with all interventions delivered in a standardised form, maintaining a unified design and timing. If the effectiveness of the three interventions is established, the MOU MindCare application will represent a significant contribution to the complex system of health care in Czechia, helping many oncological patients fight the struggles associated with cancer treatment and recovery without the need for low-availability face-to-face treatments. However, the study also has the potential to expand research findings on a much more general level. First, it opens the door for a systematic examination of the expected differences in the specific effects of the individual interventions, which stem from their differential theoretical foundations. Second, thanks to high power, sample homogeneity, and embeddedness in standard medical care, the study provides an excellent opportunity to examine the effects on both psychological and biological outcomes as well as the associations between them. The design allows the disease- and treatment-related variables that might have an impact on the biomarkers of stress to be entered as covariates in the statistical model and directly tested, which makes the study especially suitable for the exploration of immunoendocrine outcomes.
Still, there are several limitations and risks associated with the current design. Since the study is organically embedded in routine post-treatment care, we expect lower dropout rates compared to similar studies; however, the data collection points, especially for biological variables, might become somewhat unsynchronised with psychological measurements due to logistic reasons, which might be limiting for the exploration of the associations between psychological and physiological markers of stress. Another issue that might potentially affect the results of the study and their interpretability is low adherence to the intervention programme. Although participants will only be recruited if they confirm their ability and motivation to work with the MOU MindCare application, it might still happen that they decide at some point that the way the intervention is delivered does not suit their personal preferences and stop using it. In our study, we will test the level of programme adherence as a covariate to evaluate its impact on the overall results. Finally, although the homogenous sample and the fact that the intervention programmes are set at a late stage of oncological treatment (i.e., after the completion of adjuvant therapy) makes it more likely that true effects will be detected by restricting the sources of unsystematic variance, the same two aspects of the study will also inherently result in limited generalisability of results. In practice, patients might be more motivated to use the application at earlier stages of cancer treatment, at which the effectiveness of the individual interventions might be different. While the impact on biomarkers might be difficult to study in diverse samples of cancer patients, in order to obtain sufficient evidence of the overall effectiveness of the MOU MindCare intervention programmes in reducing stress and improving mental health, further research will have to be conducted with different types of cancer patients.
Trials status
The trial recruitment started on 06 June 2022. currently recruiting (Ncurrent = 80 as of January 10, 2023). Recruitment will continue until February 2024. The follow-up assessment is expected to be completed by December 2024.
Ethical statement
The project and the informed consent form have been discussed with and approved by the Ethics Committee Institutional Review Board of the Masaryk Memorial Cancer Institute (approved 10/06/2021) and the Ethics Committee of the Faculty of Medicine, Masaryk University (approved 16/06/2021).
Funding
This study is funded by the Ministry of Health of the Czech Republic, grants no. NU22-09-00056 and NU21-09-00558, the Ministry of Education, Youth and Sports of the Czech Republic, NPO 5.1 Programme EXCELS, grant no. 2/11/LX22NPO5107, and Masaryk University, grants no. MUNI/A/1126/2021 and MUNI/A/1319/2022.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors wish to thank Dominika Mokrá from Merck Sharp & Dohme for the coordination of IT specialists involved in the development of the MOU MindCare App and Merck Sharp & Dohme (MSD) for financial support of the MOU MindCare App.
Footnotes
The MOU MindCare application will also collect responses to three brief self-report items assessing the participant's current emotional state, which will be prompted via notifications three times per day throughout the eight-week period of the intervention programme. However, this measure is not treated as one of the outcomes of the present study and will not be analysed in the main RCT report. Instead, it will be analysed separately together with the detailed adherence and usability data generated by the application (possibly with data from other users not included in the present RCT), as explained in footnote 2.
The MOU MindCare application itself will monitor the behaviour of the participant in the following adherence parameters: the first launch of the application after installation and log-in; each launch of the application or activation of the application from sleep mode; running each exercise (audio, video, tip, text); time and duration of application use and engagement with each activity; finishing – watching the audio and video to the end; closing of the exercise; return to the exercises in the library (even after the end of the programme). However, these data will require additional time for export and processing and will not be included in the principal analysis of primary and secondary outcomes.
Appendix A. Content of the MBCT-Ca intervention
| Module | Content |
|---|---|
| Introduction | Introduction to the programme Explanation of tools and how to use the application |
| 1. Automatic pilot |
Introducing mindfulness and the topic of the automatic pilot: Mindfulness and its relevance to mental health Experiencing the present moment through our senses Learning to ground through body awareness The skill of taking a break in the middle of the day |
| 2. New way of knowing |
Understanding how thoughts influence feelings, bodily sensations, and actions: Recognising how the mind (often unconsciously) interprets everything that happens Learning to stabilise attention on the breath Exploring thoughts, emotions and bodily sensations during pleasant events |
| 3. Befriending the breath and the body in movement |
Anchoring the attention on the breath and the body in movement: Cultivation of mindfulness during movement Brief sitting practice Developing a habit of practicing short meditation practice (Breathing Space) several times during the day Exploring thoughts, emotions and bodily sensations during unpleasant events |
| 4. Learning to respond |
Recognising reactivity within anxious or ruminative patterns of the mind: Introduction to a longer sitting meditation Developing a skill of tuning to physical sensations in the body (Body Barometer Practice) Developing kindly attitude to oneself in difficult moments Understanding the vicious circle of anxious preoccupation in cancer patients |
| 5. Gently being with the difficult |
Learning to stop and notice patterns of mind that signal the arrival of distress: Locating physical sensations within the body Noticing and exploring unpleasant physical sensations related to the difficulty Learning to stay open to all aspects of experience with tenderness |
| 6. Thoughts are not facts |
Learning to recognise that thoughts are impermanent, empty, and essentially impersonal: Allowing thoughts to come and go Developing a habit of using Breathing Space when feeling overwhelmed by thoughts Returning attention to the chosen anchor whenever needed |
| 7. Taking care of myself |
Charting an overview of personal patterns and learning how to make choices that support well-being: Identifying nourishing and depleting activities of everyday life Understanding how activities relate to moods Using activities as a way of lifting the mood Understanding the difference and usefulness of selective and open awareness |
| 8. A new beginning |
Review of the whole programme and a plan for the future: Understanding the key domains of mindfulness Identifying practices that have been useful and helpful Creating a plan for maintaining and improving well-being in the future |
Appendix B. Positive psychology modules and their objectives
| Module | Objective |
|---|---|
| Introduction | Introduction to the programme Explanation of tools and how to use the application |
| 1. Focus on the bright sides of life |
Explaining psychological well-being and the concept of PERMA: Key components of the PERMA concept of psychological well-being and their relevance in daily life Focus on everyday positive experiences |
| 2. Positive emotions and the power of gratitude |
Enhancing emotional well-being: Importance of positive emotions and their effect on mental and physical well-being Increasing emotional well-being by acknowledging and savouring positive emotions Developing the skill of gratitude |
| 3. Good relationships and positive communication |
Acknowledging the relevance of relationships, and how positive communication can be helpful in maintaining supportive relationships: Importance of interpersonal relations Caring for and improving the quality of relationships to help maintain and strengthen psychological well-being |
| 4. Identification and use of strengths |
Identifying and developing of character strengths: Classification and explanation of character strengths and virtues Strength-spotting and strength use Spotting strengths in others |
| 5. Positive thinking: optimism and hope |
Developing optimistic and hopeful thinking: Importance of positive thinking and its impact on psychological well-being Adopting and using the optimistic thinking style Developing the skill of maintaining hope Dealing with the future with a positive attitude |
| 6. Positive activities and flow |
Acknowledging the relevance of intentional positive activities and how flow can increase life satisfaction: The concept of optimal experience (flow) Planning and promoting positive activities, alone or with others |
| 7. The meaningfulness of life |
Enhancing meaningfulness of life: Awareness of the importance of having a purpose in life Finding a purpose through character strengths Allowing growth through adversity Importance of connectedness and a sense of oneness |
| 8. Harmony and inner balance |
Establishing inner balance and harmony in life: Revealing and using your own resources of psychological well-being and resilience Creating a positive portfolio Review of the whole programme and its benefits Creating a plan for maintaining and improving psychological well-being in the future |
Appendix C. Autogenic training modules and their objectives
| Module | Objective |
|---|---|
| Introduction | Introduction to the programme Explanation of tools and how to use the application |
| 1. Muscular relaxation: The feeling of heaviness |
The body & mind phenomenon and principles of physical relaxation based on Jacobson's Progressive Muscular Relaxation (PMR) Introduction to the PMR approach to physical relaxation and how it can be used in everyday life Finding motivation to practice daily |
| 2. Passive concentration on feeling warm |
Enhancing focus on the first step of the Autogenic Training – feeling of heaviness without the necessity of body activation The importance of concentration and its effect on mental and physical relaxation Increasing the experience of relaxation through daily practice The skill of focusing on body sensations |
| 3. Practice of perceiving heaviness and warmth + calm cardiac activity and concentration on the respiratory mechanism |
Continued practice of heaviness and warmth, followed by two short sensations of calm breathing and heart beating The significance of the calming effect of passive concentration Improving the quality of concentration to help maintain and strengthen the effect of relaxation on the body and mind |
| 4. Concentration on the warmth in the abdominal region |
Recognising and enhancing the effect of imagination Focusing on the body-warming sensation in the abdominal region, and associating it with the feeling of security Maintaining motivation for daily practice Recognising the increase in enjoyment stemming from enhanced concentration and relaxation skills |
| 5. Practicing the first five steps – supporting the patience |
Continued practice of the first five steps Importance of maintaining concentration for longer period of time The skill of enjoying positive sensations inside the body Dealing with imperfection and finding the individual intensity level for each step and sensation during relaxation |
| 6. Passive concentration on coolness in the cranial region |
Focusing on coolness in the cranial region (forehead) and understanding how this sensation can increase positive outcomes of relaxation Differences between a full AT exercise and practicing each step separately Planning and promoting relaxation in everyday life |
| 7. Practice makes perfect! |
Enhancing AT practice in different durations Importance of individual approach to practicing relaxation Finding purpose in practice through recognising positive influences on the body and mind Allowing improvement through feelings of security, imagination, and experience of joy Recognising the importance of self-awareness and self-reflection |
| 8. The future is starting, enjoy this moment! |
Establishing autonomous motivation to practice AT Learning to choose the appropriate duration and intensity of AT based on current needs or intentions Review of the benefits of AT Principles of using AT to achieve healthy and balanced life |
References
- van Agteren J., Iasiello M., Lo L., Bartholomaeus J., Kopsaftis Z., Carey M., Kyrios M. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat. Hum. Behav. 2021;5:631–652. doi: 10.1038/s41562-021-01093-w. [DOI] [PubMed] [Google Scholar]
- Andersson G., Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni M.H., Dhabhar F.S. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer. 2019;125(9):1417–1431. doi: 10.1002/cncr.31943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antony M.M., Bieling P.J., Cox B.J., Enns M.W., Swinson R.P. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol. Assess. 1998;10(2):176–181. doi: 10.1037/1040-3590.10.2.176. [DOI] [Google Scholar]
- Baer R.A., Smith G.T., Lykins E., Button D., Krietemeyer J., Sauer S., Walsh E., Duggan D., Williams J.M.G. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bartley T. John Wiley & Sons; 2016. Mindfulness: A Kindly Approach to Being With Cancer. [Google Scholar]
- Bener A., Alsulaiman R., Doodson L.G., El Ayoubi H.R. Comparison of reliability and validity of the breast cancer depression anxiety stress scales (DASS-21) with the Beck depression inventory-(BDI-II) and hospital anxiety and depression scale (HADS) Int. J. Behav. Res. Psychol. 2016;4(4):197–203. doi: 10.19070/2332-3000-1600035. [DOI] [Google Scholar]
- Bolier L., Abello K.M. In: Wiley-Blackwell Handbook of Positive PsychologicalInterventions. Parks A.C., Schueller S.M., editors. Wiley-Blackwell; 2014. Online positive psychological interventions: state of the art and future directions; pp. 286–309. [Google Scholar]
- Bower J.E. Behavioral symptoms in breast cancer patients and survivors: fatigue, insomnia, depression, and cognitive disturbance. J. Clin. Oncol. 2008;26(5):768–777. doi: 10.1200/JCO.2007.14.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower J.E., Ganz P.A., Irwin M.R., Cole S.W., Carroll J., Kuhlman K.R., Petersen L., Garet D., Asher A., Hurvitz S.A., Crespi C.M. Acute and chronic effects of adjuvant therapy on inflammatory markers in breast cancer patients. JNCI Cancer Spectrum. 2022;6(4) doi: 10.1093/JNCICS/PKAC052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredle J.M., Salsman J.M., Debb S.M., Arnold B.J., Cella D. Spiritual well-being as a component of health-related quality of life: the functional assessment of chronic illness therapy—spiritual well-being scale (FACIT-Sp) Religions. 2011;2(1):77–94. doi: 10.3390/rel2010077. [DOI] [Google Scholar]
- Bruggeman Everts F.Z., van der Lee M.L., de Jager Meezenbroek E. Web-based individual mindfulness-based cognitive therapy for cancer-related fatigue — a pilot study. Internet Interv. 2015;2(2):200–213. doi: 10.1016/J.INVENT.2015.03.004. [DOI] [Google Scholar]
- Casellas-Grau A., Font A., Vives J. Positive psychology interventions in breast cancer. A systematic review. Psycho-Oncology. 2014;23(1):9–19. doi: 10.1002/pon.3353. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Eckerling A., Ricon-Becker I., Sorski L., Sandbank E., Ben-Eliyahu S. Stress and cancer: mechanisms, significance and future directions. Nat. Rev. Cancer. 2021;21(12):767–785. doi: 10.1038/s41568-021-00395-5. [DOI] [PubMed] [Google Scholar]
- FACIT . FACIT.org; 2007. FACIT-Sp: functional assessment of chronic illness therapy – spiritual well-being.https://www.facit.org/measures/FACIT-Sp November 16. [DOI] [PubMed] [Google Scholar]
- Golden-Kreutz D.M., Browne M.W., Frierson G.M., Andersen B.L. Assessing stress in cancer patients: a second-order factor analysis model for the perceived stress scale. Assessment. 2004;11(3):216–223. doi: 10.1177/1073191104267398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks T., Schotanus-Dijkstra M., Hassankhan A., De Jong J., Bohlmeijer E. The efficacy of multi-component positive psychology interventions: a systematic review and meta-analysis of randomized controlled trials. J. Happiness Stud. 2020;21(1):357–390. doi: 10.1007/s10902-019-00082-1. [DOI] [Google Scholar]
- Hulbert-Williams N.J., Beatty L., Dhillon H.M. Psychological support for patients with cancer: evidence review and suggestions for future directions. Curr. Opin. Support. Palliat. Care. 2018;12(3):276–292. doi: 10.1097/SPC.0000000000000360. [DOI] [PubMed] [Google Scholar]
- Kaufman E.A., Xia M., Fosco G., Yaptangco M., Skidmore C.R., Crowell S.E. The difficulties in emotion regulation scale short form (DERS-SF): validation and replication in adolescent and adult samples. J. Psychopathol. Behav. Assess. 2016;38(3):443–455. doi: 10.1007/s10862-015-9529-3. [DOI] [Google Scholar]
- Kim H.G., Cheon E.J., Bai D.S., Lee Y.H., Koo B.H. Stress and heart rate variability: a meta-analysis and review of the literature. Psychiatry Investig. 2018;15(3):235–245. doi: 10.30773/pi.2017.08.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloter E., Barrueto K., Klein S.D., Scholkmann F., Wolf U. Heart rate variability as a prognostic factor for cancer survival–a systematic review. Front. Physiol. 2018;9 doi: 10.3389/fphys.2018.00623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koncz A., Demetrovics Z., Takacs Z.K. Meditation interventions efficiently reduce cortisol levels of at-risk samples: a meta-analysis. Health Psychol. Rev. 2021;15(1):56–84. doi: 10.1080/17437199.2020.1760727. [DOI] [PubMed] [Google Scholar]
- Krafft A.M., Martin-Krumm C., Fenouillet F. Adaptation, further elaboration, and validation of a scale to measure hope as perceived by people: discriminant value and predictive utility Vis-à-Vis dispositional hope. Assessment. 2019;26(8):1594–1609. doi: 10.1177/1073191117700724. [DOI] [PubMed] [Google Scholar]
- Lakens D., Caldwell A.R. Simulation-based power analysis for factorial analysis of variance designs. Adv. Methods Pract. Psychol. Sci. 2021;4(1):1–14. doi: 10.1177/2515245920951503. [DOI] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav. Res. Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Lukat J., Margraf J., Lutz R., van der Veld W.M., Becker E.S. Psychometric properties of the positive mental health scale (PMH-scale) BMC Psychol. 2016;4(1):1–14. doi: 10.1186/s40359-016-0111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matis J., Svetlak M., Slezackova A., Svoboda M., Šumec R. Mindfulness-based programs for patients with cancer via eHealth and mobile health: systematic review and synthesis of quantitative research. J. Med. Internet Res. 2020;22(11) doi: 10.2196/20709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazor M., Paul S.M., Chesney M.A., Chen L.M., Smoot B., Topp K., Conley Y.P., Levine J.D., Miaskowski C. Perceived stress is associated with a higher symptom burden in cancer survivors. Cancer. 2019;125(24):4509–4515. doi: 10.1002/cncr.32477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough M.E., Emmons R.A., Tsang J.-A. The grateful disposition: a conceptual and empirical topography. J. Pers. Soc. Psychol. 2002;82(1):112–127. doi: 10.1037/0022-3514.82.1.112. [DOI] [PubMed] [Google Scholar]
- Minowa C., Koitabashi K. Effects of autogenic training on perioperative anxiety and pain in breast cancer patients. Kitakanto Med. J. 2013;63(1):1–11. doi: 10.2974/kmj.63.1. [DOI] [Google Scholar]
- Neff K.D. Development and validation of a scale to measure self-compassion. Self Identity. 2003;2:223–250. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- Nissen E.R., Zachariae R., O’Connor M., Kaldo V., Jørgensen C.R., Højris I., Borre M., Mehlsen M. Internet-delivered mindfulness-based cognitive therapy for anxiety and depression in cancer survivors: predictors of treatment response. Internet Interv. 2021;23 doi: 10.1016/J.INVENT.2021.100365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor D.B., Thayer J.F., Vedhara K. Stress and health: a review of psychobiological processes. Annu. Rev. Psychol. 2021;72:663–688. doi: 10.1146/annurev-psych-062520-122331. [DOI] [PubMed] [Google Scholar]
- Rådmark L., Sidorchuk A., Osika W., Niemi M. A systematic review and meta-analysis of the impact of mindfulness based interventions on heart rate variability and inflammatory markers. J. Clin. Med. 2019;8(10) doi: 10.3390/jcm8101638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schanche E. The transdiagnostic phenomenon of self-criticism. Psychotherapy. 2013;50(3):316–321. doi: 10.1037/a0032163. [DOI] [PubMed] [Google Scholar]
- Schultz J.H., Luthe W. Grune & Stratton; 1959. Autogenic Training: A Psychophysiologic Approach to Psychotherapy. [Google Scholar]
- Seligman M. Free Press; 2011. Flourish. [Google Scholar]
- Stetter F., Kupper S. Autogenic training: a meta-analysis of clinical outcome studies. Appl. Psychophysiol. Biofeedback. 2002;27(1):45–98. doi: 10.1023/A:1014576505223. [DOI] [PubMed] [Google Scholar]
- Tang Y.Y., Hölzel B.K., Posner M.I. The neuroscience of mindfulness meditation. Nat. Rev. Neurosci. 2015;16(4):213–225. doi: 10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- Tian R., Hou G., Li D., Yuan T.F. A possible change process of inflammatory cytokines in the prolonged chronic stress and its ultimate implications for health. Sci. World J. 2014;2014 doi: 10.1155/2014/780616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster K., Cella D., Yost K. The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual. Life Outcomes. 2003;1 doi: 10.1186/1477-7525-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willems R.A., Bolman C.A., Lechner L., Mesters I., Gunn K.M., Ross X.S., Olver I. Online interventions aimed at reducing psychological distress in cancer patients: evidence update and suggestions for future directions. Curr. Opin. Support. Palliat. Care. 2020;14(1):27–39. doi: 10.1097/SPC.0000000000000483. [DOI] [PubMed] [Google Scholar]
- Zainal N.Z., Booth S., Huppert F.A. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: a meta-analysis. Psycho-Oncology. 2013;22(7):1457–1465. doi: 10.1002/pon.3171. [DOI] [PubMed] [Google Scholar]
- Zhang P., Mo L., Li X., Wang Q. Psychological intervention and its immune effect in cancer patients: a meta-analysis. Medicine. 2019;98(38) doi: 10.1097/MD.0000000000017228. [DOI] [PMC free article] [PubMed] [Google Scholar]