ABSTRACT
This systematic review mainly focuses on the effects of curcumin on oral cancer cells at the molecular level and summarizes the results of the studies. We searched and analyzed various databases such as Pub Med, ProQuest, Google Scholar, Science Direct, and Scopus. Searches were conducted from 2006 to 2021. This systematic review evaluated various effects of curcumin on oral cancer at the molecular level. All the studies related to the effects of curcumin on oral cancer, both in-vivo and in-vitro, were included. After abstract and text screening a total of 13 articles were finally selected for the study based on the inclusion and exclusion criteria. All most all the included studies reported that after treating the cell lines with curcumin there is a reduction in cell proliferation and cell growth, analyzed using MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) assay. Curcumin also induces S phase cell cycle arrest and also prevents Tregs migration. The curcumin reverses the process of epithelial mesenchymal transition (EMT) back to mesenchymal epithelial transition (MET). From this review, it is concluded that curcumin inhibited proliferation, migration, invasion, and metastasis, and induced apoptosis via modulating multiple signaling pathways in oral cancer cell lines. But further clinical trials are needed for a detailed evaluation of the effects of curcumin on patients with oral cancer.
Keywords: Apoptosis, curcumin, molecular level, oral squamous cell carcinoma
INTRODUCTION
Oral squamous cell carcinoma (OSCC) is the most common type of oral cancer, which is highly invasive in nature is among the 10 most common cancers worldwide. Tobacco and alcohol consumption are the main risk factors involved in the etiology of OSCC. The human papilloma virus (HPV) also plays a role in the risk factor associated with OSCC. Despite various treatment modalities, the survival rates remain around 50%, over the past three decades.[1]
Any food ingredient that provides medical and health benefits is known as nutraceutical. Curcumin is the most promising and effective nutraceutical, which is currently most widely investigated for the treatment of various systemic disorders and cancer.[2] Curcumin is a botanical agent extracted from the rhizome (root) of the curcuma longa. It belongs to a ginger family (perineal herb) that is broadly grown in the south and south-east Asia and it is also an active constituent of turmeric. Curcumin (diferuloylmethane), dimethoxy-curcumin, and bisdemethoxycurcumin are the three main components. It is used as a healing agent in biliary disorders, anorexia, cough, diabetic wounds, hepatic disorders, rheumatism, and sinusitis.[3] To reduce the treatment morbidities for head and neck cancer, curcumin can be effectively used which has the anticancer property and also displays a wide range of pharmacological activities such as antioxidant and anti-inflammatory.[4] The data collected from various studies from in vitro cell line models as well as in vivo animal xenograft models have demonstrated that curcumin inhibited head and neck cancer cell proliferation and migration.
Transcriptional factor nuclear factor-kappa B (NF-κB), transcriptional factor CCAAT/enhancer-binding protein (C/EBP), cyclins/cyclin-dependent kinases, beta-cell lymphoma-2 (Bcl-2) family proteins, matrix metalloproteinases (MMPs), AKT/mTOR signaling pathway (phosphatidyl-inositol-3-kinase/mammalian target of rapamycin), and signal transducer and activator of transcription-3 (STAT3) signaling pathway have been demonstrated to be dysregulated in head and neck cancer. Increasing evidence shows that curcumin could modulate these genes, producing anti-cancer effects in head and neck cancer.[4]
The various molecular targets of curcumin are interleukin (IL)-1, -2, -6, -8 (interleukins), tumor necrotic factor-alpha (TNF-α), kinase activity epidermal growth factor receptor (EGFR) kinase, mitogen-activated protein kinase protein kinase-A (MAPK PKA), protein kinase-B (PKB), protein kinase-C (PKC), Janus kinase (JAK), transcriptional factor AP-1, b-catenin, cyclic AMP response element-binding protein (CREB), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), peroxisome proliferator-activated receptor-gamma (PPARg), STAT3, p53, c-myc (master regulator of cell cycle entry and proliferative metabolism), hypoxia-inducible factor-1 (HIF1).[2] Treatment with curcumin also improved immunoglobulin E (Ig) E, proinflammatory cytokine IL-4, transforming growth factor-beta, IL-17, interferon-gamma levels, and type 1/type 2 helper cells (Th1)/(Th2) ratio in conditions with disturbance in the immune system.[5] This systematic review mainly focuses on the effects of curcumin on oral cancer cells in molecular level and to summarize the results of these studies.
MATERIALS AND METHODS
The substructure of this systematic review is prepared according to the EQUATOR guideline and preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. The focused question is “Does treating with curcumin have any effects on oral cancer at the molecular level?”
Study design
This systematic review evaluated various effects of curcumin on oral cancer at the molecular level.
Eligibility criteria
Inclusion criteria
All experimental studies done to evaluate the effects of curcumin on oral cancer were included. Studies which used only curcumin as the treatment were included. No time or language restrictions were applied. Both in-vivo and in-vitro studies were included.
Exclusion criteria
We excluded case reports, literature reviews, letter to the editor, personal opinions, book chapters, conference papers and studies using animal models. Studies which had a combination treatment with curcumin and any other agent were also excluded.
Information sources
The following databases were incorporated in the systematic search for relevant literature: Pub Med, ProQuest, Google Scholar, Science Direct and Scopus. Searches were conducted from 2006 to 2021.
Search terms
(Curcumin AND Oral cancer) OR (Clinical Trials On Curcumin) OR (Turmeric on Oral Cancer) OR (Therapeutic Efficacy of Curcumin) OR (In-Vitro Studies on curcumin).
Study selection
Phase 1—Title screening.
Phase 2—Abstract screening.
Phase 3—Full text screening.
In every phase, the studies were screened for inclusion and exclusion criteria. The studies which me the inclusion criteria were selected and the following characteristics were recorded: Author, year of study, country of research, study type, sample size and number of patients, cell lines, assays performed, duration of the study, the dosage of the drug and conclusion.
RESULTS
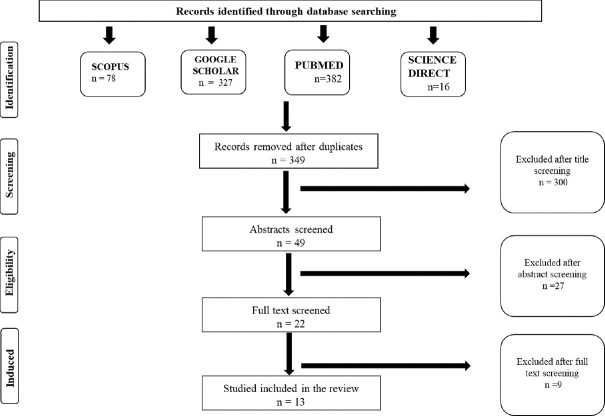
A summary of the results of the included studies is shown in Table 1. A total of 3689 articles were found from various scientific databases, with search expressions relevant to our study. After removal of irrelevant studies, 803 articles were selected for initial screening. In the second phase, 349 duplicates were excluded, leaving 454 articles for further screening. After abstract and text screening a total of 13 articles were finally selected based on the inclusion and exclusion criteria of the systematic review.[6-18] The selection process was carried out following PRISMA STATEMENT [Figure 1].
Table 1.
List of included studies and their main characteristics
| Name of the researcher | Year of the study | In-vitro/In-vivo | Place | Sample size | Assay | Cell lines | Duration | Dosage | Conclusion of the study |
|---|---|---|---|---|---|---|---|---|---|
| Gabriel Alvares Borges et al.[23] | 2018 | In-vitro | India | 3 | 1. Western blotting 2. MTT assay 3. Sphere formation assay 4. QRT-PCR | 1. HPV16 positive OSCC cell line-1 2. HPV16 negative OSCC cell line-2 | 24 hours—cell proliferation and QRT-PCR 7-10 days-sphere formation | 0-50 µM | Downregulation of miR-21 expression on treating with curcumin is seen in both HPV positive and HPV negative oral cancer cell lines but higher effects are seen in HPV positive cancer cell lines and curcumin also inhibits cell growth in oral cancer cells (in-vitro) |
| Ji Young Kim et al.[7] | 2012 | In-vitro | South Korea | 1 | 1. Cell viability assay 2. Apoptosis assay 3. ROS measurement 4. Western blot analysis | OSCC cell line (YD1OB) | 24 hours | 10-40 µM | Curcumin activates autophagy in oral squamous cell carcinoma and it is activated by curcumin induced ROS production. Curcumin also accelerates apoptotic molecules in oral squamous cell carcinoma. |
| Shengkai Liao et al.[8] | 2011 | In-vitro | China | 1 | 1. Colonogenic assay 2. Real time RT PCR 3. Annexin V assay 4. Western blot 5. Invasion assay 6. ELISA 7. Flow cytometry 8. Luciferase assay | Human OSCC cell line | 24, 48, and 72 hours | 2.5, 5.0, 7.5 µM | Curcumin induce apoptosis, inhibits cell growth, downregulates NOTCH-1 pathway which in turn leads to downregulation of BCL-2, MMP9, VEGF and cyclin D in oral squamous carcinoma cell lines. |
| Alok Mishra et al.[9] | 2015 | In-vitro | India | 1 | 1. MTT assay 2. PCR 3. Northern blot 4. Electrophoretic mobility shift assay | Human oropharyngeal squamous cell cancer cell lines | 24, 48, 72 h | 0-100 µM | Curcumin downregulates HPV transcription ( NF-κB and AP-1) in HPV positive oral cancer cell lines. Curcumin also inhibits transcription of E6 oncogene in HPV positive oral cancer cell lines |
| Can Xiao et al.[10] | 2014 | In-vitro | China | 1 | 1. MTT assay 2. qRT-PCR 3. colony formation assay 4. Western blot | Human tongue squamous cancer cell lines | 72 h. | 20, 40, 60 µM | Curcumin induces the expression of miR-9 that mediates the inhibition of SSC9 cells proliferation and Wnt/βcatenin signaling pathway in human tongue squamous cell cancer cell lines |
| Yu-Chuan Lin et al.[11] | 2010 | In-vitro | Taiwan | 1 | 1. Cell cycle analysis 2. Flow cytometry | Human oral SAS cell lines | 24 h | 0-30 µM | The inhibition effects of curcumin on the growth of human oral squamous carcinoma in vitro were significant. |
| Chao Ma et al.[12] | 2020 | In-vitro | China | 1 | 1. Cell proliferation assay 2. Cell migration assay 3. TUNEL assay 4. Flow cytometry 5. Western blot | Human tongue cancer cell lines | 24 h | 0-100 µM | Curcumin inhibits cell proliferation, cell migration, apoptosis, and induces S phase cell cycle arrest in tongue cancer cell lines. Curcumin can be effectively used in treating oral cancers. |
| Charlotte Kötting et al.[13] | 2021 | In-vitro | Germany | 1 | 1. Annexin V/apoptosis assay | HNSCC cell lines | 48 h. | 5, 10, and | Curcumin is a potent NF-κB inhibitor that |
| 2. Western blot 3. Flow cytometry 4. ELISA 5. RT q- PCR 6. Migration assay 7. NF-κB ELISA | 20 µM | is able to reverse the process of EMT back to MET, reducing Treg-attracting chemokine CCL22, with visible inhibition of Treg migration. | |||||||
| Tian Liu et al.[14] | 2021 | In-vitro | China | 2 | 1. Colony formation assay 2. Western blot 3. RT q-PCR 4. Cell transfection 5. Dual luciferase | HSC 3 and CAL 33 cell lines | 24-48 h. | 5-20 µM | Inhibits the proliferation and NF-κB activity of OSCC cells and also decreases the expression of f Sp1, p65 and HSF1 in OSCC cells |
| Feng Liao et al.[15] | 2018 | In-vitro | China | 1 | 1. MTT assay 2. Western blot 3. IHC 4. Immunofluorescence 5. Flow cytometry | CAD 27 and Fadu cell lines | - | - | On treating with curcumin reduction in cell proliferation and growth was seen. And also decreased the expression of PDL1 and p-STA was seen in CAD 27 and fadu cell lines |
| Yuichi Ohnish et al.[17] | 2020 | In-vitro | Japan | 2 | 1. Scratch wound healing cell migration assay 2. Matrigel cell invasion assay 3. Western blot | The human tongue-derived OSCC cell line HSC-4 and Ca9-22 | 2 h scratch wound healing cell 48 h-matrigel cell invasion assay | 15 µM | Pre- treatment with Curcumin results in reduced cell invasion in hepatocyte growth factor (HGF) induced HSC-4 cell lines. And also, it reduces Epithelial mesenchymal transition in both HGF induced HSC-4 and Ca9-22 cell lines by repressing c-Met and ERK activation. |
| Ardito F et al.[16] | 2018 | In-vitro | Italy | 1 | 1. MTT assay 2. Migration assay 3. Apoptosis assasssy | TSCC cell lines | 24, 48, 72 h | 0, 5, 10, 20, 50 µM | Reduction in cell proliferation, apoptosis and migration was seen on treating with curcumin at different time and concentration. |
| Lei Zhen et al.[21] | 2014 | In-vitro | China | 1 | 1. Cell proliferation assay 2. Cell cycle analysis 3. Transwell cell Matrigel invasion assay 4.Real time PCR 5.Western blot | SCC-25 cell lines | 24, 48 h |
Figure 1.
PRISMA statement
The studies were conducted in various countries such as India (2), China (5), Italy (1), Germany (1), South Korea (1), and Taiwan (1). All the studies were published from 2010 to 2021 in the English language. Both in-vivo (1) and in-vitro (12) studies were included. All the studies evaluated various assays such as MTT (3-(4,5-Dimethylthiazol-2-yl)-2,5-Dipenyltetrazolium Bromide) assay, Apoptosis assay/Annexin V assay, migration assay, proliferation assay, flow cytometry, western blot, northern blot, reactive oxygen species (ROS) measurement, real-time reverse transcriptase-polymerase chain reaction (RT PCR), enzyme-linked immunoassay (ELISA), immune histochemistry (IHC), colony formation assay luciferase assay and immunofluorescence. All the studies were done on human oral cancer cell lines, two of which were performed on HPV-positive oral cancer cases.
Cell cycle arrest was assessed by flow cytometry with propidium iodide (PI) staining. Apoptosis was assessed directly, mostly through flow cytometry with annexin V-FITC (family of intracellular proteins that binds to phosphatidylserine) and PI staining or apoptosis detection kits, or indirectly, through the analysis of apoptosis-related proteins expression with western blot and immunofluorescence. The summary of the descriptive characteristics of the included studies is tabulated in Table 1.
The dose of curcumin used in the included studies ranges from 0 to 100 μm. Every study that is included has reported that after treating the cell lines with curcumin there is a reduction in cell proliferation and cell growth, when analyzed using MTT assay. One study reported that the NOTCH-1 pathway (Notch homolog, translocation-associated [drosophila]) was downregulated which was analyzed using RT PCR and western blot after treating the cell lies with curcumin. The included studies reported that there is down-regulation of miR-2 1 and 9 (MicroRNA), nuclear factor kappa-light-chain-enhancer of activated beta cells (NF-κB), activator protein-1 (AP-1), wingless and Int-1/beta (Wnt/β) catenin pathway, specificity protein-1 (Sp1), p65, and heat shock transcription factor-1 (HSF1) in OSCC cell lines. Curcumin also induces S phase cell cycle arrest and also prevents Tregs migration. It is also reported to reverse the process of EMT back to MET.
DISCUSSION
Curcumin (diferuloylmethane) is a polyphenol compound extracted from the rhizome of the plant curcuma longa. It is usually pigmented yellow or orange, with a variety of biological properties such as anti-inflammatory, antibacterial, antifungal, antioxidant, antitumor, and wound healing.[18] Curcumin, desmethoxycurcumin, and bisdemethoxycurcumin, collectively known as curcuminoids, constitute the biologically active constituents of curcuma longa L or turmeric. Poor oral bioavailability limits the beneficial action of curcumin. The combination of curcuminoids and the essential oil of turmeric can enhance the oral bioavailability of curcumin.[19] Curcumin is highly lipophilic, has poor gastrointestinal absorption, and is mostly eliminated without being absorbed, therefore, curcumin has an extremely low level of bioavailability. According to a study by Lao et al.,[20] the maximum concentrations of curcumin in the blood when 10 or 12 g of curcumin taken orally, were 50.5 and 57.6 ng/ml, respectively.
A total of 13 research articles were included in the study, which consisted of 12 in-vitro and 1 in-vivo studies. The included studies evaluated various assays such as MTT assay, apoptosis assay/annexin V assay, Migration assay, proliferation assay, flow cytometry, western blot, northern blot, ROS measurement, real-time RT PCR, ELISA, IHC, colony formation assay luciferase assay and immunofluorescence. The studies were done on human oral cancer cell lines, of which two studies were performed on HPV-positive oral cancer cell lines.
In a study done by Shengkai Liao et al.[8] curcumin induced apoptosis and caused growth inhibition which was dose and time-independent. It also caused downregulation of NOTCH-1 and Wnt (Wingless-related integration site) pathway which was analyzed using real-time quantitative reverse transcription polymerase chain reaction (QRT-PCR) which in turn leads to downregulation of BCL-2 and cyclin-D1, matrix metalloproteinases-9 (MMP9), vascular endothelial growth factor (VEGF) expression. Curcumin downstream the expression of MMP9 and VEGF which are involved in tumor cell invasion and progress in CAL-27 (oral adenosquamous carcinoma) cell lines.
A study done by Alok Mishra et al.[9] reported that curcumin causes decreased cell viability and morphological changes in HPV-positive oral cancer cell lines. When analyzed using northern blot they found that curcumin inhibits E-6 mediated P53 downregulation in HPV-positive cancer cell lines. When treated with 100 μm of curcumin it downregulated E6 (viral oncogene). It also inhibits NF-κB and AP-1 in HPV-positive cancer cell lines. In a study done by Can Xiao et al.[10] it was found that curcumin induces the expression of miR9, which mediates the inhibition of SCC9 cell proliferation and also inhibits the Wnt/βcatenin signaling pathway.
Zhen et al.[21] conducted an in-vitro study, the results of which showed that curcumin inhibited SCC-25 cells proliferation and induced the arrest of G2/M phase in a dose-dependent manner. It was also reported to downregulate MMP-2, MMP-9, uPA and uPAR expression. They also revealed that curcumin regulated the p-EGFR and EGFR downstream signaling molecules including Akt, ERK1/2, and STAT3 and finally concluded that curcumin reduced the EGF-induced phosphorylation of EGFR and suppressed EGF-triggered SCC-25 cells invasion.[21]
Curcumin regulates multiple signaling pathways, however, the underlying mechanisms remain unclear.[19,22] Recently, it has been reported that curcumin mediated epigenetics regulation by modulating DNA methylation, histone modifications and miRNA expression in various human cancers.[22] Curcumin inhibited proliferation, migration, invasion and metastasis. They, in turn, induced apoptosis via modulating multiple signaling pathways in oral cancer cell lines. But further clinical trials are needed for a detailed evaluation of the effects of curcumin on patients with oral cancer.
Author contributions
All authors contributed to manuscript and design. Material preparation and data collection were performed by Akhilesh Kumar Singh, Naresh Kumar Sharma, Nitesh Mishra, Arjun Mahajan, Aswathi Krishnan, Ravina Rajpoot, Janani Anand Kumar, and Arun Pandey. The first draft of manuscript was written by Nitesh Mishra and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zlotogorski A, Dayan A, Dayan D, Chaushu G, Salo T, Vered M. Nutraceuticals as new treatment approaches for oral cancer–I:Curcumin. Oral Oncol. 2013;49:187–91. doi: 10.1016/j.oraloncology.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Sunagawa Y, Katanasaka Y, Hasegawa K, Morimoto T. Clinical applications of curcumin. Pharm Nutr. 2015;3:131–5. [Google Scholar]
- 3.Shishodia S, Chaturvedi MM, Aggarwal BB. Role of curcumin in cancer therapy. Curr Probl Cancer. 2007;31:243–305. doi: 10.1016/j.currproblcancer.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Gao W, Chan JY, Wei WI, Wong TS. Anti-cancer effects of curcumin on head and neck cancers. Anticancer Agents Med Chem. 2012;12:1110–6. doi: 10.2174/187152012803529736. [DOI] [PubMed] [Google Scholar]
- 5.Memarzia A, Khazdair MR, Behrouz S, Gholamnezhad Z, Jafarnezhad M, Saadat S, et al. Experimental and clinical reports on anti-inflammatory, antioxidant, and immunomodulatory effects of Curcuma longa and curcumin, an updated and comprehensive review. Biofactors. 2021;47:311–350. doi: 10.1002/biof.1716. [DOI] [PubMed] [Google Scholar]
- 6.Bano N, Yadav M, Das BC. Differential inhibitory effects of curcumin between HPV+ve and HPV–ve oral cancer stem cells. Front Oncol. 2018;8:412. doi: 10.3389/fonc.2018.00412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JY, Cho TJ, Woo BH, Choi KU, Lee CH, Ryu MH, et al. Curcumin-induced autophagy contributes to the decreased survival of oral cancer cells. Arch Oral Biol. 2012;57:1018–25. doi: 10.1016/j.archoralbio.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Liao S, Xia J, Chen Z, Zhang S, Ahmad A, Miele L, et al. Inhibitory effect of curcumin on oral carcinoma CAL-27 cells via suppression of Notch-1 and NF-κB signalling pathways. J Cell Biochem. 2011;112:1055–65. doi: 10.1002/jcb.23019. [DOI] [PubMed] [Google Scholar]
- 9.Mishra A, Kumar R, Tyagi A, Kohaar I, Hedau S, Bharti AC, et al. Curcumin modulates cellular AP-1, NF-kB, and HPV16 E6 proteins in oral cancer. Ecancermedicalscience. 2015;9:525. doi: 10.3332/ecancer.2015.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao C, Wang L, Zhu L, Zhang C, Zhou J. Curcumin inhibits oral squamous cell carcinoma SCC-9 cells proliferation by regulating miR-9 expression. Biochem Biophys Res Commun. 2014;454:576–80. doi: 10.1016/j.bbrc.2014.10.122. [DOI] [PubMed] [Google Scholar]
- 11.Lin YC, Chen HW, Kuo YC, Chang YF, Lee YJ, Hwang JJ. Therapeutic efficacy evaluation of curcumin on human oral squamous cell carcinoma xenograft using multimodalities of molecular imaging. Am J Chin Med. 2010;38:343–58. doi: 10.1142/S0192415X10007890. [DOI] [PubMed] [Google Scholar]
- 12.Ma C, Zhuang Z, Su Q, He J, Li H. Curcumin has anti-proliferative and pro-apoptotic effects on tongue cancer in vitro:A study with bioinformatics analysis and in vitro experiments. Drug Des Devel Ther. 2020;14:509–18. doi: 10.2147/DDDT.S237830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kötting C, Hofmann L, Lotfi R, Engelhardt D, Laban S, Schuler PJ, et al. Immune-stimulatory effects of curcumin on the tumor microenvironment in head and neck squamous cell carcinoma. Cancers. 2021;13:1335. doi: 10.3390/cancers13061335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu T, Long T, Li H. Curcumin suppresses the proliferation of oral squamous cell carcinoma through a specificity protein 1/nuclear factorκBdependent pathway. Exp Ther Med. 2021;21:202. doi: 10.3892/etm.2021.9635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liao F, Liu L, Luo E, Hu J. Curcumin enhances anti-tumour immune response in tongue squamous cell carcinoma. Arch Oral Biol. 2018;92:32–7. doi: 10.1016/j.archoralbio.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Ardito F, Perrone D, Giuliani M, Testa NF, Muzio LL. Effects of curcumin on squamous cell carcinoma of the tongue:An in vitro study. Curr Top Med Chem. 2018;18:233–43. doi: 10.2174/1568026618666180412153824. [DOI] [PubMed] [Google Scholar]
- 17.Ohnishi Y, Sakamoto T, Zhengguang L, Yasui H, Hamada H, Kubo H, et al. Curcumin inhibits epithelial-mesenchymal transition in oral cancer cells via cMet blockade. Oncol Lett. 2020;19:4177–82. doi: 10.3892/ol.2020.11523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basak SK, Bera A, Yoon AJ, Morselli M, Jeong C, Tosevska A, et al. A randomized, phase 1, placebo-controlled trial of APG-157 in oral cancer demonstrates systemic absorption and an inhibitory effect on cytokines and tumour-associated microbes. Cancer. 2020;126:1668–82. doi: 10.1002/cncr.32644. [DOI] [PubMed] [Google Scholar]
- 19.Tang W, Du M, Zhang S, Jiang H. Therapeutic effect of curcumin on oral diseases:A literature review. Phytother Res. 2020 doi: 10.1002/ptr.6943. doi:10.1002/ptr.6943. [DOI] [PubMed] [Google Scholar]
- 20.Lao CD, Ruffin MT, 4th, Normolle D, Heath DD, Murray SI, Bailey JM, et al. Dose escalation of a curcuminoid formulation. BMC Complement Altern Med. 2006;6:10. doi: 10.1186/1472-6882-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhen L, Fan D, Yi X, Cao X, Chen D, Wang L. Curcumin inhibits oral squamous cell carcinoma proliferation and invasion via EGFR signalling pathways. Int J Clin Exp Pathol. 2014;7:6438–46. [PMC free article] [PubMed] [Google Scholar]
- 22.Arun P, Sagayaraj A, Mohiyuddin SA, Santosh D. Role of turmeric extract in minimising mucositis in patients receiving radiotherapy for head and neck squamous cell cancer:A randomised, placebo-controlled trial. J Laryngol Otol. 2020;134:159–64. doi: 10.1017/S0022215120000316. [DOI] [PubMed] [Google Scholar]
- 23.Borges GA, Rego DF, Assad DX, Coletta RD, De Luca Canto G, Guerra ENS. In vivo and in vitro effects of curcumin on head and neck carcinoma:a systematic review. J Oral Pathol Med. 2017;46:3–20. doi: 10.1111/jop.12455. [DOI] [PubMed] [Google Scholar]