ABSTRACT
Introduction:
Contemporary incisions used to access the frontozygomatic (FZ) sutures are the lateral brow and upper blepharoplasty incisions which are associated with specific limitations and complications. The authors describe the use of sub-brow incision as an alternate approach for exposure of the FZ region.
Methods:
This is a prospective cohort study involving patients requiring surgical management of zygomatico maxillary complex (ZMC) fractures with fixation at FZ suture alone or along with fixation at infra-orbital rim and/or zygomaticomaxillary buttress. A sub-brow incision was used to expose the fracture and fixation was done with a 4-hole miniplate. The parameters evaluated were specific to the FZ region (sub-brow incision), namely surgical access, bleeding, fracture exposure time, post-operative scar, and pain. Each patient was reviewed on 1st, 5th, 7th, 10th, 30th, and 90th day.
Results:
The study sample included eight male patients. The mean age was 30 years. The sub-brow incision demonstrated favorable postoperative outcomes; adequate exposure was achieved in all 8 patients. The scar formation was found to be higher on the 7th day and the least scar formation was seen by the third month. The mean pain score was found to be high on first post-operative day and the least pain was seen by the 10th day. The mean score of surgical field bleeding was found to be 1.75 which signified mild bleeding according to Fromme’s scale. The mean time taken for adequate exposure of the fracture was 6.62 min. All the assessment parameters were statistically significant (P value <0.01).
Conclusion:
Sub-brow incision is an effective approach for ORIF of zygomatic fractures at FZ suture. The technique is quick, simple, and associated with minimal complications.
Keywords: Eyebrows, fracture, maxillofacial injuries, open reduction, trauma, Zygoma
INTRODUCTION
Zygomaticomaxillary complex (ZMC) fractures constitute a higher percentage of maxillofacial trauma. Literature reveals that the greater incidence of ZMC fractures is attributed to its prominent disposition.[1] ZMC plays an important role in the maintenance of facial dimensions and the protection of the eyeball. The ZMC is composed of 4 processes and 5 articulations. The processes are temporal, frontal, maxillary, and infraorbital. The articulations include zygomatico-temporal (ZT), zygomatico-frontal (FZ), zygomatico-maxillary (ZM), spheno-zygomatic (SZ), and infraorbital. ZMC fractures are characterized by diastasis at the above-mentioned sutures, leading to variable clinical features such as deranged facial aesthetics and functional disturbances such as altered vision and limited mouth opening. Therefore, meticulous reduction and fixation of these fractures are necessary, for the ideal restoration of function and aesthetics.[2]
ORIF of ZMC fractures is challenging because of the pentapodal structure of ZMC and its articulations. Literature reveals five types of fixations of ZMC fractures namely: (1) One point fixation at ZM buttress or FZ suture, (2) Two-point fixation at ZM buttress and FZ suture, (3) Three-point fixation at ZM buttress, FZ suture and Infraorbital buttress, (4) Four-point fixation at ZM buttress, FZ suture, Infraorbital buttress, and ZT suture. (5) Five-point fixation at ZM buttress, FZ suture, Infraorbital buttress, ZT suture and SZ suture.
Studies have concluded that fixation at the FZ suture is crucial for the post-operative stability of ZMC fractures.[3-6] Presently, the incisions commonly used to access the FZ buttress are the lateral brow[7] and upper blepharoplasty incisions.[8] But these approaches are associated with cosmetic and technical limitations. The problems associated with lateral brow incision include limited surgical access to the FZ suture and the possibility of the development of an unaesthetic, linear focal alopecia along the line of incision.[9] Also, in individuals with the poor extension of the eyebrow on the lateral side, the placement of the lateral brow incision is contraindicated.[9] In contrast, the upper blepharoplasty incision ensures excellent surgical access and camouflage of scar. But the incision is technique sensitive and associated with a wide range of complications. Improper dissection following this incision is associated with the risk of breaching the orbital septum which may result in injury to the lacrimal gland and orbital fat.[10] Hematoma, lagophthalmos, wound dehiscence, asymmetry and diplopia are the other complications associated with upper blepharoplasty incision.[11]
Currently, Sub brow incision is used by plastic surgeons for cosmetic purposes like brow lift procedures.[12] In the maxillofacial field, this approach has been used for the management of supra-orbital fractures[13] and management of the nasal bone fractures.[14] There is no literature that cites the use of sub-brow incision for exposure of FZ suture for ORIF of the ZMC fractures.
The aim of this study was to assess the efficacy of the sub-brow incision in providing optimal exposure for access and fixation of ZMC fracture at the FZ suture and evaluate the surgical outcome. The authors hypothesized that sub-brow incision would provide adequate exposure of the FZ region and good post-operative outcome of ORIF of ZMC fractures at the FZ region. The study was designed as a prospective cohort study, to assess intra-operative and post-operative parameters.
The specific objectives of the study were to assess the (1) surgical access to Fronto zygomatic (FZ) suture for ORIF of ZMC fracture (2) intra-operative time needed to expose the FZ suture (3) the degree of surgical field bleeding (4) postoperative pain and (5) grade of postoperative scarring, related to FZ region (sub -brow incision).
MATERIALS AND METHODS
Study design
The following research was a prospective cohort study involving patients with traumatic injury to ZMC with separation at the frontozygomatic suture. The study received the appropriate permission from the Institutional Review Board (SRMDC/IRB/2019/MDS/No. 401). The research was carried out in compliance with the Helsinki declaration and the STROBE principles.
Hypothesis
The null hypothesis was that ORIF of ZMC fractures using sub-brow incision [Figure 1] would not provide adequate exposure of the FZ region and good surgical outcomes. The alternate hypothesis was that ORIF of ZMC fractures using sub-brow incision would provide adequate exposure of the FZ region and a good surgical outcomes.
Figure 1.

Incisions to approach FZ suture region. (a) Lateral brow incision. (b) Sub brow incision. (c) Blepharoplasty incision
Patient selection
The study was carried out on 8 patients who reported to our unit of Oral and Maxillofacial Surgery with ZMC fracture which required ORIF. Patients were explained about the procedure as well as the study and written consent was obtained for the same in English and vernacular language. The inclusion criteria consisted of the following: patients aged 20-40 years and patients with fractured ZMC requiring fixation at FZ suture alone or along with fixation at the infra-orbital rim and/or zygomaticomaxillary buttress. The exclusion criteria comprised patients above 40 years and below 20 years, patients with undisplaced or hairline fractures, not requiring ORIF of the ZMC fracture, and patients with a laceration in the eyebrow region.
Methodology
The recruited sample was evaluated in detail for the history of trauma, clinical symptoms, and signs. They were documented using a standardized case sheet format. The study was conducted and parameters were assessed as detailed below. All patients were thoroughly examined for signs and symptoms of Zygomatico-maxillary fractures by inspection and palpation [Figures 2 and 3]. Computed tomography (CT) imaging was done to assess fracture in all three sections (coronal, sagittal, and axial sections) as well as in 3D formats [Figure 4]. The patients underwent ORIF of ZMC fracture with fixation at FZ suture, under general anesthesia. A standardized surgical procedure was followed by a single surgeon (2nd author) in all the patients recruited for the study as mentioned; The surgical site was prepared with betadine solution. The sub-brow incision was marked and the FZ region was infiltrated with 2% LA (1:100,000) with adrenaline. The incision was placed with no. 15 BP blade just beneath the hairline of the eyebrow, in the shadow region; beginning from the middle of the eye- brow, till the tail of the eyebrow [Figure 5]. The incision was extended through the skin, subcutaneous tissue, orbicularis oculi muscle, and periosteum to expose the FZ suture. The incision was extended laterally when needed, without damaging any important anatomical structures and the fracture site was exposed. Fracture reduction was done using intraoral (Balasubramanian approach) or extraoral approach (Gillies approach). A 4-hole plate with a gap was contoured and adapted on the frontozygomatic process. two screws were placed on each side of the fractured site [Figure 6]. Hemostasis was achieved and layer-wise closure was done using Vicryl (3-0) for subcutaneous tissues and Prolene for the skin. Fracture patterns that required additional points of fixation were approached by transconjunctival/subsidiary incision for fixation at the infraorbital rim and vestibular incision for fixation at the zygomaticomaxillary buttress. Post-operatively, the topical antibiotic ointment was applied for the cutaneous incisions and dressing was placed. All the patients were evaluated for postoperative outcomes by clinical examination [Figures 7 and 8] and CT imaging [Figure 9].
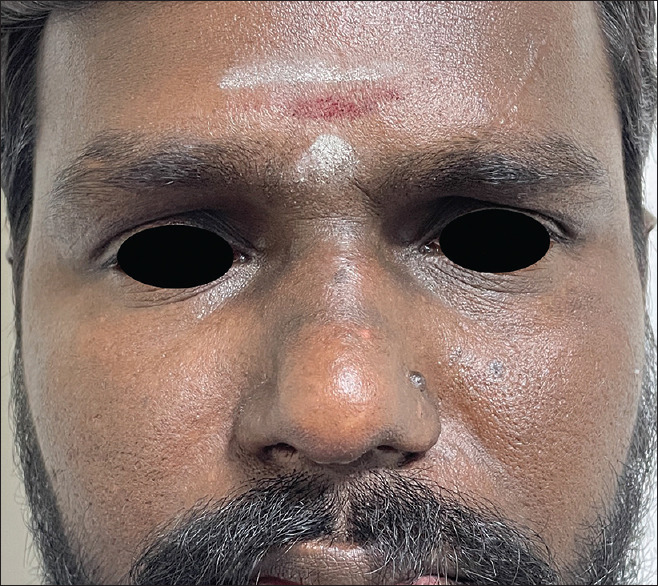
Figure 2.

Pre operative clinical picture of a patient with ZMC fracture, frontal view
Figure 3.

Pre operative clinical picture of a patient with ZMC fracture, lateral view
Figure 4.

Pre operative Computed Tomography of a patient with ZMC fracture, 3D view
Figure 5.

Intra operative placement of incision
Figure 6.

Intra operative fracture fixation
Figure 7.
Post operative clinical picture of a patient with ZMC fracture, frontal view
Figure 8.

Post operative clinical picture of a patient with ZMC fracture, lateral view
Figure 9.

Post operative Computed Tomography of a patient with ZMC fracture, 3D view
Parameters and assessment scales
The patients were assessed periodically, in the intra-operative and post-operative phases. All the assessment parameters used are detailed; The intraoperative parameters included surgical access, fracture exposure time, and surgical field (bleeding), related to the FZ region. Surgical access was defined as the exposure required to fix two screws on either side of the FZ suture. It was recorded as ‘yes’ if the exposure was achieved to fix two screws on either side of the fracture and recorded as ‘no’ if the exposure was not achieved. Fracture exposure time was defined as the time taken from placement of incision to fracture exposure, using a stop-watch. It was measured in minutes.
Surgical field (bleeding) was defined as the intra-operative bleeding that occurred during ORIF at the FZ region. It was assessed using Fromme’s scale.[15]
The post-operative parameters consisted of pain and scarring. Post-operative pain was defined as the pain and discomfort perceived by the patient in the postoperative period. All the patients were instructed to indicate the severity of pain using the Visual Analog Scale (VAS).[16] A value of 0 indicated no pain and 10 indicated severe pain.
Postoperative scar was defined as the appearance of the healed incision in the post-operative period. The assessment was done using the modified vancouver scar scale (MVSS).[17]
Review protocol
All patients were reviewed systematically for assessment parameters by the investigator as follows; Post-operative pain was reviewed in all the patients on the 1st day, 5th day, 10th day, and 30th day. Postoperative scar was reviewed in all the patients on the 7th day, 30th day, and 90th day.
Statistical tools
The findings of the normality test, the Kolmogorov–Smirnov test, and the Shapiro-Wilk test show that the study followed a normal distribution. As a result, a parametric test was used to assess the data. Descriptive statistics were done to assess the mean among the study variables. The mean values reported for all of the variables included in the study were compared using one-way ANOVA. To analyze pair-wise comparison, a post hoc test was used. Analysis of data was done using SPSS (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY: IBM Corp. Released 2019). The significance threshold was set at 5% (=0.05). P values less than 0.05 were deemed statistically significant.
RESULTS
The study sample included eight patients (all males). The mean age was 30 years, with a range of 21 to 40 years. Adequate surgical access was achieved in all the patients to fix two screws on either side of the fracture. The scar formation was found to be higher on the seventh day and the least scar formation was seen by the 90th day [Table 1]. The results demonstrated a significant variance of the mean scar scores within three time periods of review (P-value <0.01).The post hoc test revealed that the pairwise comparison of means within groups also demonstrated statistically significant variance. The mean pain score was found to be high on first day and the least pain was seen by the 30th day [Table 2]. The results demonstrated a significant variance of the mean pain scores within the three time periods of review (P value <0.001). The post hoc test revealed that the pairwise comparison of means within groups also demonstrated statistically significant variance.
Table 1.
Mean scar score demonstrated at 3-time intervals
| Variables | 7th day | 1st month | 3rd month | P |
|---|---|---|---|---|
| Mean+/-Std. deviation | 5.25+/-0.76 | 3.6+/-0.95 | 1.75+/-0.90 | <0.01 |
Table 2.
Mean post-operative pain demonstrated at 3-time intervals
| Variables | 1st day | 5th day | 10th day | 1st month | P |
|---|---|---|---|---|---|
| Mean+/-Std. deviation | 4.25+/-1.27 | 2.75+/-1.67 | 1.14+/-1.07 | 0.42+/-0.53 | <0.001 |
The mean score for assessment of surgical field bleeding was found to be 1.75 [Table 3] which signified mild bleeding according to Fromme’s scale. The mean time taken for adequate exposure of the fracture was 6.62 min.
Table 3.
Mean surgical field bleeding (Fromme’s scale)
| Variables | Surgical field bleeding (Fromme’s Scale) |
|---|---|
| Mean | 1.75 |
| Std. Deviation | +/-1.07 |
Based on the results, the null hypothesis that ORIF of ZMC fractures using sub-brow incision would not provide adequate exposure of the FZ region and good surgical outcome was rejected.
DISCUSSION
The zygomaticomaxillary (ZMC) complex constitutes one of the key structures which establish the facial dimensions in the transverse as well as anteroposterior planes. In addition to contributing to facial aesthetics, the ZMC is vital for the protection of the globe and its efficient movements. Further, ZMC plays a significant part in dissipating masticatory load. Hence, proper restoration of this anatomic landmark is crucial, following fractures.[18] However, because of the chances of displacement in multiple planes, including translatory movements along the x, y, and z axes as well as rotatory movements along the x, y, and z axes, reducing and fixing a fractured zygomatic bone is difficult.[19]
Why fixation at the FZ region is important?
Stable fixation of ZMC fractures is achieved by incorporating the FZ suture as one of the points of fixation.[3] With a single point-fixation of the ZMC fracture at the frontozygomatic suture area, Champy et al.[20] had documented good outcomes. Biomechanical study of the facial skeleton demonstrates that fixation of a miniplate across the FZ suture is necessary for the following reasons; (1) It resists translation along the long axis, which is perpendicular to the plane of miniplate fixation[21] (2) It counteracts rotatory displacement under masticatory load.[22] A study conducted by Elkahwagi and Eldegwi[3] evaluated the pre-operative and post-operative restoration of facial symmetry through a single point fixation at FZ by a follow-up till 2 years and demonstrated excellent cosmetic and functional outcomes. Fujioka et al.[23] evaluated the post-operative stability of single point fixation of ZMC fracture at FZ through a CT analysis, at time intervals of one week, two months, and six months. They observed satisfactory outcomes and stability similar to three-point fixation. A finite element analysis (FEA) study performed by Sarkarat et al.,[24] compared the stress, strain, linear and rotational displacement along the fixation points at the FZ suture, ZM buttress, and infraorbital rim and concluded that the stability of fixation at FZ was found to be better compared than the other two locations. Thus, the importance of fixation at the FZ suture has been established clearly by clinical, radiological, and FEA studies.
Hence, fixation at the FZ region is crucial for the effective outcome of ORIF of ZMC fractures and mandates exposure of the FZ region.
Incisions to approach FZ suture
The incisions most frequently used to expose the FZ region are i) Lateral brow[7] and ii) Upper blepharoplasty.[8] However these approaches present specific intra-operative limitations and post-operative complications. To hide the scar, a lateral brow incision[7] is made inside the hairline of the brow. The incision extends through, the skin, subcutaneous tissue, as well as orbicularis oculi muscle. However, it is commonly linked to focal alopecia, which impairs facial appearance. Further, it provides restricted surgical access due to its farther positioning/location, about to the FZ suture, and difficulty in retraction due to the thickness of soft tissue in the eyebrow region. The incision may also be unsuitable in patients with sparse eye-brow on the lateral aspect. Blepharoplasty incision is cosmetically superior but requires expertise to perform the technique.
The upper blepharoplasty incision is also called the upper-eyelid approach, upper-eyelid crease, or supratarsal fold approach.[8] The incision is placed in the fold formed naturally by the opening of the palpebral fissure, termed the supratarsal fold. If the fold is not appreciable, the incision is placed 10 mm superiorly to the eyelash line in the middle part and 6-7 mm superiorly to the lateral canthus in the lateral or temporal part.
Blepharoplasty incision is advantageous in gaining adequate access to the frontozygomatic suture while camouflaging the scar which gets retracted inwards within the fold while opening the eye.[25] Despite of the advantages cited in the literature, this approach is less frequently adopted due to limitations such as technique sensitivity and potential complications specifically hematoma, lagophthalmos, wound dehiscence, asymmetry, and diplopia along with the chances of injury to the lacrimal gland.[10]
The utilization of a sub-brow incision for the exposure, reduction, and fixation of the FZ area in the treatment of ZMC fractures was investigated in our study. The study analyzed the ease of the technique in accessing the fracture and gaining adequate exposure to facilitate ideal fixation. “Sub-brow” incision has been mentioned in literature for cosmetic procedures like brow lifts, by plastic and cosmetic surgeons.[12] The use of “Sub-brow” incision in the field of maxillofacial trauma is limited; the only literature available, mentions its use for the management of the supra-orbital rim and nasal bone fractures.[13,14] Ours is the first study that has used this incision to approach the FZ region for ORIF of ZMC fractures.
Efficacy of sub-brow incision
In this prospective observational study, patients were managed by ORIF of zygomaticomaxillary fractures with fixation at frontozygomatic suture using Subbrow incision. The intra-operative and post-operative assessment parameters were assessed thoroughly as per the follow-up timeline. Based on the assessment, the efficacy of the sub-brow was found to be satisfactory in all the cases. Exposure, as well as fixation of fracture, was easily achievable with minimal bleeding. The technique was found to be simple and quick. This is reflected in reduced pain in the surgical site and better patient comfort in the immediate postoperative period.
The technique was easy to perform, thus improving the surgeon’s comfort. In the postoperative period, scarring along the incision line was assessed according to the modified vancouver scar scale (MVSS) at a regular time intervals The scar was found to be aesthetically acceptable and minimal. This may be attributed to the positioning of the incision in the concave area of the face (below the prominence of the eye-brow). This is substantiated by Zitelli,[26] who demonstrated unesthetic scarring in convex areas in contrast to imperceptible scarring involving concave areas.
Sub-brow incision versus conventional incisions
Many studies have evaluated the wide range of advantages and limitations offered by the lateral brow and upper blepharoplasty incisions.
The lateral brow incision is more common than the other incisions because it allows easy and quick access to the superolateral orbital rim.[27,28] During this procedure, there is no danger of harm to any functionally significant neurovascular structures. The resultant scar is typically well-covered as long as the incision is made inside the brow hairs. However, when the scalpel is improperly angulated to the hair follicle while making the incision, it may result in focal alopecia. Adequate care needs to be taken to ensure tricophytic closure. Furthermore, to acquire greater exposure or follow the orbital boundary, a lateral or inferior extension of the incision line placed outside the hair-bearing area might result in a cosmetically compromised scar.[9] Moreover, the two major limitations associated with lateral brow incision are limited access and unesthetic scarring.
Upper blepharoplasty incision is associated with excellent exposure to the FZ region. It is also superior in terms of camouflaging the scar in the supratarsal skin fold.[28-30] Nevertheless, supratarsal fold incision is more technique sensitive and prone to more complications than the lateral brow incision.
Sub-brow incision demonstrates numerous advantages in comparison with the above incisions;
In addition to providing adequate exposure for fixation at the FZ region, the incision ensured minimal surgical bleeding and post-operative pain, as evaluated by objective scales. Further, the resultant scar was favorable. The technique was simple and easy to master. Moreover, unlike lateral-brow incision, sub-brow incision can be placed even in patients with sparse eyebrow, without compromise in esthetics, as it is positioned in the concave periorbital region.
Limitations of sub-brow incision
The limitation of sub-brow incision is restricted medial extension due to the presence of supra-orbital nerve which emerges out of the supraorbital foramen, at the junction of the medial 1/3rd and lateral 2/3rds of the palpebral fissure width.
Limitations of the study
The smaller sample size is a limitation of the study. This could not be averted because of the difficulties faced in the recruitment of an ideal sample, conforming to the selection criteria because of the pandemic. Moreover, a randomized clinical trial would be more effective in evaluating the efficacy of the incision in comparison with the conventional incision, lateral brow.
CONCLUSION
A sub brow incision is an effective approach for open reduction and internal fixation of zygomatic fractures. It provides adequate exposure of the FZ region and convenient fixation while facilitating quick surgical access. The technique is simple, providing a good surgical field. The post-operative outcomes following sub-brow incision demonstrate favorable scarring and good patient comfort. The incision may be considered a viable alternative to conventional incisions used to approach the FZ region.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Ethical statement
Ethical Clearance was obtained from Institutional Review Board, with Ref no SRMDC/1RB/2019/MDS/No.401 dated 02/02/2022.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Subhashraj K, Nandakumar N, Ravindran C. Review of maxillofacial injuries in Chennai, India:A study of 2748 cases. Br J Oral Maxillofac Surg. 2007;45:637–9. doi: 10.1016/j.bjoms.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 2.Kurita M, Okazaki M, Ozaki M, Tanaka Y, Tsuji N, Takushima A, et al. Patient satisfaction after open reduction and internal fixation of zygomatic bone fractures. J Craniofac Surg. 2010;21:45–9. doi: 10.1097/SCS.0b013e3181c36304. [DOI] [PubMed] [Google Scholar]
- 3.Elkahwagi M, Eldegwi A. Minimally invasive single-point stabilization of zygomaticomaxillary complex fractures. J Maxillofac Oral Surg. 2021;1:1–8. doi: 10.1007/s12663-021-01520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chakranarayan A, Thapliyal GK, Sinha R, Suresh MP. Efficacy of two point rigid internal fixation in the management of zygomatic complex fracture. J Maxillofac Oral Surg. 2009;8:265–9. doi: 10.1007/s12663-009-0065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soejima K, Sakurai H, Nozaki M, Kitazawa Y, Takeuchi M, Yamaki T, et al. Semi-closed reduction of tripod fractures of zygoma under intraoperative assessment using ultrasonography. J Plast Reconstr Aesthet Surg. 2009;62:499–505. doi: 10.1016/j.bjps.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 6.Mohammadinezhad C. Evaluation of a single miniplate use in treatment of zygomatic bone fracture. J Craniofac Surg. 2009;20:1398–402. doi: 10.1097/SCS.0b013e3181acdc25. [DOI] [PubMed] [Google Scholar]
- 7.Hwang K. One-point fixation of tripod fractures of zygoma through a lateral brow incision. J Craniofac Surg. 2010;21:1042–4. doi: 10.1097/SCS.0b013e3181e48607. [DOI] [PubMed] [Google Scholar]
- 8.McRae M, Frodel J. Midface fractures. Facial Plast Surg. 2000;16:107–14. doi: 10.1055/s-2000-12572. [DOI] [PubMed] [Google Scholar]
- 9.Fonseca R, Barber D, Powers M, Frost D. Oral and Maxillofacial Trauma. St. Louis, Mo: Elsevier Saunders; 2013. [Google Scholar]
- 10.Rega AJ, Ziccardi VB, Granick M. Cosmetically favorable scars using the upper blepharoplasty incision. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:627–8. doi: 10.1016/j.tripleo.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 11.Oestreicher J, Mehta S. Complications of blepharoplasty:Prevention and management. Plast Surg Int. 2012;2012:252368. doi: 10.1155/2012/252368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naik M. Blepharoplasty and periorbital surgical rejuvenation. Indian J Dermatol Venereol Leprol. 2013;79:41–51. doi: 10.4103/0378-6323.104668. [DOI] [PubMed] [Google Scholar]
- 13.Hwang K, Kim DJ. Reduction of supraorbital fractures via a short sub-brow incision. J Craniofac Surg. 2018;29:2164–5. doi: 10.1097/SCS.0000000000004738. [DOI] [PubMed] [Google Scholar]
- 14.Anchlia S, Domadia H, Chaudhari P, Gosai H, Rajpoot D, Patel H, et al. “The modified subbrow incision”- A boon for nasal bone fractures. Int J Oral Maxillofac Surg. 2019;48:37. [Google Scholar]
- 15.Choi WS, Samman N. Risks and benefits of deliberate hypotension in anaesthesia:A systematic review. Int J Oral Maxillofac Surg. 2008;37:687–703. doi: 10.1016/j.ijom.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Singha S, Dhirawani RB, Asrani S, Agrawal A, Taank J. Evaluation of treatment outcome after impacted mandibular third molar surgery with and without autologous platelet concentrates. SRM J Res Dent Sci. 2019;10:72. [Google Scholar]
- 17.Finlay V, Burrows S, Kendell R, Berghuber A, Chong V, Tan J, et al. Modified Vancouver Scar Scale score is linked with quality of life after burn. Burns. 2017;43:741–6. doi: 10.1016/j.burns.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Pau CY, Barrera JE, Kwon J, Most SP. Three-dimensional analysis of zygomatic-maxillary complex fracture patterns. Craniomaxillofac Trauma Reconstr. 2010;3:167–76. doi: 10.1055/s-0030-1263082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rudderman RH, Mullen RL. Biomechanics of the facial skeleton. Clin Plast Surg. 1992;19:11–29. [PubMed] [Google Scholar]
- 20.Champy M, Lodde JP, Kahn JL, Kielwasser P. Attempt at systematization in the treatment of isolated fractures of the zygomatic bone:Techniques and results. J Otolaryngol. 1986;15:39–43. [PubMed] [Google Scholar]
- 21.Atul P, Ramesh KS, Surinder M. Rigid internal fixation of zygoma fractures:A comparison of two-point and three-point fixation. Indian J Plast Surg. 2007;40:18–24. [Google Scholar]
- 22.Deveci M, Eski M, Gurses S, Yucesoy CA, Selmanpakoglu N, Akkas N. Biomechanical analysis of the rigid fixation of zygoma fractures:An experimental study. J Craniofac Surg. 2004;15:595–602. doi: 10.1097/00001665-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Fujioka M, Yamanoto T, Miyazato O, Nishimura G. Stability of one-plate fixation for zygomatic bone fracture. Plast Reconstr Surg. 2002;109:817–8. doi: 10.1097/00006534-200202000-00068. [DOI] [PubMed] [Google Scholar]
- 24.Sarkarat F, Ebrahimi S, Kahali R, Pirhadi Rad A, Khosravi M, Rakhshan V. Finite element simulation of displaced ZMC fracture after fixation with resorbable and non-resorbable one-point mini-plates and applying normal to severe occlusal loads. Trauma Monthly. 2019;24:1–7. [Google Scholar]
- 25.Strong EB, Sykes JM. Zygoma complex fractures. Facial Plast Surg. 1998;14:105–15. doi: 10.1055/s-0028-1085306. [DOI] [PubMed] [Google Scholar]
- 26.Zitelli JA. Secondary intention healing:An alternative to surgical repair. Clin Dermatol. 1984;2:92–106. doi: 10.1016/0738-081x(84)90031-2. [DOI] [PubMed] [Google Scholar]
- 27.Yamsani B, Gaddipati R, Vura N, Ramisetti S, Yamsani R. Zygomaticomaxillary complex fractures:A review of 101 cases. J Maxillofac Oral Surg. 2016;15:417–24. doi: 10.1007/s12663-015-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marinho RO, Freire-Maia B. Management of fractures of the zygomaticomaxillary complex. Oral Maxillofac Surg Clin North Am. 2013;25:617–36. doi: 10.1016/j.coms.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 29.Strong EB, Gary C. Management of zygomaticomaxillary complex fractures. Facial Plastic Surg Clin. 2017;25:547–62. doi: 10.1016/j.fsc.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Ellis E, Zide MF. Periorbital approaches. In: Ellis E, Zide MF, editors. Surgical Access to the Facial Skeleton. Baltimore (MD): Williams &Wilkins; 1995. [Google Scholar]


