ABSTRACT
The conditions of health-care professionals including dental fraternity have been extremely affected during the COVID-19 pandemic. Dental care workers have suspended all routine dental activities with the fear of transmission of the virus from aerosol-generating dental procedures. They have also stood with medical care professionals as frontline warriors because of the exponentially overburdened of the COVID-19-positive patients worldwide. With the available literature, the aim of this article is to address the trajectories of the life of oral health workers during the outbreak of COVID-19 as well as to analyze what measures shall be taken to improve their overall physical, mental, social, and economic health and precautions while working in dental environment.
Keywords: COVID-19, dental care workers, frontline warriors, quality of life
INTRODUCTION
Severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) outspreads from person to person through close contact and gives rise to COVID-19. It is highly contagious and can communicate primarily through droplets and fomites.[1] In addition, it spreads by nasal or salivary discharge when a person sneezes or coughs on a nearby person.[2] The World Health Organization on March 11, 2020, has declared SARS-CoV-2 as a pandemic due to its global spread. As of November 8, 2020, more than 49.7 million people globally have been infected with more than 1.2 million deaths.[3]
Coronaviruses are enveloped, positive-sense, single-stranded RNA viruses having a glycoprotein spike on its surface. During infection, this glycoprotein mediates in binding of acetyl-converting enzyme-2 receptor and facilitates the cell entry.[1] The span of the COVID-19 incubation period is from 2 to 12 days with a mean of ~ 6.4 days.[4]
The clinical outcomes after exposure to SARS-CoV-2 can vary from asymptomatic infection to mild flu to severe acute respiratory distress and death. Substantial pressures on health-care systems have been put for COVID-19 patients. It has also disrupted non-COVID-19 health-care sector including the dental profession.[1]
The activity of dentists has been negatively impacted during the COVID-19 outbreak. The possibility of cross-infection during dental care is high; hence, routine dental activities have been suspended.[5] The dental students are also restricted to attend preclinics, clinical skills, no grant to research work, cancellation of academic conferences, and graduation ceremonies.[6] Besides, the number of COVID-19 cases is rising exponentially; therefore, dentists also stand as frontline warriors with the medical fraternity.[7] As a result, the fear of being getting infected with COVID-19, the imposition of nationwide lockdown, cancellation of previous appointments, great revenue loss, have created psychological tension in the form of stress, depression, and anxiety, among dentists.[6]
Social distancing, avoiding crowding, taking extra measures to maintain personal cleanliness, facing limitations to perform their daily activities, keeping updates of COVID-19 reports, bounding to do work from home, are some of the preventive measures which are taken to reduce the transmission of COVID-19 infection. It results in the deterioration of social and physical being and hampers the quality of life.[8]
This article aims to describe the stress faced by the dental community in India due to coronavirus, impairment of quality of life, and measures to reduce psychosocial tension. Furthermore, it also aims to analyze what precautions must be taken to prevent the cross-transmission of the virus while performing dental activities as the nation is being undergoing phase-wise unlocking.
MATERIALS AND METHODS
Search strategy for study identification
The electronic database platform including PubMed, Google Scholar, Cochrane library, and Internet access was utilized to perform the literature search for COVID-19. Either medical subject heading terms or identical terms/keywords were employed to explore such terms. The search terms were then consolidated with an “OR” and PICO categories and finally assimilated using “AND” to produce a reasonable query. Ultimately, to yield the results, specific databases were adjusted.
Eligibility criteria
All human studies, irrespective of study design, to evaluate the impact of COVID-19 on dental care workers, were included. The population could be living in any community. Studies excluded were (i) impact on oral health workers other than COVID-19 and (ii) non-English articles.
Study selection and data collection
A total of 31 articles were identified in the preliminary search. Six articles were removed due to duplicity, while eight were excluded during the screening. Out of them, a total of nine scientific research articles including available internet data and guidelines issued by recognized dental bodies were incorporated. The remaining eight excluded articles were in foreign languages [Figure 1].
Figure 1.
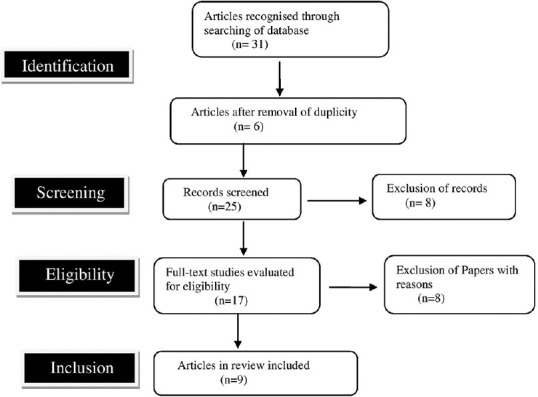
Systematic review diagram showing the study selection process for adapted desired reporting items
Summary measures
The primary outcome of this study was to measures the effects of COVID-19 on the life of dental care workers in terms of (1) psychological and economic impact and (2) quality of life. The secondary measures included education to reduce stress and precautions while working in dental environment.
JOURNEY OF DENTAL CARE WORKERS DURING THE COVID-19 PANDEMIC
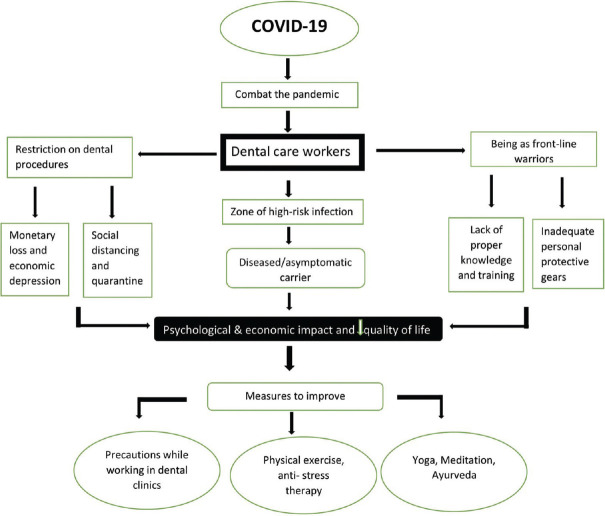
With the available literature, we have described the journey of dental fraternity during the COVID-19 outbreak with their possible preventive measures [Figure 2] in more detail in the following sub-sections. The analysis of various studies is given in Table 1.
Figure 2.
Schematic diagram illustrating the impacts of the COVID-19 outbreak on dental care workers and its possible management
Table 1.
Summaries of various studies
| Author’s name | Type of study | Number of participants/studies | Conclusion |
|---|---|---|---|
| Pascoe et al., 2017[8] | Meta-analysis | 42 studies | Yoga asanas appear to be associated with improved regulation of the sympathetic nervous system and hypothalamic–pituitary–adrenal system in various populations |
| Fong et al., 2020[9] | Cross sectional study | 590 participants | Approximately one-third of the participants (29.7%) had moderate-to-severe depression, and participants aged 18 to 25 were found to have higher scores in PHQ-9 |
| Peng et al., 2020[10] | Review | The participants in dental practice are exposed to tremendous risk of 2019-nCoV infection due to face-to-face communication, exposure to bodily fluids, and handling of sharp instruments | |
| Barabari and Moharamzadeh, 2020[11] | Review | COVID-19 has had many immediate complications for dentistry, of which some may have further long-term impacts on clinical practice, dental education, and dental research | |
| Stojanov et al., 2021[12] | Cross-sectional study | 201 HCWs | Poor QoS and HRQoL correlated with high health anxiety and severe depressive symptoms and several demographic characteristics |
| Nguyen et al., 2020[13] | Prospective cohort study | Among 2,035,395 community individuals and 99,795 frontline HCWs | Compared with the general community, frontline HCWs had a HR of 11·6 (95% CI: 10·9-12·3) for reporting a positive test. Frontline HCWs had a significantly increased risk of COVID-19 infection, highest among HCWs who reused PPE or had inadequate access to PPE |
| Suryavanshi et al., 2020[14] | Online survey | 197 HCWs | Demonstrated a high prevalence of symptoms of depression and anxiety and low QoL among Indian HCPs during the COVID-19 pandemic |
| Izzetti et al., 2020[15] | Review | 3 studies | Importance of infection control is crucial in limiting the effects of virus diffusion |
| Fallahi et al., 2020[16] | Review | A comprehensive protocol should be followed for managing possible exposure to patients or those suspected of having coronavirus |
PHQ: Patient Health Questionnaire, QoS: Quality of sleep, HRQoL: Health-Related Quality of Life, HR: Hazards ratio, CI: Confidence interval, HCPs: Health-care professionals, QOL: Quality of Life, HCWs: Health-care workers, COVID-19: Coronavirus disease 2019
The psychological and economic impact of COVID-19 on dentists and dental students
The COVID-19 pandemic is a remarkable psychological and physiological stressor for individuals, as well as health-care workers (HCWs) including dental workers across worldwide. Stress can be termed as “feeling of emotional and physical tension which arises from any event that threatens our homeostasis.”[17] While “the fear of the unknown is called as anxiety,” that is the inherent body response to stress.[18] Depression is explained as a state of detachment in routine activities.
Even before the announcement of lockdown, dentists had restricted their routine dental procedure to reduce aerosol generation in the form of using vibrating ultrasonic, high-speed electronic devices, which are responsible for the transmission of COVID-19 infection.[19] Dentists frequently come in contact with blood, saliva, and serum that are favorable niche for the COVID-19 infection. Dental surgeons were also aware of getting an infection from asymptomatic patients as there was a lack of sufficient number of personal protective equipment (PPE).[10] Hence, during the lockdown, private dental practitioners were bound to do only emergency services and postponed all elective procedures.[19] They were also compelled to stay at home if no emergency was needed. This has eventually resulted in the economic depression.[8]
Globally, the catastrophic effects of COVID-19 pandemic on dental education including teaching and training were noticed quite early as there was a demand for social distancing as well as to avoid face-to-face contacts.[20] The ultimate goal of dental training is to educate dentists to treat their patients independently with effective and safety outcomes. To achieve the desired outcome, this profession requires lots of arrangements for dental teachers with specific training, education, and learning methodologies. Hence, the tactics used in virtual training for dental occupation particularly in clinical practices remains as an obstacle for all universities worldwide. Besides, within the given time and limited resources, the training skills gained by dental students are mentally exhausting as these need outstanding motor skills and fine manual expertise.[11]
In addition, restrictions on nonessential research projects, interruption of laboratory-based dental research activities, and postgraduate student research projects, were imposed due to obligatory government and institutional policies.[11] All the decisions have been taken to save the lives of undergraduate and postgraduate dental students by reducing their exposure from COVID-19-suspected patients.[19] Moreover, dental residents, faculties, and students in affiliated hospitals are working for the care of COVID-19-positive patients as frontline warriors with other health-care professionals (HCPs). As a result, they have also put their health at a risk.[21]
The COVID-19 crisis has also shown that we have undervalued the contribution of the groundwork, education, and services of e-oral health including teledentistry.[22] Perhaps, the expected recovery period may be prolonged and uncertainty for monetary gains, sustaining high-quality learning and training programs, and the progression of community-based oral health-care activities has increased economic and psychological stress, anxiety, and depression among the dental students and dentists globally including India.[21]
Impairment of quality of life
During the pandemic with a state of emergency lockdown, dental surgeons along with HCWs have worked under high-risk condition with limited resources. It includes social contact restriction even also from their families, friends, and well-wishers, which besides has detrimentally affected their physical, social, and emotional well-being.[12]
Being the frontline HCPs as compared with the general population, they have three times higher possibility of reporting COVID-19 test been positive.[13] Furthermore, social media coverage on COVID-19-related reports has disturbed the HCWs emotionally. They have also experienced the stigma of social isolation and anxiety, which leads to the impairment of quality of life.[14] Apart from that, they are also having a fear of transmission of the virus to their family members if they got infected or becoming an asymptomatic carrier.[12]
Due to lack of proper training, knowledge, less workforce, inadequate protective gears, and overburdened workload, HCPs have worked restlessly with lots of work engagement. This ultimately has resulted in a lower quality of sleep due to chronic mental stress.[12] More often, increased physical strain due to inadequate rest and frequent usage of electronic gadgets even in the hospitals for maintaining the records of the patients have become a cause of continuous physical stiffness such as pain in shoulder, neck, and upper extremity.[8]
Besides, as the nation is under the unlocking phase, still all dental institutes across India are only treating emergency patients as dental treatment is a multi-sitting as well as aerosol-generating procedure. The dental clinics are either not functioning properly or treating cases as suggested by the Indian Dental Association; therefore, the oral health care is crucially affected. Thus, the monetary outcome of this pandemic has increased the cost of dental treatment and has reduced the financial gains of dental institutes as well as the income of dental practitioners. Overall, this revenue loss has also led to a poor quality of life.[23]
Furthermore, recent studies have found that inflammation plays an important role in the pathophysiology of distress disorders including depression and anxiety. The study of Greco has probed the interrelation between pro- and anti-inflammatory cytokine genes which include interleukin (IL)-1b, IL-1 receptor 2, nuclear factor kappa beta 2, tumor necrosis factor alpha) and stages of anxiety.[24] Most of the reported research have also enlightened a significant relationship between higher levels of anxiety and depression and deteriorating health condition. It is usually indicated by dyspnea, fatigue, nausea, and pain, as well as poorer quality of life. In addition, fatigue impact, pain effects, and symptoms of depression and anxiety are associated with work and ruining of daily activities.[25] Overall, this has brought about a disturbance between psychological attitude and work–life balance.
Measures to improve psychological tension and quality of life
Various measures are available to reduce stress and enhance health-related quality of life including yoga, exercises, meditation, and Ayurveda. The role of yoga seems to ameliorate the physiology of stress by reducing the levels of cortisol and cytokines as well as maintaining blood pressure.[9]
Yoga includes asanas, yogic kriyas, and pranayama, which have inhibitory effects on inflammatory cytokines including IL-1, IL-6, IL-8, and C-reactive protein. Meditation along with yoga has pleiotropic effects which help in improving pulmonary function and tolerance of exercise.[26] The stimulation of vagal tone due to the anti-inflammatory, anti-stress, and anti-infectious actions of yoga and meditation (with mantra uchcharana) results in a “calm and compose” mode in the place of “flight or fight” and eventually boost up the immune system.[27]
Various vehicles of Ayurveda also intend the entry portals responsible for the nosocomial infection. In mild cases, intake of hot water, hot food, and medicinal herbs; gargling medicated water, inhalation of steam, and local applications may be beneficial for symptomatic relief or as preventive measures. The concerned plants used in Rasayana therapy and Ashwagandha may help enhance the host immunity by modulating central goals related to COVID-19.[26]
Besides, adequate physical activity with a balanced diet increases the blood circulation, detoxifies the body, and strengthens the mental and physical health.[8] The habit of handwashing at regular intervals and avoidance of facial contact is also promoted to reduce the transmission of the virus.[28]
Precautions for dental procedures
Even though dental practices are at higher risk for COVID-19 virus diffusion, certain dental procedures cannot be deferred. Therefore, it is necessary to follow precautions for dental health-care personnel to carry out these activities as per the guidelines issued by the Centers for Disease Control and Prevention on August 28, 2020[29] and the DCI on May 7, 2020.[30] Ensuring proper ventilation system in dental clinics is of utmost importance in the current pandemic situation. This can be done by maintaining air circulation with natural air through frequent opening of windows and using an independent exhaust blower to extract the room air into the atmosphere and creating a unidirectional flow of air away from the patient. An indoor portable air-cleaning system equipped with an HEPA filter and ultraviolet light is also recommended for the same.[31]
Antiseptic solution such as povidone-iodine has efficacy >99.99% against enveloped and nonenveloped viruses.[23] Hence, 0.2% to 1% povidone-iodine is recommended to patients for a preprocedural mouth rinse for 1 min. Other solutions including 1% hydrogen peroxides and 0.05% to 0.1% cetylpyridinium chloride also show promising results, whereas chlorhexidine mouthwashes are usually not advocated.[15] Hand-operated instruments such as manual scalers should be preferred over aerosol-generating devices. In cases where aerosol-generating procedures are necessary to be performed, application of rubber dam isolation and usage of high-volume evacuators (HVE) are strongly suggested to prevent the transmission of COVID-19 infection through aerosol and splatter. HVE is basically a suction device that draws a large volume of air over a period of time, as compared to low-volume evacuators which pulls a significantly lower volume of air.[28] Anti-retraction handpieces should be promoted which mitigate the dispersal and dissemination of droplets.[16] In ultrasonic scalers, 10% povidone-iodine can be employed. It can also be filled in the bottle connected to the dental chairs with a dilution of 1:9 with water.[23]
After seeing every patient, proper disinfection of the dental chair along with all the auxiliary parts within 3 feet of distance should be done, using 1% sodium hypochlorite, and the chair should be cleaned and sterilized using a cotton/gauge piece by employing an inner to outer surface approach and left for drying. New cotton/gauge piece should be used for every surface.[31] Along with proper handwashing for 60 s, dental care workers should also apply 60% to 85% isopropyl alcohol solution for hand rubs before wearing gloves. PPE including masks, protective eye shield, gowns, surgical gloves, head caps, face shields, and shoe covers are highly recommended. Proper disposal of medical waste should be done while disposing medically infectious waste.[28]
CONCLUSION
The authors conclude that the dental fraternity is also playing an integral role during this pandemic era. Moreover, this specialty is on worst hit because aerosol-generating dental procedures are limited to reduce the transmission of the virus. Eventually, oral care workers are dragging in psychological stress. On the contrary, this field is less funded and least prioritized by the government. Hence, dental care workers during their work should take extra precautions as well as do regular anti-stress therapy to improve the quality of life because the effectiveness of vaccine against COVID-19 is still undergoing research.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2:A preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396:467–78. doi: 10.1016/S0140-6736(20)31604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chu DK, Duda S, Solo K, Yaacoub S, Schunemann H. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19:A systematic review and meta-analysis. J Vasc Surg. 2020;72:1500. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Coronavirus Disease (COVID-19) Situation Weekly Epidemiological Update. [Last accessed on 2020 Nov 10]. Available from:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports .
- 4.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill. 2020;25:2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vergara-Buenaventura A, Chavez-Tuñon M, Castro-Ruiz C. The mental health consequences of coronavirus disease 2019 pandemic in dentistry. Disaster Med Public Health Prep. 2020;14:e31–4. doi: 10.1017/dmp.2020.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alzahrani SB, Alrusayes AA, Aldossary MS. Impact of COVID-19 on dental education. Int J Health Sci Res. 2020;10 [Google Scholar]
- 7.Sharma Y. Future of dentistry due to COVID-19. [Last accessed on 2020 Oct 15];Open Access J Biogeneric Sci Res. 2020 4:01. Available from:https://actascientific.com/ASDS-4-8.php . [Google Scholar]
- 8.Pascoe MC, Thompson DR, Ski CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures:A meta-analysis. Psychoneuroendocrinology. 2017;86:152–68. doi: 10.1016/j.psyneuen.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Fong BY, Wong MC, Law VT, Lo MF, Ng TK, Yee HH, et al. Relationships between physical and social behavioural changes and the mental status of homebound residents in Hong Kong during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6653. doi: 10.3390/ijerph17186653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barabari P, Moharamzadeh K. Novel coronavirus (COVID-19) and dentistry –A comprehensive review of literature. Dent J (Basel) 2020;8:E53. doi: 10.3390/dj8020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stojanov J, Malobabic M, Stanojevic G, Stevic M, Milosevic V, Stojanov A. Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. Int J Soc Psychiatry. 2021;67:175–81. doi: 10.1177/0020764020942800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen LH, Drew DA, Joshi AD, Guo CG, Ma W, Mehta RS, et al. Risk of COVID-19 among frontline healthcare workers and the general community:A prospective cohort study. Lancet Public Health. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suryavanshi N, Kadam A, Dhumal G, Nimkar S, Mave V, Gupta A, et al. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020;10:e01837. doi: 10.1002/brb3.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Izzetti R, Nisi M, Gabriele M, Graziani F. COVID-19 transmission in dental practice:Brief review of preventive measures in Italy. J Dent Res. 2020;99:1030–8. doi: 10.1177/0022034520920580. [DOI] [PubMed] [Google Scholar]
- 16.Fallahi HR, Keyhan SO, Zandian D, Kim SG, Cheshmi B. Being a front-line dentist during the COVID-19 pandemic:A literature review. Maxillofac Plast Reconstr Surg. 2020;42:12. doi: 10.1186/s40902-020-00256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Selye H. The Stress of Life. New York: McGraw-Hill; 1956. [Google Scholar]
- 18.Holland K. Anxiety:Causes, Symptoms, Treatment, and More. [Last accessed on 2018 May 24]. Available from:https://www.healthline.com/health/anxiety .
- 19.Coulthard P. Dentistry and coronavirus (COVID-19) –Moral decision-making. Br Dent J. 2020;228:503–5. doi: 10.1038/s41415-020-1482-1. [DOI] [PubMed] [Google Scholar]
- 20.Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19):Emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–7. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Emami E. COVID-19:Perspective of a dean of dentistry. JDR Clin Trans Res. 2020;5:211–3. doi: 10.1177/2380084420929284. [DOI] [PubMed] [Google Scholar]
- 22.International Association for Dental Research. e-Oral Health Network IADR. 2020. [Last accessed on 2020 Apr 03]. Available from:https://www.e-oralhealth.org/#2 .
- 23.Krishna Prasad D, Anupama Prasad D, Parakh M. Coronavirus and its impact on dental fraternity. J Health Allied Sci NU. 2020 [doi:10. 10.1055/s-0040-1713835] [Google Scholar]
- 24.Greco F, Altieri VM, Esperto F, Mirone V, Scarpa RM. Impact of COVID-19 pandemic on health-related quality of life in uro-oncologic patients:What should we wait for? Clin Genitourin Cancer. 2021;19:e63–e68. doi: 10.1016/j.clgc.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Enns MW, Bernstein CN, Kroeker K, Graff L, Walker JR, Lix LM, et al. The association of fatigue, pain, depression and anxiety with work and activity impairment in immune mediated inflammatory diseases. PLoS One. 2018;13:e0198975. doi: 10.1371/journal.pone.0198975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tillu G, Chaturvedi S, Chopra A, Patwardhan B. Public health approach of ayurveda and yoga for COVID-19 prophylaxis. J Altern Complement Med. 2020;26:360–4. doi: 10.1089/acm.2020.0129. [DOI] [PubMed] [Google Scholar]
- 27.Bushell W, Castle R, Williams MA, Brouwer KC, Tanzi RE, Chopra D, et al. Meditation and yoga practices as potential adjunctive treatment of SARS-CoV-2 infection and COVID-19:A brief overview of key subjects. J Altern Complement Med. 2020;26:547–56. doi: 10.1089/acm.2020.0177. [DOI] [PubMed] [Google Scholar]
- 28.Richards W. Being a dentist in the pandemic. Evid Based Dent. 2020;21:58–9. doi: 10.1038/s41432-020-0095-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guidance for Dental Settings, Issued by Centre for Disease Control and Prevention on 2020. Aug 28, [Last accessed on 2020 Oct 13]. Available from:https://www.cdc.gov/oralhealth/infectioncontrol/statement .
- 30.Dental Clinic Protocols Issued by Dental Council of India, on 2020. Aug 28, [Last accessed on 2020 Oct 11]. Available from:https://www.dciindia.gov.in/Admin/NewsArchives/Dental%20Clinics%20Protocols%20Final.pdf .
- 31.Guidelines for Dental Professionals in COVID-19 Pandemic Situation, Issued on 2020. May 19, [Last accessed on 2020 Oct 15]. Available from:https://www.mohfw.gov.in/pdf/DentalAdvisoryF.pdf .