Abstract
Introduction
In the last few years, online psychotherapy programs have burgeoned since they are a more accessible and scalable treatment option compared to in-person therapies. While these online programs are promising, understanding the user experience and perceptions of care is essential for program optimization.
Methods
This study investigated the experiences of end-users who had previously received online psychotherapy through a web-based platform. A 35-item multiple-choice survey was developed by the research team and distributed to past users to capture their perceptions of the program.
Results
The survey yielded 163 responses, with a 90 % completion rate. Participants were predominantly white and female, with an average age of 42 years. While most participants preferred in-person therapy, they also reported the benefits of the online psychotherapy program. Participants had positive perceptions of the platform, the quality and interaction of their therapist, and the homework assignments and skills covered. Lack of motivation to complete weekly homework assignments was cited as a common struggle.
Discussion
The findings support online psychotherapy as a beneficial digital mental health tool and highlight some areas for improvement. Scalability and accessibility are key benefits of the platform. At the same time, improvements in participant engagement, including those from equity-seeking and equity-deserving groups, may enhance the efficacy of the programs offered.
Keywords: Online psychotherapy, Mental health, User experience, Mental health treatment accessibility, Online care perception, Telehealth
Highlights
-
•
Impressions of the program, the therapists, and the technology were positive.
-
•
Most participants had increased confidence to handle their symptoms after completion.
-
•
Low motivation to complete modules and homework assignments was cited as a concern.
1. Introduction
1.1. Background
Mental health concerns have increased substantially over the last few years. The lifetime prevalence of mental health disorders has reached nearly 50% (Kessler et al., 2007) and 1 in 5 Canadians is diagnosed with a mental health disorder every year (Ahmad et al., 2015). The high demand for care has left the Canadian healthcare system overwhelmed, demonstrated by long service wait times (CMHO, 2020) and annual economic costs of over 50 billion CAD annually (Lim et al., 2008). The inability to meet patient needs has highlighted the importance of developing new and innovative solutions. In response to the gaps exacerbated by restrictions related to the COVID-19 pandemic, there has been a rapid expansion in the development and use of digital mental health interventions (DMHIs) (Gooding, 2019; Sorkin et al., 2021). Additionally, the concomitant increase in mental health concerns like anxiety and depression during this time necessitated scalable treatment methods. DMHIs can support personalized patient care, reduce inequities, and improve treatment accessibility (Gratzer et al., 2021). Indeed, many healthcare organizations and clinicians, have integrated the use of virtual care platforms into their practices, translating into large-scale shifts and substantial increases in patient visits (Gratzer et al., 2021).
DMHIs encompass various formats and are frequently disseminated via smartphones, the internet, and augmented or virtual reality (Mohr et al., 2013). Among these, internet-based interventions are the most frequently studied (Etzelmueller et al., 2020a; Wei et al., 2020; Lattie et al., 2019). Online psychotherapy interventions typically model traditional in-person psychotherapies and can vary in level of guidance, automation, and time (Baños et al., 2022). For instance, a common form of online psychotherapy is online cognitive behavioral therapy (e-CBT), which applies the widely validated principles of in-person cognitive behavioral therapy to address unbalanced thinking patterns and behaviors (Wright et al., 2019a; Alavi and Omrani, 2019). These online interventions can be fully self-guided or administered with asynchronous therapist guidance. In the latter, the therapist can interact with the patient remotely to answer any questions or concerns and provide feedback on therapy-related assignments (Wright et al., 2019a; Alavi and Omrani, 2019). Compared to in-person approaches, online psychotherapy has demonstrated several benefits, such as being resource and cost-efficient, accessible, and offering the patient the opportunity to go over therapy content at their own pace and as many times as needed (Alavi and Omrani, 2019). The online therapy experience can also be enriched through multimedia learning, online homework, and ethical tracking of patient engagement with the therapy platform (Wright et al., 2019b). Despite these benefits and the comparable efficacy between online and in-person psychotherapy interventions (Carlbring et al., 2018), the user experience (UX) with this treatment modality is typically underinvestigated (Lemon et al., 2020).
To supplement this gap, the current study investigated patient perceptions of an online psychotherapy platform. UX can delineate how an individual interacts and perceives DMHIs and is critical to enhancing and optimizing therapy content and design. For example, in a UX analysis of e-CBT for depression, users viewed the therapy format as convenient, discreet, and personalizable (Stawarz et al., 2018). Findings like these can help validate therapy design and improve treatment efficacy, effectiveness, adherence, and engagement.
1.2. Aims and objectives
The current study explored the experiences of individuals who had previously used the Online Psychotherapy Tool (OPTT). OPTT is a secure and interactive cloud-based online platform that administers diagnosis-specific therapist-guided asynchronous treatment programs (OPTT Inc, 2023). Given that this was one of the first studies to investigate participant experiences with the OPTT platform, a robust survey was developed and disseminated to capture general perceptions and features that were important to previous users.
2. Materials and methods
2.1. Study design
This cross-sectional study was reviewed for ethical compliance by the Health Sciences and Affiliated Teaching Hospitals Research Ethics Board at Queen's University in Kingston, Canada. The study used purposive sampling to recruit individuals who had previously used OPTT in research studies conducted at Queen's University. A web link to the survey description and consent letter was emailed to eligible individuals. The consent letter and survey were administered online via Qualtrics (Qualtrics, Provo, UT). Upon completion of the survey, participants would be entered into a draw to receive 1 of 20 Amazon gift cards valued at 25 CAD. Participation was voluntary and anonymous. To ensure that emails and responses were unlinked and anonymized, consenting participants provided their email in the online consent letter to be contacted for the gift card draw. Subsequently, they were sent a separate link to the email address provided to complete the survey anonymously. The survey was available from November 6, 2022, to January 8, 2023. Weekly reminders were sent during this period to encourage participation. Individuals who were not interested were instructed to send an email response to remove their names from the contact list.
Between July 18, 2019, and September 15, 2022, several clinical trials were conducted at Queen's University to investigate the efficacy of online psychotherapy programs delivered through OPTT. These online psychotherapy programs are based on widely validated CBT principles which focus on the connections between thoughts, feelings, and behaviours, identifying and modifying maladaptive thoughts and behaviours, and coping with stressful situations (Alavi and Omrani, 2019; Padesky and Greenberger, 2016; Almlöv et al., 2011). These studies provided diagnosis-specific online psychotherapy and recruited adults 18 years of age and older with a variety of psychiatric conditions, including anxiety, depression, posttraumatic stress disorder, insomnia, obsessive-compulsive disorder, bipolar disorder, binge-eating disorder, and alcohol use disorder. All diagnoses were confirmed in these trials by a psychiatrist. Additionally, some of the online psychotherapy programs specifically addressed mental health problems faced by oncology and palliative care patients, correctional workers, and people experiencing depression and anxiety related to the COVID-19 pandemic (Alavi et al., 2021a; Alavi et al., 2021b; Eadie et al., 2023; Philipp-Muller et al., 2021; Stephenson et al., 2021; Alavi et al., 2020). The programs were targeted at addressing the symptom severity of the primary diagnosis (i.e., anxiety severity for anxiety disorders, depressive symptom severity for depression, etc.). Participants with a comorbid diagnosis that met inclusion criteria for multiple programs would be enrolled in the program to address their diagnosis having the largest negative effect on their quality of life.
OPTT's online psychotherapy programs comprise 10 to 13 pre-designed weekly asynchronous psychotherapy sessions followed by homework assignments to reinforce the session's concepts. Participants submit their weekly homework assignments through the OPTT platform to their therapist, who then reviews the homework assignment and provides personalized feedback. Previous participants who completed a minimum of two OPTT psychotherapy sessions were eligible to take part in the survey.
2.2. Survey development
The post-participation self-reporting survey was developed by the research team and uploaded onto Qualtrics (Qualtrics, Provo, UT). The survey was created following an extensive literature review, consulting previously validated instruments, and reviewing qualitative data from a previous study exploring the online care needs of a subset of the participants (Moghimi et al., 2022). A sample of n = 12 research team members tested the survey and provided feedback. Following revisions, the final 35-item survey (Appendix A - Survey with Responses) captured demographic variables (10 items), mental health treatment history (3 items), use and perceptions of OPTT (9 items), general impressions of the psychotherapy program (7 items), and written reviews and feedback of the program (6 items). General impressions were measured on a 5-point Likert scale, and feedback was in the form of open-ended question responses. The validity and reliability of the final survey were not assessed.
2.3. Data analysis
Qualtrics (Qualtrics, Provo, UT) statistical analysis software was used for all descriptive analyses. Missing data were not imputed, and each item was assessed individually. Therefore, reported count percentages were relative to the total responses of the specific item. Categorical variables were reported using the frequency of responses and percentages, and continuous variables were reported as medians, means, ranges, and standard deviations. Chi-squared tests were done to evaluate any possible correlations between the demographic characteristics of participants (i.e., race, gender, employment status, etc.), completion status, and perceptions of the program. Independent sample t-tests were used to assess continuous parametric variables and Mann-Whitney U tests were used to assess continuous non-parametric variables at a significance level of α = 0.05. Quantitative analysis was conducted using IBM SPSS Statistics for Mac, version 24 (IBM Corp., Armonk, NY, USA). All analyses were conducted by co-authors not affiliated with OPTT Inc.
3. Results
3.1. Participants
The survey was sent to 352 eligible participants. Of these, 22 individuals asked to be removed from the contact list and explicitly indicated that they did not want to participate in the survey. No specific reason was indicated. Due to ethical and confidentiality reasons, only demographic data from those consenting to partake in the survey study were captured. In total, 163 responses were recorded (response rate = 46.3 %, completion rate = 89.6 %; n = 147/163) from previous users of the OPTT platform between November 6, 2022, and January 9, 2023. The average age of participants was 41.9 (SD = 14.6) years, ranging between 19 and 75 years. At the time of the survey, 71.2 % of participants (n = 116/162) were employed, and 52.8 % (n = 85/162) did not have children. Fig. 1 displays the average household incomes of participants. Additional demographic details of the participants can be found in Table 1. There were no demographic variables with a statistically significant relation to the likelihood of completing the program.
Fig. 1.
The average annual income of participants (n = 157) represented in Canadian dollars (CAD).
Table 1.
Demographic breakdown of survey participants.
| Category | n (%) |
|---|---|
| Gender identity (n = 163) | |
| Woman | 163 (70.1) |
| Man | 44 (26.8) |
| Prefer to self-describe | 2 (1.2) |
| Non-binary | 2 (1.2) |
| Prefer not to answer | 1 (0.6) |
| Biological sex (n = 163) | |
| Female | 120 (73.2) |
| Male | 44 (26.8) |
| Ethnicity (n = 163) | |
| White (European descent) | 136 (82.9) |
| Multiethnic | 7 (4.3) |
| South Asian (Bangladeshi, Indian, Indo-Caribbean, Pakistani, Sri Lankan descent) | 5 (3.0) |
| Black (African, African Canadian, Afro-Caribbean descent) | 3 (1.8) |
| East Asian (Chinese, Japanese, Korean, Taiwanese descent) | 3 (1.8) |
| Middle Eastern (Arab, Persian, Afghan, Egyptian, Kurdish, Lebanese, Turkish descent) | 2 (1.2) |
| Latin American (Hispanic, Latin American descent) | 1 (0.6) |
| Southeast Asian (Cambodian, Filipino, Indonesian, Thai Vietnamese descent) | 1 (0.6) |
| Indigenous (First Nation, Inuk/Inuit, Métis descent) | 1 (0.6) |
| Other | 4 (2.4) |
| Prefer not to answer | 1 (0.6) |
| Marital status (n = 162) | |
| Married | 66 (40.5) |
| Single, never married | 53 (32.5) |
| Divorced | 17 (10.4) |
| Common-law | 14 (8.6) |
| Separated | 8 (4.9) |
| Widowed | 2 (1.2) |
| Other | 3 (1.8) |
| Highest level of education completed (n = 162) | |
| Bachelor's degree | 57 (35.0) |
| Diploma | 37 (22.7) |
| High school diploma | 30 (18.4) |
| Graduate degree | 24 (14.7) |
| Advanced diploma | 10 (6.1) |
| Other | 5 (3.1) |
3.2. Patient mental health intervention profile
Most participants (64.2 %; n = 104/161) were receiving medication for their mental health at the time of survey completion. Additionally, most participants (63 %; n = 102/161) had received CBT (Fig. 2) before partaking in OPTT's psychotherapy program.
Fig. 2.
Previous forms of therapy received by the participants (n = 161), not including the online program delivered through OPTT.
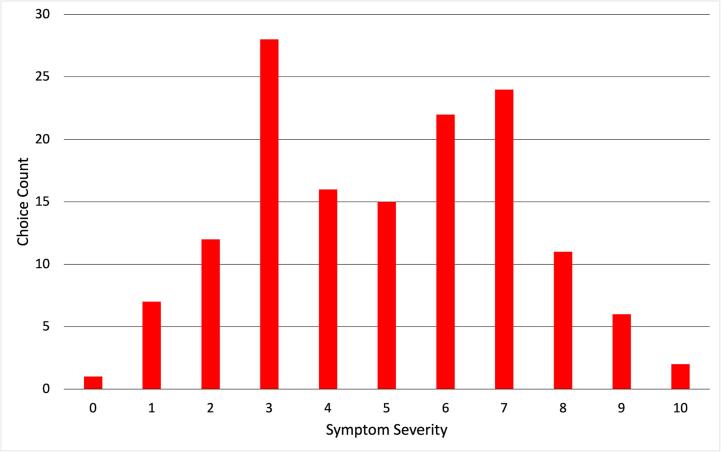
Not including OPTT, previous therapy experiences included in-person delivery (74.8 %; n = 98/131), video-call (50.4 %; n = 66/131), phone call (26.0 %; n = 34/131), in-person group therapy (22.1 % n = 29/131), online delivery with therapist support (19.1 %; n = 25/131), group video-call (14.5 %; n = 19/131), online delivery without therapist support (5.3 %; n = 7/131), and other (3.8 %; n = 5/131). A small number of participants (3.8 %; n = 5/131) reported no previous therapy experiences other than OPTT. Participants were also asked to rate the severity of their current mental health symptoms on a scale of 0–10, with 0 being the lowest possible severity, and 10 being the highest possible severity (mean = 4.92, n = 151; Fig. 3) There was no statistically significant relationship between symptom severity and year of program completion (p = 0.680; Table 2).
Fig. 3.
Participant severity rating of their current mental health symptoms, with 0 being the lowest severity, and 10 being the most severe (x-axis). The y-axis represents the participant count.
Table 2.
Relationship between the year of program completion and current self-reported symptom severity.
| Year of program completion (n = 96) | Average symptom severity (N) |
|---|---|
| 2022 | 4.88 (42) |
| 2021 | 4.36 (22) |
| 2020 | 5.40 (5) |
| 2019 | 5.00 (3) |
| 2016 | 8.00 (1) |
| Unsure | 5.25 (24) |
3.3. Treatment preferences
The programs with most enrollments on OPTT were the anxiety and depression programs (n anxiety = 100/160; n depression = 77/160) followed by posttraumatic stress disorder (n = 16/160; Table 3). Most (69.6 %; n = 111/160) participants completed all sessions in their psychotherapy program. Among non-completers, the reasons cited for stopping the program included the therapist being impersonal (n = 18/45), sessions not being engaging (n = 17/45), not seeing a change in symptoms (n = 15/45), preference for in-person format over online format (n = 15/45), not enjoying completing the homework assignments (n = 10/45), finding the homework assignments overwhelming (n = 9/45), not wanting to write as much (n = 9/45), lack of time (n = 3/45), spending too much time completing the therapy sessions (n = 3/45), personal reasons (n = 3/45), symptoms improving (n = 2/45), the program being too long (n = 1/45), and other (n = 25/45). Most participants (72.7 %; n = 111/153) accessed OPTT through their computer, with 20.8 % (n = 32/153) using their cellphones, 5.8 % (n = 9/153) using their tablets, and 0.6 % (n = 1/153) using another type of device.
Table 3.
OPTT psychotherapy programs survey respondents were enrolled in.
| Program (n = 160) | n (%) |
|---|---|
| Anxiety | 100 (62.1) |
| Depression | 77 (47.8) |
| Posttraumatic stress disorder | 16 (9.9) |
| Insomnia | 10 (6.2) |
| obsessive-compulsive disorder | 10 (6.2) |
| correctional workers and other public safety personnel | 9 (5.6) |
| Oncology and palliative care | 8 (5.0) |
| COVID-19 | 5 (3.1) |
| Bipolar disorder | 2 (1.2) |
| Binge-eating disorder | 1 (0.6) |
| Relapse prevention | 1 (0.6) |
| Other | 2 (1.2) |
| Unsure | 11 (8.5) |
3.4. Post-treatment perception
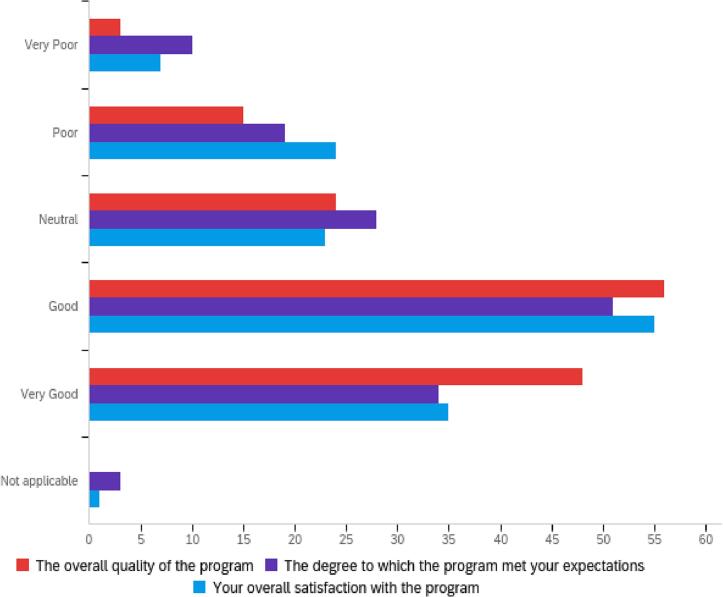
Upon completion of the program, 60.6 % (n = 94/154) of participants said they preferred in-person psychotherapy to other delivery mediums. Moreover, 38.7 % (n = 60/154) preferred to interact with their therapist through video call, 21.9 % (n = 34/154) preferred phone call interaction, 14.2 % (n = 22/154) preferred online text only, 12.3 % (n = 19/154) had no preference, 2.6 % (n = 4/154) selected “other,” and 9.0 % (n = 14/154) were unsure. Most participants rated their perceptions of the online psychotherapy programs (Fig. 4), exercises, and homework assignments (Fig. 5) as good. Additional perceptions of the technology, therapists, sessions, and long-term effects of the program can be seen in Table 4. Fig. 6 details participants' agreement with various statements regarding the skills covered in the program.
Fig. 4.
Participants (n = 153) general impressions of the online psychotherapy program. The x-axis represents the number of respondents for each impression (y-axis).
Fig. 5.
Participants (n = 148) impressions of the exercises and homework assignments. The x-axis represents the number of respondents for each impression (y-axis).
Table 4.
Participants overall perceptions of the technology, therapists, sessions, and long-term treatment effects. Values represent the percentage of participants for each category.
| Very poor-poor | Neutral/not applicable | Good-very good | |
|---|---|---|---|
| General impressions of the technology (n = 153) | |||
| General experience using the platform | 17.5 | 16.9 | 65.6 |
| User-friendliness of the platform | 16.3 | 15.7 | 68.0 |
| Ability to access the program without significant technical barriers | 7.8 | 16.3 | 75.8 |
| Helpfulness of the IT support | 3.9 | 61.0 | 35.1 |
| General impressions of interactions with the therapist(s) (n = 149) | |||
| Quality and relevance of the therapist feedback | 16.8 | 15.4 | 67.8 |
| Helpfulness of the therapist | 12.7 | 23.3 | 64.0 |
| Overall experience working with the therapist | 12.1 | 20.1 | 67.8 |
| Degree of comfort disclosing to the therapist | 10.1 | 15.4 | 74.5 |
| Degree of empathy displayed by the therapist | 9.3 | 18.7 | 72.0 |
| Availability of the therapist | 8.1 | 27.5 | 64.4 |
| Therapists ability to guide participants through the program | 8.0 | 21.3 | 70.7 |
| Ease of understanding the therapists feedback | 7.4 | 12.2 | 80.4 |
| Confidence in the therapists knowledge | 4.0 | 25.5 | 70.5 |
| The speed at which the therapist provided feedback | 2.0 | 16.7 | 81.3 |
| General impressions of the online psychotherapy sessions (n = 149) | |||
| Motivation to complete the sessions | 26.7 | 22.0 | 51.3 |
| Helpfulness of information received to effectively deal with mental health problems | 18.7 | 18.0 | 63.3 |
| Overall impression of the sessions | 18.7 | 17.3 | 64.0 |
| Relevance of the sessions to mental health problems | 15.4 | 16.8 | 67.8 |
| Impressions about receiving new sessions once per week | 9.3 | 21.3 | 69.3 |
| Appropriateness of the time spent on each session | 8.7 | 23.3 | 68.0 |
| Appropriateness of the number of sessions | 8.0 | 30.7 | 61.3 |
| Clarity of the information in each session | 5.3 | 8.0 | 86.7 |
| Appropriateness of the order of sessions | 2.7 | 25.3 | 72.0 |
| General impressions of the long-term effects of the program (n = 148) | |||
| Likelihood to reference the material covered in the future | 42.6 | 29.1 | 28.4 |
| Likelihood to repeat the program in the future if seeking help | 40.3 | 23.5 | 36.2 |
| Likelihood that positive outcomes of the program will be sustained | 23.0 | 33.1 | 43.9 |
| Likelihood to recommend the program to someone else in the future | 22.8 | 24.8 | 52.3 |
| Likelihood to seek more treatment in the future | 4.0 | 23.5 | 72.5 |
Fig. 6.
Participants (n = 148) agreement with statements regarding the skills taught in the online psychotherapy program. Values represent the percentage of participants for each category.
Most (49.0 %, n = 75/152) participants said they were more confident in their ability to manage their mental health symptoms after completing the program, with 29.4 % (n = 45/152) saying no, and 21.6 % (n = 33/152) being unsure. Most participants (75.6 %) did not experience any unwanted negative events related to the program's online format.
4. Discussion
The current study explored the UX and treatment perceptions of OPTT users. Overall, participants were pleased with the therapy and reported therapeutic benefits. Most participants considered their interactions with the therapists to be positive. Some concerns over the helpfulness and relevance of the therapy content were highlighted by participants, as well as some citing low motivation levels to complete weekly sessions. The survey results also provided critical information to support program development, such as improving skills covered in the psychotherapy programs.
Despite the benefits of online psychotherapy and the generally positive user perceptions, asynchronous delivery may impact perceptions of and motivation to participate in the program (Schmidt et al., 2019; Fernandez et al., 2015; Kobak et al., 2017). In line with previous studies (Stawarz et al., 2018; Pedersen et al., 2020), the UX survey presented a mixed response regarding motivation to complete the online therapy sessions and homework assignments. Half of the participants reported good or very good motivation levels; the other half ranged from neutral to poor and very poor. Future studies should investigate therapy components associated with low motivation among users. Focusing on engagement, other programs have used group chats (Hucker and McCabe, 2015), video games (Lohse et al., 2013), and more periodic reminders (Schneider et al., 2013) to increase patient motivation and treatment adherence in online psychotherapy programs. Individuals who completed online psychotherapy programs previously have cited an enhanced feeling of control, a sense of duty to themselves and the research team, and a sense of needing to complete a task as motivating factors (Donkin and Glozier, 2012). Future iterations of the OPTT program should consider methods to increase participants' accountability without sacrificing autonomy.
A preference for in-person versus online therapy was also observed - a sentiment that is commonly reported in the literature (Holst et al., 2017; Richardson et al., 2020a). While the benefits of online psychotherapy have been noted previously in the literature, the low uptake of online resources from the general population highlights the need for better promotion of these interventions (Richardson et al., 2020a). Factors associated with this preference include the therapist-patient therapeutic relationship and perceptions of the level of personalized care (Casey and Clough, 2015). Previous work has found that while patients have a generally positive view of online psychotherapy, comparing it to its in-person counterpart reveals a lack of therapist rapport as a limiting factor, particularly during the transition to online care during the COVID-19 pandemic (Richardson et al., 2020b; Giordano et al., 2022). The current findings further highlight the need to find a more optimal balance between face-to-face interaction and asynchronous delivery (Etzelmueller et al., 2020b). One way to accomplish this can be through a stepped-care model where the intensity of treatment (i.e., therapist interaction) is personalized to each patient (Nicholas et al., 2019; Mohr et al., 2019; Cornish, 2020). This could involve having various levels of treatment intensity ranging from fully asynchronous delivery, scaling up to asynchronous delivery with some therapist interaction, to fully synchronous delivery with a therapist, depending on each patient's needs. To maintain the scalability benefits of online psychotherapy when personalizing care level, automating this intensity decision can be used (Saarni et al., 2022; Ah Lee, 2018; Jacobson and Nemesure, 2021; Matson et al., 2022) Accordingly, OPTT has recently begun using artificial intelligence (AI) technologies to determine the appropriate level of therapist involvement for each user based on their symptomatology level (Rodrigues et al., 2022). Similarly, a review from Graham and colleagues highlights the utility of AI in the mental healthcare system, allowing for more objective measurement of patient progress and classification, personalizing treatment plans, and automating patient monitoring (Graham et al., 2019).
Concerning long-term perceptions of the program, many participants were unlikely to use the therapy material in the future or use the platform again. Nevertheless, nearly three-quarters of participants said they were likely to seek more treatment in the future. This suggests that even if they were unlikely to use OPTT again, most participants were open to receiving additional psychiatric treatment in the future. In contrast, treatment-seeking behaviours are typically low in people with mental health problems (Henderson et al., 2013). This result may be associated with the widely reported accessibility and convenience of online psychotherapy, which has been found to have a destigmatizing effect (Goh et al., 2021). However, it is important to recognize the inherent bias of this assumption as the sample of users who used OPTT and chose to complete this survey may be conformed by individuals with strong help-seeking behaviours (Haapea et al., 2007).
This study is one of the few that has directly investigated the UX of end-users for online mental health interventions, and the most robust investigation into the OPTT platform specifically (Pedersen et al., 2020; Apolinário-Hagen et al., 2017; Lillevoll et al., 2013). Previous work has mainly investigated usage rates and patterns, with some comparisons between the patient perception of general online versus in-person mental health care (Richardson et al., 2020a; Richardson et al., 2020b; Giordano et al., 2022). However, this current study provides true novelty in the in-depth investigation into one specific online platform and a focus on patient perceptions of various aspects of care. Despite its novelty, the study's limitations must be addressed. First, the ethnicity of this sample was predominantly cisgender white (European descent) and well-educated (bachelor's degree or higher) Additional efforts are needed to understand the unique needs of equity-seeking and equity-deserving groups and provide more equitable and accessible mental healthcare (Moagi et al., 2021; Myers, 2019; Memon et al., 2016). Since members of these groups face significant barriers to accessing mental health care including language, physical, and cultural barriers (Moagi et al., 2021; Myers, 2019; Memon et al., 2016), recruiting these groups is essential for informing inclusive and equitable programs. Additionally, the survey did not include a demographic question regarding sexual orientation, another important study variable that will be incorporated into future versions of this survey to better understand the perspectives of marginalized groups (Moagi et al., 2021). Finally, the validity and reliability of the survey were not assessed in this study, despite going through several iterations of construction and revision by a group of qualified team members. However, the main goal of this survey was to be exploratory, providing insight into participant perceptions of online care and any potential demographic trends that came with these perceptions. The findings should be interpreted accordingly, and future work will be done to assess the validity and reliability of this survey.
4.1. Conclusions
This study found that the overall perception and impression of the online psychotherapy program delivered through OPTT was generally positive, citing beneficial therapist interaction, easy-to-comprehend and complete homework assignments, and relatable and engaging content. Most survey participants reported that they left the program feeling more confident in their ability to manage their mental health symptoms. Though participants were mixed in their motivation to complete the online therapy sessions and homework assignments, most reported a preference for in-person therapy, suggesting further emphasis needs to be made on adapting the program to support consistent engagement and motivation week-to-week. The scalability benefits of online psychotherapeutic interventions are promising as the demand for high-quality care continues to grow. As these programs become further refined over time, they can continue to contribute to supporting the healthcare system as an effective treatment option for patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
NA and MO co-founded the Online Psychotherapy Tool (i.e., OPTT) and have ownership stakes in OPTT Inc. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2023.100623.
Contributor Information
Callum Stephenson, Email: callum.stephenson@queensu.ca.
Elnaz Moghimi, Email: elnaz.moghimi@queensu.ca.
Gilmar Gutierrez, Email: gilmar.gutierrez@queensu.ca.
Jasleen Jagayat, Email: 21jkj2@queensu.ca.
Georgina Layzell, Email: 22gl6@queensu.ca.
Charmy Patel, Email: 12cp42@queensu.ca.
Mohsen Omrani, Email: mohsen@optt.ca.
Nazanin Alavi, Email: nazanin.alavi@queensu.ca.
Appendix A. Supplementary data
Supplementary material
References
- Ah Lee S.K. Classification of SmartMentalTech services and application for comprehensive mental healthcare stepped-care model (CMHSCM): health psychological approach. Procedia Comput. Sci. 2018;141:302–310. [Google Scholar]
- Ahmad S., Briante C., Khan M., Smetanin P., Stiff D. Canadian Electronic Library; 2015. The life and economic impact of major mental illnesses in Canada. [Google Scholar]
- Alavi N., Omrani M. Springer; 2019. Online Cognitive Behavioral Therapy: An E-mental Health Approach to Depression and Anxiety. [Google Scholar]
- Alavi N., et al. Using the online psychotherapy tool to address mental health problems in the context of the COVID-19 pandemic: protocol for an electronically delivered cognitive behavioral therapy program. JMIR Res. Protoc. 2020;9 doi: 10.2196/24913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alavi N., et al. Delivering an online cognitive behavioural therapy program to address mental health challenges faced by correctional workers and other public safety personnel: protocol. JMIR Res. Protoc. 2021 doi: 10.2196/30845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alavi N., et al. Feasibility and efficacy of delivering cognitive behavioral therapy through an online psychotherapy tool for depression: protocol for a randomized controlled trial. JMIR Res. Protoc. 2021;10 doi: 10.2196/27489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almlöv J., et al. Therapist effects in guided internet-delivered CBT for anxiety disorders. Behav. Cogn. Psychother. 2011;39:311–322. doi: 10.1017/S135246581000069X. [DOI] [PubMed] [Google Scholar]
- Apolinário-Hagen J., Vehreschild V., Alkoudmani R.M. Current views and perspectives on E-mental health: an exploratory survey study for understanding public attitudes toward internet-based psychotherapy in Germany. JMIR Ment. Health. 2017;4 doi: 10.2196/mental.6375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baños R.M., Herrero R., Vara M.D. What is the current and future status of digital mental health Interventions? Span. J. Psychol. 2022;25 doi: 10.1017/SJP.2022.2. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018;47:1–18. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- Casey L.M., Clough B.A. The Psychology of Social Networking. Vol. 1. De Gruyter Open; 2015. 8. Making and keeping the connection: improving consumer attitudes and engagement in e-mental health interventions; pp. 90–103. [DOI] [Google Scholar]
- CMHO . 2020. CMHO Report on Wait Lists and Wait Times for Children and Youth Mental Health Care in Ontario. [Google Scholar]
- Cornish P. Springer International Publishing; 2020. Stepped Care 2.0: A Paradigm Shift in Mental Health. [DOI] [Google Scholar]
- Donkin L., Glozier N. Motivators and motivations to persist with online psychological interventions: a qualitative study of treatment completers. J. Med. Internet Res. 2012;14 doi: 10.2196/jmir.2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eadie J., et al. Developing and implementing a web-based relapse prevention psychotherapy program for patients with alcohol use disorder: protocol for a randomized controlled trial. JMIR Res. Protoc. 2023;12 doi: 10.2196/44694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etzelmueller A., et al. Effects of internet-based cognitive behavioral therapy in routine care for adults in treatment for depression and anxiety: systematic review and meta-analysis. J. Med. Internet Res. 2020;22 doi: 10.2196/18100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etzelmueller A., et al. Effects of internet-based cognitive behavioral therapy in routine Care for Adults in treatment for depression and anxiety: systematic review and meta-analysis. J. Med. Internet Res. 2020;22 doi: 10.2196/18100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez E., Salem D., Swift J.K., Ramtahal N. Meta-analysis of dropout from cognitive behavioral therapy: magnitude, timing, and moderators. J. Consult. Clin. Psychol. 2015;83:1108–1122. doi: 10.1037/ccp0000044. [DOI] [PubMed] [Google Scholar]
- Giordano C., Ambrosiano I., Graffeo M.T., Caro A.D., Gullo S. Research in Psychotherapy: Psychopathology, Process and Outcome. Vol. 25. 2022. The transition to online psychotherapy during the pandemic: a qualitative study on patients’ perspectives. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh Y.-S., Ow Yong Q.Y.J., Tam W.-S.W. Effects of online stigma-reduction programme for people experiencing mental health conditions: a systematic review and meta-analysis. Int. J. Ment. Health Nurs. 2021;30:1040–1056. doi: 10.1111/inm.12893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gooding P. Mapping the rise of digital mental health technologies: emerging issues for law and society. Int. J. Law Psychiatry. 2019;67 doi: 10.1016/j.ijlp.2019.101498. [DOI] [PubMed] [Google Scholar]
- Graham S., et al. Artificial intelligence for mental health and mental illnesses: an overview. Curr. Psychiatry Rep. 2019;21:116. doi: 10.1007/s11920-019-1094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratzer D., et al. Our digital moment: innovations and opportunities in digital mental health care. Can. J. Psychiatry Rev. Can. Psychiatr. 2021;66:5–8. doi: 10.1177/0706743720937833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haapea M., et al. Non-participation may bias the results of a psychiatric survey. Soc. Psychiatry Psychiatr. Epidemiol. 2007;42:403–409. doi: 10.1007/s00127-007-0178-z. [DOI] [PubMed] [Google Scholar]
- Henderson C., Evans-Lacko S., Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am. J. Public Health. 2013;103:777–780. doi: 10.2105/AJPH.2012.301056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holst A., et al. Patients’ experiences of a computerised self-help program for treating depression – a qualitative study of internet-mediated cognitive behavioural therapy in primary care. Scand. J. Prim. Health Care. 2017;35:46–53. doi: 10.1080/02813432.2017.1288813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hucker A., McCabe M.P. Incorporating mindfulness and chat groups into an online cognitive behavioral therapy for mixed female sexual problems. J. Sex Res. 2015;52:627–639. doi: 10.1080/00224499.2014.888388. [DOI] [PubMed] [Google Scholar]
- Jacobson N.C., Nemesure M.D. Using artificial intelligence to predict change in depression and anxiety symptoms in a digital intervention: evidence from a transdiagnostic randomized controlled trial. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s world mental health survey initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- Kobak K.A., Wolitzky-Taylor K., Craske M.G., Rose R.D. Therapist training on cognitive behavior therapy for anxiety disorders using internet-based technologies. Cogn. Ther. Res. 2017;41:252–265. doi: 10.1007/s10608-016-9819-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattie E.G., et al. Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J. Med. Internet Res. 2019;21 doi: 10.2196/12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemon C., Huckvale K., Carswell K., Torous J. A narrative review of methods for applying user experience in the design and assessment of mental health smartphone interventions. Int. J. Technol. Assess. Health Care. 2020;36:64–70. doi: 10.1017/S0266462319003507. [DOI] [PubMed] [Google Scholar]
- Lillevoll K.R., et al. Patients’ experiences of helpfulness in guided internet-based treatment for depression: qualitative study of integrated therapeutic dimensions. J. Med. Internet Res. 2013;15 doi: 10.2196/jmir.2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim K.-L., Jacobs P., Ohinmaa A., Schopflocher D., Dewa C.S. A new population-based measure of the economic burden of mental illness in Canada. Chronic Dis. Can. 2008;28:92–98. [PubMed] [Google Scholar]
- Lohse K., Shirzad N., Verster A., Hodges N., Van der Loos H.F.M. Video games and rehabilitation: using design principles to enhance engagement in physical therapy. J. Neurol. Phys. Ther. 2013;37:166. doi: 10.1097/NPT.0000000000000017. [DOI] [PubMed] [Google Scholar]
- Matson L.M., Adler A.B., Quartana P.J., Thomas C.L., Lowery-Gionta E.G. Management of Acute Stress Reactions in the military: a stepped care approach. Curr. Psychiatry Rep. 2022;24:799–808. doi: 10.1007/s11920-022-01388-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memon A., et al. Perceived barriers to accessing mental health services among black and minority ethnic (BME) communities: a qualitative study in Southeast England. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2016-012337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moagi M.M., Wath A.E.van D., Jiyane P.M., Rikhotso R.S. Mental health challenges of lesbian, gay, bisexual and transgender people: an integrated literature review. Health SA Gesondheid. 2021;26 doi: 10.4102/hsag.v26i0.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghimi E., et al. A qualitative exploration of the mental health challenges and therapeutic needs of Canadian correctional workers. Front. Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.1004143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D.C., Burns M.N., Schueller S.M., Clarke G., Klinkman M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. Gen. Hosp. Psychiatry. 2013;35:332–338. doi: 10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D.C., et al. A randomized noninferiority trial evaluating remotely-delivered stepped care for depression using internet cognitive behavioral therapy (CBT) and telephone CBT. Behav. Res. Ther. 2019;123 doi: 10.1016/j.brat.2019.103485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers C.R. Using telehealth to remediate rural mental health and healthcare disparities. Issues Ment. Health Nurs. 2019;40:233–239. doi: 10.1080/01612840.2018.1499157. [DOI] [PubMed] [Google Scholar]
- Nicholas J., et al. Stepping up: predictors of ‘Stepping’ within an iCBT stepped-care intervention for depression. Int. J. Environ. Res. Public Health. 2019;16:4689. doi: 10.3390/ijerph16234689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OPTT Inc . 2023. A digital mental health platform for efficient delivery of supervised digital therapies.https://www.optt.ca/ [Google Scholar]
- Padesky C.A., Greenberger D. Guilford Press; 2016. The Clinician's Guide to CBT Using Mind Over Mood. [Google Scholar]
- Pedersen M.K., Mohammadi R., Mathiasen K., Elmose M. Internet-based cognitive behavioral therapy for anxiety in an outpatient specialized care setting: a qualitative study of the patient’s experience of the therapy. Scand. J. Psychol. 2020;61:846–854. doi: 10.1111/sjop.12665. [DOI] [PubMed] [Google Scholar]
- Philipp-Muller A.E., et al. Combining ketamine and internet-based cognitive behavioral therapy for the treatment of posttraumatic stress disorder: protocol for a randomized controlled trial. JMIR Res. Protoc. 2021;10 doi: 10.2196/30334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson C.G., Slemon A., Gadermann A., McAuliffe C., Thomson K., Daly Z., Salway T., Currie L.M., David A., Jenkins E. Use of asynchronous virtual mental health resources for COVID-19 pandemic-related stress among the general population in Canada: cross-sectional survey study. JMIR. 2020;22 doi: 10.2196/24868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson C.G., Slemon A., Gadermann A., McAuliffe C., Thomson K., Daly Z., Salway T., Currie L.M., David A., Jenkins E. Use of asynchronous virtual mental health resources for COVID-19 pandemic-related stress among the general population in Canada: cross-sectional survey study. J. Med. Internet Res. 2020;22 doi: 10.2196/24868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues S.M., et al. Digital health-enabled community-centered care: scalable model to empower future community health workers using human-in-the-loop artificial intelligence. JMIR Form. Res. 2022;6 doi: 10.2196/29535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarni S., et al. 2022. The Finnish therapy navigator – Digital support system for introducing stepped care in Finland. [Google Scholar]
- Schmidt I.D., Forand N.R., Strunk D.R. Predictors of dropout in internet-based cognitive behavioral therapy for depression. Cogn. Ther. Res. 2019;43:620–630. doi: 10.1007/s10608-018-9979-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider F., de Vries H., Candel M., van de Kar A., van Osch L. Periodic email prompts to re-use an internet-delivered computer-tailored lifestyle program: influence of prompt content and timing. J. Med. Internet Res. 2013;15 doi: 10.2196/jmir.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorkin D.H., et al. Rise in use of digital mental health tools and Technologies in the United States during the COVID-19 pandemic: survey study. J. Med. Internet Res. 2021;23 doi: 10.2196/26994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stawarz K., Preist C., Tallon D., Wiles N., Coyle D. User experience of cognitive behavioral therapy apps for depression: an analysis of app functionality and user reviews. J. Med. Internet Res. 2018;20 doi: 10.2196/10120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson C., et al. Using electronically delivered therapy and brain imaging to understand obsessive-compulsive disorder pathophysiology: protocol for a pilot study. JMIR Res. Protoc. 2021;10 doi: 10.2196/30726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei N., et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J. Zhejiang Univ.-Sci. B. 2020;21:400–404. doi: 10.1631/jzus.B2010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright J.H., Mishkind M., Eells T.D., Chan S.R. Computer-assisted cognitive-behavior therapy and Mobile apps for depression and anxiety. Curr. Psychiatry Rep. 2019;21:62. doi: 10.1007/s11920-019-1031-2. [DOI] [PubMed] [Google Scholar]
- Wright J.H., et al. Computer-assisted cognitive-behavior therapy for depression: a systematic review and meta-analysis. J. Clin. Psychiatry. 2019;80:3573. doi: 10.4088/JCP.18r12188. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material