Abstract
The incidence of both atrial fibrillation (AF) and coronary artery disease (CAD) increases with advancing age. They share common risk factors and very often coexist. Evidence points to an intricate relationship between atrial tissue excitability and neuronal remodeling with ischemia at the microcirculatory level. In this review, we delineated this complex relationship, identified a common theme between the two, and discussed how the knowledge of this relationship translates into a positive and meaningful impact in patient management. Recent research indicates a high prevalence of CAD among AF patients undergoing coronary angiography. Further, the incidence of AF is much higher in those suffering from CAD compared to age-matched adults without CAD underlying this reciprocal relationship. CAD adversely affects AF by promoting progression via re-entry and increasing excitability of atrial tissue as a result of ischemia and electrical inhomogeneity. AF in turn accelerates atherosclerosis via endothelial dysfunctional and inflammation and together with enhanced thrombogenicity and hypercoagulability contribute to micro and macrothrombi throughout cardiovascular system. In a nutshell, the two form a vicious cycle wherein one disease promotes the other. Most AF recommendations focuses on rate/rhythm control and prevention of thromboembolism. Very few studies have discussed the importance of unmasking coexistent CAD and how the treatment of underlying ischemia will impact the burden of AF in these patients. Inflammation and endothelial dysfunction remain central to both disease processes and form a handsome therapeutic target in the management of the two diseases. The relationship between AF and CAD is complex and much more than mere coincidence. The two diseases share common risk factor and pathophysiology. Hence, it is impractical to treat them in isolation. Accordingly, we share the implications of managing underlying ischemia and inflammation to positively impact and improve quality of life among AF patients.
Keywords: Atrial fibrillation, Coronary artery disease, Antithrombotic therapy, Ischemia, Early rhythm control, Endothelial dysfunction
Core Tip: Evidence points to an intricate relationship between atrial tissue excitability and neuronal remodeling with ischemia at the microcirculatory level. In this review, we delineated this complex relationship, identified a common theme between the two, and discussed how the knowledge of this relationship translates into a positive and meaningful impact on patient management.
INTRODUCTION
Cardiovascular diseases including coronary artery disease (CAD) and atrial fibrillation (AF) along with other cardiovascular diseases remain the leading cause of morbidity and mortality worldwide[1]. The prevalence of both CAD and AF increases with advancing age and they often coexist[2-5]. However, this relationship is not a mere coincidence and recent evidence points to the intricate relationship between the two. Dedicated studies have demonstrated a high prevalence of CAD among nonvalvular AF patients, with majority of AF (> 50%) patients having underlying CAD as identified by invasive or computed tomography coronary angiography[5-7]. This is significantly higher than the prevalence of CAD in the general population, which is estimated to be about 12%-14%. Furthermore, there is abundant evidence that AF is an independent risk factor for CAD and incident acute coronary syndromes[4,8,9]. The interrelationship of the two is further highlighted by the fact that the people with coexistent AF and CAD have a more severe CAD and higher SYNTAX scores compared to those without AF[8,10]. Also, the morbidity and mortality is significantly higher when CAD is associated with paroxysmal or persistent AF with increased odds for developing heart failure, ventricular arrythmias, and major adverse cardio-cerebro vascular events (MACCEs)[4,8-10]. However, despite the obvious association, this relationship is also influenced by a number of confounding risk factors such as diabetes, hypertension, age, and obesity which are common to both CAD and AF. Hence, this leads to confusion in establishing causality and reverse causality solely based on the results from registries and observational studies.
A recent mendelian randomization study by Yan et al[4] shed important light on this relationship and concluded beyond doubt that CAD is an independent risk factor for AF after removing all bias. Furthermore, they made an argument that treatment and prevention of AF is crucial to prevent MACCE among CAD patients[4]. Hence, the two might be more closely related than thought, and logically the therapeutic strategies are expected to be similar as well.
PATHOPHYSIOLOGICAL BASIS OF THE RELATIONSHIP
The basic pathology in CAD is the formation and progression of atherosclerotic plaques in coronary arteries leading to narrowing and resultant myocardial ischemia. Indeed, this process is identical in other vascular beds involved by atherosclerotic process and manifests as variable clinical presentation depending on the vasculature involved. In the heart, the same can manifest as acute coronary syndrome (ACS) or chronic coronary syndrome (CCS) depending upon the progression and stability of the atherosclerotic plaques. The major pathophysiological pathways involved in initiation and progression of AF include re-entry and focal ectopic activity. The re-entry is in turn promoted by the short refractoriness, slowed conduction, and atrial remodeling as a result of atrial dilatation. The enhanced automaticity of the atrial tissue stems from the enhanced early afterdepolarizations (EADs) and delayed afterdepolarizations (DADs)[9,11].
Common risk factors
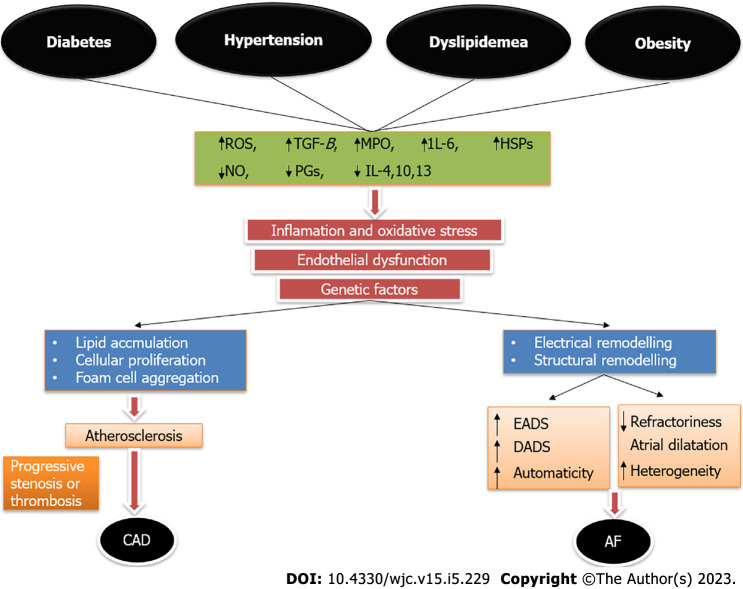
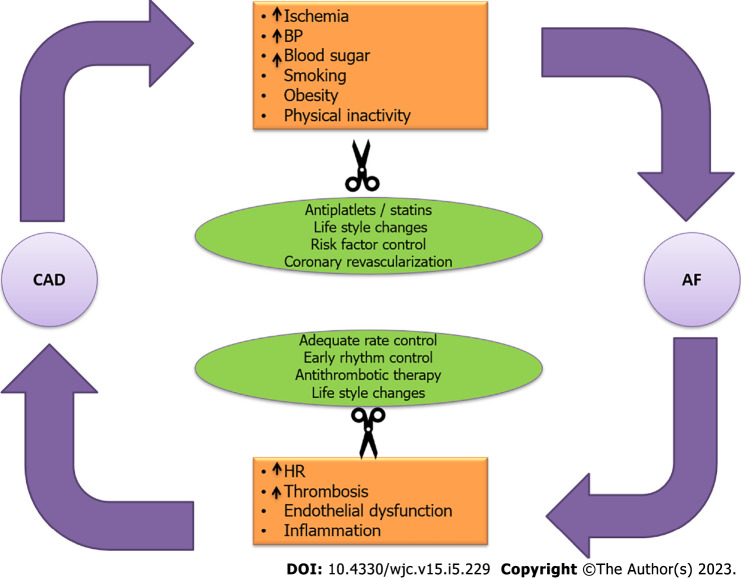
The two diseases share identical risk factors, which trigger varied pathophysiological responses culminating in either or both of the two diseases. Diabetes mellitus (DM), hypertension, advancing age, dyslipidemia, obesity, smoking, and decreased physical activity are the major risk factors for CAD as per abundant evidence in the scientific literature. Indeed, these very same risk factors remain the most commonly implicated factors responsible for the initiation and progression of AF[8,9,11,12]. The interplay of the various risk factors and their role in the pathogenesis of AF and CAD have been demonstrated in Figure 1.
Figure 1.
Interplay of various common risk factors in the pathogenesis of coronary artery disease and atrial fibrillation. Variable genetic expression manifests as varied clinical phenotype in the form of either or both atrial fibrillation and coronary artery disease in an individual. AF: Atrial fibrillation; CAD: Coronary artery disease; EAD: Early after depolarization; DAD: Delayed after depolarization; HSPs: Heat shock proteins; IL: Interleukin; MPO: Myeloperoxidase; NO: Nitric oxide; PGs: Prostaglandins; ROS: Reactive oxygen species; TGF-β: Transforming growth factor beta.
DM particularly in the setting of poorly controlled blood sugars is a major risk factor for initiation of AF. Research has shown a consistent positive correlation between increasing hemoglobin A1C and AF burden. The most popular hypothesis for this association is the structural alteration and fibrosis in atrial myocardium as a result of inflammation, endothelial dysfunction, formation of reactive oxygen intermediates, and deposition of advanced glycation end products[13,14]. All of these to a large extent result in microvascular dysfunction and atrial tissue hypoxemia. Prolonged action potential duration secondary to ischemia pave the way for EADs and DADs. Often there is coexistent autonomic neuropathy and dysfunction in DM, which together with altered calcium (Ca2+) and Ina homeostasis contributes to the progression of AF[15].
Hypertension remains the most common risk factor for both AF and CAD. It increases the risk of development of AF by more than 30% for any given age[16]. Left ventricular hypertrophy and subsequent diastolic dysfunction in longstanding hypertension contributes to atrial dilatation and dysfunction. Furthermore, alterations in the renin angiotensin aldosterone system along with the increased expression of pro-inflammatory cytokines induce atrial fibrosis[17,18]. The net result of these pathogenic mechanisms is the development of focal aberrant ectopic firing due to altered Ca2+ homeostasis and the development of re-entry circuits along clinical or subclinical fibrosis in atrial myocardium[19].
Obesity is often associated with other cardiovascular comorbidities, which contribute to enhanced overall MACCE risk. In addition, many advocate that obesity is an inflammatory disease process characterized by increased expression of various pro-inflammatory cytokines and resultant endothelial dysfunction. This often correlates with increased left atrial volume and fibrosis, which have a pathogenic role in the development of AF[20]. According to certain estimates, the risk of AF increases in a linear fashion with increasing body mass index (BMI) and roughly a 1 kg/m2 increase in BMI confers a 4% increased risk of developing AF[9,21].
Positive feedback cycle
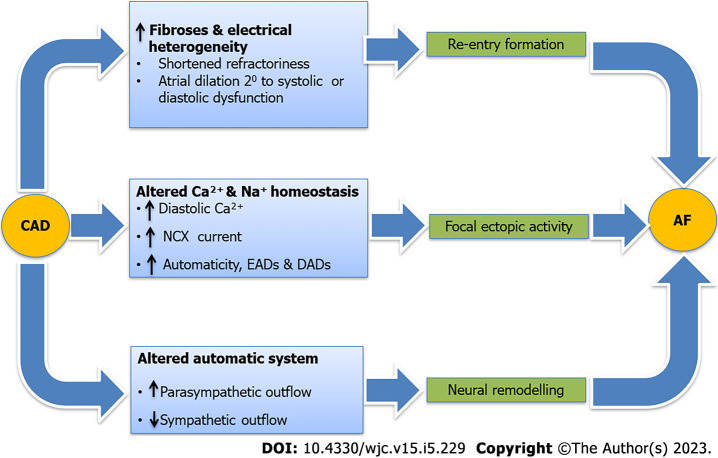
Besides sharing common risk factors, CAD and AF by themselves have a direct relationship with each other. A positive feedback mechanism between the two, culminates in a vicious cycle resulting in increased the burden of the two diseases. CAD comprising both macrovascular and microvascular disease leads to ischemia of the atrial tissue which precedes local inflammation and culminates in fibrosis and prolonged conduction times, all of which trigger the three principle mechanisms involved in the pathogenesis of AF which are focal ectopy, re-entry and neural alteration. In addition, there is heterogeneity in the electrical conduction, altered Ca2+ and sodium currents, and autonomic system dysregulation, all of which promote the progression and persistence of AF[4,8,9,11,12,22,23] (Figure 2).
Figure 2.
Pathogenic mechanism that predisposes an individual suffering from coronary artery disease to develop atrial fibrillation. AF: Atrial fibrillation; CAD: Coronary artery disease; NCX: Na+/Ca2+ exchanger; EAD: Early after depolarization; DAD: Delayed after depolarization.
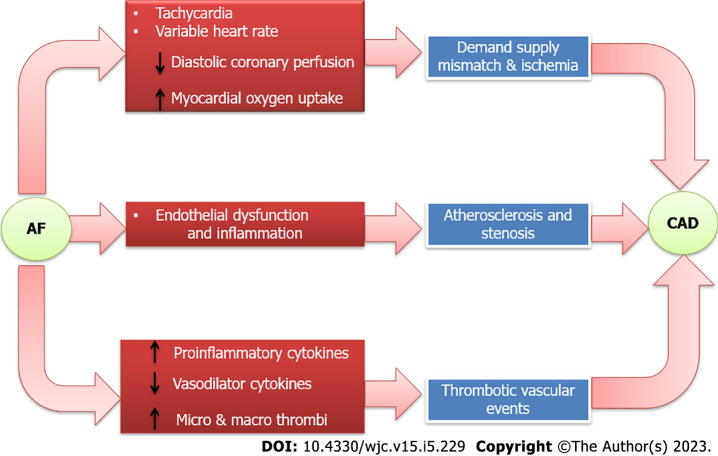
On the other end, AF by itself can induce the two key pathogenic mechanisms involved in CAD, namely endothelial dysfunction and inflammation. Decreased release of nitric oxide coupled with increased expression of von Willebrand factor is the key pathogenic process in endothelial dysfunction[9,11,17]. AF also triggers systemic and myocardial inflammation by virtue of enhancing expression of protease-activated receptors and inflammatory cytokines, which not only initiate atherosclerotic process but also contribute to plaque instability and resultant ACS. Besides this, the beat-beat variability resulting in inefficient contractility and reduced cardiac output also contribute to reduced coronary blood flow and resultant ischemia independent of atherosclerotic CAD. Coagulation system activation coupled with enhanced platelet activity due to increased expression of p-selectin and cluster of differentiation 63 (CD63) on endothelial cells leads to micro and macro thrombi, which not only increases the risk of cerebrovascular accident but also ACS[24-26] (Figure 3).
Figure 3.
Pathogenic mechanisms that predispose an individual suffering from atrial fibrillation to develop coronary artery disease. AF: Atrial fibrillation; CAD: Coronary artery disease; NCX: Na+/Ca2+ exchanger.
The two more often than not coexist and together they confer worse outcomes than when the two occur in isolation. When AF complicates pre-existing CCS or ACS, it leads on to higher MACCE events including stroke, heart failure, and cardiogenic shock and also doubles overall cardiovascular mortality[8,9,11,27]. Further, it complicates clinical decision making and predisposes an individual to not only increased thrombotic events but also to major bleeding events secondary to aggressive antithrombotic therapy, which is often indicated. As a result, there is a need for a comprehensive assessment and management of the two diseases in conjunction and not as separate disease entities. The two diseases more often than not are linked in their etiopathogenesis and warrant kindred treatment to break the links which propagate the two diseases.
Differences in pathogenesis of AF in CAD patients compared to those without CAD
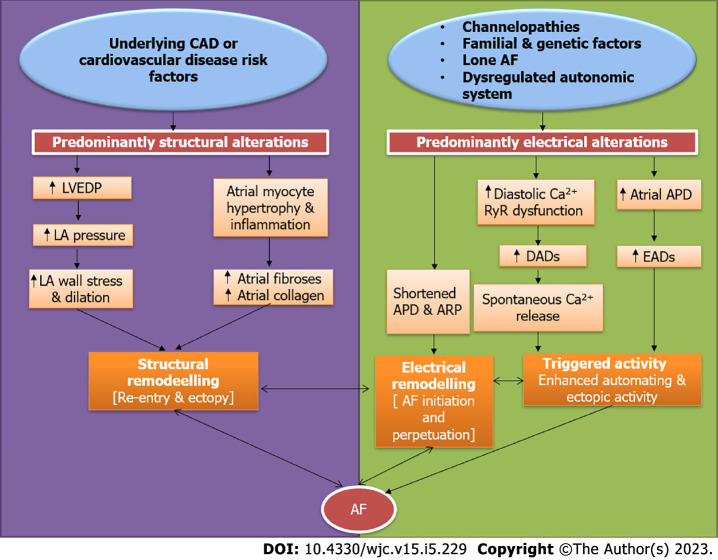
The vast majority of patients suffering from AF (> 85%) have underlying CAD or cardiovascular risk factors including hypertension, diabetes, obesity, and dyslipidemia. In less than 15% of all AF patients, none of these risk factors are present[28,29]. Most of them are relatively younger and commonly labeled as lone AF. Familial AF also contributes to a fraction of lone AF patients with well-defined chromosomal abnormalities most notably 10q22-q24[9,29]. The basic difference in the pathophysiology of AF in individuals having underlying cardiovascular risk factors and CAD predominantly is that they have structural alterations in the atrial tissue, which predispose them to develop electrical remodeling or directly lead to re-entry and ectopy culminating in AF. On the other hand, AF occurring in younger individuals without any risk factors is often attributable to the electrical remodeling as a result of abnormal Ca2+ homeostasis, dysregulated ryanodine receptors, altered action potential durations, and reduced atrial refractory period. All of these culminate in changes in ion channel function, enhanced automaticity and atrial ectopy, which is a precursor to AF[28-30]. Whatever may be the initial insult, the pathways soon converge and either of the structural or the electrical remodeling ultimately aggravates the other resulting in a vicious cycle of AF initiation and progression (Figure 4). Another important difference is in the clinical presentation and outcomes. Patients with underlying cardiovascular risk factors and CAD have less symptoms related to AF, but rather commonly present with complications related to AF including heart failure or stroke. By contrast, the risk of thromboembolism is relatively lesser in the lone AF/familial AF patients, who very often present to outpatient clinics with symptoms related to AF such as recurrent palpitations or dyspnea[28,30]. Given the aggressive disease course with accelerated atherosclerosis and thromboembolism in those with underlying cardiovascular risk factors, there is a need for the aggressive control of risk factors and institution of effective antithrombotic therapies to prevent complications.
Figure 4.
Key differences in the pathogenesis of atrial fibrillation in patients with underlying coronary artery disease or risk factors compared to those without underlying cardiovascular risk factors. AF: Atrial fibrillation; APD: Action potential duration; ARP: Absolute refractory period; CAD: Coronary artery disease; DAD: Delayed after depolarization; EAD: Early after depolarization; LA: Left atrium; LVEDP: Left ventricular end-diastolic pressure; RyR: Ryanodine receptor.
IMPLICATION ON CHA2DS2VASC SCORE AND STROKE RISK
A consistent pool of evidence points towards the increased burden of AF in those having coexistent CAD compared to those without CAD[8,11,27]. Furthermore, this increased duration and burden of AF translates into increased MACCE events in patients with coexistent CAD compared to those without CAD. Therefore, it makes sense that people with AF and coexistent CAD need better risk factor modification, pharmacological therapy for CAD, and more aggressive antithrombotic therapy to prevent adverse outcomes[6,31].
Among the components of the CHA2DS2VASc score, the symbol ‘V’ stands for vascular disease. The widely accepted determinants of this vascular disease as per the guidelines are prior myocardial infarction, peripheral artery disease, or the presence of an aortic plaque. Most of the current guidelines and online medical calculators thus do not account for CAD as a determinant of ‘V’ while calculating the CHA2DS2VASc score[32,33]. Therefore, this gives an impression that underlying CAD status (excluding past myocardial infarction) has no bearing on stroke risk as determined by the CHA2DS2VASc score.
However, in a recent, large, prospective study by Steensig et al[6], underlying CAD not only was very frequent among AF patients, but more importantly CAD was strongly associated with elevated thromboembolic risk beyond the usual components of the CHA2DS2VASc score[6]. Hence, the study made a strong case for inclusion of significant angiographically proven CAD in the ‘V’ component of the CHA2DS2VASc score to more comprehensively account for the thromboembolic risk in a given individual with AF. Indeed, this made a turning point in the approach to managing AF patients and the same was reflected in the European Society of Cardiology 2020 AF guidelines. For the first time, angiographically proven CAD was included as a determinant of in the ‘V’ in the CHA2DS2VASc score[34]. Since then, the inclusion of significant CAD has gained acceptance among practicing cardiologists as evidenced by a recent survey by the European Heart Rhythm Association, wherein 79% of the respondents were aware of the inclusion of significant CAD and employed the same in their practice[35].
A recent study by Shi et al[36] shed new insights into the stroke risk in AF patients. They concluded that among AF patients with coexistent CAD, the stroke risk was not dependent on AF but on the atherosclerotic risk factors and the presence of CAD. They made a strong case for aggressive risk factor modification in particularly underlying CAD for stroke reduction in AF patients[36].
CLINICAL IMPACT OF UNDERLYING CAD ON AF
Recent evidence supports the close association of AF and CAD. Not only does underlying CAD increase the odds of developing AF but it also has significant therapeutic and clinical implications. Consistent literature points towards increased MACCE in AF patients, who have underlying CAD compared to those without underlying CAD. Furthermore, complexity in administering appropriate antithrombotic regimen is a challenge and it predisposes an individual to increased minor and major bleeding events. Hence, given the significant therapeutic and prognostic implications of CAD on AF, a more holistic and balanced approach is needed while managing the two diseases, as it is impractical to treat either one in isolation. Table 1 highlights the prominent studies over the last three decades, which have analyzed the clinical impact of underlying CAD in AF patients[6,36-44]. Consistently, underlying CAD in AF patients has been shown to correlate positively with worse overall outcomes.
Table 1.
Prominent studies over the last three decades highlighting the clinical impact of underlying coronary artery disease in patients suffering from atrial fibrillation
|
Ref.
|
Year
|
Type of study
|
Number of patients
|
Principal findings and comment
|
| Petersen et al[37] | 1990 | Double blind RCT | 516 | Active angina was the only independent predictor of stroke on multivariate analysis [OR of 3.3 (95%CI: 1.3-8.9, P = 0.02)] |
| Ezekowitz et al[38] | 1995 | RCT | 516 | Active angina was an independent predictor of silent brain infarctions (15% vs 5% in those without angina; P = 0.02) |
| Van Walraven et al[39] | 2003 | Metanalysis of 6 RCTs | 2501 | Observed rate of stroke or TIAs was 3-fold higher in group with history of angina (5.6 vs 1.4 events/100 patient years; P = 0.002) |
| Goto et al[40] | 2008 | Observational cohort study | 63589 | MACCE events were consistently higher at 12 mo in AF patients with concomitant CAD compared to those without CAD (19.70 vs 14.52; P < 0.05) |
| Olesen et al[41] | 2012 | Registry based cohort study | 87202 | Stroke risk significantly higher in AF patients who had underlying CAD or past history of MI [HR of 1.14 (1.03-1.27)] |
| Rasmussen et al[42] | 2011 | Observational cohort study | 3315 | Risk of stroke or death significantly higher among those with underlying CAD [HR of 1.99 (1.46-2.72)] |
| Anandasundaram et al[43] | 2013 | Systematic review of 19 observational studies | 6465 | Atherosclerotic vascular disease was a significant independent predictor of stroke, thromboembolism and mortality in AF patients (P < 0.05) |
| Steensig et al[44] | 2018 | Prospective cohort study | 12690 | CAD was independently associated with increased risk of ischemic stroke in AF patients. Concomitant CAD increased stroke risk by 29% compared to AF patients without CAD [crude IRR of 1.62; (1.41-1.87)] |
| Steensig et al[6] | 2018 | Observational cohort study | 96430 | CAD was an independent predictor of composite endpoints [adjusted IRR, 1.25; (1.06-1.47)] over and above the usual components of vascular disease in CHA2DS2VASC score |
| Shi et al[36] | 2021 | Observational cohort study | 2335 | Risk of stroke was more dependent on underlying atherosclerotic risk factors than AF per say (P < 0.001) |
AF: Atrial fibrillation; CAD: Coronary artery disease; CI: Confidence interval; HR: Hazard ratio; IRR: Incidence rate ratio; MACCE: Major adverse cardio-cerebro vascular event; MI: Myocardial infarction; OR: Odds ratio; RCT: Randomized control trial; TIA: Transient ischemic attack.
“COMBINED APPROACH” TO REDUCING THE BURDEN OF THE TWO DISEASES
A recent article by Fanaroff et al[27] and the accompanying editorial nicely summarize the impact of coexistent AF and CAD on various clinical endpoints[27,45]. The main theme of the paper was the heightened thrombogenicity when the two occur together and authors concluded that the downstream risk of recurrent ACS and percutaneous coronary intervention (PCI) was extremely high in these group of patients compared to when they occurred in isolation. While they focused on only one and a very important aspect of this relationship, others have gone beyond the antithrombotic therapy. Another very relevant aspect is the enhanced atherogenicity throughout the systemic vasculature, which has been well documented in literature and elaborated upon in this review. The coexistence of the two sets in motion a vicious cycle that culminates in accelerated atherosclerosis and its various clinical manifestations[9,28,30]. Besides the increased thrombogenicity and atherogenicity conferred as a result of the coexistence of the two diseases, there is a direct relationship of one with the other disease. Such that, one disease can directly lead to the other and vice versa (Figures 2 and 3). Hence, targeting and breaking the common links between the two makes sense and should be considered in any individual suffering from either of the two diseases (Figure 5).
Figure 5.
Vicious cycle between coronary artery disease and atrial fibrillation that culminates in a positive feedback as a result of the connections as highlighted in the orange boxes. Strategies to break this cycle are also depicted in the green ovals. AF: Atrial fibrillation; BP: Blood pressure; CAD: Coronary artery disease; HR: Heart rate.
THERAPEUTIC STRATEGIES FOR DISRUPTING THE VICIOUS CYCLE
Similar to all cardiovascular diseases, the prevention starts with risk factor control and modification right at the primary care level. Controlling the most commonly implicated risk factors including physical activity, obesity, dietary modifications with reduced intake of sweetened foods and salt, smoking cessation, blood pressure control, and management of dyslipidemia and blood sugars when altered leads to a reduction of both CAD and AF[9,11]. The optimal control of these risk factors markedly reduces ones odds of developing CAD and AF by inhibiting common initiating pathways and weakening the links between them two (Figure 5).
When one of the two diseases is diagnosed in a given individual, every attempt should be made to unmask the other disease as very often the two are associated. Coexistent CAD has been reported in more than half of AF patients in various studies[5-7,46]. Thus, diagnosing the concomitant CAD by invasive or noninvasive seems logical. This translates into optimal management of not only the masked CAD and in reducing the burden of AF but also predicts an individual’s thromboembolic risk and guides optimal antithrombotic regimen[6,27]. Similarly, in those with CAD and other risk factors, the occurrence of MACCE events including stroke and heart failure should be followed by active surveillance for paroxysmal or persistent AF by appropriate rhythm monitoring tools. Unmasking paroxysmal AF guides institution of oral anticoagulants which leads to significant reduction of not only thromboembolic risk but also myocardial infarction among CAD patients.
Besides primary prevention, in those with established CAD and/or AF, the key to improve outcomes is simultaneous and optimal control of both the disease. Accordingly, given the intricate relationship between the two, it is impractical to treat the two in isolation. Most therapies that reduce the burden of either of these diseases, invariably also modifies and reduces the burden of the other disease. For example, statins that are used in CAD, have been shown to reduce the incidence and burden of AF[47]. Also, therapies aimed at reducing the burden of CAD including PCI or bypass graft surgery, have shown to significantly reduce the burden of concomitant AF and improve morbidity and mortality. Likewise, therapies such as rate control in AF patients using beta blockers or calcium channel blockers also significantly reduce coronary ischemia and myocardial oxygen uptake[48].
SPECIFIC THERAPIES
Antithrombotic agents
Antithrombotic agents encompass both antiplatelet and oral anticoagulants. Both CAD and AF are characterized by heightened thrombogenicity in the blood and resultant ischemic events. This is logarithmical increase in this thrombogenicity when the two coexist. To further complicate clinical decision making, there is an increased risk of bleeding as well attributable to these antithrombotic drugs. Balancing ischemic and bleeding risk in a given patient remains the top priority and necessitates adherence to clinical practicing guidelines.
The choice of antithrombotic agents in coexistent CAD and AF depends upon the clinical status of the underlying CAD. In patients suffering from CCS and AF, the consensus is towards the use of oral anticoagulants alone, preferably using the newer oral anticoagulants (NOACs). Recent research has shown that NOACs alone fair comparably to the combination of NOACs and aspirin but with the advantage of significantly lower risk of bleeding.
The decision making in AF patients with ACS and those undergoing PCI and stenting is however complex. In patients with ACS the recommendations are combining a P2Y12 antiplatelet agent with an oral anticoagulant (preferably NOAC over vitamin K analogues) for at least 6-12 mo after ACS and then continuing only oral anticoagulant beyond 1 year. In those undergoing PCI, the guidelines recommend triple antithrombotic therapy including aspirin, P2Y12 agent and a NOAC for the 1st month following PCI, followed by dual therapy with a P2Y12 agent and NOAC for 6-12 mo and continuing only a NOAC in most patients beyond the 1st year. However, despite the evidence and clear guidelines only a minority of AF and CAD patients receive optimal antithrombotic therapy largely attributable to the gaps in knowledge, fear of bleeding or physician preference rendering these patients at high risk of recurrent ischemic events[27,49,50].
Statins
Statins have emerged as one of the most important and first-line therapy for prevention and treatment of CAD. Besides its lipid-lowering effects, it has pleiotropic effects on the form of reduction in inflammation in the atherosclerotic plaques and improving plaque stability. Recent studies have shown that the early initiation of statin therapy in ACS patients help in reducing the incidence of atrial and ventricular arrythmias[47,51]. These beneficial actions are in part attributable to the improved autonomic control and improved myocardial stability. A large recent metanalysis has shown that prior statin use markedly reduced the incidence of new-onset AF after admission for ACS[47]. Hence, early statin use and adequate lipid control are essential for reducing AF burden among CAD patients.
Rate controlling and antianginal agents
Tachycardia in AF predisposes patients with underlying CAD to recurrent myocardial ischemia due to increased myocardial oxygen consumption and reduced diastolic coronary perfusion at higher heart rates. This not only translates into worse symptoms but roughly doubles the risk of ACS in this population. Hence, rate control is the initial and most crucial step in managing people with both CAD and AF. Beta blockers and nondihydropyridine calcium channel blockers are the preferred agents in this regard and the resting target heart rate is less than 110/min[9,48]. Ivabradine is ineffective in controlling heart rates in AF patients and on the contrary may even aggravate AF as was seen in the SIGNIFY trial and a recent meta-analysis[52,53]. Hence, it should be avoided in AF. Digoxin, although an effective drug in controlling the heart rates in AF patients especially those with left ventricular dysfunction, is best avoided in patients with CAD for the fear of predisposition to arrythmias and worsening myocardial ischemia due to increased myocardial oxygen consumption[48].
Among the choice of antianginal agents in patients symptomatic despite adequate rate control, ranolazine is preferred among the second-line drugs, as it prevents the automaticity in atrial tissue by suppressing diastolic depolarization and atrial tissue excitability in addition to suppressing the early and delayed after depolarizations. All of this results in the increased initiation and progression of AF. Moreover ranolazine use is tied to better rhythm control in AF patients in a recent meta-analysis[54,55]. Trimetazidine is a second-line antianginal used especially in those with underlying left ventricular dysfunction. It largely has a neutral effect on underlying AF and can be used as an add-on therapy in those with ischemic cardiomyopathy and AF. Limited data have suggested that favorable effects on P-wave duration and dispersion may help reduce the incidence of AF in these subgroup of patients[56]. The use of nitrate and nicorandil in AF should be avoided as these have been tied with increased incidence and aggravation of underlying AF in CAD patients[48].
Early rhythm control strategy
Early rhythm control strategy preferably with catheter ablation has been increasingly realized as an effective means of reducing the overall MACCE events in patients suffering from AF[57-59]. The benefit is most in those with high comorbidly burden and in those with a recent diagnosis of AF. There has been a clear trend in the superiority of rhythm control compared to rate control in recent years largely attributable to the incremental benefit of early rhythm over rate control alone in terms of improved overall symptoms and quality of life scores and reduced heart failure hospitalizations, stroke, dementia, and overall cardiovascular death[57,58]. This has reflected in increasing recommendations for catheter ablations in multiple subsets of patients including those with underlying CAD. Since AF is common in patients with underlying CAD and high comorbidity burden, all attempts should be made to diagnose it early and accordingly if symptoms are not controlled despite initial medical therapy and rate control, catheter ablation should be considered.
Targeting endothelial dysfunction
Robust evidence points towards the central role of endothelial dysfunction in CAD initiation and progression. Further, endothelial dysfunction now is increasingly realized as an important mediator in AF pathogenesis as well[60]. Often it coexists with other cardiovascular comorbidity such as diabetes, hypertension, dyslipidemia, and obesity. Decreased expression of nitric oxide, inflammation, increased oxidate stress, increased apoptosis, and vascular remodeling all contribute to endothelial dysfunction at the cellular level. Endothelial dysfunction as diagnosed by flow-mediated vasodilation often correlates with increased systemic vascular complications and poor outcomes[61]. Endothelial dysfunction is a dynamic thing and is reversible to large extent with appropriate intervention. At present, the only therapy to improve endothelial dysfunction includes aggressive risk factor modification including smoking cessation, appropriate blood pressure and blood glucose control, weight reduction, and exercise. Pharmacological therapies including antithrombotic therapies and statins also have shown incremental benefit in addition to lifestyle intervention. Other pharmacological agents including calcium channel blockers, angiotensin inhibitors, antioxidant agents, betablockers, phosphodiesterase inhibitors, nicorandil, ivabradine, and l-arginine have also shown some benefit in small studies but it is yet early stages to comment on the role of these agents in improving endothelial dysfunction in clinical practice[9,60,61].
Therapies targeting inflammation
Inflammation is implicated in pathogenesis of both CAD and AF. The testimony of the same lies in the fact that many antiinflammatory drugs have shown incremental benefit in reducing the incidence and burden of either of the two diseases. While evidence is more robust for its positive impact in CAD, data are emerging on its role in AF patients[62,63]. Two large randomized studies have already shown the positive impact of colchicine and canakinumab in reducing MACCE events in CAD patients attributable to decreased inflammation[64,65]. On the other hand emerging evidence shows that therapies targeting inflammation indeed prevent the occurrence or decrease the recurrences of AF in CAD patient. Recent studies have shown that colchicine or corticosteroids administration after catheter ablation can help reduce recurrence of AF[63].
Effect of diabetes and antidiabetics drugs on AF and CAD
Diabetes remains one of the largest independent risk factors for development of atherosclerosis. Approximately one-third of all patients suffering from diabetes have concomitant CAD, which remains the leading cause of morbidity and mortality in the diabetic population[66]. Recent evidence points to the excess prevalence of AF in diabetic population, independent of other cardiovascular risk factors[67,68]. Furthermore, patients with concomitant AF and diabetes have worse clinical outcomes including excess stroke, dementia, and heart failure compared to AF in the absence of diabetes[67,69]. Diabetes confers enhanced systemic vascular atherogenicity and thrombogenicity, which in part is driven by endothelial dysfunction and inflammation, a pathogenic process very similar to both AF and CAD. The major contributors to this pathogenesis include the direct glucose and free fatty acid toxicity at the cellular levels, which results in excess of reactive oxygen species, advanced glycation end-products, upregulation of the polyol, hexosamine, and protein kinase C pathways. This results in dysregulated cellular metabolism and mitochondrial function, which are essential for normal endothelial function and its antiinflammatory and antithrombotic properties[67,68]. As such, this relationship is very relevant while managing patients with AF and/or CAD. Naturally, there is a desire to use antidiabetic drugs, which help improve the burden of these diseases. Table 2 illustrates the prominent effects of various classes of antidiabetic drugs on AF and CAD. Expectedly, the antidiabetic drugs, which improve the clinical endpoints of either CAD or AF, are expected to confer a beneficial effect on the other disease as well. Overall, antidiabetic drugs that have consistently shown incremental benefit in reducing burden of either AF and CAD include sodium-glucose cotransporter-2 inhibitors, dipeptidyl peptidase-4 inhibitors, and metformin. Accordingly, we believe that these agents should preferentially be used during institution of antidiabetic therapy in these patients ahead of agents, which have neutral or harmful effects on either of the two diseases (sulfonylureas, thiazolidinediones)[68,70].
Table 2.
Impact of various antidiabetic agents on the burden of atrial fibrillation and coronary artery disease and their surrogate endpoints
|
Antidiabetic drug class
|
Impact on AF burden/ surrogate end points
|
Impact on CAD burden/ surrogate end points
|
| Insulin[71] | Increased (↑) | Neutral or increased (-/↑) |
| Metformin[72] | Reduced (↓) | Reduced (↓) |
| Sulfonylureas[71] | Neutral (-/↑) | Increased (↑↑) |
| Thiazolidinediones[73] | Reduced or neutral (-/↓) | Increased (↑↑) |
| DPP-4 inhibitors[74] | Reduced (-/↓) | Reduced (↓) |
| GLP-1 receptor agonists[75] | Neutral or slightly increased (-/↑) | Reduced (↓↓) |
| SGLT-2 inhibitors[76] | Reduced (↓↓) | Reduced (↓↓↓) |
AF: Atrial fibrillation; CAD: Coronary artery disease; DPP-4: Dipeptidyl peptidase-4; GLP-1: Glucagon-like peptide 1; SGLT-2: Sodium-glucose cotransporter-2.
CONCLUSION
The relationship between AF and CAD is complex and the two are intricately related at the pathophysiological level. The two diseases share common risk factors and pathogenesis and often culminate in a vicious cycle. Hence, it is impractical to treat them in isolation. The worsening of one is invariably accompanied by accelerated progression of the other disease as well. Accordingly, we share the implications of this relationship in diagnoses and management of the two diseases. In this review, we discuss the key strategies to break the cycle and highlight the recent, evidence-based therapeutic options to break the common links between the two and reduce morbidity and mortality.
Footnotes
Conflict-of-interest statement: All authors have no conflicts of interest to declare.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Cardiology, 3445007; European society of Cardiology, 1036629.
Peer-review started: February 4, 2023
First decision: February 20, 2023
Article in press: May 6, 2023
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Berezin AE, Ukraine; Patoulias D, Greece S-Editor: Li L L-Editor: Filipodia P-Editor: Yu HG
Contributor Information
Akash Batta, Department of Cardiology, Dayanand Medical College and Hospital, Ludhiana 141001, Punjab, India.
Juniali Hatwal, Department of Internal Medicine, Post Graduate Institute of Medical Education & Research, Chandigarh 160012, India.
Akshey Batta, Department of Medicine and Surgery, Sohana Multi Super Specialty Hospital, Mohali 160062, Punjab, India. akashbatta02@gmail.com.
Samman Verma, Department of Cardiology, Post Graduate Institute of Medical Education & Research, Chandigarh 160012, India.
Yash Paul Sharma, Department of Cardiology, Post Graduate Institute of Medical Education & Research, Chandigarh 160012, India.
References
- 1.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol . 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weng LC, Preis SR, Hulme OL, Larson MG, Choi SH, Wang B, Trinquart L, McManus DD, Staerk L, Lin H, Lunetta KL, Ellinor PT, Benjamin EJ, Lubitz SA. Genetic Predisposition, Clinical Risk Factor Burden, and Lifetime Risk of Atrial Fibrillation. Circulation . 2018;137:1027–1038. doi: 10.1161/CIRCULATIONAHA.117.031431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kornej J, Henger S, Seewöster T, Teren A, Burkhardt R, Thiele H, Thiery J, Scholz M. Prevalence of atrial fibrillation dependent on coronary artery status: Insights from the LIFE-Heart Study. Clin Cardiol . 2020;43:1616–1623. doi: 10.1002/clc.23490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan T, Zhu S, Xie C, Zhu M, Weng F, Wang C, Guo C. Coronary Artery Disease and Atrial Fibrillation: A Bidirectional Mendelian Randomization Study. J Cardiovasc Dev Dis . 2022;9 doi: 10.3390/jcdd9030069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma YP, Batta A, Makkar K, Hatwal J, A Gawalkar A, Kaur N, Malhi TS, Kasinadhuni G, Gupta H, Panda P, Barwad P. Angiographic profile and outcomes in persistent non-valvular atrial fibrillation: A study from tertiary care center in North India. Indian Heart J . 2022;74:7–12. doi: 10.1016/j.ihj.2021.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steensig K, Olesen KKW, Thim T, Nielsen JC, Jensen SE, Jensen LO, Kristensen SD, Bøtker HE, Lip GYH, Maeng M. Should the Presence or Extent of Coronary Artery Disease be Quantified in the CHA2DS2-VASc Score in Atrial Fibrillation? A Report from the Western Denmark Heart Registry. Thromb Haemost . 2018;118:2162–2170. doi: 10.1055/s-0038-1675401. [DOI] [PubMed] [Google Scholar]
- 7.Nucifora G, Schuijf JD, Tops LF, van Werkhoven JM, Kajander S, Jukema JW, Schreur JH, Heijenbrok MW, Trines SA, Gaemperli O, Turta O, Kaufmann PA, Knuuti J, Schalij MJ, Bax JJ. Prevalence of coronary artery disease assessed by multislice computed tomography coronary angiography in patients with paroxysmal or persistent atrial fibrillation. Circ Cardiovasc Imaging . 2009;2:100–106. doi: 10.1161/CIRCIMAGING.108.795328. [DOI] [PubMed] [Google Scholar]
- 8.Michniewicz E, Mlodawska E, Lopatowska P, Tomaszuk-Kazberuk A, Malyszko J. Patients with atrial fibrillation and coronary artery disease - Double trouble. Adv Med Sci . 2018;63:30–35. doi: 10.1016/j.advms.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Liang F, Wang Y. Coronary heart disease and atrial fibrillation: a vicious cycle. Am J Physiol Heart Circ Physiol . 2021;320:H1–H12. doi: 10.1152/ajpheart.00702.2020. [DOI] [PubMed] [Google Scholar]
- 10.Motloch LJ, Reda S, Larbig R, Wolff A, Motloch KA, Wernly B, Granitz C, Lichtenauer M, Wolny M, Hoppe UC. Characteristics of coronary artery disease among patients with atrial fibrillation compared to patients with sinus rhythm. Hellenic J Cardiol . 2017;58:204–212. doi: 10.1016/j.hjc.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Mekhael M, Marrouche N, Hajjar AHE, Donnellan E. The relationship between atrial fibrillation and coronary artery disease: Understanding common denominators. Trends Cardiovasc Med . 2022 doi: 10.1016/j.tcm.2022.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Dixit S. Clarifying the association between atrial fibrillation and coronary artery disease. Trends Cardiovasc Med . 2022 doi: 10.1016/j.tcm.2022.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Goudis CA, Korantzopoulos P, Ntalas IV, Kallergis EM, Liu T, Ketikoglou DG. Diabetes mellitus and atrial fibrillation: Pathophysiological mechanisms and potential upstream therapies. Int J Cardiol . 2015;184:617–622. doi: 10.1016/j.ijcard.2015.03.052. [DOI] [PubMed] [Google Scholar]
- 14.Wang A, Green JB, Halperin JL, Piccini JP Sr. Atrial Fibrillation and Diabetes Mellitus: JACC Review Topic of the Week. J Am Coll Cardiol . 2019;74:1107–1115. doi: 10.1016/j.jacc.2019.07.020. [DOI] [PubMed] [Google Scholar]
- 15.Polina I, Jansen HJ, Li T, Moghtadaei M, Bohne LJ, Liu Y, Krishnaswamy P, Egom EE, Belke DD, Rafferty SA, Ezeani M, Gillis AM, Rose RA. Loss of insulin signaling may contribute to atrial fibrillation and atrial electrical remodeling in type 1 diabetes. Proc Natl Acad Sci U S A . 2020;117:7990–8000. doi: 10.1073/pnas.1914853117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verdecchia P, Angeli F, Reboldi G. Hypertension and Atrial Fibrillation: Doubts and Certainties From Basic and Clinical Studies. Circ Res . 2018;122:352–368. doi: 10.1161/CIRCRESAHA.117.311402. [DOI] [PubMed] [Google Scholar]
- 17.Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol . 2015;12:230–243. doi: 10.1038/nrcardio.2015.2. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka Y, Obata K, Ohmori T, Ishiwata K, Abe M, Hamaguchi S, Namekata I, Tanaka H. Angiotensin II Induces Automatic Activity of the Isolated Guinea Pig Pulmonary Vein Myocardium through Activation of the IP₃ Receptor and the Na⁺-Ca(2+) Exchanger. Int J Mol Sci . 2019;20 doi: 10.3390/ijms20071768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jansen HJ, Mackasey M, Moghtadaei M, Belke DD, Egom EE, Tuomi JM, Rafferty SA, Kirkby AW, Rose RA. Distinct patterns of atrial electrical and structural remodeling in angiotensin II mediated atrial fibrillation. J Mol Cell Cardiol . 2018;124:12–25. doi: 10.1016/j.yjmcc.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Zimmerman MC, Lazartigues E, Sharma RV, Davisson RL. Hypertension caused by angiotensin II infusion involves increased superoxide production in the central nervous system. Circ Res . 2004;95:210–216. doi: 10.1161/01.RES.0000135483.12297.e4. [DOI] [PubMed] [Google Scholar]
- 21.Bookani KR, Ostovaneh MR, Venkatesh BA, Sharma S, Allison M, Greenland P, Heckbert S, Wu CO, Bluemke DA, Lima J. Adiponectin, left atrial remodeling, and atrial fibrillation: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol . 2019;73:499–499. [Google Scholar]
- 22.Alexander B, MacHaalany J, Lam B, van Rooy H, Haseeb S, Kuchtaruk A, Glover B, Bayés de Luna A, Baranchuk A. Comparison of the Extent of Coronary Artery Disease in Patients With Versus Without Interatrial Block and Implications for New-Onset Atrial Fibrillation. Am J Cardiol . 2017;119:1162–1165. doi: 10.1016/j.amjcard.2016.12.032. [DOI] [PubMed] [Google Scholar]
- 23.Marcus GM, Whooley MA, Glidden DV, Pawlikowska L, Zaroff JG, Olgin JE. Interleukin-6 and atrial fibrillation in patients with coronary artery disease: data from the Heart and Soul Study. Am Heart J . 2008;155:303–309. doi: 10.1016/j.ahj.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raphael CE, Heit JA, Reeder GS, Bois MC, Maleszewski JJ, Tilbury RT, Holmes DR Jr. Coronary Embolus: An Underappreciated Cause of Acute Coronary Syndromes. JACC Cardiovasc Interv . 2018;11:172–180. doi: 10.1016/j.jcin.2017.08.057. [DOI] [PubMed] [Google Scholar]
- 25.O'Neal WT, Soliman EZ, Howard G, Howard VJ, Safford MM, Cushman M, Zakai NA. Inflammation and hemostasis in atrial fibrillation and coronary heart disease: The REasons for Geographic And Racial Differences in Stroke study. Atherosclerosis . 2015;243:192–197. doi: 10.1016/j.atherosclerosis.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garg PK, O'Neal WT, Chen LY, Loehr LR, Sotoodehnia N, Soliman EZ, Alonso A. American Heart Association's Life Simple 7 and Risk of Atrial Fibrillation in a Population Without Known Cardiovascular Disease: The ARIC (Atherosclerosis Risk in Communities) Study. J Am Heart Assoc . 2018;7 doi: 10.1161/JAHA.117.008424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fanaroff AC, Li S, Marquis-Gravel G, Giri J, Lopes RD, Piccini JP, Wang TY. Atrial Fibrillation and Coronary Artery Disease: A Long-Term Perspective on the Need for Combined Antithrombotic Therapy. Circ Cardiovasc Interv . 2021;14:e011232. doi: 10.1161/CIRCINTERVENTIONS.121.011232. [DOI] [PubMed] [Google Scholar]
- 28.Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circ Res . 2017;120:1501–1517. doi: 10.1161/CIRCRESAHA.117.309732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Markides V, Schilling RJ. Atrial fibrillation: classification, pathophysiology, mechanisms and drug treatment. Heart . 2003;89:939–943. doi: 10.1136/heart.89.8.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bizhanov KA, Аbzaliyev KB, Baimbetov AK, Sarsenbayeva AB, Lyan E. Atrial fibrillation: Epidemiology, pathophysiology, and clinical complications (literature review) J Cardiovasc Electrophysiol . 2023;34:153–165. doi: 10.1111/jce.15759. [DOI] [PubMed] [Google Scholar]
- 31.Guo Y, Wang Y, Li X, Shan Z, Shi X, Xi G, Lip GYH ChiOTEAF Registry Investigators. Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry: protocol for a prospective, observational nationwide cohort study. BMJ Open . 2018;8:e020191. doi: 10.1136/bmjopen-2017-020191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation . 2019;140:e125–e151. doi: 10.1161/CIR.0000000000000665. [DOI] [PubMed] [Google Scholar]
- 33.Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P. [2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS] Kardiol Pol . 2016;74:1359–1469. doi: 10.5603/KP.2016.0172. [DOI] [PubMed] [Google Scholar]
- 34.Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL. Corrigendum to: 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J . 2021;42:4194. doi: 10.1093/eurheartj/ehab648. [DOI] [PubMed] [Google Scholar]
- 35.Zhang J, Lenarczyk R, Marin F, Malaczynska-Rajpold K, Kosiuk J, Doehner W, Van Gelder IC, Lee G, Hendriks JM, Lip GYH, Potpara TS. The interpretation of CHA2DS2-VASc score components in clinical practice: a joint survey by the European Heart Rhythm Association (EHRA) Scientific Initiatives Committee, the EHRA Young Electrophysiologists, the Association of Cardiovascular Nursing and Allied Professionals, and the European Society of Cardiology Council on Stroke. Europace . 2021;23:314–322. doi: 10.1093/europace/euaa358. [DOI] [PubMed] [Google Scholar]
- 36.Shi B, Liu D, Wang Q, Geng X, Hou Q, Gu G, Xie R, Cui W. Relationship among atrial fibrillation, the CHA(2)DS(2)-VASc score and ischaemic stroke in patients with coronary artery disease: a propensity score matching study in Hebei, China. BMC Cardiovasc Disord . 2021;21:474. doi: 10.1186/s12872-021-02276-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Petersen P, Kastrup J, Helweg-Larsen S, Boysen G, Godtfredsen J. Risk factors for thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Arch Intern Med . 1990;150:819–821. [PubMed] [Google Scholar]
- 38.Ezekowitz MD, James KE, Nazarian SM, Davenport J, Broderick JP, Gupta SR, Thadani V, Meyer ML, Bridgers SL. Silent cerebral infarction in patients with nonrheumatic atrial fibrillation. The Veterans Affairs Stroke Prevention in Nonrheumatic Atrial Fibrillation Investigators. Circulation . 1995;92:2178–2182. doi: 10.1161/01.cir.92.8.2178. [DOI] [PubMed] [Google Scholar]
- 39.van Walraven C, Hart RG, Wells GA, Petersen P, Koudstaal PJ, Gullov AL, Hellemons BS, Koefed BG, Laupacis A. A clinical prediction rule to identify patients with atrial fibrillation and a low risk for stroke while taking aspirin. Arch Intern Med . 2003;163:936–943. doi: 10.1001/archinte.163.8.936. [DOI] [PubMed] [Google Scholar]
- 40.Goto S, Bhatt DL, Röther J, Alberts M, Hill MD, Ikeda Y, Uchiyama S, D'Agostino R, Ohman EM, Liau CS, Hirsch AT, Mas JL, Wilson PW, Corbalán R, Aichner F, Steg PG REACH Registry Investigators. Prevalence, clinical profile, and cardiovascular outcomes of atrial fibrillation patients with atherothrombosis. Am Heart J . 2008;156:855–863, 863.e2. doi: 10.1016/j.ahj.2008.06.029. [DOI] [PubMed] [Google Scholar]
- 41.Olesen JB, Lip GY, Lane DA, Køber L, Hansen ML, Karasoy D, Hansen CM, Gislason GH, Torp-Pedersen C. Vascular disease and stroke risk in atrial fibrillation: a nationwide cohort study. Am J Med . 2012;125:826.e13–826.e23. doi: 10.1016/j.amjmed.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 42.Rasmussen LH, Larsen TB, Due KM, Tjønneland A, Overvad K, Lip GY. Impact of vascular disease in predicting stroke and death in patients with atrial fibrillation: the Danish Diet, Cancer and Health cohort study. J Thromb Haemost . 2011;9:1301–1307. doi: 10.1111/j.1538-7836.2011.04308.x. [DOI] [PubMed] [Google Scholar]
- 43.Anandasundaram B, Lane DA, Apostolakis S, Lip GY. The impact of atherosclerotic vascular disease in predicting a stroke, thromboembolism and mortality in atrial fibrillation patients: a systematic review. J Thromb Haemost . 2013;11:975–987. doi: 10.1111/jth.12177. [DOI] [PubMed] [Google Scholar]
- 44.Steensig K, Olesen KKW, Thim T, Nielsen JC, Jensen SE, Jensen LO, Kristensen SD, Bøtker HE, Lip GYH, Maeng M. CAD Is an Independent Risk Factor for Stroke Among Patients With Atrial Fibrillation. J Am Coll Cardiol . 2018;72:2540–2542. doi: 10.1016/j.jacc.2018.08.1046. [DOI] [PubMed] [Google Scholar]
- 45.Brener SJ. What Happened to the Cycle of Knowledge? Circ Cardiovasc Interv . 2021;14:e011549. doi: 10.1161/CIRCINTERVENTIONS.121.011549. [DOI] [PubMed] [Google Scholar]
- 46.Kotalczyk A, Guo Y, Fawzy AM, Wang Y, Lip GYH. Outcomes in elderly Chinese patients with atrial fibrillation and coronary artery disease. A report from the Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry. J Arrhythm . 2022;38:580–588. doi: 10.1002/joa3.12744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wibawa K, Dewangga R, Nastiti KS, Syah PA, Suhendiwijaya S, Ariffudin Y. Prior statin use and the incidence of in-hospital arrhythmia in acute coronary syndrome: A systematic review and meta-analysis. Indian Heart J . 2023;75:9–16. doi: 10.1016/j.ihj.2023.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Manolis AJ, Poulimenos LE, Ambrosio G, Kallistratos MS, Lopez-Sendon J, Dechend R, Mancia G, Camm AJ. Medical treatment of stable angina: A tailored therapeutic approach. Int J Cardiol . 2016;220:445–453. doi: 10.1016/j.ijcard.2016.06.150. [DOI] [PubMed] [Google Scholar]
- 49.Matsuzawa Y, Kimura K, Yasuda S, Kaikita K, Akao M, Ako J, Matoba T, Nakamura M, Miyauchi K, Hagiwara N, Hirayama A, Matsui K, Ogawa H AFIRE Investigators. Antithrombotic Therapy for Atrial Fibrillation and Coronary Artery Disease in Patients With Prior Atherothrombotic Disease: A Post Hoc Analysis of the AFIRE Trial. J Am Heart Assoc . 2021;10:e020907. doi: 10.1161/JAHA.121.020907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Angiolillo DJ, Bhatt DL, Cannon CP, Eikelboom JW, Gibson CM, Goodman SG, Granger CB, Holmes DR, Lopes RD, Mehran R, Moliterno DJ, Price MJ, Saw J, Tanguay JF, Faxon DP. Antithrombotic Therapy in Patients With Atrial Fibrillation Treated With Oral Anticoagulation Undergoing Percutaneous Coronary Intervention: A North American Perspective: 2021 Update. Circulation . 2021;143:583–596. doi: 10.1161/CIRCULATIONAHA.120.050438. [DOI] [PubMed] [Google Scholar]
- 51.Zagidullin NS, Michels G, Zagidullin SZ. Statins and their antiarrhythmic activity. Cardiovasc Ther Prev . 2023;6:116–121. [Google Scholar]
- 52.Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R SIGNIFY Investigators. Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med . 2014;371:1091–1099. doi: 10.1056/NEJMoa1406430. [DOI] [PubMed] [Google Scholar]
- 53.Martin RI, Pogoryelova O, Koref MS, Bourke JP, Teare MD, Keavney BD. Atrial fibrillation associated with ivabradine treatment: meta-analysis of randomised controlled trials. Heart . 2014;100:1506–1510. doi: 10.1136/heartjnl-2014-305482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Miles RH, Passman R, Murdock DK. Comparison of effectiveness and safety of ranolazine versus amiodarone for preventing atrial fibrillation after coronary artery bypass grafting. Am J Cardiol . 2011;108:673–676. doi: 10.1016/j.amjcard.2011.04.017. [DOI] [PubMed] [Google Scholar]
- 55.Guerra F, Romandini A, Barbarossa A, Belardinelli L, Capucci A. Ranolazine for rhythm control in atrial fibrillation: A systematic review and meta-analysis. Int J Cardiol . 2017;227:284–291. doi: 10.1016/j.ijcard.2016.11.103. [DOI] [PubMed] [Google Scholar]
- 56.Gunes Y, Tuncer M, Guntekin U, Akdag S, Gumrukcuoglu HA. The effects of trimetazidine on p-wave duration and dispersion in heart failure patients. Pacing Clin Electrophysiol . 2009;32:239–244. doi: 10.1111/j.1540-8159.2008.02208.x. [DOI] [PubMed] [Google Scholar]
- 57.Camm AJ, Naccarelli GV, Mittal S, Crijns HJGM, Hohnloser SH, Ma CS, Natale A, Turakhia MP, Kirchhof P. The Increasing Role of Rhythm Control in Patients With Atrial Fibrillation: JACC State-of-the-Art Review. J Am Coll Cardiol . 2022;79:1932–1948. doi: 10.1016/j.jacc.2022.03.337. [DOI] [PubMed] [Google Scholar]
- 58.Rillig A, Borof K, Breithardt G, Camm AJ, Crijns HJGM, Goette A, Kuck KH, Metzner A, Vardas P, Vettorazzi E, Wegscheider K, Zapf A, Kirchhof P. Early Rhythm Control in Patients With Atrial Fibrillation and High Comorbidity Burden. Circulation . 2022;146:836–847. doi: 10.1161/CIRCULATIONAHA.122.060274. [DOI] [PubMed] [Google Scholar]
- 59.Kim D, Yang PS, Joung B. Optimal Rhythm Control Strategy in Patients With Atrial Fibrillation. Korean Circ J . 2022;52:496–512. doi: 10.4070/kcj.2022.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Khan AA, Thomas GN, Lip GYH, Shantsila A. Endothelial function in patients with atrial fibrillation. Ann Med . 2020;52:1–11. doi: 10.1080/07853890.2019.1711158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Su JB. Vascular endothelial dysfunction and pharmacological treatment. World J Cardiol . 2015;7:719–741. doi: 10.4330/wjc.v7.i11.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Varghese B, Feldman DI, Chew C, Valilis E, Blumenthal RS, Sharma G, Calkins H. Inflammation, atrial fibrillation, and the potential role for colchicine therapy. Heart Rhythm O2 . 2021;2:298–303. doi: 10.1016/j.hroo.2021.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou X, Dudley SC Jr. Evidence for Inflammation as a Driver of Atrial Fibrillation. Front Cardiovasc Med . 2020;7:62. doi: 10.3389/fcvm.2020.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tardif JC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, Pinto FJ, Ibrahim R, Gamra H, Kiwan GS, Berry C, López-Sendón J, Ostadal P, Koenig W, Angoulvant D, Grégoire JC, Lavoie MA, Dubé MP, Rhainds D, Provencher M, Blondeau L, Orfanos A, L'Allier PL, Guertin MC, Roubille F. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N Engl J Med . 2019;381:2497–2505. doi: 10.1056/NEJMoa1912388. [DOI] [PubMed] [Google Scholar]
- 65.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ CANTOS Trial Group. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med . 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 66.Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol . 2018;17:83. doi: 10.1186/s12933-018-0728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bano A, Rodondi N, Beer JH, Moschovitis G, Kobza R, Aeschbacher S, Baretella O, Muka T, Stettler C, Franco OH, Conte G, Sticherling C, Zuern CS, Conen D, Kühne M, Osswald S, Roten L, Reichlin T of the Swiss‐Investigators. Association of Diabetes With Atrial Fibrillation Phenotype and Cardiac and Neurological Comorbidities: Insights From the Swiss-AF Study. J Am Heart Assoc . 2021;10:e021800. doi: 10.1161/JAHA.121.021800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee TW, Lee TI, Lin YK, Chen YC, Kao YH, Chen YJ. Effect of antidiabetic drugs on the risk of atrial fibrillation: mechanistic insights from clinical evidence and translational studies. Cell Mol Life Sci . 2021;78:923–934. doi: 10.1007/s00018-020-03648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Batta A, Sharma YP, Hatwal J, Panda P, Kumar BGV, Bhogal S. Predictors of dementia amongst newly diagnosed non-valvular atrial fibrillation patients. Indian Heart J . 2022;74:505–509. doi: 10.1016/j.ihj.2022.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lăcătușu CM, Grigorescu ED, Stătescu C, Sascău RA, Onofriescu A, Mihai BM. Association of Antihyperglycemic Therapy with Risk of Atrial Fibrillation and Stroke in Diabetic Patients. Medicina (Kaunas) . 2019;55 doi: 10.3390/medicina55090592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liou YS, Yang FY, Chen HY, Jong GP. Antihyperglycemic drugs use and new-onset atrial fibrillation: A population-based nested case control study. PLoS One . 2018;13:e0197245. doi: 10.1371/journal.pone.0197245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chang SH, Wu LS, Chiou MJ, Liu JR, Yu KH, Kuo CF, Wen MS, Chen WJ, Yeh YH, See LC. Association of metformin with lower atrial fibrillation risk among patients with type 2 diabetes mellitus: a population-based dynamic cohort and in vitro studies. Cardiovasc Diabetol . 2014;13:123. doi: 10.1186/s12933-014-0123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pallisgaard JL, Lindhardt TB, Staerk L, Olesen JB, Torp-Pedersen C, Hansen ML, Gislason GH. Thiazolidinediones are associated with a decreased risk of atrial fibrillation compared with other antidiabetic treatment: a nationwide cohort study. Eur Heart J Cardiovasc Pharmacother . 2017;3:140–146. doi: 10.1093/ehjcvp/pvw036. [DOI] [PubMed] [Google Scholar]
- 74.Chang CY, Yeh YH, Chan YH, Liu JR, Chang SH, Lee HF, Wu LS, Yen KC, Kuo CT, See LC. Dipeptidyl peptidase-4 inhibitor decreases the risk of atrial fibrillation in patients with type 2 diabetes: a nationwide cohort study in Taiwan. Cardiovasc Diabetol . 2017;16:159. doi: 10.1186/s12933-017-0640-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Monami M, Nreu B, Scatena A, Giannini S, Andreozzi F, Sesti G, Mannucci E. Glucagon-like peptide-1 receptor agonists and atrial fibrillation: a systematic review and meta-analysis of randomised controlled trials. J Endocrinol Invest . 2017;40:1251–1258. doi: 10.1007/s40618-017-0698-7. [DOI] [PubMed] [Google Scholar]
- 76.Zelniker TA, Bonaca MP, Furtado RHM, Mosenzon O, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Budaj A, Kiss RG, Padilla F, Gause-Nilsson I, Langkilde AM, Raz I, Sabatine MS, Wiviott SD. Effect of Dapagliflozin on Atrial Fibrillation in Patients With Type 2 Diabetes Mellitus: Insights From the DECLARE-TIMI 58 Trial. Circulation . 2020;141:1227–1234. doi: 10.1161/CIRCULATIONAHA.119.044183. [DOI] [PubMed] [Google Scholar]