Abstract
Objectives
To prospectively evaluate parent supportive behaviors (PSB) for child physical activity (PA) and neighborhood environment variables on changes in child PA over 3 years.
Study design
Secondary data analysis of the Now Everybody Together for Amazing and Healthful Kids-Works study with 534 parent-child (age 2-4 years) dyads randomized to a community-based pediatric obesity prevention intervention for 3 years (92% retention). PSB and neighborhood environmental variables were examined in relation to changes in child moderate-to-vigorous PA (MVPA), light and sedentary activity, and screen time. Child and parent accelerometry data were collected at visit 0, 12, 24, and 36 months. Mixed multivariate models were used to examine independent and interactive effects of parent-level and neighborhood-level variables on changes in child PA outcomes.
Results
PSB significantly interacted with visit on change in child MVPA (β = 0.12) and sedentary behaviors (β = -0.18). Over 3 years, a 1-unit increase in PSB was associated with an average increase of 4.3 minutes/day of MVPA and an average decrease of 6.5 minutes/day of sedentary time. Significant main effects were observed for PSB and 3-year change in child screen time (β = -0.05). The children of parents with higher PSB at baseline watched an average of 1.8 fewer minutes/day of screen time compared with parents with lower baseline PSB. Neighborhood-level variables were not significantly associated with changes in child PA outcomes.
Conclusions
Parents who increase their supportive behaviors for their child's PA have children who are more physically active and less sedentary over time. Interventions to increase preschool-age children's PA may enhance their effectiveness by targeting parents' supportive behaviors for their child's PA.
Keywords: physical activity, child, parent support, longitudinal, neighborhood
Physical activity (PA) in children can promote a healthy body weight and reduce cardiometabolic risk factors.1, 2, 3, 4, 5, 6, 7 However, 46% of preschool-age children do not meet the recommendations for daily 60 minutes of moderate-to-vigorous PA (MVPA).8 Children from low income households show larger declines in PA compared with higher income children during the transition into adolescence,9 and this reflects a broader pattern of health disparities by socioeconomic status.9, 10, 11, 12, 13, 14, 15, 16, 17
In a social determinants of health framework, the neighborhood environment and parent supportive behaviors (PSB) for child PA are potential important influences on developmental trajectories of PA in children from low income households.18, 19, 20, 21, 22, 23, 24 “Neighborhood environment” is a complex, multidimensional construct22,25, 26, 27, 28 that may include physical features, such as proximity to playgrounds, parks, and green spaces, the presence of retail food outlets, as well as socioeconomic characteristics such as neighborhood poverty, safety dimensions such as traffic or crime danger (objective or perceived), and unemployment rates. Previous research on the neighborhood environment and child PA generally focused on crime and traffic safety22,26 and economic variables.29, 30, 31 However, new measures of the environment have been developed to capture the broader social determinants of health constructs that include neighborhood-level social, educational, economic, and health environmental components.32, 33, 34
In theory, parent behaviors that support child PA could overcome or mitigate neighborhood limitations that otherwise might inhibit child PA. PSB include modeling PA, such as doing PA with their child, and coordinating PA logistics, such as taking the child to places for PA. Both PSB—modeling and coordinating PA for children—are consistently associated cross-sectionally with higher child PA.35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47 Parent decisions about where and when preschool-age children can be physically active may or may not be bounded by the neighborhood environment, including parent perceptions of neighborhood safety, walkability, and availability and quality of recreational opportunities.26,28,29,35, 36, 37, 38,40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50
Solutions to promote low-income preschool-age children's PA can be strengthened by better understanding how parent-level and neighborhood-level variables interact or independently contribute.26,29,35, 36, 37, 38, 39, 40 The present longitudinal study examines the influence of neighborhood environment and PSB on changes in child PA over a 3-year period. The study is a secondary data analysis from the Now Everybody Together for Amazing and Healthful Kids (NET)-Works randomized controlled trial (2010-2018).51 It was hypothesized that neighborhood environment and PSB would independently influence changes in child PA over a 3-year period. In addition, PSB were hypothesized to interact with neighborhood variables, such that adverse neighborhood environments would have a negative impact on children's decline in PA only when PSB were low.
Methods
The NET-Works study (2012-2010) was a 3-year, parent-targeted, multilevel community-based childhood obesity prevention intervention.51 Over an 18-month period, 534 low-income, racially/ethnically diverse parent-child dyads were recruited through 14 primary care clinics in the Minneapolis-St Paul metro area. Home measurement visits were completed across all seasons at baseline (prior to randomization), 12, 24, and 36 months. Parent-child dyads were randomized to a multilevel, parent-targeted obesity prevention intervention or to a usual-care comparison group. Intervention components included home visiting, community parenting classes, and linkages to neighborhood PA and food resources through the home visiting and parenting class components. More details about the intervention are reported elsewhere.51 Cohort retention in the parent study was 92% at 36 months. This study was reviewed and approved by the University of Minnesota IRB. All parents consented to participate.
This research used the following measures from the NET-Works parent study: (1) neighborhood environment variables that include an objective composite index summarizing neighborhood socioeconomic, health, environmental, and educational resources, and a set of parent-reported neighborhood safety variables; (2) parent behavior variables, including PSB (self-report) and parent PA (accelerometry); and (3) child PA (accelerometry). NET-Works data were collected in participants' homes by trained research staff at baseline, 12, 24, and 36 months.
Child Opportunity Index
The childhood opportunity index (COI)32 was used in the parent study NET-Works to capture several constructs of neighborhood influences that might be most relevant for preschool-age to elementary-school-age children from low-income families. Home addresses from NET-Works families at baseline were geocoded and linked to neighborhood assessments of child opportunity and disadvantage at the level of the census tracts to create the COI (www.diversitydatakids.org).32 Drawing from the social determinants of health field, neighborhood-level social and economic, education, and health and environment indicators were constructed from several neighborhood-level indicators of these constructs. The COI is a composite measure of items derived from census data for specific zip codes and includes neighborhood-level indicators of educational, economic, social, and health opportunities.32 Example variables for each of the 3 subareas include (1) social and economic opportunity (neighborhood foreclosure rate, poverty rate, unemployment rate, public assistance rate, proximity to employment); (2) health and environmental opportunity (retail healthy food availability, proximity to toxic waste release sites, volume of nearby toxic release, proximity to parks and open spaces, housing vacancy rates, proximity to health care facilities); and (3) educational opportunity (adult educational attainment, student school poverty rate, reading proficiency rate, math proficiency rate, early childhood education neighborhood participation patterns, high school graduate rate, proximity to high quality [accredited] early childhood education centers, proximity to early childhood education centers of any type), where lower index scores reflect worse neighborhood conditions. The census data derived measures are converted to z scores to capture neighborhood level position on the variables. The composite Cronbach alpha coefficient was .9133 Categories were used in this analysis to compare neighborhoods with very low/low opportunity and moderate/high opportunity.32, 33, 34
Perceived Neighborhood Safety (Parent-Reported)
Parents reported the extent to which they agreed or disagreed with each of the following statements about traffic density, road safety, and walking safety in their neighborhood48,49: (1) “There is heavy traffic in our local streets”; (2) “There are no lights/street crossings for us to use”; (3) “We have to cross several streets to get to play areas"; (4) “It is safe to walk in the neighborhood”; (5) “Our neighborhood is safe from crime.” Response options were strongly agree; agree; neither; disagree; and strongly disagree.
Parent behavior variables were selected based on the theoretical model for the NET-Works parent study,21 and from the empirical literature on parent variables associated with child PA.35,37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51 Parent supportive behaviors specifically related to child PA include role modeling and logistic behaviors such as verbal encouragement, watching their child play, playing with their child, taking the child to places for play, such as parks and playgrounds.36 The questions were (1) “During the past week how often have you encouraged this child to be active or actively play?”; (2) “During the past week how often have you done a physical activity or actively played with this child?”; (3) “During the past week how often have you taken this child to a place where he/she can do physical activities or active play?’; (4) “During the past week how often have you watched this child take part in physical activities or active play outside the home?”. Response options were never; once; sometimes; almost daily; and daily.
Three additional parent supportive behaviors questions were asked: (1) “Do you limit active play indoors?”; (2) “Do you limit outdoor play in your yard?”; and (3) “Do you limit outdoor play in the neighborhood?”. Response options were all of the time; most of the time; some of the time; and rarely.
Parent reported enjoyment of PA was also measured with a Likert-scale response format (ie, not at all; a little; neutral; somewhat; a lot).
Local park use with their child was measured by asking the parent to report the frequency with which they visited with their child each specific park or playground within a 1-mile radius around their home as shown to them on a tailored home-specific map.36,51
Child media use was measured with 3 questions reported by the parent: (1) “On an average weekday, how many hours does <this child> watch TV?”; (2) “On an average weekend day, how many hours does <this child> watch TV?”; (3) “On an average day, how many hours does <this child> play video or computer games, or use a computer for something that is not school work? (Include activities such as Play Station, Xbox, hand held video games, computer games, and the Internet.).” The weekday and weekend TV viewing hours were weighted (×5 for weekday and ×2 for weekend day) and summed with the average hours per day of small screen/video game use.51
PA was measured at baseline, 12, 24, and 36 months in both the parent and the child in each enrolled household using a commercially available ActiGraph GT3X+. ActiGraph monitors have been used in numerous studies to assess PA in children.45, 46, 47,50,52, 53, 54, 55 The validity of the ActiGraph has been examined in several studies involving children age 2-18 years.53, 54, 55, 56, 57, 58, 59 The index children and parent in the study wore the GT3X+ monitor on the right hip for 7 complete days. The monitoring period included 2 weekend days and 5 weekdays. The valid wear time criteria (minimums) were 4 days (3 weekdays and 1 weekend day) of at least 6 hours of awake time per day with 33% nonzero epochs per hour. Accelerometry data were used to create minutes of sedentary activity, light activity, and moderate and vigorous PA, using child-specific and adult-specific cutpoints.8,60 Minutes per day, standardized to a 12-hour wear-time day, were computed for sedentary activity, light activity, and moderate/vigorous PA.
Demographic variables were self-reported by the participating parent and included child age, sex, race, ethnicity, parent age, sex, race, ethnicity, employment status, household income, and education. Parent and child height and weight were measured with the participant in light clothing without shoes according to a standardized protocol. Weight was measured to the nearest kilogram and height was measured to the nearest 0.1 centimeter. Measures were conducted in duplicate and averaged. Body mass index (BMI) was computed as weight in kilograms divided by the square of height in meters.
Statistical Analyses
Analyses were conducted using SAS v 4.0 (SAS Institute) and R version 3.6.2 (R Core Team, 2019). Mixed model regression was used to examine associations between each of the baseline neighborhood variables, mean and change over time in parent supportive behaviors, and mean and change over 36 months in child PA. Separate models were fit for each of the following dependent variables: change in child MVPA, light activity, sedentary activity, and screen time. Change was examined using the statistical framework of mixed effects models. In the present study, preliminary models were tested with both the fixed effects and the random effects for each of the regression coefficients – the intercept, and the slope terms (for the time variable and the other time-varying covariates). None of the random effects for the time variable and the other time-varying covariates were found to be statistically significant, and thus, were removed from the models. The only random effect that was modeled was for the intercept term. The time predictor and the other time-varying covariates were only allowed to have the fixed-effect.
Potential covariates were selected for inclusion based on a priori knowledge of the literature about demographic differences in child physical activity. Child age, sex, and BMI, and parent education, marital status, and household income, and treatment group assignment, were included in each model as covariates.
Forward model selection was used to determine which neighborhood and parent supportive variables were included in the model. The variables that were significant in individual models were included in a multivariate model with their interaction terms with the time variable to examine their independent and potentially interactive effect on changes in child PA outcomes. Significance was evaluated as the variables showing a nonzero effect with a 95% CI. The variables examined in individual models included the following: parent baseline PA (MVPA, light, and sedentary, for each of those specific child PA outcomes, respectively); parent supportive behaviors (mean of 4 items); parent enjoyment of PA (single Likert-scale item); parent frequency (past month) of taking child to a local park within 1-mile radius of home (visual map-based parks around home); parent perceived neighborhood traffic safety; parent perceived neighborhood safety from crime; parent perceived safe to walk in neighborhood; and the COI (composite-based categorical variable).
The COI has been used as a composite index in previous research. Thus, a priori, the decision was made to use the scale as a categorical composite. In exploratory post-hoc analyses, each of the 3 subindices were examined in multivariate analyses (social/economic; health/environment; education). The reason for this exploratory analysis was to determine whether, in this sample, and for these specific neighborhoods, there might be certain social or economic neighborhood variables that are particularly relevant for PA changes among these young children from racially/ethnically diverse low-income families.
The PA outcome variables had an average of 14.6% missing data across the follow up time points (12, 24, and 36 months; complete PA data were available at baseline on 534 children). The media use variable had an average of 8.6% missing data. The data for all variables were tested for the missing data mechanism and were determined to be missing at random. The missing values were then imputed using the MissMech package in R.61 The imputation was performed using key demographic variables: treatment group, child age, child sex, child BMI, baseline outcome variable, race, highest household education, and annual household income. A sensitivity analysis was performed which showed that the imputed data were not significantly different from the original data based on a 2-sample t test [t (404) = -1.15, P = .25].
Results
Demographic variables, neighborhood, and parent supportive behavior variables at baseline are shown in Table I; 37% of parents reported a household income of less than $15 000 per year, 55% had completed high school or less education, 62% of parents reported that they were not born in the US, 68% were married, and 56% were working for pay full or part time; 58% of children were of Hispanic ethnicity. The average BMI percentile for age and sex was 81.7 (SD = 14.3). PSB were evenly distributed across the response categories (from lower to higher levels of support). Parent perceptions of the neighborhood environment were generally positive across all of the items queried. Perception of crime was low and parents felt safe walking in the neighborhood. The frequency of parent-reported use of parks and green spaces within 1 mile of their home was low (over one-half reported no use) and 74% of families lived in neighborhoods with low or very low child opportunities.
Table I.
Parent, child, and neighborhood environment variables at baseline in the NET-Works Study (N = 534 dyads)
| Household variables | % (N) | Mean (SD)[range] |
|---|---|---|
| Household income (annual; $) | ||
| 1 <$15 000 | 37.6 (201) | |
| 2 $15 000-$24 999 | 25.3 (135) | |
| 3 $25 000+ | 37.1 (198) | |
| Household education | ||
| 1 <High school | 33.3 (178) | |
| 2 High school | Diploma | 22.1 (118) |
| 3 Some college/technical | 25.7 (137) | |
| 4 Bachelor's degree or more | 18.9 (101) | |
| Marital status | ||
| Married | 68.7 (367) | |
| Not married | 31.3 (167) | |
| Employment status | ||
| Full time | 29.8 (159) | |
| Part time | 27.7 (148) | |
| Not working for pay | 42.5 (227) | |
| Child variables | ||
| Age (y) | 3.4 (0.65) [2.1- 4.3] | |
| Hispanic ethnicity | ||
| Yes | 58.4 (312) | |
| No | 41.6 (222) | |
| Race/ethnicity | ||
| Non-Hispanic White | 12.5 (67) | |
| Non-Hispanic Black | 18.4 (98) | |
| Hispanic | 58.4 (312) | |
| Multiracial | 8.4 (45) | |
| Other | 2.2 (12) | |
| Sex | ||
| Female | 50.9 (272) | |
| Male | 49.1 (262) | |
| BMI kg/m2 | 17.6 (1.8) [15.3-27.7] | |
| BMI percentile | 81.7 (14.3) [50.3-99.9] | |
| Child PA (accelerometry) | ||
| MVPA standardized min/d | 78.5 (24.0) | |
| Sedentary PA standardized min/d | 428.4 (46.1) | |
| Light PA standardized min/d | 213.1 (31.6) | |
| Media/screen time (h/d) | 2.8 (1.7) | |
| Parent variables | ||
| Age (y) | 31.9 (6.4) [17.1-67.2] | |
| Sex (female) | 91.7 (486) | |
| BMI kg/m2 | 30.1 (7.0) [17.2-69.4] | |
| Parent PA (accelerometry) | ||
| MVPA standardized min/d | 15.5 (14.4) | |
| Sedentary PA standardized min/d | 441.9 (68.3) | |
| Light PA standardized | 262.6 (62.5) | |
| Parent supportive behaviors for child PA∗ (mean of 4 items) | 2.5 (.82) | |
| 4 = daily; 3 = almost daily | ||
| 2 = sometimes; 1 = once; 0 = never | ||
| 0-1.75 | 22.1 (118) | |
| 2-2.33 | 24.2 (129) | |
| 2.5-2.75 | 23.7 (125) | |
| 3-4 | 30.0 (162) | |
| Parent enjoyment of PA | ||
| Not at all | 3.4 (18) | |
| A little | 12.6 (67) | |
| Neutral | 11.6 (62) | |
| Somewhat | 29.4 (157) | |
| A lot | 43.1 (230) | |
| Local park use with children (past mo) (map around home) | 3.5 (6.6) [0-50] | |
| 0 | 50.9 (268) | |
| 1-2 | 15.3 (81) | |
| 3-5 | 14.1 (74) | |
| 6-50 | 19.7 (104) |
| Neighborhood environment variables∗ | |||
|---|---|---|---|
| COI composites | Social/economic | Health/environment | Education |
| Very low | 11 | 22 | 56 |
| Low | 39 | 151 | 218 |
| Moderate | 75 | 222 | 170 |
| High | 214 | 119 | 75 |
| Very high | 186 | 11 | 6 |
| Perceived neighborhood safety: traffic safety† | 10.0 (2.8) [3-15] | ||
| Neighborhood is safe from crime | |||
| 1 strongly agree | 15.6 (82) | ||
| 2 agree | 39.3 (207) | ||
| 3 neither | 13.5 (71) | ||
| 4 disagree | 23.7 (125) | ||
| 5 strongly disagree | 8.0 (42) | ||
| Safe to walk in neighborhood | |||
| 1 strongly agree | 24.2 (128) | ||
| 2 agree | 52.0 (275) | ||
| 3 neither | 7.8 (41) | ||
| 4 disagree | 10.2 (54) | ||
| 5 strongly disagree | 5.9 (31) | ||
Parent supportive behaviors: During the past week, how often have you encouraged this child to be active or actively play? How often have you done a physical activity or actively played with your child? How often have you taken this child to a place where s/he can do physical activity or active play? Have you watched this child take part in physical activities or active play outside the home?
Traffic safety: there is heavy traffic in our local streets; there are no lights/street crossings for us to use; we have to cross several streets to get to play areas (sum 3 items) 1 = strongly disagree; 5 = strongly agree.
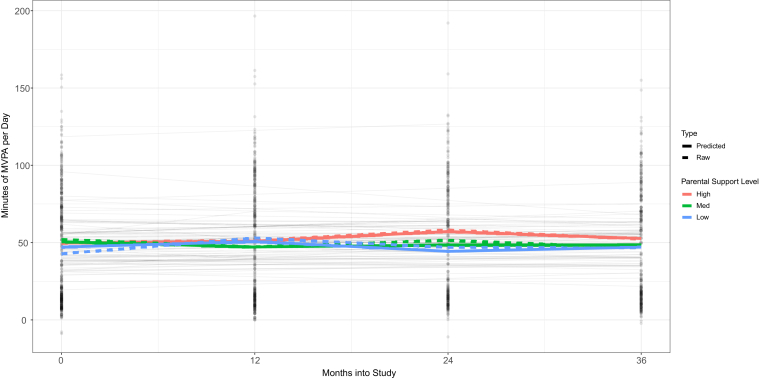
The results of the mixed effects model for change in child MVPA are shown in Table II (top). In this model, PSB showed a significant interaction effect with visit (β = 0.12). This indicates that parents with a one-point higher PSB score have children who increase their MVPA by 4.3 minutes/day over 3 years. Figure 1 shows the pattern of change in MVPA over time by PSB level. Parents who increased their PSB over time (red line) had children whose MPVA minutes per day increased the most over the 3-year period (maximum child MVPA increase at 24 months). These results also show that the baseline effect was nonsignificant. This indicates that the overall level of the parents’ supportive behaviors was less impactful than the sustained increase in the level of PSB over the 3-year period.
Table II.
Neighborhood environment and PSB for child PA: predictors of 3-year change in child PA and screen time
| MVPA (standardized min/d) | ||
|---|---|---|
| Variables | Estimate (SE) | 95% CI |
| Intercept | 107.64 (7.61) | 92.72, 122.56 |
| Visit∗ | −0.25 (.10) | −0.45, -0.05 |
| Treatment | 0.066 (1.98) | −3.81, 3.94 |
| Visit∗ treatment | 0.010 (0.06) | −0.11, 0.13 |
| Age (y) | −1.68 (1.32) | −4.28, 0.91 |
| Sex (ref: boys) | −11.62 (1.71) | −15.00, -8.28 |
| Hispanic (yes) | −0.54 (2.04) | −4.55, 3.46 |
| BMI (kg/m2) | −0.67 (.30) | −1.26, -0.07 |
| Parent MVPA | ||
| (baseline) | 0.10 (.04) | 0.02, 0.17 |
| Parent limit play indoors | ||
| (baseline) | −1.61 (.54) | −2.66, -0.56 |
| PSB × visit | 0.12 (.04) | 0.05, 0.20 |
| Neighborhood COI (ref: high) | −2.44 (2.00) | −6.35, 1.47 |
| Light PA | ||
|---|---|---|
| Variables | Estimate (SE) | 95% CI |
| Intercept | 189.70 (9.79) | 170.50, 208.89 |
| Visit | 0.04 (.06) | −0.07, 0.16 |
| Treatment | 5.05 (2.51) | 0.14, 9.96 |
| Visit∗ treatment | −0.11 (0.09) | −0.28, 0.06 |
| Age (y) | −1.12 (1.58) | −4.20, 1.98 |
| Sex (ref: boys) | 5.21 (2.05) | 1.19, 9.23 |
| Hispanic (yes) | 5.98 (2.48) | 1.13, 10.84 |
| BMI (kg/m2) | 0.35 (0.39) | −0.41, 1.10 |
| Parent light PA | ||
| (baseline) | 0.03 (.01) | 0.01, 0.06 |
| Neighborhood COI (ref: high) | 0.41 (2.38) | −4.24, 5.08 |
| Sedentary activity | ||
|---|---|---|
| Variables | Estimate (SE) | 95% CI |
| Intercept | 392.78 (17.30) | 358.86, 426.69 |
| Visit | 0.32 (0.23) | −0.13, 0.76 |
| Treatment | −5.00 (3.81) | −12.48, 2.48 |
| Visit∗ treatment | 0.13 (0.14) | −0.15, 0.40 |
| Age (y) | 1.50 (2.42) | −3.23, 6.24 |
| Sex (ref: boys) | 4.78 (3.14) | −1.38, 10.93 |
| Hispanic (yes) | −4.34 (3.83) | −11.85, 3.17 |
| BMI (kg/m2) | 0.22 (0.60) | −0.96, 1.41 |
| Parent sedentary | ||
| behavior (baseline) | 0.05 (.02) | 0.02, 0.09 |
| PSB × visit | −0.18 (.09) | −0.35, -0.01 |
| Neighborhood COI (ref: high) | 0.84 (3.64) | −6.30, 7.98 |
| Screen time | ||
|---|---|---|
| Variables | Estimate (SE) | 95% CI |
| Intercept | 1.77 (0.16) | 1.46, 2.09 |
| Visit | −0.001 (.001) | −0.003, 0.000 |
| Treatment | −0.03 (0.04) | −0.11, 0.04 |
| Visit∗ treatment | −0.003 (0.001) | −0.01, 0.00 |
| Age (y) | 0.07 (.03) | 0.02, 0.13 |
| Sex (ref: boys) | −0.13 (.04) | −0.20, -0.07 |
| Hispanic (yes) | −0.08 (.04) | −0.16, -0.002 |
| BMI (kg/m2) | −0.003 (0.01) | −0.02, 0.01 |
| PSB (baseline) | −0.05 (.02) | −0.08, -0.02 |
| Neighborhood COI (ref: high) | −0.06 (.04) | −0.14, 0.02 |
Bolded areas highlight significant variables.
Household income, parent education, and marital status are nonsignificant covariates in all models and are not shown.
Visit is baseline, 12, 24, and 36 months.
Figure 1.
Changes over 3 years in low-income preschool-age children's MVPA by PSB. (PSB less than 2 = “low” and PSB above 2.75 = “high” based on the quantiles of the data).
In addition to PSB, significant main effects were observed for the variables parent MVPA and parent limiting the child's indoor play. Parents who were more active at baseline had children who were more active on average over the 3-year period. Parents who limited indoor play at baseline had children who were less active on average over the 3-year period. In addition, results showed that the average level of MVPA was higher among boys and lower among children with higher BMI. None of the neighborhood environment variables were significantly associated with changes in child MVPA.
The results from the analysis of the change in light PA show no significant interaction effects between any variables and visit (Table II). The significant main effects are as follows: children with parents with more frequent light activity (β = 0.03); female children (β = 5.09); and children of Hispanic ethnicity (β = 5.95) had more minutes per day of light activity over 3 years compared with parents with less frequent light activity, male children, or children of non-Hispanic ethnicity. None of the neighborhood environment variables were significantly associated with changes in child light PA.
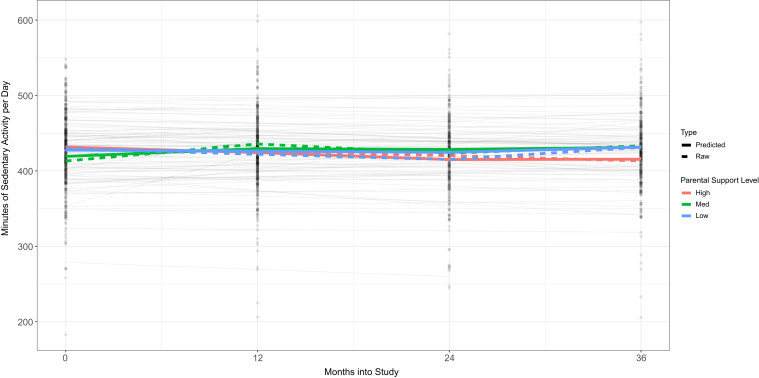
The results from the analysis of the change in sedentary activity show a significant interaction effect between PSB and visit (β = -0.18) (Table II and Figure 2). This indicates that as parents increased their supportive behaviors over time, child sedentary activity decreased by an average of -6.5 minutes/day over 3 years. Figure 2 shows that parents whose PSB increased over time had children whose sedentary activity decreased over time (maximum decrease at 24 months). Significant main effects were observed for parent sedentary activity (β = 0.04; parents with more sedentary activity at baseline had children with on average more minutes of sedentary activity per day over the 3-year period). None of the neighborhood environment variables were significantly associated with changes in child sedentary PA.
Figure 2.
Changes over 3 years in low-income preschool-age children's sedentary activity by PSB. (PSB less than 2 = “low” and PSB above 2.75 = “high” based on the quantiles of the data).
The media use outcome model did not show significant interaction effects for any of the variables with visit (Table II). However, significant main effects were observed for PSB (β = -0.05; parents with higher PSB had children with on average -1.8 fewer minutes per day of media use over 3 years); child age (β = 0.07; older children at baseline had on average more minutes per day of use); and sex (β = -0.13) (boys had on average more minutes per day of media use than girls over the 3-year period). None of the neighborhood environment variables were significantly associated with changes in child media use.
Post-hoc exploratory analyses were conducted to explore the possibility that certain subscales of the COI might be significant predictors of changes in child PA. In these exploratory analyses, we reran the models a second time, including the 3 COI subscales in place of the single composite index. Results showed that only the social/economic subscale was significantly associated with change in child MVPA, sedentary time, and screen time. The direction of association was opposite to expected for MVPA and sedentary time. Higher social/economic neighborhood opportunity was associated with lower overall MVPA, and higher sedentary time. Associations were in the expected direction for media use/screen time, with higher neighborhood opportunity associated with less media use/screen time.
Discussion
Among this sample of lower income, racially/ethnically diverse families, parents who over 3 years increased their supportive behaviors (eg, role modeling, logistic behaviors) for their child's PA had children who significantly increased their MVPA and decreased sedentary activity over 3 years. Although the absolute change in child PA and sedentary behaviors was small from an individual-level or clinical perspective, the magnitude of change is important from a population-level perspective.62,63 In addition, children of parents with higher supportive PA behaviors at baseline significantly decreased their television/small screen use time over 3 years. Parents' own MVPA and light PA at baseline significantly positively predicted average levels over 3 years of their child's MVPA and light PA, respectively. These results are consistent with the 2 available longitudinal studies that showed that parent supportive behaviors were associated with either an increase or less decrease in child PA over time.49,50 Parent perceptions of neighborhood safety were not significantly associated with changes in child PA over 3 years. Interestingly, neighborhood-level variables captured by the COI, such as poverty, educational level, crime, walkability, or presence of parks or food retail outlets, were not significantly associated with changes in child PA over 3 years in models that included parent- and home-level variables.
These results suggest that modifiable parent behaviors that support child PA can significantly improve child PA levels over time. Regardless of certain types of neighborhood features or resources, low-income parents can play an effective role in increasing their child's PA levels over time. Encouraging their child to play and be active, engaging in PA with their child, taking their child to places to be physically active, and praising their child for being physically active are behaviors parents can engage in to support their child's PA. Parent concerns about neighborhood crime and traffic safety and objective social, physical, and economic neighborhood characteristics seem to be less significant barriers to child increases in PA in the context of positive supportive parenting behaviors for child PA. The children in the present study were pre-school-age, and so the parents may have greater influence and control over when, where, and how their child engages in PA and play, compared with parents of school-age children. The Minneapolis metropolitan area has many local parks and green spaces, and most parents reported feeling safe in their neighborhoods. Thus, the present findings may not hold for parents who live in neighborhoods they perceive as unsafe.
Research and theories related to health equity have identified a wide range of social, economic, and physical environmental variables that affect health outcomes. The COI can be viewed as a broad neighborhood environmental measure of the constructs related to health equity, and it includes social, educational, and health-related constructs. The subscale composites represent distal environmental influences on health outcomes, compared with similar variables measured at the individual household level. For example, the social and economic opportunity subscale indicator variables include the neighborhood percentage of people with incomes below poverty. The neighborhood poverty level and the individual household income variable each may have independent associations with child health behaviors like PA. However, a child's individual household income is a more proximal variable than neighborhood poverty level, and, thus, might be expected to have a stronger influence on child PA behaviors. Most previous research has not included both neighborhood-level and individual-household-level measures of similar constructs, so often it has not been possible to simultaneously evaluate the effects of distal and proximal variables.
For the present analysis, it was recognized that the neighborhood environment is an important determinant of health outcomes. The COI represented an available, multidimensional measure of the wide-ranging factors at the neighborhood level that might be important to examine in relationship to child health behavior outcomes. We had no a priori hypothesis about which specific social determinants of health constructs might predict changes in child health behaviors, over and above similar variables that were measured at the individual household level. Therefore, we chose to use the composite COI a priori to be consistent with the existing research literature and because few data were available to guide an a priori selection of social determinants constructs in relation to child PA. In addition, we had parent reported perceptions of the neighborhood built environment and parent reported frequency of use with their child of parks near their home.
The present study had several strengths and some limitations. Strengths included a diverse, low-income sample with a high retention rate over 3 years, accelerometry PA measures in children and their parent, several measures of different parent supportive behaviors, and both perceived and objective aspects of the neighborhood environment. The multilevel nature of the data and the questions addressed is also a strength. Limitations include lack of specific data on seasonality and use of the built environment, and community-based PA resources. The study was conducted in a geographic location that experiences extremely cold and long winter weather. Families were enrolled in the study for 3 years, and, thus, all seasons were captured regarding the key predictor and outcome variables. However, because of the severe winter weather, it would be desirable to examine the variability in levels and types of parent supportive behaviors and use of the community PA resources across different seasons. The COI measure of the neighborhood environment has strengths and limitations, and the research on the more distal social determinants of child PA warrants exploration with both broad measures such as the COI and with neighborhood measures that are more specific to child PA. Another limitation of the study that is shared by many studies in the behavioral sciences is the use of a Likert-scale metric for the PSB score. PSB is measured using categorical response options and it is unclear how much change an increase or decrease in one unit represents. Therefore, it is difficult to quantify the amount of change in PSB that produces a given number of minutes of change in child MVPA or sedentary behavior. This limitation is inherent in measures that use Likert-type response options to capture the frequency of self-reported behaviors.
Parents who increase their supportive behaviors for their child's PA have children who are more physically active and less sedentary over time. Community-based interventions to increase preschool-age children's PA may enhance their effectiveness by targeting parents' supportive behaviors for their child's PA.
Footnotes
Supported by award U01HD068990, with additional support from R21 HL144559-01 and other members of Childhood Obesity Prevention and Treatment Research Consortium (awards U01HL103622, U01HL103629, U01HL103620, U01HL103561) from the National Heart, Lung, and Blood Institute; the Eunice Kennedy Shriver National Institute of Child Health and Human Development; and the Office of Behavioral and Social Sciences Research, National Institutes of Health. The authors declare no conflicts of interest.
References
- 1.Ekelund U., Luan J., Sherar L.B., Eslinger D.W., Griew P., Cooper A. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307:704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steele R.M., Brage S., Corder K., Wareham N.J., Ekelund U. Physical activity, cardiorespiratory fitness, and the metabolic syndrome in youth. J Appl Physiol. 2008;105:342–351. doi: 10.1152/japplphysiol.00072.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sardinha L.B., Andersen L.B., Anderssen S.A., Quiterio A.L., Ornelas R., Froberg K., et al. Objectively measured time spent sedentary is associated with insulin resistance independent of overall and central body fat in 9-to 10-year-old Portuguese children. Diabetes Care. 2008;31:569–575. doi: 10.2337/dc07-1286. [DOI] [PubMed] [Google Scholar]
- 4.Stamatakis E., Coombs N., Tiling K., Mattocks C., Cooper A., Hardy L.L., et al. Sedentary time in late childhood and cardiometabolic risk in adolescence. Pediatrics. 2015;135:e1432–e1441. doi: 10.1542/peds.2014-3750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Council on Sports Medicine and Fitness, Council on School Health Active healthy living: prevention of childhood obesity through increased physical activity. Pediatrics. 2006;117:1834–1842. doi: 10.1542/peds.2006-0472. [DOI] [PubMed] [Google Scholar]
- 6.Janssen I., Leblanc A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brambilla P., Pozzobon G., Pietrobelli A. Physical activity as the main therapeutic tool for metabolic syndrome in childhood. Int J Obes (Lond) 2011;35:16–28. doi: 10.1038/ijo.2010.255. [DOI] [PubMed] [Google Scholar]
- 8.Troiano R.P., Berrigan D., Dodd K.W., Masse L.C., Tilert T., McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 9.National Academies of Sciences Engineering, and Medicine. A Roadmap to Reducing Child Poverty. Washington, DC: The National Academies Press; 2019. https://www.nap.edu/catalog/25246/a-roadmap-to-reducing-child-poverty [PubMed]
- 10.Schreier H.M.C., Chen E. Socioeconomic status and the health of youth: a multilevel, multidomain approach to conceptualizing pathways. Psychol Bull. 2013;139:606–654. doi: 10.1037/a0029416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(Suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- 12.Nader P.R., Bradley R.H., Houts R.M., McRitchie S.L., O'Brien M. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA. 2008;300:295–305. doi: 10.1001/jama.300.3.295. [DOI] [PubMed] [Google Scholar]
- 13.Pate R.R., O'Neill J.R., Brown W.H., Pfeiffer K.A., Dowda M., Addy C.L. Prevalence of compliance with a new physical activity guideline for preschool-age children. Childhood Obes. 2015;11:415–420. doi: 10.1089/chi.2014.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson S.E., Economos C.D., Must A. Active play and screen time in US children aged 4 to 11 years in relation to sociodemographic and weight status characteristics: a nationally representative cross-sectional analysis. BMC Public Health. 2008;8:366. doi: 10.1186/1471-2458-8-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belcher B.R., Berrigan D., Dodd K.W., Emken B.A., Chou C.P., Spruijt-Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Med Sci Sports Exerc. 2010;42:2211–2221. doi: 10.1249/MSS.0b013e3181e1fba9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beets M.W., Bornstein D., Dowda M., Pate R.R. Compliance with national guidelines for physical activity in US preschoolers: measurement and interpretation. Pediatrics. 2011;127:658–664. doi: 10.1542/peds.2010-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Francis S.L., Morrissey J.L., Letuchy E.M., Levy S.M., Janz K.F. Ten-year objective physical activity tracking: Iowa Bone Development Study. Med Sci Sports Exerc. 2013;45:1508–1514. doi: 10.1249/MSS.0b013e31828b2f3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keyes K.M., Galea S. Setting the agenda for a new discipline: population health science. Am J Public Health. 2016;106:633–634. doi: 10.2105/AJPH.2016.303101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaplan G.A., Everson S.A., Lynch J.W. In: Promoting health: intervention strategies from social and behavioral research. Smedley B., Syme S.L., editors. The National Academies Press; Washington, DC: 2000. The contribution of social and behavioral research to an understanding of the distribution of disease: a multilevel approach; pp. 31–55. [Google Scholar]
- 20.Committee on Capitalizing on Social Science and Behavioral Research to Improve the Public's Health. Promoting health: intervention strategies from social and behavioral research. Smedley B., Syme S., editors. Am J Health Promot. 2001;15:149–166. doi: 10.4278/0890-1171-15.3.149. [DOI] [PubMed] [Google Scholar]
- 21.Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol. 1992;47:6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 22.Gordon-Larsen P., Nelson M.C., Page P., Popkin B.M. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 23.Glass T.A., McAtee M.J. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62:1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 24.Suglia S.F., Shelton R.C., Hsiao A., Wang Y.C., Rundle A., Link B.G. Why the neighborhood social environment is critical in obesity prevention. J Urban Health. 2016;93:206–212. doi: 10.1007/s11524-015-0017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evenson K.R., Sotres-Alvarez D., Herring A.H., Messer L., Laraia B.A., Rodriguez D.A. Assessing urban and rural neighborhood characteristics using audit and GIS data: derivation and reliability of constructs. IJBNPA. 2009;6:44. doi: 10.1186/1479-5868-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giles-Corti B., Donovan R.J. The relative influence of individual, social and physical environment determinants of physical activity. Soc Sci Med. 2002;54:1793–1812. doi: 10.1016/s0277-9536(01)00150-2. [DOI] [PubMed] [Google Scholar]
- 27.Bedimo-Rung A.L., Mowen A.J., Cohen D.A. The significance of parks to physical activity and public health: a conceptual model. Am J Prev Med. 2005;28(2 Suppl 2):159–168. doi: 10.1016/j.amepre.2004.10.024. [DOI] [PubMed] [Google Scholar]
- 28.Sugiyama T., Leslie E., Giles-Corti B., Owen N. Physical activity for recreation or exercise on neighborhood streets: associations with perceived environmental attributes. Health Place. 2009;15:1058–1063. doi: 10.1016/j.healthplace.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Davison K.K., Lawson C.T. Do attributes in the physical environment influence children's physical activity? A review of the literature. Int J Behav Nutr Phys Act. 2006;3:19. doi: 10.1186/1479-5868-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cradock A.L., Kawachi I., Colditz G.A., Hannon C., Melly S.J., Wiecha J.L., et al. Playground safety and access in Boston neighborhoods. Am J Prev Med. 2005;28:357–363. doi: 10.1016/j.amepre.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 31.Zhu X., Lee C. Walkability and safety around elementary schools economic and ethnic disparities. Am J Prev Med. 2008;34:282–290. doi: 10.1016/j.amepre.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 32.Acevedo-Garcia D., McArdle N., Hardy E.F., Crisan U.I., Romano B., Norris D., et al. The child opportunity index: improving collaboration between community development and public health. Health Affairs. 2014;33:1948–1957. doi: 10.1377/hlthaff.2014.0679. [DOI] [PubMed] [Google Scholar]
- 33.Roubinov D.S., Hagan M.J., Boyce W.T., Adler N.E., Bush N.R. Family Socioeconomic status, cortisol, and physical health in early childhood: the role of advantageous neighborhood characteristics. Psychosom Med. 2018;80:492–501. doi: 10.1097/PSY.0000000000000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kersten E.E., Adler N.E., Gottlieb L., Jutte D.P., Robinson S., Roundfield K., et al. Neighborhood child opportunity and individual-level pediatric acute care use and diagnoses. Pediatrics. 2018;141:e20172309. doi: 10.1542/peds.2017-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Veitch J., Salmon J., Ball K. Individual, social and physical environmental correlates of children's active free-play: a cross-sectional study. Int J Behav Nutr Phys Act. 2010;7:11. doi: 10.1186/1479-5868-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.French S.A., Sherwood N.E., Mitchell N.R., Fan Y. Park use is associated with less sedentary time among low-income parents and their pre-school child: the NET-Works study. Prev Med Rep. 2017;5:7–12. doi: 10.1016/j.pmedr.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hinkley T., Crawford D., Salmon J., Okely A.D., Hesketh K. Preschool children and physical activity: a review of correlates. Am J Prev Med. 2008;34:435–441. doi: 10.1016/j.amepre.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 38.Sallis J.F., Nader P.R., Broyles S.L., Berry C.C., Elder J.P., McKenzie T.L., et al. Correlates of physical activity at home in Mexican-American and Anglo-American preschool children. Health Psychol. 1993;12:390–398. doi: 10.1037//0278-6133.12.5.390. [DOI] [PubMed] [Google Scholar]
- 39.Sallis J.F., Prochaska J.J., Taylor W.C. A review of correlates of physical activity in children and adolescents. Med Sci Sports Exerc. 2000;32:963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 40.Loprinzi P.D., Trost S.G. Parental influences on physical activity behavior in preschool children. Prev Med. 2012;50:129–133. doi: 10.1016/j.ypmed.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 41.Fan Y., Chen Q. Family functioning as a mediator between neighborhood conditions and children's health: evidence from a national survey in the United States. Soc Sci Med. 2012;74:1939–1947. doi: 10.1016/j.socscimed.2012.01.039. [DOI] [PubMed] [Google Scholar]
- 42.Hamilton K., White K. Identifying parents' perceptions about physical activity: a qualitative exploration of salient behavioural, normative and control beliefs among mothers and fathers of young children. J Health Psychol. 2010;15:1157–1169. doi: 10.1177/1359105310364176. [DOI] [PubMed] [Google Scholar]
- 43.Trost S.G., Sallis J.F., Pate R.R., Freedson P.S., Taylor W.C., Dowda M. Evaluating a model of parental influence on youth physical activity. Am J Prev Med. 2003;25:277–282. doi: 10.1016/s0749-3797(03)00217-4. [DOI] [PubMed] [Google Scholar]
- 44.Fan Y., French S.A., Das K.V. Family structure and park use among parents. Am J Prev Med. 2012;43:520–526. doi: 10.1016/j.amepre.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 45.Barkin S., Banda J.A., Buchowski M.S., Stevens J., Bangdiwala S., Evenson K., et al. Parent's physical activity associated with preschooler activity in underserved populations. Am J Prev Med. 2017;52:424–432. doi: 10.1016/j.amepre.2016.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fuemmeler B.F., Anderson C.B., Masse L.C. Parent-child relationship of directly measured physical activity. Int J Behav Nutr Phys Act. 2011;8:17. doi: 10.1186/1479-5868-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dunton G.F., Liao Y., Almanza E., Jerrett M., Spruijt-Metz D., Pentz M.A. Locations of joint physical activity in parent-child pairs based on accelerometer and GPS monitoring. Ann Behav Med. 2013;45(Suppl 1):S162–S172. doi: 10.1007/s12160-012-9417-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Datar A., Nicosia N., Shier V. 2013. Parent perceptions of neighborhood safety and children's physical activity, sedentary behavior, and obesity: evidence from a national longitudinal study. Am J Epidemiol. 2013;177:1065–1073. doi: 10.1093/aje/kws353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crawford D., Cleland V., Timperio A., Salmon J., Andrianopoulos N., Roberts R., et al. The longitudinal influence of home and neighborhood environments on children's body mass index and physical activity over 5 years: the CLAN study. Int J Obesity. 2010;34:1177–1187. doi: 10.1038/ijo.2010.57. [DOI] [PubMed] [Google Scholar]
- 50.Davison K.K., Jago R. Change in parent and peer support across ages 9 to 15 years and adolescent girls' PA. Med Sci Sports Exerc. 2009;41:1816–1825. doi: 10.1249/MSS.0b013e3181a278e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.French S.A., Sherwood N.E., Veblen-Mortenson S., Crain A.L., JaKa M.M., Mitchell N.R., et al. NET-Works randomized clinical trial: results of a three year childhood obesity prevention intervention for preschool-aged children. Am J Public Health. 2018;108:1695–1706. doi: 10.2105/AJPH.2018.304696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dunton G.F., Liao Y., Almanza E., Jerrett M., Spruitz-Metz D., Chou C-P., et al. Joint physical activity and sedentary behavior in parent-child pairs. Med Sci Sports Exerc. 2012;44:1473–1480. doi: 10.1249/MSS.0b013e31825148e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sallis J.F., Wendell C.T., Dowda M., Freedson P.S., Pate R.R. Correlates of vigorous physical activity for children in grades 1 through 12: comparing parent-reported and objectively measured physical activity. Pediatr Exerc Sci. 2002;14:30–44. [Google Scholar]
- 54.Taylor W.C., Sallis J.F., Dowda M., Freedson P.S., Eason K., Pate R.R. Activity patterns and correlates among youth: differences by weight status. Pediatr Exerc Sci. 2002;14:418–431. [Google Scholar]
- 55.Toschke J.A., von Kries R., Rosenfeld E., Toschke A.M. Reliability of physical activity measures from accelerometry among preschoolers in free-living conditions. Clin Nutr. 2007;26:416–420. doi: 10.1016/j.clnu.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 56.Van Cauwenberghe E., Gubbels J., De Bourdeaudhuij I., Cardon G. Feasibility and validity of accelerometer measurements to assess physical activity in toddlers. Int J Behav Nutr Phys Act. 2011;8:67. doi: 10.1186/1479-5868-8-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cliff D.P., Reilly J.J., Okely A.D. Methodological considerations in using accelerometers to assess habitual physical activity in children ages 0-5 years. J Sci Med Sport. 2009;12:557–567. doi: 10.1016/j.jsams.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 58.Hislop J.F., Bulley C., Mercer T.H., Reilly J.J. Comparison of accelerometry cut points for physical activity and sedentary behavior in preschool children: a validation study. Pediatr Exerc Sci. 2012;24:563–576. doi: 10.1123/pes.24.4.563. [DOI] [PubMed] [Google Scholar]
- 59.Pate R.R., Pfeiffer K.A., Trost S.G., Ziegler P., Dowda M. Physical activity among children attending preschools. Pediatrics. 2004;114:1258–1263. doi: 10.1542/peds.2003-1088-L. [DOI] [PubMed] [Google Scholar]
- 60.Matthew C.E. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37(11 Suppl):S512–S522. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 61.Jamshidian M., Jalal S., Jansen C. MissMech: an R Package for Testing Homoscedasticity, Multivariate Normality, and Missing Completely at Random (MCAR) J Stat Software. 2014;56:1–31. [Google Scholar]
- 62.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 63.Jeffery R.W. Risk behaviors and health: contrasting individual and population perspectives. American Psychologist. 1989;44:1194–1202. doi: 10.1037//0003-066x.44.9.1194. [DOI] [PubMed] [Google Scholar]