Abstract
Background
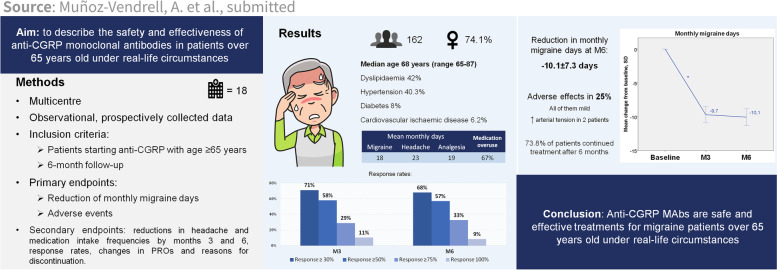
Anti-CGRP monoclonal antibodies have shown notable effectiveness and tolerability in migraine patients; however, data on their use in elderly patients is still lacking, as clinical trials have implicit age restrictions and real-world evidence is scarce. In this study, we aimed to describe the safety and effectiveness of erenumab, galcanezumab and fremanezumab in migraine patients over 65 years old in real-life.
Methods
In this observational real-life study, a retrospective analysis of prospectively collected data from 18 different headache units in Spain was performed. Migraine patients who started treatment with any anti-CGRP monoclonal antibody after the age of 65 years were included. Primary endpoints were reduction in monthly migraine days after 6 months of treatment and the presence of adverse effects. Secondary endpoints were reductions in headache and medication intake frequencies by months 3 and 6, response rates, changes in patient-reported outcomes and reasons for discontinuation. As a subanalysis, reduction in monthly migraine days and proportion of adverse effects were also compared among the three monoclonal antibodies.
Results
A total of 162 patients were included, median age 68 years (range 65–87), 74.1% women. 42% had dyslipidaemia, 40.3% hypertension, 8% diabetes, and 6.2% previous cardiovascular ischaemic disease. The reduction in monthly migraine days at month 6 was 10.1 ± 7.3 days. A total of 25.3% of patients presented adverse effects, all of them mild, with only two cases of blood pressure increase. Headache and medication intake frequencies were significantly reduced, and patient-reported outcomes were improved. The proportions of responders were 68%, 57%, 33% and 9% for reductions in monthly migraine days ≥ 30%, ≥ 50%, ≥ 75% and 100%, respectively. A total of 72.8% of patients continued with the treatment after 6 months. The reduction in migraine days was similar for the different anti-CGRP treatments, but fewer adverse effects were detected with fremanezumab (7.7%).
Conclusions
Anti-CGRP mAbs are safe and effective treatments in migraine patients over 65 years old in real-life clinical practice.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s10194-023-01585-2.
Keywords: Calcitonin gene-related peptide, Monoclonal antibodies, Migraine, 65 years old, Real-world
Introduction
Monoclonal antibodies (mAbs) targeting calcitonin gene-related peptide (CGRP) or its receptor have undeniably led to a new era for the treatment of migraine, given their generally fast and sustained effect and high responder rates [1]. The tolerability and safety of these treatments have been proven in diverse studies [2–4]. For this reason, its prescription in clinical practice is wide, although restricted in patients with previous cardiovascular or cerebral ischaemic events. However, data on anti-CGRP mAb use in elderly patients are still lacking, as clinical trials have implicit age restrictions and real-world evidence are still scarce.
Phase-3 trials of all four anti-CGRP mAbs included patients from 18 to 65 years old, with some exceptions. Both HALO studies [5, 6] and the FOCUS trial [7] with fremanezumab included patients up to 70 years old, and the PROMISE-1 trial [8] with eptinezumab included patients up to 75 years old. Post hoc analyses of these studies showed comparable treatment efficacy and safety in patients over 50 [9] and 60 years old [10]. The CONQUER trial with galcanezumab also included 29 patients from 65 to 75 years old (13 of them were enrolled in galcanezumab), with no meaningful differences in their clinical outcomes [11]. Nonetheless, clinical trials excluded patients with certain comorbidities (including cardiovascular risk factors or psychiatric disorders) and clinical characteristics (such as the presence of daily headache or medication overuse), thus raising the need for real-life studies to confirm similar results in other subsets of patients.
A recent study compared the effectiveness and safety of erenumab in real-life in patients over and under 65 years old, with similar reported outcomes, but was limited to a small sample of 15 patients per group [12].
In the present study, we aimed to evaluate the effectiveness and safety of anti-CGRP mAbs in migraine patients over 65 years old in a real-life multicentric cohort in Spain.
Methods
Patients
In this observational retrospective study of prospectively collected data from 18 different Spanish headache centres, we included consecutive patients starting any of the three commercialized anti-CGRP mAbs (erenumab, galcanezumab or fremanezumab) from December 2019 to June 2022 with the diagnosis of migraine according to ICHD-3 criteria [13] and who were over 65 years old by the date of initiation. According to the required criteria by the Spanish government for anti-CGRP mAb funded prescription, all recruited patients presented more than 8 monthly migraine days, with failure of at least 3 migraine preventive medications, including onabotulinum toxin A (BTX-A) for chronic migraine [14].
Anti-CGRP mAbs were administered monthly (erenumab 70 or 140 mg, galcanezumab 120 mg + 240 mg for the loading dose, or fremanezumab 225 mg) or quarterly (fremanezumab 675 mg) by subcutaneous injection. Each treatment was decided based upon individual patient characteristics at the discretion of the attending physician, as well as the association of concomitant oral preventive treatments or BTX-A.
Outcome measures
All clinical data were prospectively collected at each centre from the moment of anti-CGRP initiation, with quarterly scheduled visits and a minimum follow-up of 6 months. The presence of comorbidities at baseline was retrospectively extracted from clinical records. The following variables were collected: age, sex, time since migraine diagnosis, episodic or chronic migraine and time since chronification, presence of aura, previous migraine preventive treatments, concomitance of oral preventive treatments or BTX-A injections and presence of comorbidities (cardiovascular risk factors, peripheral artery disease, cerebrovascular or cardiac ischaemic disease, obstructive sleep apnoea, chronic obstructive pulmonary disease, liver disease, nephropathy, psychiatric disorders or others). Clinical variables that were collected quarterly included the following: monthly migraine days (MMD), monthly headache days (MHD), frequency of monthly headache days by maximum intensity of pain (in a 4-point scale: none, mild, moderate or severe), monthly acute medication intake (MAMI), Headache Impact Test (HIT-6), Migraine Disability Assessment test (MIDAS), Patients’ Global Impression of Change (PGIC) scale (except in the baseline visit), presence of adverse effects and treatment discontinuation reasons. Headache parameters (MMD, MHD, MAMI and headache days by maximum intensity) were collected with standardized paper or electronic headache diaries brought by the patients on each clinical appointment. A headache day was defined as any calendar day with a documented headache episode. A migraine day was defined as a day with a headache that lasts at least 4 h and meets ICHD-3 criteria for migraine or probable migraine [13]; or a day with a headache that is successfully treated with a triptan, ergotamine, or other migraine-specific acute medication.
The primary endpoints included the reduction in MMD after 6 months of treatment and the presence of adverse effects. The secondary endpoints included the reduction in MMD after 3 months, the reduction in MHD and MAMI after 3 and 6 months, the change in frequency of days by intensity, the 30%, 50%, 75% and 100% response rates, changes in the HIT-6, MIDAS and PGIC scale scores, and the reasons for treatment discontinuation during the 6-month follow-up (due to inefficacy or adverse events). As a subanalysis of the cohort, the reduction in monthly migraine days and the proportion of adverse effects were also compared among the three monoclonal antibodies and between patients with and without concomitant oral treatment, concomitant BTX treatment and medication overuse at baseline.
Statistical analysis
Primary and secondary endpoints were assessed using a descriptive analysis. Categorical variables were presented as absolute frequencies. Demographic and clinical variables were presented as medians and ranges or means and standard deviations according to the distribution. The normality of the distribution of each variable was evaluated with Kolmogorov–Smirnov and Shapiro–Wilk tests. Changes in mean MMD, MHD and MAMI were assessed by paired sample t-test. Differences in MMD and the proportion of adverse effects between the different mAbs were assessed by ANOVA. Differences in MMD and the proportion of adverse effects between patients with and without medication overuse, concomitant oral treatment and concomitant BTX-A treatment were assessed by chi square test or independent sample t-test as appropriate. A sensitivity analysis using the “last observation carried forward” technique was performed for quantitative endpoints at month 6, as some patients discontinued treatment after month 3.
The results of all the statistical analyses were interpreted with confidence intervals of 95% and a significance level of 5%. Statistical analyses were performed in SPSS v.20 (SPSS Inc., Chicago, USA). No statistical power calculation was conducted prior to the study. The sample size was based on the available data from the participating centres.
Ethics approval and consent to participate
The study was approved by the Ethical Committee of the coordinating centre with reference EOM030/22. The confidential information of the patients was handled in accordance with Spanish regulations.
Results
A total of 162 patients were included. Of these, 28 were lost to follow-up after discontinuing treatment at month 3 due to inefficacy or intolerance (these patients were not included in the analysis of frequency variables at month 6 but were included as non-responders in the global analysis at month 6; a sensitivity analysis of these frequency variables by “last observation carried forward” was performed to validate these results, see Appendix 1).
The median age was 68 years (range 65–87), and 74.1% of the patients were women. A total of 80.9% had chronic migraine, and 13% had aura. The median migraine onset age was 18 (IQR 14–26.5), and the time since chronification in cases of chronic migraine was 120 months (IQR 24.8–185). The patients’ comorbidities are detailed in Table 1. Previous and concomitant treatments are detailed in Table 2. At baseline, 37 patients (22.9%) were taking more than one oral concomitant treatment. A total of 23.5% of patients were treated with erenumab, 52.5% with galcanezumab, and 24.1% with fremanezumab (29 [17.9%] with monthly dose, and 10 [6.2%] with quarterly dose).
Table 1.
Patients’ reported comorbidities at baseline
| Comorbidity | n (%) |
|---|---|
| Dyslipidaemia | 68 (42.0) |
| Hypertension | 70 (40.3) |
| Anxiety | 53 (32.7) |
| Depression | 53 (32.7) |
| Fibromyalgia | 16 (9.9) |
| Smoking | 15 (9.3) |
| Diabetes | 13 (8.0) |
| Obstructive sleep apnoea | 12 (7.4) |
| Hypothyroidism | 11 (6.8) |
| Tumours | 10 (6.2) |
| Chronic obstructive pulmonary disease | 7 (4.3) |
| Peripheral artery disease | 5 (3.1) |
| Liver disease | 5 (3.1) |
| Nephropathy | 5 (3.1) |
| Cardiac ischaemic disease | 4 (2.5) |
| Cerebral ischaemic disease | 1 (0.6) |
| Others | 31 (19.1) |
Table 2.
Previous and concomitant preventive treatments at baseline
| Medication | Previous [n (%)] | Concomitant [n (%)] |
|---|---|---|
| Topiramate | 138 (85.2) | 12 (7.4) |
| Beta-blocker | 117 (72.2) | 33 (20.4) |
| Amitriptyline | 140 (86.4) | 25 (15.4) |
| Flunarizine | 100 (61.7) | 1 (0.6) |
| Anti-hypertensive | 69 (42.6) | 36 (22.2) |
| Onabotulinum toxin A | 141 (87.0) | 31 (19.1) |
| Others | 103 (63.6) | 44 (27.2) |
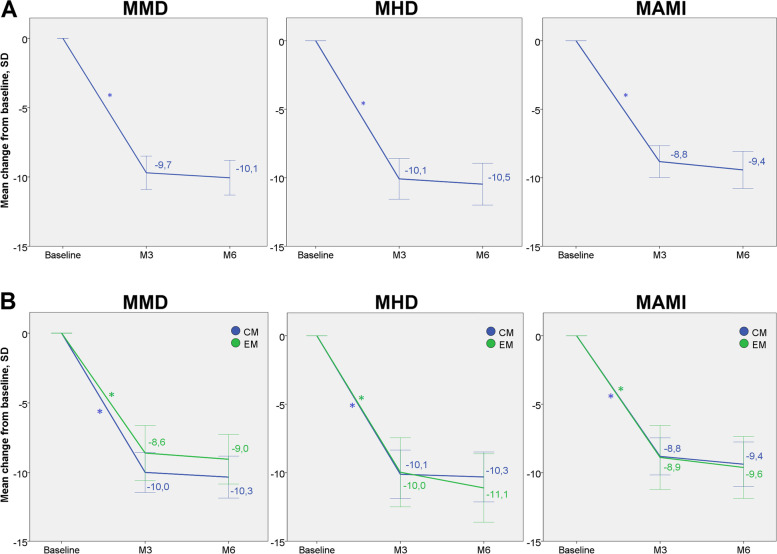
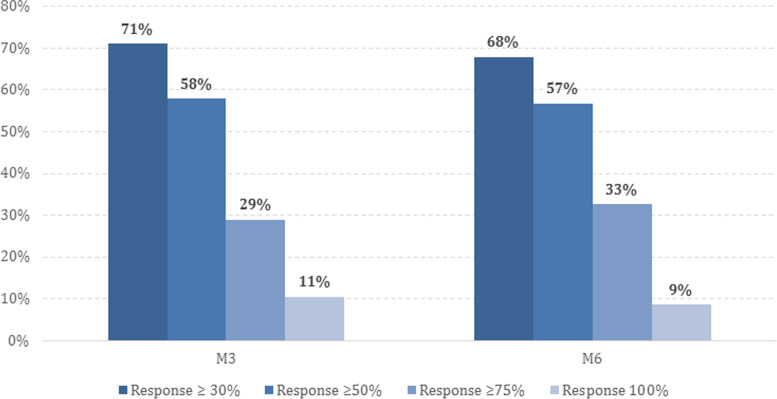
Clinical characteristics at baseline and during the follow-up are detailed in Table 3. The reduction in MMD at 6 months was -10.1 ± 7.3 days (p = 0.0001). Forty-one patients (25.3%) presented adverse effects at some point during the follow-up, which are detailed in Table 4. The reduction in MMD after 3 months and the reduction in MHD and MAMI after 3 and 6 months were also significant (see Fig. 1). The proportion of responders is shown in Fig. 2. After clinical evaluation at month 6, 118 patients (72.8%) continued with the treatment and 44 patients (27.2%) discontinued, 36 (22%) due to inefficacy and 8 (4.9%) due to adverse effects. Treatment was discontinued in 28 patients (17.3%) at month 3 (20 due to inefficacy and 8 due to adverse effects: 1 injection site reaction, 1 incident of hypertension, 1 incident of migraine worsening, 1 incident of hypotension, 1 incident of transient facial erythema, 1 incident of general discomfort, 1 incident of unsteadiness and 1 incident of dizziness) and in 16 patients (9.9%) at month 6 (all due to inefficacy). At month 3, patients who discontinued anti-CGRP MAbs were taking erenumab in 4 cases (all due to inefficacy), galcanezumab in 19 (13 due to inefficacy, 6 due to adverse effects), and fremanezumab in 5 (3 due to inefficacy, 2 due to adverse effects). At month 6, patients who discontinued treatment were taking erenumab in 7 cases, galcanezumab in 7, and fremanezumab in 2 (all due to inefficacy).
Table 3.
Clinical characteristics at baseline, at month 3 (M3) and at month 6 (M6)
| Baseline | M3 | M6 | |
|---|---|---|---|
| N | 162 | 162 | 134 |
| MMD [mean ± SD] | 18.0 ± 7.5 | 9.8 ± 9.0 | 7.3 ± 7.6 |
| MHD [mean ± SD] | 23.3 ± 6.9 | 15.0 ± 10.5 | 12.5 ± 10.0 |
| Intensities [mean ± SD] | n = 113/162 | n = 114/162 | n = 96/134 |
| Mild days/month | 4.3 ± 6.3 | 6.1 ± 8.4 | 6.0 ± 8.4 |
| Moderate days/month | 8.3 ± 7.5 | 4.9 ± 6.2 | 3.4 ± 4.3 |
| Severe days/month | 9.3 ± 8.1 | 2.9 ± 5.4 | 2.2 ± 4.1 |
| MAMI [mean ± SD] |
18.9 ± 8.0 n = 153/162 |
11.1 ± 9.3 n = 147/162 |
9.4 ± 8.9 n = 129/134 |
| Medication overuse [n (%)] | 107 (66.5) | 57 (35.2) | 37 (27.8) |
| HIT-6 [mean ± SD] |
65.9 ± 7.8 n = 141/162 |
57.1 ± 11.9 n = 135/162 |
55.2 ± 11.1 n = 114/134 |
| MIDAS [mean ± SD] |
80.3 ± 71.3 n = 129/162 |
45.2 ± 62.0 n = 121/162 |
34.4 ± 48.1 n = 101/134 |
| PGIC [mean ± SD] | - |
3.78 ± 2.0 n = 130/162 |
4.13 ± 2.1 n = 110/134 |
| Concomitant oral treatment [n (%)] | 102 (63.0) | 89 (55.3) | 64 (47.8) |
| Concomitant onabotulinum toxin A [n (%)] | 31 (19.1) | 25 (15.5) | 18 (13.4) |
MMD monthly migraine days, SD standard deviation, MHD monthly headache days, MAMI monthly acute medication intake
Missing data is shown below each variable
Table 4.
Adverse effects during the follow-up
| Adverse effect [n (%)] | M3 (n = 162) | M6 (n = 134) |
|---|---|---|
| Any | 33 (20.4) | 19 (14.2) |
| Constipation | 16 (9.9) | 16 (9.9) |
| Injection site reaction | 6 (3.7) | 1 (0.6) |
| Dizziness | 3 (1.8) | 1 (0.6) |
| Hypertension | 2 (1.2) | 0 |
| General discomfort | 2 (1.2) | 1 (0.6) |
| Unsteadiness | 1 (0.6) | 0 |
| Hypotension | 1 (0.6) | 0 |
| Headache worsening | 1 (0.6) | 0 |
| Transient facial erythema | 1 (0.6) | 0 |
Fig. 1.
Change in MMD, MHD and MAMI after 3 (M3) and 6 months (M6). A Global mean changes in the entire cohort. B Mean changes by diagnosis at baseline: chronic migraine (CM) or episodic migraine (EM). *p < 0.001. Confidence intervals of 95%. MMD = monthly migraine days; MHD = monthly headache days; MAMI = monthly acute medication intake; SD = standard deviation, M3 = month 3; M6 = month 6; CM = chronic migraine; EM = episodic migraine
Fig. 2.
Proportion of ≥ 30%, ≥ 50%, ≥ 75% and 100% responders after 3 (M3) and 6 months (M6). M3 = month 3; M6 = month 6
Baseline characteristics and the reduction in MMD at month 6 were similar for the three different anti-CGRP mAbs, but the proportion of adverse effects was significantly lower for fremanezumab (see Table 5). Constipation was more frequent for erenumab (54.5% versus 40.9% for galcanezumab and 4.5% for fremanezumab), and injection site reaction was observed only in 7 patients who were given galcanezumab.
Table 5.
Baseline characteristics and effectiveness and safety outcomes between different anti-CGRP mAbs
| Erenumab | Galcanezumab | Fremanezumab | p | |
|---|---|---|---|---|
| n | 38 | 85 | 39 | |
| Baseline differences | ||||
| Age [mean ± SD] | 69.8 ± 5.0 | 69.8 ± 4.4 | 68.8 ± 3.7 | 0.485 |
| Proportion of chronic migraine [n (%)] | 29 (76.3) | 70 (82.4) | 32 (82.1) | 0.721 |
| MMD [mean ± SD] | 19.5 ± 7.9 | 17.6 ± 7.2 | 17.2 ± 7.7 | 0.365 |
| MHD [mean ± SD] | 22.8 ± 7.1 | 22.7 ± 7.1 | 24.9 ± 6.1 | 0.228 |
| Medication overuse [n (%)] | 27 (71.1) | 56 (65.9) | 24 (63.2) | 0.760 |
| MIDAS [mean ± SD] |
73.3 ± 66 n = 33/38 |
89.5 ± 79 n = 68/85 |
66.2 ± 54.7 n = 28/39 |
0.284 |
| Concomitant onabotulinum toxin A [n (%)] | 5 (13.2) | 20 (23.5) | 6 (15.4) | 0.322 |
| Primary endpoints | ||||
| MMD reduction at M6 [mean ± SD] |
-9.9 ± 8.2 n = 34/38 |
-10.4 ± 7.3 n = 66/85 |
-9.6 ± 6.5 n = 34/39 |
0.890 |
| Total adverse effects [n (%)] | 15 (39.5) | 23 (27.1) | 3 (7.7) | 0.005 |
MMD monthly migraine days, M6 month 6, SD standard deviation
Missing data is shown below each variable
The reduction in MMD at M6 was not significantly different between patients with medication overuse at baseline and those without (-10.4 ± 8.2 days vs. -9.4 ± 5.2 days respectively, p = 0.459), nor the proportion of adverse effects (25.2% vs. 24.1% respectively, p = 0.872). Similarly, no difference was observed in the reduction in MMD at M6 between patients with concomitant oral medication at baseline and those without (-9.6 ± 7.5 days vs. -10.8 ± 7.0 days respectively, p = 0.335), and neither in the proportion of adverse effects (27.5% vs. 21.7% respectively p = 0.414). Regarding concomitant BTX-A use at baseline, no difference was observed in reduction in MMD at M6 between patients with and without concomitant BTX-A use (-8.1 ± 5.8 vs. -10.5 ± 7.6 respectively, p = 0.288), nor in the proportion of adverse effects (22.6% vs. 26.0% respectively, p = 0.698).
There were no missing data on MMD, MHD, medication overuse and concomitant treatments. Data on MAMI, monthly headache frequency categorized by intensities, and HIT-6, MIDAS and PGIC scales were not available for all patients; therefore, those patients were not included in the calculation of global means for each of those variables at each visit. Missing data for each variable is shown in Tables 3, 4 and 5. There were no other missing data.
Discussion
The results of this study revealed a significant reduction in headache frequency after 6 months of anti-CGRP mAb treatment in migraine patients over 65 years old (-10.1 ± 7.3 days in MMD and -10.5 ± 8.9 days in MHD), with ≥ 30%, ≥ 50%, ≥ 75% and 100% responder rates at month 6 of 68%, 57%, 33% and 9%, respectively. Patient-reported outcomes were also improved by month 6, including HIT-6 (65.9 ± 7.8 to 55.2 ± 11.1) and MIDAS (80.3 ± 71.3 to 34.4 ± 48.1) scores. These results are similar to previously reported outcomes in the general population in real-life [15–17].
Medication intake was also significantly reduced by month 6 (-9.2 ± 7.6 days in MAMI), with a prominent decrease in medication overuse rates (66.5% at baseline compared to 27.8% at month 6). These findings support the effectiveness of anti-CGRP mAbs in migraine patients with medication overuse, as previously suggested [18, 19]. This point is of special interest in the present cohort of older patients, assuming they are at a higher risk of analgesic medication side effects due to higher comorbidities, including ischaemic events [20].
Oral preventive medications for the treatment of migraine have a high rate of adverse effects, especially in older patients, in whom polypharmacy is frequent and susceptibility to intolerance is higher [21]. Treatment with anti-CGRP mAbs is an excellent alternative, given its minimal risk of interactions [22] and its beneficial effect in reducing the use of oral preventive treatments, as shown in our series (63% of concomitant oral treatment reduced to 47.8% at month 6).
The safety of using anti-CGRP mAbs to treat patients over 65 years old is still uncertain, given that patients included in clinical trials were selected and real-world data are scarce. As expected, the real-life circumstances of our study revealed a high prevalence of comorbidities among the patients, including dyslipidaemia (42%), hypertension (40.3%), anxiety (32.7%), depression (32.7%) and even cardiovascular ischaemic disease (6.2%). Even so, the proportion of reported adverse effects was relatively low after 6 months of treatment (25.3%), without any ischaemic event or other serious complication detected during the follow-up, and comparable to what has been reported in the general population [2–4, 23]. Only 8 patients (4.9%) discontinued anti-CGRP treatment due to adverse effects. These data provide evidence of the safety of using anti-CGRP mAbs in a setting of elderly patients with increased cardiovascular risk factors and comorbidities.
Special mention should be given to 2 patients (1.2%) who presented hypertension after mAb initiation. One of them presented with a transient increase in their diastolic readings without previous arterial hypertension diagnosis after the first dose of galcanezumab, but he did not require any specific treatment and allowed continuation of galcanezumab treatment. The other, who already had a known diagnosis of hypertension, presented with two hypertensive crises on the same day of the first and second administration of monthly fremanezumab; while that patient didn’t suffer target organ damage, she required prompt antihypertensive rescue treatment, thus leading to fremanezumab discontinuation. Consequently, caution should arise when prescribing anti-CGRP in older patients with resistant arterial hypertension, and specific monitoring should be considered.
In the present study, the reduction in MMD was not different between the 3 different anti-CGRP mAbs. However, fewer adverse effects were observed in the fremanezumab group (7.7%) than in the erenumab (39.5%) and galcanezumab (27.1%) groups, limited to only 3 patients who presented with constipation, transient facial erythema and a hypertensive crisis. This finding must be interpreted with caution, as the number of patients per group is relatively low, and for now, published meta-analyses have failed to find consistent differences between anti-CGRP mAbs safety and tolerability [24–26]. A possible explanation for this phenomenon could reside in the fact that a considerable proportion of patients with fremanezumab received quarterly doses, which implies fewer absolute days of subcutaneous administration compared to galcanezumab, and therefore a lower probability of local reaction; and that a slightly different mechanism of action than erenumab (which binds to the CGRP receptor) seems to minimize the incidence of constipation [27]. A higher proportion of patients with galcanezumab were observed in the present cohort, which is probably explained by the exclusive authorization of this MAb in particular in some regions of Spain during the time of the study.
Some limitations must be considered for this study. First, follow-up was limited to 6 months after the first treatment with anti-CGRP mAbs, which can omit patients responding later or after a mAb switch, and those presenting delayed drug adverse events. Second, although all clinical follow-up variables were prospectively collected, the presence of baseline comorbidities was assessed retrospectively, which can lead to biases of information if some conditions were unnoticed or not registered in the clinical records, and the use and dosing of concomitant treatments was poorly controlled. Likewise, missing data in the prospectively collected variables and the loss of follow-up of the patients who discontinued treatment at M3 may reduce the reliability of the results, even with the sensitivity analysis, which only considers missing data due to treatment discontinuation. Finally, when creating different arms to compare outcomes between anti-CGRP treatments, the number of patients per group was relatively low, thus generating low statistical power. Further studies are needed to confirm these findings supporting the effectiveness and safety of anti-CGRP mAb use in older migraine patients.
Conclusion
Anti-CGRP mAbs are safe and effective treatments for migraine patients over 65 years in real-life clinical practice. Treatment with fremanezumab had fewer adverse effects in our cohort. No differences were observed in patients with and without concomitant oral treatment, concomitant BTX treatment and medication overuse at baseline. Further studies are needed in different populations, with larger samples and with a greater inclusion of prospective variables to increase the robustness of our results.
Supplementary Information
Additional file 1: Appendix 1. Sensitivity analysis of quantitative endpoints at month 6.
Acknowledgements
We would like to gratefully recognize the labour of all the collaborating centres involved in this project, and to acknowledge the junior section of the Spanish Society of Neurology's Headache Study Group (GECSEN) for the promotion of the initiative of this study. We also thank all the patients who participated in this study. We thank CERCA Programme / Generalitat de Catalunya for institutional support.
Authors’ contributions
AMV and SC contributed to the collection, analysis and interpretation of the data and to the writing of the manuscript; EC, AA, MTF, CN, MO, JC, JP, JCM, FJMM, AMO, MRS, SSL, MPNP, NM, ALB, LMCS, SMGS, JGU, LRF, AGM, SQ, AEI, SGL, MVCS, VAO, JGA, NBI, RB, SDI and PPR contributed to the collection of the data; and MHV, EC and PPR contributed to the interpretation of the data and to the revision of the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analysed during this study are available from the corresponding author on reasonable request from any qualified investigator.
Declarations
Competing interests
AMV, SC, JC and JP have received honoraria from Teva, Lilly, Roche, UCB, Bial, Chiesi, Allergan, Esai, Zambon, Kern Pharma, Pfizer, Biogen Idec, Novartis, TEVA, Merck, Janssen, Neuraxpharm, Genzyme, Sanofi, Bayer, Almirall and/or Celgene.
EC has received honoraria from Novartis, Chiesi, Lundbeck, Medscape. He is junior editor for Cephalalgia.
Marta Torres-Ferrus has received honoraria as a consultant or speaker for Allergan-Abbvie, Almirall, Chiesi, Eli Lilly, Novartis, and Teva.
Alicia Alpuente has received honoraria as speaker from Abbvie and for education from Novartis and Eli Lilly.
CN has received honoraria from Lilly, Novartis, Teva and Chiesi.
JCM has received honoraria from Lilly, Novartis, Teva, Abbvie-Allergan, Lundbeck, Chiesi, Bial, Neuraxpharm, Schwabe. FJMM has received honoraria from Lilly, Novartis, Teva, Abbvie-Allergan y Chiesi.
AMO has received honoraria from Lilly, Novartis, Allergan-Abbvie, Bial, Eisai, Grünenthal, Almirall or Neuraxpharm.
SSL has received honoraria from Allergan, Amgen, Chiesi, Eisai, Exeltis, Novartis, and Teva.
NM has received honoraria from Teva, Novartis, Lilly and Abbvie.
LMCS and SMGS have received honoraria from Lilly and Teva.
AGM has received education funding from Lilly, Novartis, Roche, TEVA, Abbvie-Allergan, & Daichi and speaker honoraria from TEVA.
NBI has received honoraria from Zambon, Actelion, Lilly and Teva.
RB has received honoraria from Abbvie, Neuraxpharma, Abbott, Teva, Novartis, Pfizer, Lilly, Almirall, Noema, Exeltis, Ergon, Neurodiem, Menarini, Biogen, Lundbeck and Medtronik.
SD has received honoraria from Abbvie, Ipsen, Lilly, Lundbeck, Novartis and Teva.
P.P.R. has received honoraria as a consultant and speaker, in the last three years, for: AbbVie, Amgen, Biohaven, Chiesi, Eli Lilly, Lundbeck, Medscape, Novartis, Pfizer and Teva. Her research group has received research grants from AbbVie, Novartis and Teva; and, has received funding for clinical trials from Alder, AbbVie, Amgen, Biohaven, Electrocore, Eli Lilly, Lundbeck, Novartis and Teva. She is the Honorary Secretary of the International Headache Society. She is in the editorial board of Revista de Neurologia, associate editor for Cephalalgia, Headache, Neurologia, Frontiers of Neurology. She is a member of the Clinical Trials Guidelines Committee and Scientific Committee of the International Headache Society. She has edited the Guidelines for the Diagnosis and Treatment of Headache of the Spanish Neurological Society. She is the founder of www.midolordecabeza.org. Pozo-Rosich P does not own stocks from any pharmaceutical company.
MH-V has received honoraria for participating on advisory boards and for collaborations as consultant, scientific communications, speaker, research support as well as funding for travel and congress-attending expenses for Abbie-Allergan, Novartis, Lilly, Almirall, Chiesi, Esai, Exeltis, Kern Pharma, Menarini, TEVA and Zambon. His research group has received research grants from Abbie-Allergan; and has received funding for clinical trials from Lilly, Novartis, TEVA.
MO, MRS, MPNP, ALB, JGU, LRF, SQ, AEI, SGL, MVCS, VAO and JGA have nothing to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Charles A, Pozo-Rosich P. Targeting calcitonin gene-related peptide: a new era in migraine therapy. Lancet. 2019;394:1765–1774. doi: 10.1016/S0140-6736(19)32504-8. [DOI] [PubMed] [Google Scholar]
- 2.Ashina M, Goadsby PJ, Reuter U, et al. Long-term efficacy and safety of erenumab in migraine prevention: Results from a 5-year, open-label treatment phase of a randomized clinical trial. Eur J Neurol. 2021;28:1716–1725. doi: 10.1111/ene.14715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sakai F, Suzuki N, Ning X, et al. Long-term safety and tolerability of Fremanezumab for migraine preventive treatment in Japanese outpatients: a multicenter, randomized, open-label study. Drug Saf. 2021;44:1355–1364. doi: 10.1007/s40264-021-01119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vernieri F, Altamura C, Aurilia C, et al. Effectiveness, safety, and tolerability of galcanezumab in a real-life setting in patients with migraine in Italy (the GARLIT study) Neurol Sci. 2020;41:487–488. doi: 10.1007/s10072-020-04669-y. [DOI] [PubMed] [Google Scholar]
- 5.Dodick DW, Silberstein SD, Bigal ME, et al. Effect of Fremanezumab compared with placebo for prevention of episodic migraine. JAMA. 2018;319:1999. doi: 10.1001/jama.2018.4853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silberstein SD, Dodick DW, Bigal ME, et al. Fremanezumab for the preventive treatment of chronic migraine. N Engl J Med. 2017;377:2113–2122. doi: 10.1056/NEJMoa1709038. [DOI] [PubMed] [Google Scholar]
- 7.Ferrari MD, Diener HC, Ning X, et al. Fremanezumab versus placebo for migraine prevention in patients with documented failure to up to four migraine preventive medication classes (FOCUS): a randomised, double-blind, placebo-controlled, phase 3b trial. Lancet. 2019;394:1030–1040. doi: 10.1016/S0140-6736(19)31946-4. [DOI] [PubMed] [Google Scholar]
- 8.Ashina M, Saper J, Cady R, et al. Eptinezumab in episodic migraine: A randomized, double-blind, placebo-controlled study (PROMISE-1) Cephalalgia. 2020;40:241–254. doi: 10.1177/0333102420905132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martin V, Tassorelli C, Ettrup A, et al. Eptinezumab for migraine prevention in patients 50 years or older. Acta Neurol Scand. 2022;145:698–705. doi: 10.1111/ane.13603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nahas SJ, Naegel S, Cohen JM, et al. Efficacy and safety of fremanezumab in clinical trial participants aged ≥60 years with episodic or chronic migraine: pooled results from 3 randomized, double-blind, placebo-controlled phase 3 studies. J Headache Pain. 2021;22:141. doi: 10.1186/s10194-021-01351-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mulleners WM, Kim B-K, Láinez MJA, et al. Safety and efficacy of galcanezumab in patients for whom previous migraine preventive medication from two to four categories had failed (CONQUER): a multicentre, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 2020;19:814–825. doi: 10.1016/S1474-4422(20)30279-9. [DOI] [PubMed] [Google Scholar]
- 12.Cetta I, Messina R, Zanandrea L, et al. Comparison of efficacy and safety of erenumab between over and under 65-year-old refractory migraine patients: a pivotal study. Neurol Sci. 2022;43:5769–5771. doi: 10.1007/s10072-022-06190-w. [DOI] [PubMed] [Google Scholar]
- 13.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 14.Ministerio de Sanidad, Consumo y Bienestar Social, Agencia Española de Medicamentos y Productos Sanitarios. Informe de Posicionamiento Terapéutico de erenumab (Aimovig®) en la profilaxis de migraña. IPT 62/2019 V1, (15 de noviembre de 2019). Informe de Posicionamiento Terapéutico de galcanezumab (Emgality®) en la profilaxis de migraña. IPT 63/2019 V1, (15 de noviembre de 2019). Informe de Posicionamiento Terapéutico de fremanezumab (Ajovy®) en la profilaxis de migraña. IPT, 11/2020. V1. [1 Oct 2022].
- 15.de Vries LS, Verhagen IE, van den Hoek TC, et al. Treatment with the monoclonal calcitonin gene-related peptide receptor antibody erenumab: A real-life study. Eur J Neurol. 2021;28:4194–4203. doi: 10.1111/ene.15075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vernieri F, Altamura C, Brunelli N, et al. Galcanezumab for the prevention of high frequency episodic and chronic migraine in real life in Italy: a multicenter prospective cohort study (the GARLIT study) J Headache Pain. 2021;22:35. doi: 10.1186/s10194-021-01247-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barbanti P, Egeo G, Aurilia C, et al. Fremanezumab in the prevention of high-frequency episodic and chronic migraine: a 12-week, multicenter, real-life, cohort study (the FRIEND study) J Headache Pain. 2022;23:46. doi: 10.1186/s10194-022-01396-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caronna E, Gallardo VJ, Alpuente A, et al. Anti-CGRP monoclonal antibodies in chronic migraine with medication overuse: real-life effectiveness and predictors of response at 6 months. J Headache Pain. 2021;22:120. doi: 10.1186/s10194-021-01328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koumprentziotis I-A, Mitsikostas DD. Therapies targeting CGRP signaling for medication overuse headache. Curr Opin Neurol. 2022;35:353–359. doi: 10.1097/WCO.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 20.McKinley EC, Lay CL, Rosenson RS, et al. Risk for ischemic stroke and coronary heart disease associated with migraine and migraine medication among older adults. J Headache Pain. 2021;22:124. doi: 10.1186/s10194-021-01338-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soni PP, Lee M, Shadbehr N, Ahmed ZA. Recent advances in the management of migraine in older patients. Drugs Aging. 2020;37:463–468. doi: 10.1007/s40266-020-00776-9. [DOI] [PubMed] [Google Scholar]
- 22.Cohen F, Yuan H, DePoy EMG, Silberstein SD. The Arrival of Anti-CGRP Monoclonal Antibodies in Migraine. Neurotherapeutics. 2022;19:922–930. doi: 10.1007/s13311-022-01230-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alex A, Vaughn C, Rayhill M. Safety and tolerability of 3 CGRP monoclonal antibodies in practice: a retrospective cohort study. Headache J Head Face Pain. 2020;60:2454–2462. doi: 10.1111/head.13956. [DOI] [PubMed] [Google Scholar]
- 24.Yang C-P, Zeng B-Y, Chang C-M, et al. Comparative effectiveness and tolerability of the pharmacology of monoclonal antibodies targeting the calcitonin gene-related peptide and its receptor for the prevention of chronic migraine: a network meta-analysis of randomized controlled trials. Neurotherapeutics. 2021;18:2639–2650. doi: 10.1007/s13311-021-01128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deng H, Li G, Nie H, et al. Efficacy and safety of calcitonin-gene-related peptide binding monoclonal antibodies for the preventive treatment of episodic migraine – an updated systematic review and meta-analysis. BMC Neurol. 2020;20:57. doi: 10.1186/s12883-020-01633-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi M, Guo J, Li Z, et al. Network meta-analysis on efficacy and safety of different anti-CGRP monoclonal antibody regimens for prophylaxis and treatment of episodic migraine. Neurol Res. 2021;43:932–949. doi: 10.1080/01616412.2021.1940672. [DOI] [PubMed] [Google Scholar]
- 27.Messina R, Huessler E-M, Puledda F, et al (2023) Safety and tolerability of monoclonal antibodies targeting the CGRP pathway and gepants in migraine prevention: A systematic review and network meta-analysis. Cephalalgia. 43(3). 10.1177/03331024231152169 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix 1. Sensitivity analysis of quantitative endpoints at month 6.
Data Availability Statement
The datasets used and/or analysed during this study are available from the corresponding author on reasonable request from any qualified investigator.