ABSTRACT
Background:
Online education has become a norm since the pandemic and it was a complete change for the medical curriculum. Many students missed patient interaction, which was a crucial part of their learning.
Aim:
This study was designed to know the perceptions of online teaching of both the non-competency-based medical education (non-CBME) and competency-based medical education (CBME) curriculum during the coronavirus disease 2019 (COVID-19) pandemic, learning outcomes, and health-related problems due to online teaching-learning in medical undergraduates.
Materials and Methods:
It was an online survey done after ethics approval. The survey questionnaire was sent to all medical undergraduates via email or WhatsApp and responses were recorded after informed consent. The total number of students who completed the survey was 346.
Results:
66% of students found that online classes were not as enjoyable as offline. 66% found them time-saving with learning at their own pace. 85% felt they learned no clinical skills, and 80.6% said there was a lack of practical demonstrations. 71% experienced digital fatigue, 62% missed learning in a group, and 73% felt the poor motivation to study. Only 30% and 18.7% were confident enough to take a history or do an examination of the patient, respectively, after online clinics. 33% were confident to appear for university theory and only 11% for practical exams. The health problems faced due to online teaching included somatic complaints, sleep disturbances anxiety, and depressive symptoms in 40% of students.
Conclusions:
The students were dissatisfied with online teaching. Learning outcomes were affected, as they were not confident to appear for university exams. Hence, though teaching happened during the pandemic, the online education imparted revealed lacunae and health effects.
Keywords: Health outcomes, learning outcomes, medical education, online teaching
The coronavirus disease 2019 (COVID-19) pandemic has impacted all aspects of our lives, including education and the economy, as we know it.[1] The subsequent implementation of social distancing during the COVID-19 pandemic has forced colleges and universities to empty their classrooms and keep students away from institutions. Hence, online classes have become a key component in the continuity of education.[1]
Medical schools are known for their intensive curriculum and workload.[2] There has been a sudden shift in teaching modality from traditional face-to-face lectures to online teaching, with problems being faced by teachers and students alike.[3] For teachers, the method is new, and also an added responsibility. Medical students have borne the brunt of a monotonous series of lectures without breaks with limited interpersonal or patient interactions.[1-4] Though the new competency-based medical education (CBME) curriculum implemented from batch 2019 has taken into consideration the modules on group discussions, attitudes, ethics and communication, implementing these in the online format required some time.[5] The non-CBME pre-final and final year students who needed actual patient interactions and clinics to observe procedures, surgeries, etc., lost on this learning.
Several researchers studied the perception of online teaching but very few reflect upon the learning outcomes of the students from this online education. Hence, the present study was designed to understand in undergraduate medical students of an urban medical college and tertiary hospital, the perceptions of online teaching of both the non-CBME and CBME curriculum during the COVID-19 pandemic, learning outcomes of the online education, and health-related problems due to online teaching-learning.
MATERIALS AND METHOD
This was a cross-sectional study conducted online in an urban medical college after institutional ethics committee (IEC) approval over 1.5 months. A survey questionnaire was designed by the faculty members from the department of psychiatry, community medicine, pharmacology and therapeutics, and anatomy, which comprised of closed-ended Y/N type questions, Likert scale questions, multiple-choice questions, and open-ended questions. The questionnaire was then validated by the faculty of the department of medical education. It included demographic details, and questions regarding perceptions of online teaching like the schedule of the online classes, modalities used, advantages, disadvantages, common demotivators experienced, etc.
The learning outcomes were recorded on a 5-point Likert scale on domains of knowledge, practical skills, and communication skills. The health outcomes had questions on somatic symptoms, anxiety, depression, and social behaviors [Appendix 1].
The survey form was distributed to only the undergraduate medical students of this medical college attached to a tertiary care hospital via WhatsApp class groups, and class email groups available from the college administrative section. Students not willing to give consent for participation, interns, PG residents, BPMT, BOTH, BPTH, and nursing students of the college were excluded from the study. Snowball sampling method was used. The total number of undergraduate students was 864 and we had a 40% response rate to the survey.[6] The total number of respondents who completed the survey was 346. The data was entered in MS Excel, and sociodemographic variables and perceptions about online teaching, learning, and health outcomes were analyzed using descriptive statistics and frequency distribution.
Ethics committee/Institutional review board’s permission
The study was assessed and approved by the institutional ethics committee with reference number EC/OA-122/2021, dated July 1, 2021.
RESULTS
The total number of respondents who completed the survey was 346. The age range of the respondents was 18–25 years with a mean age of 20.5 ± 2.5 years. 59.5% [206/346] were males, 39.9% [138/346] were females and 0.5%[1] preferred not to disclose the gender. 24.5% [85/346] were from the first year, 29.1% [101/346] from the second year, 22.2% [77/346] from the third, and 23.9% [83/346] were from the final year of medical school, respectively.
Common perceptions of online teaching
66.2% [229/346] of the students had no exposure to any online teaching before the pandemic. Maximum participants stated that the online teaching started in April/May 2020. The online teaching was scheduled for 7–8 h for the first year, 3–4 h for the second year, and 1–2 h for third and final year students. Majority [86%] expressed that each class was of 1 h with a break of 5–10 min between classes. However, only 42.8% [218/346] found the online teaching schedule convenient as compared to 34.4% [119/346] who did not whereas 22.8% [79/346] of the students were unsure about the same. Among the different teaching methods, live lectures [95.3%] accounted for the most Figure 1.
Figure 1.
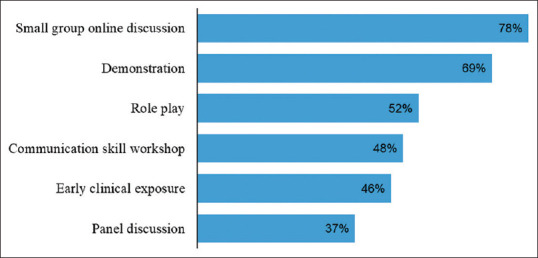
Online teaching methods for first and second year CBME
67.7% [126/186] of students agreed that the CBME curriculum was followed Figure 2.
Figure 2.
Online teaching methods for third year students
100% of the students had missed their clinical postings for an average of 9 months duration. 89.3% [143/160] were unsatisfied with the practical skills taught in online classes and 11.2% [18/160] were unsure. 68.1% [109/160] of students said that adequate teaching was not done during the online clinical postings whereas 20.0% [32/160] of the students were neutral.
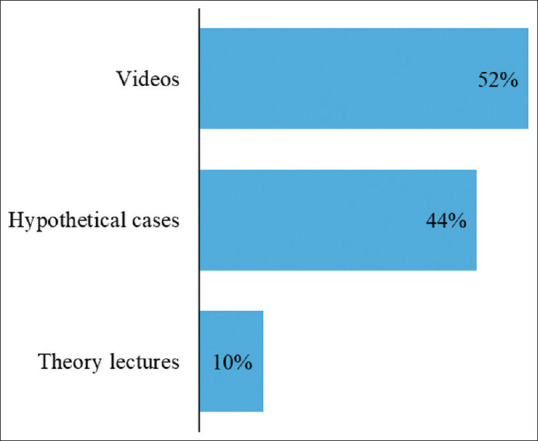
Though 66.7% [231/346] students said that online classes were not as enjoyable as off-line, many perceived that it had some advantages too Figure 3.
Figure 3.
Advantages of online education
However, when their perceptions about limitations of online teaching were considered, then 84.6% [293/346] felt that they gained no clinical experience, 80.6% [279/346] said there was a lack of practical demonstrations, 70.8% [245/346] expressed digital fatigue, 65.6% [227/346] gave connectivity issues, 62.1% [215/346] found a reduction in their social life and missed learning in a group, 61% [210/346] students felt that teaching was monotonous, 50% [173/346] expressed disturbances due to background noise which caused a lack of concentration, 33.2% [115/346] students felt that essential doubts were not resolved.
When the students were asked for suggestions to improve the problems faced, only 11.3% [39/346] students suggested teachers use whiteboards and markers and have small group discussions as the possible solutions.
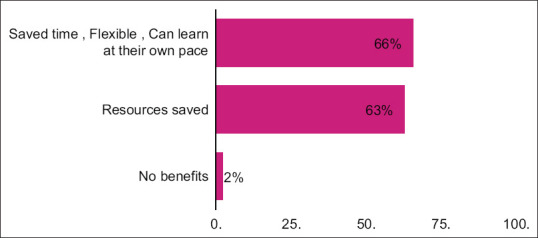
An analysis of the motivation revealed that 73.4% [254/346] students felt online teaching led to poor motivation and the common demotivators experienced were lack of self-discipline in 85.9% [219/254], no physical group discussion with friends in 78.9% [200/254], lack of competitive environment in 69.1% [176/254] with the home being a comfortable space, and lack of motivation to study in 55.1% [140/254] students Figure 4.
Figure 4.
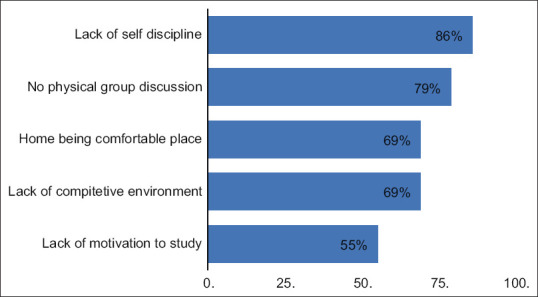
Common demotivators of online education
Learning outcomes of attending online education
The students were asked for their perceptions regarding the learning outcomes, which were categorized as per knowledge, practical skills, and communication skills. On analysis of the knowledge domain, only 19% [68/346] of students felt they were able to recall most of the information taught in the class and were able to explain a particular topic confidently whereas 40% [138/346] disagreed and the other 40% [140/346] students were neutral. Only 24.6% [83/346] said that their doubts were resolved in the online lecture, though 55.5% [190/346] of them agreed that doubts asked by other students in online lectures helped them to clear their concepts. Only 23.7% [82/346] of students felt confident to appear for the university theory examination.
When their practical skills were looked into, then only 13.5% [47/346] of students said that they were able to grasp the practical skills taught online, with only 12% [42/346] being confident enough to perform the acquired skill. Only 18.7% [47/256] of the second, third, and final year students were confident enough to do a clinical examination of a patient with only 11.2% [39/346] being confident to appear for university practical examinations.
When we looked at the communication skills of the students, then only 28.5% [71/256] felt they would be able to establish rapport with the patient, 23% [61/256] were confident to talk to a patient, and only 30% [75/256] students felt confident to take a history of a patient.
Health outcomes while attending online classes
The students faced several health-related problems during the online teaching. 42.7% [148/346] of the students had several somatic disturbances, which included eyestrain in 89.8% [133/148], posture difficulties in 75.6% [112/148], headaches in 71.6% [106/148], and auditory fatigue in 50% [74/148] of the students. 42.7% [148/346] of them experienced sleep disturbances, which included difficulty in falling asleep in 73.6% [109/148], insomnia in 41.2% [61/148], and early morning awakening in 31.7% [47/148] of the students. 31.5% [109/346] of the students gave depressive symptoms, which predominantly included sadness of mood in 77.0% [84/109], followed by lethargy in 70.6% [77/109], hopelessness in 69.7% [76/109], reduced interest in pleasurable activities in 66.9% [73/109], and crying in 46.7% [51/109] of the students. Around 15.5% [17/109] of the students also expressed suicidal thoughts. Anxiety symptoms were given by 39.8% [138/346] of the students. 88.4% [122/138] of them gave worried about the future, 67.4% [93/138] had irritability, 63.7% [88/138] experienced restlessness with ruminations, palpitations, and tremors seen in about 25–30% of the students.
The majority of them [84.4%; 292/346] complained about missing friends [78.7%; 272/346] being on the campus, participating in extracurricular activities [71.1%; 246/346], hanging out in the canteen [69.9%; 242/346], and even communicating emotional problems to friends [52.9%; 183/346].
DISCUSSION
Several researchers across the globe studied the impact of virtual learning or online teaching as a new method of delivering the content course during the pandemic. Qualitative analysis found that time management was considered to be a dominant perspective as students reported that saving time on traveling gave them an added advantage to study more which reportedly improved their performance in exams.[7] Bączek et al.[8] also reported that frequent advantages of e-learning chosen by respondents were the ability to stay at home (69%), continuous access to online materials (69%), the opportunity to learn at your own pace (64%), and comfortable surroundings (54%). This finding is in keeping with our study where 66% of the students felt that online teaching saved time and they could learn at their own pace.[9,10] 63% also felt that resources were saved as traveling did not happen. There was no Indian data available on the content of the online teaching program or the modes of teaching used for the new CBME curriculum. Two-thirds of our CBME batches got exposure to various teaching experiences like role-plays, small group discussions, and early clinical exposure as compared to the non-CBME group where 89% were unsatisfied with the case vignettes and hypothetical cases that were taught to them instead of the live patient clinics. Hence, 100% missed the clinical postings and practical demonstrations. Our findings are contrary to studies where students accepted the innovative online clinically based pediatric module, which included online lectures, discussion forums, e-learning scenarios, clinical examination videos, and videoconferencing tutorials.[11]
Nearly 66% of our students did not find the online teaching enjoyable and 85% felt that they did not gain any clinical experience. This probably could be because learning about patients and getting exposure to several patients in a day, which was possible in the pre-pandemic period, was sorely missed by our students. Our medical college is also attached to a general hospital, which has a huge patient load and is a tertiary center where patients are seen in outpatient departments without appointments. However, other researchers reported that students found the virtual learning experience to be an effective way to deliver course content,[12] 73% of Polish students felt e-learning to be enjoyable.[8] Researchers reported that remote teaching was a poor substitute for clinical teaching and students in their country had lost 4 months of workplace experience,[13] whereas our students had lost 9 months. Clinical skills learning has been cited as a gap in remote learning curriculum for 50% of students.[10]
The challenges of online teaching reported by more than 60% of our students included lack of clinical exposure, digital fatigue, connectivity problems, and missing out on social life. Similarly, the majority of respondents chose lack of interactions with patients (70%) and technical problems with information technology (IT) equipment (54%) as the main disadvantages of online teaching,[8] whereas some felt the lectures to be too long or suboptimal in content with technical problems like the use of online tools and internet connectivity.[7] A low prevalence (18%) of digital fatigue as compared to our findings has also been reported.[10]
In a preclinical study during the pandemic, the students felt that in all curricular components, the quality of instruction was very negatively affected by the remote learning transition, especially in anatomy (49/74, 66.2%), ultrasound (39/47, 83.0%), and the ambulatory care preceptorship (51/53, 96.2%).[10] Along with this, poor motivation to study was an important factor noted by several studies which is in keeping with our findings.[10,14]
The perceptions of students on the learning outcomes via online education were disheartening. Less than 20% of the students felt that they had achieved adequate knowledge and could understand, recall, or confidently discuss the topic. Only 13% felt that they could interact with patients and had adequate practical skills to appear confidently in university practical exams. Less than 30% of the students were comfortable talking to patients or even taking a history. The period of the pandemic definitely caused a tremendous loss in the teaching and learning process and the development of clinical skills especially in the third and final years of medical school are the most important in developing career choices for specialization and confidence in treating patients. Our findings show a lack of all these skills in the undergraduates. This was also because this city being a major financial capital also had a high COVID-19 patient load due to which the general hospitals were looking after only COVID patients as compared to routine cases and with the government policies of only online classes, the students missed clinical postings and in-person patient interactions.
50.8% of students cited poor clinical skills learning, and deficiencies with history-taking and physical exam training, thus leaving them unprepared for clinical assessments and encounters.[10] Nearly (74.9%) had a clinical rotation that was cut short or canceled due to COVID-19 and 93.7% reported not being involved in clinical rotations with in-person patient contact at the time of the study.[15] Students perceived that some teachers still had difficulty in planning videoconferences, or using interactive methods through web services.[16] Thus, even if the medical course was well laid out and structured before the pandemic, structuring the clinical case discussions in virtual classrooms proved too hard, demanding, and required a great effort in interaction from both teacher and students which therefore affected the quality of medical education. Thus, overall, the confidence of the students did seem to be affected globally due to the effects of the pandemic on medical education.
Health outcomes in medical students due to the pandemic have been widely studied with nearly 84.1% feeling anxious due to the pandemic or having emotional exhaustion and burnout before and after the pandemic was seen.[15] 16.7% of students reported isolation, feelings of disconnectedness, or declining mental health in their responses.[10] They also expressed that anxiety and uncertainty made it difficult for them to focus on academics. We got higher rates of anxiety and somatic complaints in our study as compared to other researchers which could be due to methodological differences and that we specifically asked for the impact of online education on their psyche. More than 80% of our students missed socially meeting friends, campus life, and participating in activities that are essential for the holistic development of students. In a similar study, respondents mentioned missing out on extensions, parties, group projects, and even lunch or a break in the cafeteria which were a part of their college life.[16]
Our research was done in an urban medical college. The perceptions of students in rural places could be different. The low response rate from students could also impact the inferences drawn. This was a limitation of our study.
CONCLUSIONS
This study has helped in identifying the perceptions of the undergraduates about this mode of teaching and the learning outcomes. The students were dissatisfied with online teaching. Learning outcomes were affected as they were not confident to appear for university exams. Hence, though teaching happened during the pandemic, the online education imparted revealed lacunae and health effects seen in the medical undergraduates.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical statement
The study was assessed and approved by the institutional ethics committee with reference number EC/OA-122/2021, dated 1st July 2021.
Informed consent
Informed consent was obtained from all individual participants included in the study. Participant consent statement was taken as per institutional ethics committee approval along with consent taken for participation in the study and publication of the scientific results/clinical information/image without revealing their identity, name or initials. The participant is aware that though confidentiality would be maintained anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
APPENDIX 1
The COVID19 pandemic has brought a drastic shift in teaching modality from traditional facetoface lectures in college to online classes. You are invited to participate in a survey on the perception of online teaching, learning, and health outcomes during the pandemic.
I give my informed consent
Yes/no
Part A] Preliminary data
Age:
Sex: M/F/Other
Medical school year: I/II/III/IV
Part B] Perception of online teaching experience
Did you do online learning before the pandemic [it can be other than college]: Yes/No
Please fill in information about your current online classes:
Online medical teaching started since? _______
Total hours/day spent for the class:
Duration of each class: 30 min/45 min/1 h/1 h 30 min/any other______
Breaks between classes: Y/N
Time of break: 5 min/10 min/15 min/30 min/any other _____
Did you consider the online teaching schedule to be convenient?: Y/N/not sure
How are the online classes conducted? (You can choose multiple options)
Live lecture
Prerecorded lecture
Question bank discussion
Recordings of practicals/procedures
Any other format:.............
Do you feel the online sessions to be more interactive than offline classes: Y/N/not sure
If Y, then what makes it interactive: (You can choose multiple options)
Chat box/asking questions to professor/professor makes it engaging by asking questions/professor makes it engaging by discussing clinical scenarios/any other ________
Do you find the sessions more enjoyable than offline classes? Y/N/not sure
What do you feel are the benefits of attending the online classes: (You can choose multiple options)
Save time
Flexible with schedule
Can learn at one's own pace
Difficulties can be resolved one to one
Resources of transport saved
Any other.
What do you feel are the difficulties in attending the online classes: (You can choose multiple options)
Monotonous
Disturbance due to background noise
Essential doubts not resolved
No practical demonstrations
Timing of lectures
No clinical experience
Miss learning in a group
Digital fatigue
Connectivity issues
Reduced social life
Any other...............
Do you find any solution for the problems you faced? Y/N/not sure, if yes mention _____
Do you feel that online teaching leads to poor motivation? Y/N/not sure
Common demotivators experienced were: (You can choose multiple options)
Lack of competitive environment as in college premises
Home being a comfortable place
No physical group discussions with friends
Lack of selfdiscipline
Lack of motivation from teachers
Any other __________
Please answer the following questions if you are I/II year students
Do you think that the CBME curriculum was followed during online teaching? Y/N/not sure
CBME curriculum consists of the following methods of teaching, which of them were followed/are scheduled and will be done in the online classes?
Demonstrations: y/n/not sure
Small group discussion: y/n/not sure
Seminars: y/n/not sure
Communication skill workshop: y/n/not sure
Panel discussion: y/n/not sure
Roleplay: y/n/not sure
Early clinical exposure: y/n/not sure
Please answer the following questions if you are III/IV year students
-
Did you miss on your clinical postings during the pandemic? Y/n/not sure
If yes: How many months of postings............
Were online clinics scheduled for you? Y/n/not sure
Are you satisfied with the practical skills taught in online classes? Y/n/not sure
-
The online clinics included: (You can choose multiple options)
- Real patients
- Simulated patients
- Videos
- Any other.........
Do you feel that adequate teaching was done during clinical posting? Y/N/Not sure
Part C] Perception of online learning outcomes
What are your perceptions of your learning outcomes after attending online classes?
1. I am able to recall most of the information taught in the class.
Strongly agree/agree/neutral/disagree/strongly disagree
2. I am able to explain a particular topic confidently
Strongly agree/agree/neutral/disagree/strongly disagree
3. My doubts have been resolved in the online lecture
Strongly agree/agree/neutral/disagree/strongly disagree
4. Doubts asked by other students in online lectures have helped me to clear my own concepts
Strongly agree/agree/neutral/disagree/strongly disagree
5. Online sessions with help of animated videos were precise and gave a clear view of the topic
Strongly agree/agree/neutral/disagree/strongly disagree
6. I was able to grasp the practical skills taught online
Strongly agree/agree/neutral/disagree/strongly disagree
7. I feel confident enough to perform the acquired skill
Strongly agree/agree/neutral/disagree/strongly disagree
8. I feel confident about taking a history from the patient
Strongly agree/agree/neutral/disagree/strongly disagree
10. I feel confident to do a clinical examination of the patient
Strongly agree/agree/neutral/disagree/strongly disagree
11. I feel confident about appearing for theory examinations of the university
Strongly agree/agree/neutral/disagree/strongly disagree
12. I feel confident about appearing for practical examinations of the university
Strongly agree/agree/neutral/disagree/strongly disagree
Part D] Perception of health issues
What health issues did you experience while attending online classes? (You can choose multiple options)
Headache
Auditory fatigue
Posture problems
Eyestrain
Sleep disturbances
Anxiety symptoms (worrying, preoccupations, restlessness, irritability, palpitations, tremors)
Depressive symptoms (sadness, lethargy, decreased interest, feeling helpless or hopeless with the situation)
Any other _____________
-
Missing social life like (You can choose multiple options)
- Meeting friends
- Being on the campus
- Hanging out in the college canteen with your friends
- Not able to communicate your emotional problems to your friends
- Extracurricular activities like cultural fest, etc.
- Any other_____
REFERENCES
- 1.Rajab MH, Gazal AM, Alkattan K. Challenges to online medical education during the COVID-19 pandemic. Cureus. 2020;12:e8966. doi: 10.7759/cureus.8966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chatterjee S. The COVID-19 pandemic through the lens of a medical student in India. Int J Med Stud. 2020;8:82–3. [Google Scholar]
- 3.Camargo CP, Tempski PZ, Busnardo FF, Martins MD, Gemperli R. Online learning and COVID-19:A meta-synthesis analysis. Clinics. 2020;75:e2286. doi: 10.6061/clinics/2020/e2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desai D, Sen S, Desai S, Desai R, Dash S. Assessment of online teaching as an adjunct to medical education in the backdrop of COVID-19 lockdown in a developing country–An online survey. Indian J Ophthalmol. 2020;68:2399–2403. doi: 10.4103/ijo.IJO_2049_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131–2. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 6.Finchman JE. Response rates and responsiveness for surveys, standards and the Journal. Am J Pharm Educ. 2008;72:43. doi: 10.5688/aj720243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khalil R, Mansour AE, Fadda WA, Almisnid K, Aldamegh M, Al-Nafeesah A, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia:A qualitative study exploring medical students'perspectives. BMC Med Educ. 2020;20:285. doi: 10.1186/s12909-020-02208-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bączek M, Zagańczyk-Bączek M, Szpringer M, Jaroszyński A, Wożakowska-Kapłon B. Students'perception of online learning during the COVID-19 pandemic:A survey study of Polish medical students. Medicine. 2021;100:e24821. doi: 10.1097/MD.0000000000024821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hanafy SM, Jumaa MI, Arafa MA. A comparative study of online learning in response to the coronavirus disease 2019 pandemic versus conventional learning. Saudi Med J. 2021;42:324–31. doi: 10.15537/smj.2021.42.3.20200741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shahrvini B, Baxter SL, Coffey CS, MacDonald BV, Lander L. Pre-clinical remote undergraduate medical education during the COVID-19 pandemic:A survey study. BMC Med Educ. 2021;21:1–3. doi: 10.1186/s12909-020-02445-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conlon TA, Mc Carthy P, Mc Govern R, Slattery S, Yates J, Murphy S. The impact of COVID-19 on medical student education-navigating uncharted territory. Ir Med J. 2020;113:109. [PubMed] [Google Scholar]
- 12.Donohue KE, Farber DL, Goel N, Parrino CR, Retener NF, Rizvi S, et al. Quality improvement amid a global pandemic:A virtual curriculum for medical students in the time of COVID-19. MedEdPORTAL. 2021;17:11090. doi: 10.15766/mep_2374-8265.11090. doi:10.15766/mep_2374-8265.11090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cairney-Hill J, Edwards AE, Jaafar N, Gunganah K, Macavei VM, Khanji MY. Challenges and opportunities for undergraduate clinical teaching during and beyond the COVID-19 pandemic. J R Soc Med. 2021;114:113–6. doi: 10.1177/0141076820980714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guse J, Heinen I, Kurre J, Mohr S, Bergelt C. Perception of the study situation and mental burden during the COVID-19 pandemic among undergraduate medical students with and without mentoring. GMS J Med Educ. 2020;37:Doc72. doi: 10.3205/zma001365. doi:10.3205/zma001365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harries AJ, Lee C, Jones L, Rodriguez RM, Davis JA, Boysen-Osborn M, et al. Effects of the COVID-19 pandemic on medical students:A multicenter quantitative study. BMC Med Educ. 2021;21:1–8. doi: 10.1186/s12909-020-02462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chinelatto LA, Costa TRD, Medeiros VMB, Boog GHP, Hojaij FC, Tempski PZ, et al. What you gain and what you lose in COVID-19:Perception of medical students on their education. Clinics (Sao Paulo) 2020;75:e2133. doi: 10.6061/clinics/2020/e2133. doi:10.6061/clinics/2020/e2133. [DOI] [PMC free article] [PubMed] [Google Scholar]


