Abstract
Background:
Discoid lateral meniscus (DLM) has a varied and complex morphology that can be challenging to assess and treat. Preoperative magnetic resonance imaging (MRI) is frequently used for diagnosis and surgical planning; however, it is not known whether surgeons are reliable and accurate in their interpretation of MRI findings when defining the pathomorphology of DLM.
Hypothesis:
Surgeons experienced in treating DLM are able to reliably interpret DLM pathology using MRI.
Study Design:
Cohort study (diagnosis); Level of evidence, 3.
Methods:
Knee MRI scans from 44 patients (45 knees) were selected from a pool of surgically treated patients with DLM. Five reviewers (fellowship-trained pediatric sports medicine surgeons) performed independent review of each MRI scan using the PRiSM Discoid Meniscus Classification. Inter- and intraobserver reliability of the rating factors—primary (width, height, presence of peripheral instability or tear) and secondary (location of instability or tear, tear type)—was assessed using the Fleiss κ coefficient, designed for multiple readers with nominal variables (fair reliability, 0.21-0.40; moderate, 0.41-0.60; substantial, 0.61-0.80; excellent, 0.81-1.00). Reliability is reported as κ (95% CI).
Results:
Interobserver reliability in assessing most primary and secondary characteristics ranged from substantial (meniscal width) to moderate (peripheral instability, anterior instability, posterior instability, and posterior tear). Intraobserver reliability for most characteristics ranged from substantial (peripheral instability, presence of tear, anterior instability, posterior instability, and posterior tear) to moderate (meniscal width, anterior tear, and tear type). Notable exceptions were presence of tear, anterior tear, and tear type—all with fair interobserver reliability. Height had poor interobserver reliability and fair intraobserver reliability.
Conclusion:
Orthopaedic surgeons reliably interpret MRI scans using the PRiSM Discoid Meniscus Classification for the majority of DLM characteristics but vary in their assessment of height and presence and type of tear. MRI evaluation may be helpful to diagnose discoid by width and identify the presence of instability: 2 major factors in the decision to proceed with surgery. Arthroscopic evaluation should be used in conjunction with MRI findings for complete DLM diagnosis.
Keywords: discoid meniscus, magnetic resonance imaging, classification
Discoid lateral meniscus (DLM) is the most common congenital morphologic variant of the meniscus.4,6,10,13 Although it ranges in clinical presentation and corresponding pathology, the ones that require surgery often present with more complex pathomorphology. Preoperative magnetic resonance imaging (MRI) is commonly used for diagnosis and treatment planning. The ability to interpret MRI reliably and descriptively is important for preoperative planning.
Existing classification schemes, such as the commonly used Watanabe classification, 14 lack sufficient description to characterize the full spectrum of DLM pathology and cannot adequately guide treatment. The PRiSM Discoid Meniscus Classification 8 was developed to improve arthroscopic classification of DLM by assessing meniscal width and height and the presence of instability or tears. It was demonstrated in a multicenter analysis to be reliable during arthroscopy and provides a systematic and comprehensive method to characterize meniscal pathology intraoperatively. A common classification scheme for MRI and arthroscopic description of DLM would improve preoperative preparation and intraoperative assessment and allow for descriptive continuity that could benefit patient outcomes, future research, and orthopaedic education.
In the current study, fellowship-trained pediatric sports medicine surgeons acted as independent reviewers to retrospectively apply the PRiSM Discoid Meniscus Classification to preoperative MRI scans of patients who were treated for DLM. The aim was to determine if the classification could be reliably and successfully applied to MRI scans of DLM.
Methods
MRI Selection
A total of 45 MRI scans in 44 patients with varying DLM pathology were selected from a multicenter pool of surgically treated deidentified patients with DLM. All MRI scans were obtained between 2017 and 2019 and were 1.5- or 3-T closed MRI studies. Selected MRI scans had slice thickness ≤5 mm. MRI scans were selected by their quality and for a representative spectrum of pathology.
Videos were captured consisting of the pertinent sagittal, coronal, and axial cuts (all that included the lateral meniscus). This was preferentially done using existing features on the electronic imaging system to save the MRI as a video. If video capture features were not available through the imaging system, sequential scrolling through the MRI scans using smartphone video capture of comparable quality was accepted. The sequences of the pertinent MRI scans were compiled as follows:
Sagittal (T2 or proton density fat saturation): all cuts from fibular styloid (most lateral) to posterior cruciate ligament (most medial).
Coronal (T2 or proton density fat saturation): all cuts from patella (most anterior) to posterior aspect of fibula (most posterior).
Axial (T2 or proton density fat saturation): all cuts from first cut where fibula is visible (most distal) to distal pole of the patella (most proximal).
All videos were deidentified before sharing, with all patient and imaging site identifiers removed. Deidentified videos were uploaded to a secured, protected, internet-based file-sharing platform.
Classification Scheme
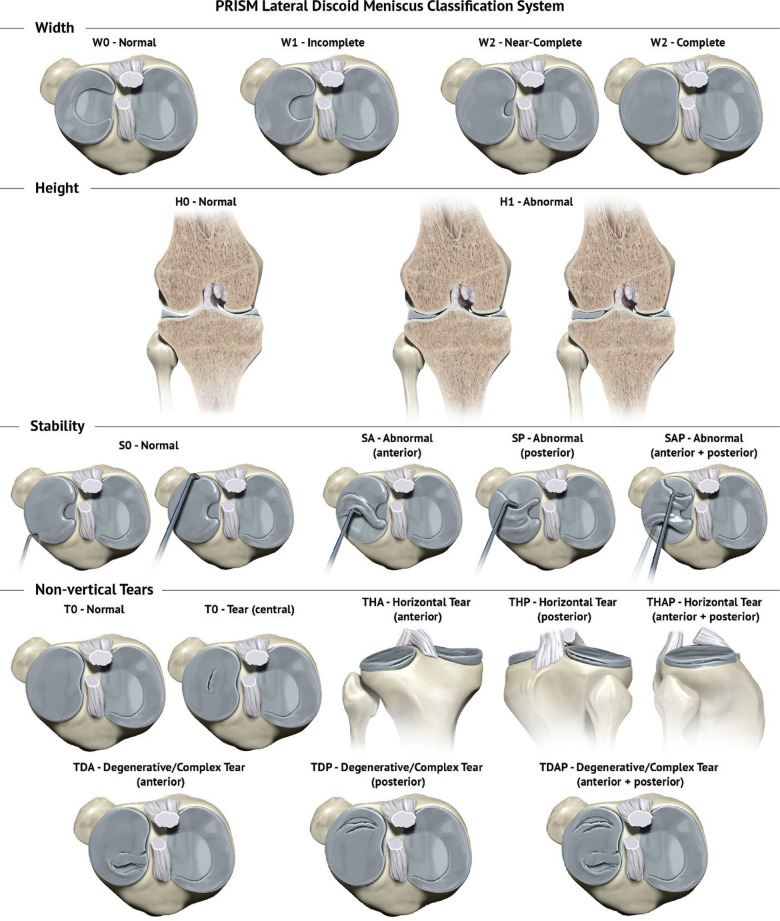
The PRiSM Discoid Meniscus Classification, 8 which describes the DLM arthroscopic characteristics of width, height, instability, and tear pattern (Figure 1), was applied to MRI interpretation. Before the study, reviewers performed a pilot study review on a selection of MRI scans outside the study series. Meetings were then held before initial review to develop a consensus on MRI findings that would correspond to the classification characteristics to improve reliability.
Figure 1.
The PRiSM Discoid Lateral Meniscus Classification. Reproduced with permission from 2021 Children’s Orthopaedic Surgery Foundation.
Width
In the arthroscopic classification, DLM width is categorized as incomplete (W1; <90% coverage of the lateral tibial plateau) and near complete/complete (W2; ≥90% coverage of the lateral tibial plateau). On MRI, this was evaluated on coronal and sagittal views (Figure 2). On coronal views, if the central edge of the meniscus does not touch the lateral tibial spine, the meniscus is classified as incomplete width (W1) (Figure 2A). If the central edge of the meniscus does extend to the lateral tibial spine, this would be designated as a complete DLM or W2 (Figure 2C). This is then confirmed on the sagittal view. Starting from the notch and scrolling laterally, a W2 meniscus would have no more than 1 consecutive cut where the anterior and posterior horns are visible as separate structures (Figure 2B) as compared with an incomplete W1 (Figure 2D). This technique of evaluating sagittal MRI is particularly useful in differentiating borderline incomplete and near complete DLM.
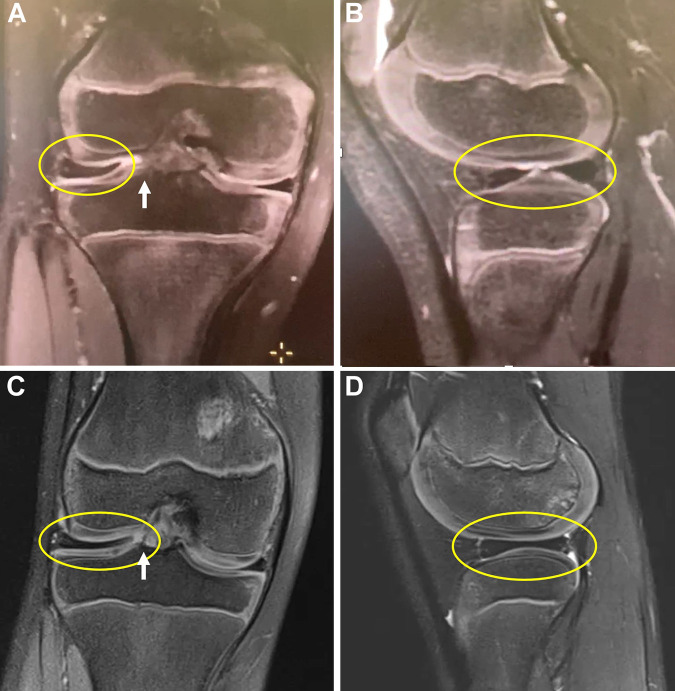
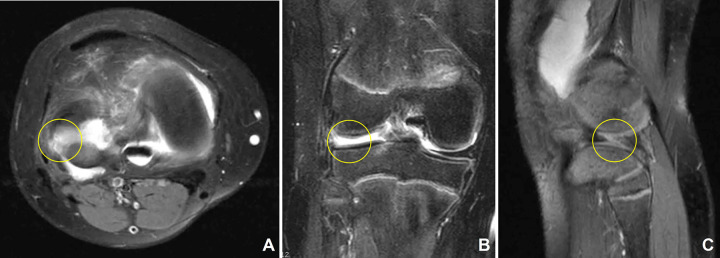
Figure 2.
Discoid lateral meniscus width classification. Incomplete width: (A) Coronal views show that the central edge of the meniscus does not touch the lateral tibial spine. (B) Sagittal image demonstrates separation of anterior and posterior horns for >1 cut, indicating incomplete width. Complete width: (C) Coronal views show that the central edge of the meniscus touches the lateral tibial spine. (D) Sagittal image reveals no separation of anterior and posterior horns.White arrow indicates lateral tibial spine. Yellow ovals highlight the discoid lateral meniscus in each image.
Height
The classification describes meniscal height, or “thickness,” as normal (H0) or abnormal (H1) if it exceeds what is expected as compared with the medial meniscal height and it lacks the expected central taper. For MRI assessment, coronal cuts were assessed for any increased height along any portion of the meniscus as compared with the corresponding medial meniscus (Figure 3). For example, the central edge of the lateral meniscus would be compared with the central edge of the medial meniscus, and the peripheral lateral meniscus would be compared with the peripheral medial meniscus.
Figure 3.
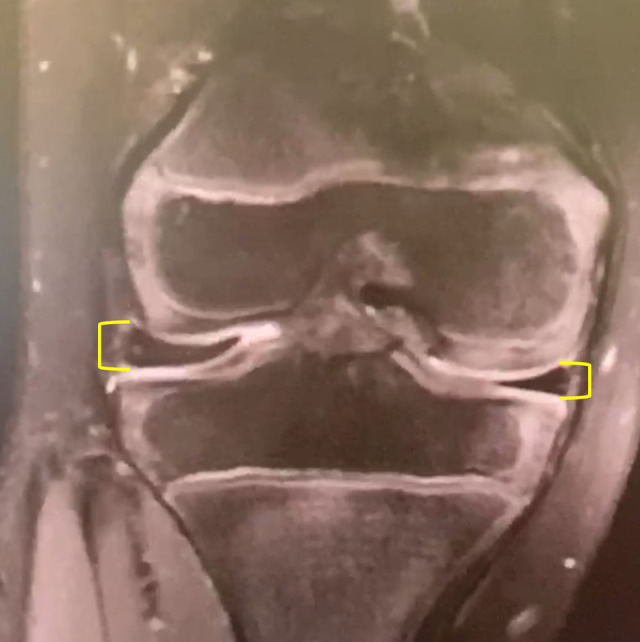
Discoid lateral meniscus height classification. Coronal cuts were used to compare the discoid lateral meniscus height to the corresponding medial meniscus. Increased height along any portion of the lateral meniscus was classified as abnormal. Yellow brackets indicate the height of the lateral and medial meniscus, demonstrating increased height of the lateral meniscus as compared with the medial meniscus at the peripheral portion of the meniscus.
Instability
The classification describes instability as absent or insufficient meniscocapsular attachments or vertical tear. This is demonstrated on arthroscopy by the ability to use a probe to translate the meniscus past the midpoint/apex of the convexity of the lateral femoral condyle. Instability is categorized as normal stability, abnormal stability in anterior half (SA), abnormal stability in posterior half (SP), and abnormal stability in anterior and posterior meniscus (SAP). Given the limitations in MRI evaluation as compared with arthroscopic evaluation to evaluate a dynamic finding such as instability, this scheme was simplified for MRI classification purposes.
Specifically, the MRI classification required only identification of the presence or absence of instability as a primary characteristic and, if present, whether it was in the anterior or posterior half of the meniscus (anterior instability, yes or no; posterior instability, yes or no). Of note, peripheral vertical tears were included in the instability category rather than the tear category because the presence of a peripheral vertical tear contributes to instability. It is also often difficult to differentiate a vertical peripheral meniscal tear from absence or insufficiency of meniscocapsular attachments.
The DLM was first evaluated on sagittal cuts (Figure 4). Obvious signs of instability included displacement or extrusion of the meniscus anteriorly or posteriorly, with anterior displacement reflecting posterior instability and posterior displacement reflecting anterior instability (Figure 4, A and C). Additionally, a thickened appearance of the anterior or posterior horn of the meniscus relative to the opposite horn (“megahorn”) was considered a sign of instability, with the location of increased thickness corresponding to the direction of displacement and the opposite horn being the site of instability (Figure 4, B and D).
Figure 4.
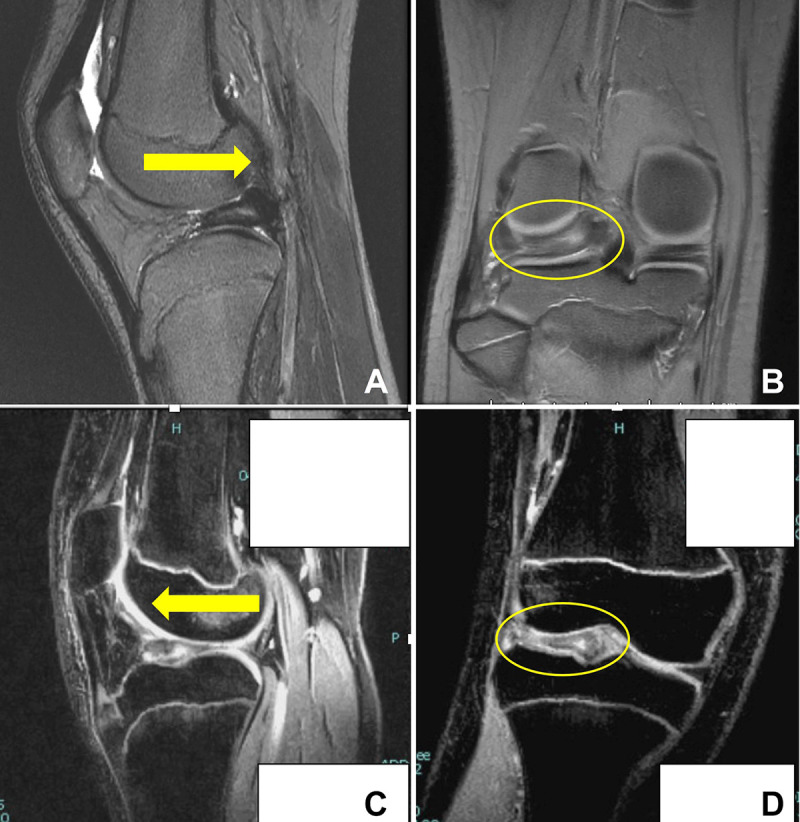
Discoid meniscus instability classification. Signs of anterior instability: (A) Arrow indicates direction of instability with attenuated appearance of meniscus anteriorly. (B) Thickened appearance of posterior horn of the meniscus relative to the opposite horn (posterior “megahorn”). Signs of posterior instability: (C) Yellow arrow indicates direction of instability with absence of meniscus posteriorly. (D) Thickened appearance of anterior horn of the meniscus relative to the opposite horn (anterior “megahorn”).Yellow oval in B and D highlight the DLM with a thickened appearance on coronal images at the posterior aspect of the knee (B) and the anterior aspect of the knee (D).
Additionally, a more subtle sign of posterior instability (SP) was the absence of popliteomeniscal fascicles with associated increased signal, indicating insufficient meniscocapsular attachments (Figure 5A). Notably, the presence of increased signal along the anterior or posterior horn alone in the absence of these other findings was not considered a specific finding associated with instability, as this could be seen in cases with knee effusion (Figure 5B).
Figure 5.
Identifying subtle instability of the discoid lateral meniscus on sagittal magnetic resonance imaging in the absence of obvious displacement. (A) Absence of popliteomeniscal fascicle (blue arrowhead) indicates insufficiency of the meniscocapsular attachment posteriorly. (B) Increased signal adjacent to the posterior horn alone with popliteomeniscal fascicle (yellow arrow) is not a sign of posterior instability.
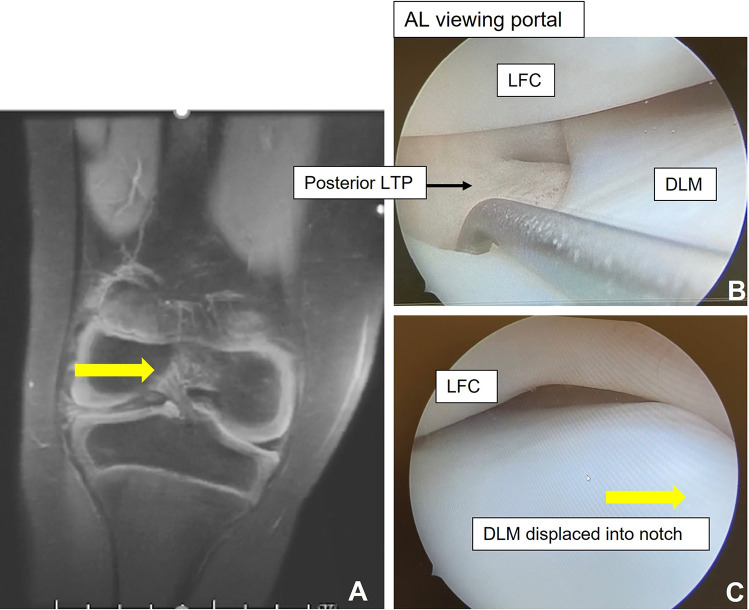
The coronal cuts were then reviewed. Obvious displacement of the meniscus into the notch, with or without attenuation along the peripheral body of the meniscus, was indicative of instability along the body of the meniscus and defined as positive instability in the anterior and posterior halves of the meniscus (SAP) (Figure 6).
Figure 6.
(A) Coronal magnetic resonance imaging of the right knee demonstrates displacement of the DLM into the notch, with yellow arrow indicating direction of displacement. (B) Arthroscopic comparison of the same knee shows instability along the body and (C) displacement of the DLM into the notch (yellow arrow identifies direction of displacement). AL, anterolateral; LFC, lateral femoral condyle; LTP, lateral tibial plateau.
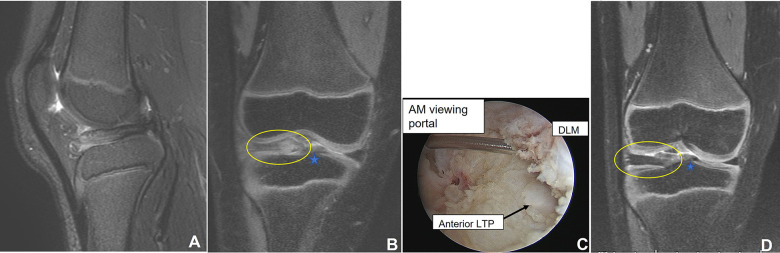
The coronal cuts were useful to look for subtle anterior instability without clear displacement. If the anterior horn or anterior root of the meniscus was not clearly visualized at the anterior tibial attachment of the ACL, this was considered a sign of anterior instability (SA) (Figure 7).
Figure 7.
Identifying subtle instability of the discoid lateral meniscus (DLM) on coronal magnetic resonance imaging in the absence of obvious displacement. (A) No obvious displacement or instability identified on sagittal image. (B) On the coronal cut at the anterior tibial insertion of the anterior cruciate ligament (blue star), there is an attenuated appearance of the anterior horn of the DLM near the root corresponding to (C) arthroscopic identification of instability at the anterior horn and root. (D) Sample DLM without anterior instability. The anterior horn is well visualized on the coronal cut at the anterior tibial insertion of the anterior cruciate ligament (blue star). Yellow ovals highlight the DLM on coronal images. AM, anteromedial; LTP, lateral tibial plateau.
Tear
In the arthroscopic classification, no tear or a tear in the central portion/saucerization zone is T0. When a tear is present, it is defined as either a horizontal tear (TH) or a degenerative/complex/radial tear (TD). These are further classified by location of tear in the anterior or posterior half of the meniscus or both:
For horizontal tear (TH): anterior half, posterior half, or anterior and posterior
For degenerative/complex/radial tear: anterior half, posterior half, or anterior and posterior half
Given the noted limitations of MRI assessment, the categories were simplified for MRI review. The primary characteristic was presence or absence of tear. Secondarily, tear location was defined as anterior (yes or no) and posterior (yes or no) and tear type as no tear, horizontal tear, or complex/degenerative tear. Horizontal cleavage tears were noted to appear as an increased linear signal within the meniscal tissue (Figure 8). Radial tears could sometimes be viewed on axial cuts (Figure 9A) but otherwise were identified by a gap interrupting the circumferentially oriented fibers of the meniscus (Figure 9B) and extending from the central into the peripheral portion of the meniscus. Finally, if multiple tear patterns were seen, the tear was defined as complex/degenerative.
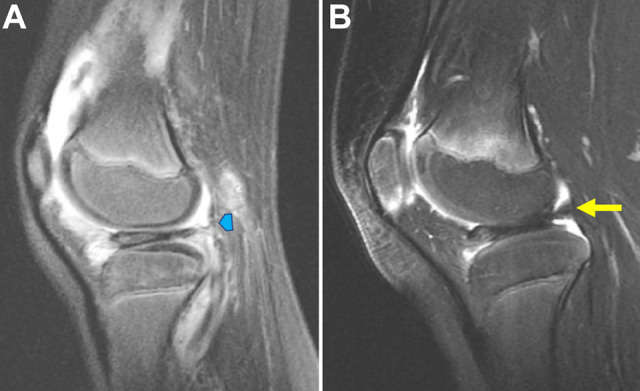
Figure 8.
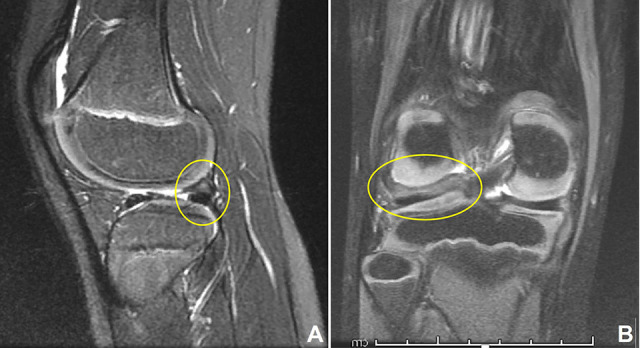
Horizontal cleavage tears appear as an increased linear signal within the meniscal tissue. (A) Sagittal and (B) coronal cuts demonstrate a horizontal tear in the posterior horn (yellow circles).
Figure 9.
Identification of radial tears (yellow circles): magnetic resonance imaging. (A) Axial sequence of the right knee demonstrates a radial tear at the midbody. More frequently seen on (B) coronal imaging or (C) peripheral sagittal cuts as absence of meniscal tissue.
MRI Review
Five reviewers (J.J.B, C.J.F., E.J., M.D.M., Z.S.S.; all sports medicine fellowship–trained surgeons with >5 years of experience in practice) performed independent reviews of each MRI scan to determine discoid meniscus classification. Reviewers were blinded to arthroscopic classification and treatment. Of the 5 reviewers, 3 (E.J., M.D.M., Z.S.S.) performed a second review of all MRI scans ≥4 weeks later. MRI scans were rerandomized between reviews using random numbers autogenerated by the spreadsheet.
Statistical Analysis
An a priori power analysis determined that a minimum of 40 cases evaluated by 5 orthopaedic surgeon raters was necessary for a properly powered study. Inter- and intraobserver reliability was calculated for primary characteristics, including width, height, and presence or absence of instability or tear. Reliabilities were also calculated for the secondary characteristics of location of instability or tear and tear type. Reliability was assessed using the Fleiss κ coefficient (fair, 0.21-0.40; moderate, 0.41-0.60; substantial, 0.61-0.80; excellent, 0.81-1.00). Fleiss κ was selected because it is designed to assess reliability among multiple readers (>2) with nominal variables.
Results
Of the 44 patients, 28 were female and 16 were male. One patient had bilateral DLM, and both knees were included in the series. The mean age of patients at the time of MRI was 12.8 years (range, 3.5-19 years).
Inter- and intraobserver reliability of primary DLM characteristics (width, height, presence of instability or tear) is listed in Table 1. Interobserver reliability of meniscal width assessment as performed by all 5 reviewers was substantial, while intraobserver reliability was moderate. Assessment of height had poor inter- and intraobserver reliability. Assessment of the presence or absence of peripheral instability had moderate interobserver and substantial intraobserver reliability. The presence or absence of a tear had fair interobserver and substantial intraobserver reliability.
Table 1.
Inter- and Intraobserver Reliability of Primary Discoid Lateral Meniscus Characteristics
| Reliability, Fleiss κ (95% CI) | ||
|---|---|---|
| Characteristic | Interobserver | Intraobserver |
| Width: incomplete/complete | 0.67 (0.58-0.76) | 0.52 (0.35-0.69) |
| Height: normal/abnormal | 0.14 (0.05-0.23) | 0.27 (0.10-0.44) |
| Stability: normal/abnormal | 0.54 (0.45-0.63) | 0.61 (0.44-0.78) |
| Tear: yes/no | 0.39 (0.29-0.48) | 0.68 (0.51-0.85) |
Table 2 lists the inter- and intraobserver reliability in assessing secondary characteristics of DLM on MRI (location of instability, location of tear, tear type). When the presence of instability was determined in the anterior or posterior half of the meniscus, interobserver reliability was moderate, while intraobserver agreement was substantial. Inter- and intraobserver reliability for the presence of a posterior tear was also moderate and substantial, respectively. The exception was identifying the presence of an anterior tear, with fair interobserver reliability and moderate intraobserver reliability. When the type of tear was identified (no tear, horizontal, or complex), interobserver reliability was fair and intraobserver reliability was moderate.
Table 2.
Inter- and Intraobserver Reliability of Secondary Discoid Lateral Meniscus Characteristics
| Reliability, Fleiss κ (95% CI) | ||
|---|---|---|
| Characteristic | Interobserver | Intraobserver |
| Instability location | ||
| Anterior: yes/no | 0.47 (0.37-0.56) | 0.68 (0.51-0.85) |
| Posterior: yes/no | 0.56 (0.47-0.65) | 0.62 (0.45-0.79) |
| Tear location | ||
| Anterior: yes/no | 0.33 (0.23-0.42) | 0.56 (0.39-0.73) |
| Posterior: yes/no | 0.41 (0.32-0.50) | 0.69 (0.52-0.86) |
| Tear type: none/horizontal/complex | 0.34 (0.28-0.41) | 0.55 (0.43-0.67) |
Discussion
The ability to preoperatively assess DLM characteristics such as tears and instability improves surgeon preparedness and may help determine the possible repair or stabilization technique that is required. Thus, an MRI classification that can be reliably and accurately used by the surgeon is critical for patient care. A previously described arthroscopic PRiSM Discoid Meniscus Classification was utilized in MRI interpretation in pediatric patients. This study found that for most characteristics evaluated, inter- and intraobserver reliability was substantial or moderate. The exceptions were assessment of height (poor interobserver and fair intraobserver reliability) and presence of tear, presence of anterior tear, and tear type (all with fair interobserver reliability).
The classification by Watanabe et al 14 is an arthroscopic classification of discoid meniscus that is widely used, assessing the size of the meniscus as complete or incomplete and whether there is posterior instability. Despite its prevalence and straightforward application, it is notably limited in its ability to describe the wide spectrum of pathology that is possible in DLM, which in turn limits its usefulness in guiding treatment. With the development of MRI as an accurate method of diagnosing DLM,2,11 others1,7,16 have proposed MRI-based classification schemes to try to address these limitations.
Ahn et al 1 proposed an MRI classification in pediatric patients (age <17 years; mean age, 9.8) using the principle of meniscal shift: no shift and anterocentral, posterocentral, and central shift. The presence of shift on MRI predicted the presence of peripheral tear seen arthroscopically, with sensitivity 65.8%, specificity 78.9%, and accuracy 72.4%. Although direction of shift was suggested as a corollary to location of peripheral tear, statistical correlation of the direction of the shift with the location of peripheral tear was not performed because the study was underpowered. The authors suggested a positive correlation between the presence of meniscal shift on MRI and meniscal repair, although this did not reach statistical significance (P = .19).
There are a few limitations to the classification scheme proposed by Ahn et al. 1 In describing only meniscal shift direction, they restrict their description to peripheral tears and instability and did not demonstrate a correlation of direction of shift with the location of the tear. Yilgor et al 15 utilized the Ahn classification in their arthroscopic comparison study and found that while MRI was highly sensitive and specific (97.8 and 100%, respectively) in determining the presence of a tear, the results were more variable when determining tear type. Of note, the patient population in the Yilgor study (median age, 26 years; range, 5-59) consisted of mostly adult patients, and the Ahn classification, based on a pediatric discoid population, may not be applicable to an adult population. Finally, in the Ahn et al study, peripheral tears were found in 13 of 43 cases categorized as no shift on MRI (false negative rate, 30.2%). It was noted by the authors that since MRI is taken with the knee in extension, a peripheral tear may be present without a shift if it is reduced at the time of the MRI.
Yoo et al 16 presented an MRI classification in pediatric patients (mean age, 10.9 years; range, 4.3-17.6) that elaborated on the concept of meniscal shift proposed by Ahn et al. 1 In their study, Yoo and colleagues evaluated signal changes (grade 0, none; grade 1, dotlike signal; grade 2, linear or bandlike signal; grade 3, linear or band extending to meniscal surface), as well as morphologic changes (variation in meniscal thickness or presence and direction of displacement). MRI review was completed by a radiologist and a fellowship-trained orthopaedic surgeon, blinded to arthroscopic findings. The classification was then compared with arthroscopic results. Notably, while intraobserver reliability was moderate to good for signal and morphologic changes and interobserver reliability was moderate for morphologic changes (intraclass correlation coefficient, 0.654), it was poor (0.311) for signal changes. The accuracy in predicting a tear in DLM was 76%, and the negative predictive value was 44%. A statistically significant correlation was found between the presence of meniscal tear and morphologic changes (P = .001). However, there was no specific correlation with tear pattern. Signal change classification had limited value in predicting tear.
Jung et al 7 proposed an MRI classification using 3 criteria and compared these with arthroscopic findings and surgical procedures: criterion 1, linear meniscal signal intensity extending to the articular surface; criterion 2, deformation or displacement of the meniscus; and criterion 3, signal change within the meniscus irrespective of deformation and displacement. Three orthopaedic surgeons blinded to arthroscopic results performed independent MRI review. Notably, Fleiss κ coefficient values for criteria 1 and 2 had fair agreement (0.337 and 0.367, respectively), and the κ value of criterion 3 had moderate agreement (0.447). Given that criterion 3 (signal change) had the highest κ value and accuracy and sensitivity after arthroscopic assessment, it was chosen by the authors as the most reliable criterion for predicting presence of tear. Further subgrouping based on the presence of deformation or displacement was then performed to postulate type and location of tear.
While Jung et al 7 did find associations between the subgroupings and the types of tears found and type of surgery performed, their finding of signal change being a reliable and useful predictor of tear seems to contradict the finding of Yoo et al. 16 Jung et al themselves note in their limitations a high false-positive rate using their classification owing to the low specificity (41.2%). Additionally, their patient population was significantly older (mean age, 30.1 years; range, 7-69); therefore, this classification may not be applicable to a pediatric population.
The PRiSM Discoid Meniscus Classification seeks to provide the most comprehensive description of discoid meniscus in its full spectrum of pathology. Similar to that by Ahn et al 1 and Yoo et al, 16 the classification includes the presence or absence of peripheral tears and instability. However, the classification recognizes that peripheral tears and instability can exist with other tear patterns, such as horizontal and radial/complex tears, whereas preexisting classifications were limited in their ability to describe these patterns in combination. While preceding MRI classifications used displacement in lieu of location of peripheral tear or did not describe location of tear, the PRiSM Discoid Meniscus Classification specifies the location of tears and instability within the anterior or posterior half of the meniscus. This is especially important given the high reported rate of anterior peripheral rim instability in DLM. 5 The anterior horn is an area that can be difficult to assess arthroscopically; as such, tears and peripheral instability are easily missed. While a systematic arthroscopic diagnostic approach3,8 is important to evaluate the discoid meniscus, having an idea of the location of instability or tears preoperatively can help direct attention and improve accuracy of arthroscopic evaluation.
Increased thickness, or height, is a factor not previously evaluated in discoid classification schemes, though it is a common feature in discoid menisci. Abnormal height of a discoid meniscus is a potential contributing factor to the classic presentation of the “snapping” knee, with the thicker meniscus catching between the femoral condyle and tibial plateau. 9 It also may be a contributing factor in the development of intrasubstance degenerative changes and horizontal cleavage tears. This pathomorphologic process and the optimal treatment of abnormal height and horizontal tears of the meniscus are not well-elucidated. The PRiSM Discoid Meniscus Classification includes meniscal height as a category to capture the true incidence of abnormal thickness to enable further research into proper treatment. The inclusion of height may have the added benefit of aiding in MRI identification of certain discoid menisci that may otherwise be missed on imaging based on a “bow-tie sign” or increased width definition alone. Specifically, Sohn et al 12 found that certain tear types, such as a large radial tear, displaced bucket-handle tear, or inverted-flap tear, can obscure the diagnosis of a DLM on MRI because of the absence of the classic bow-tie sign.
Statistically, the disagreement among reviewers in classifying abnormal height was due to the majority of DLM being thicker than normal meniscus. Therefore, any rating of normal height constituted a significant outlier that affected reliability. Meniscal height is variable at baseline, and only the rare mild partial discoid can at times present with height or thickness within normal ranges. Rather than this being an inherent flaw in the classification or our definition of abnormal height, it more likely reflects the prevalence of abnormal height as a quality of discoid meniscus and furthermore how we as surgeons have only begun to explore its significance.
Limitations
We did not use a radiologist to develop our classification or during the review process. As this classification scheme is intended for use by surgeons to aid in surgical decision making, during study design, we elected to demonstrate reliability among surgeons without the addition of a radiologist reviewer. The reviewers are experienced in the surgical treatment of discoid meniscus and routinely interpret MRI preoperatively independent of the radiology report. These methodology decisions were made to improve the results of the study. However, given that the reviewers have a special interest in treatment of discoid meniscus, took part in the development of the classification, and underwent a pre-review pilot study to improve rater reliability, this study likely represents the optimal scenario for application of the classification. It is likely that surgeons and radiologists who did not take part in the study will not be able to apply the classification to MRI interpretation with the same degree of reliability, thus potentially limiting its widespread use.
There are inherent limitations to using MRI to classify a structure or characteristic that to a degree relies on tactile feel and dynamic observation. This affected the interobserver agreement of presence and type of tears. Additionally, since the MRI scans were selected from a multicenter pool of surgically treated patients with DLM, the study sample likely reflects a more severe spectrum of symptomatic disease, skewed toward more complex and combined tear patterns. This complexity likely affected reliability in the study and may not be generalizable to all cases of DLM.
Finally, we did not evaluate the accuracy, sensitivity, or specificity of the classification by corroborating MRI findings with arthroscopic findings or treatment modalities. Future prospective studies will determine the accuracy of the PRiSM Discoid Meniscus Classification between MRI and arthroscopy.
Conclusion
The PRiSM Discoid Meniscus Classification, based on an arthroscopic evaluation, can be reliably applied to MRI. The characteristics found to be less reliable—height and location/type of tear—have not been described in previous MRI classification schemes of DLM. These DLM characteristics can interject considerable variation in treatment approaches, as they are minimally studied and warrant inclusion in a DLM classification scheme.
MRI evaluation can reliably be used to diagnose DLM by width and identify the presence of instability, which are key factors in the decision to proceed with surgery. However, definitive treatment should be guided by not only the results of MRI but the patient history and physical examination. Further studies are required to assess the accuracy of the classification scheme, as well as to determine best practice in treating the spectrum of DLM pathology.
Acknowledgment
The authors acknowledge the following members of the Pediatric Research in Sports Medicine (PRiSM) Meniscus Research Interest Group for their case contributions to this study: Matt Brown, MD; Sasha Carsen, MD; Brian Haus, MD; Benton E. Heyworth, MD; Jay Lee, MD; Lee Pace, MD; John Schlechter, MD; Tyler Stavinoha, MD; and Mark Tompkins, MD.
Footnotes
Final revision submitted January 25, 2023; accepted February 26, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: E.L.N. has received education payments from Arthrex and hospitality payments from Smith & Nephew and Vericel. M.D.M. has received education payments from Kairos Surgical. C.J.F. has received education payments from Medwest Associates. Z.S.S. has received education payments from Arthrex and Fones Marketing Management and hospitality payments from Stryker. J.J.N. has received education payments from Elite Orthopedics; consulting fees from Ceterix, Responsive Arthroscopy, and Smith & Nephew; nonconsulting fees from Smith & Nephew; and royalties from Responsive Arthroscopy. G.A.S. has received education payments from Summit Surgical. J.J.B. has received education payments from Arthrex and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1.Ahn JH, Lee YS, Ha HC, Shim JS, Lim KS. A novel magnetic resonance imaging classification of discoid lateral meniscus based on peripheral attachment. Am J Sports Med. 2009;37(8):1564–1569. [DOI] [PubMed] [Google Scholar]
- 2.Araki Y, Ashikaga R, Fujii K, et al. MR imaging of meniscal tears with discoid lateral meniscus. Eur J Radiol. 1998;27(2):153–160. [DOI] [PubMed] [Google Scholar]
- 3.Beck JJ, Schlechter J, Schmale G, Haus B, Lee J. Comprehensive arthroscopic characterization of discoid meniscus tears and instability using the PRiSM Discoid Meniscus Classification. Arthrosc Tech. 2022;11(7):e1347–e1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dickhaut SC, DeLee JC. The discoid lateral-meniscus syndrome. J Bone Joint Surg Am. 1982;64(7):1068–1073. [PubMed] [Google Scholar]
- 5.Good CR, Green DW, Griffith MH, Valen AW, Widmann RF, Rodeo SA. Arthroscopic treatment of symptomatic discoid meniscus in children: classification, technique, and results. Arthroscopy. 2007;23(2):157–163. [DOI] [PubMed] [Google Scholar]
- 6.Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthop Surg. 1996;4(4):191–200. [DOI] [PubMed] [Google Scholar]
- 7.Jung EY, Jeong S, Kim SK, Lee SS, Ryu DJ, Wang JH. A useful MRI classification for symptomatic discoid lateral meniscus. Knee Surg Relat Res. 2021;33(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee RJ, Nepple JJ, Schmale GA, et al. PRiSM Meniscus Research Interest Group. Reliability of a new arthroscopic discoid lateral meniscus classification system: a multicenter video analysis. Am J Sports Med. 2022;50(5):1245–1253. [DOI] [PubMed] [Google Scholar]
- 9.Morrissey RT, Weinstein SL. Sports medicine in the growing child. In: Morrissey RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopaedics. 6th ed. Lippincott Williams & Wilkins; 2006:1393–1394. [Google Scholar]
- 10.Neuschwander DC, Drez D, Jr, Finney TP. Lateral meniscal variant with absence of the posterior coronary ligament. J Bone Joint Surg Am. 1992;74:1186–1190. [PubMed] [Google Scholar]
- 11.Ryu KN, Kim IS, Kim EJ, et al. MR imaging of tears of discoid lateral menisci. AJR Am J Roentgenol. 1998;171(4):963–967. [DOI] [PubMed] [Google Scholar]
- 12.Sohn DW, Bin SI, Kim JM, Lee BS, Kim SJ. Discoid lateral meniscus can be overlooked by magnetic resonance imaging in patients with meniscal tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2317–2323. [DOI] [PubMed] [Google Scholar]
- 13.Washington ER, 3rd, Root L, Liener UC. Discoid lateral meniscus in children: long-term follow-up after excision. J Bone Joint Surg Am. 1995;77(9):1357–1361. [DOI] [PubMed] [Google Scholar]
- 14.Watanabe M, Takeda S, Ikeuchi H.Atlas of Arthroscopy. 2nd ed. Springer-Verlag; 1969. [Google Scholar]
- 15.Yilgor C, Atay OA, Ergen B, Doral MN. Comparison of magnetic resonance imaging findings with arthroscopic findings in discoid meniscus. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):268–273. [DOI] [PubMed] [Google Scholar]
- 16.Yoo WJ, Lee K, Moon HJ, et al. Meniscal morphologic changes on magnetic resonance imaging are associated with symptomatic discoid lateral meniscal tear in children. Arthroscopy. 2012;28(3):330–336. [DOI] [PubMed] [Google Scholar]