Abstract
Using data from the 2020 and 2021 cycles of the Survey on COVID-19 and Mental Health, we examined suicidal ideation among adults in Canada aged 18 to 34 years. The prevalence of suicidal ideation among adults aged 18 to 34 years was 4.2% in fall 2020 and 8.0% in spring 2021. The subgroup of adults aged 18 to 24 years had the highest prevalence of suicidal ideation, 10.7%, in spring 2021. Prevalence varied by sociodemographic characteristics and tended to be higher among people living in materially deprived areas. Suicidal ideation was strongly associated with pandemic-related stressors respondents experienced.
Keywords: surveillance, material deprivation, social deprivation, substance use, pandemic impacts, loneliness, anxiety, mental illness, coronavirus
Highlights
In spring 2021, the prevalence of suicidal ideation among young adults aged 18 to 34 years was 8.0%.
At 10.7%, the prevalence of suicidal ideation was highest in the subgroup of young adults aged 18 to 24 years, in spring 2021.
The odds of suicidal ideation were higher among young adults who were White versus racialized, born in Canada versus immigrated to Canada, living with low or middle income, with high school education or less, or living in a materially deprived area.
Pandemic-related experiences, stressful events and mental illness were strongly associated with suicidal ideation.
Introduction
As early as April 2020, mental health professionals were raising concerns about the impact of the COVID-19 pandemic on suicidality.1 Global suicide mortality rates remained unchanged or decreased fduring the first 9 to 15 months of the pandemic,2 but suicidal ideation, suicide attempts and self-harm have increased in some populations and contexts.3 In Canada, the prevalence of recent suicidal ideation among adults was 2.7% in 20194,5 and 2.4% in fall 2020,4 increasing significantly to 4.2% in spring 2021.5
Studies suggest that young adults may have been more likely than older people to experience mental health problems such as anxiety and depressive symptoms,6 loneliness,7 psychological distress8 and suicidality4,5,9 since the start of the pandemic. In Canada in 2019, the odds of young adults aged 18 to 34 years reporting suicidal ideation were 5.4 times that of adults aged 65 years or older; these comparative odds increased to 8.2 by fall 2020 and to 9.7 by spring 2021.4,5
Systematic reviews and meta-analyses identified pandemic-specific risk factors for suicidal ideation.3,10,11 Several reviews found that university students were at high risk for suicide-related behaviours, and associated risk factors included social isolation and mental illness.11-13 As the long-term mental health effects of the COVID-19 pandemic are unclear, continued surveillance is needed to inform comprehensive and effective responses to suicide risks, including among young adults.
The objectives of this paper were to (1)estimate the prevalence of suicidal ideation during the COVID-19 pandemic among young adults aged 18 to 34 years, by age subgroup; and (2) identify sociodemographic characteristics and pandemic-related stressors that may be associated with an increased risk of suicidal ideation in this population.
Methods
Data source
We analyzed cross-sectional data from the 2020 and 2021 cycles of the nationally representative, population-based Survey on COVID-19 and Mental Health (SCMH).14,15 Conducted by Statistics Canada with the Public Health Agency of Canada (PHAC), the SCMH was designed to collect data to assess the impacts of COVID-19 on adults’ mental health and well-being. The 2020 cycle was conducted from 11 September through 4 December 2020 (“fall 2020”), and the 2021 cycle from 1 February through 7 May 2021 (“spring 2021”).
The two SCMH cycles had nearly identical methodologies. The target population was individuals aged 18 years or older in the ten provinces and the three territorial capitals. A simple random sample of dwellings from each province and territorial capital was selected from the Dwelling Universe File, and a household member was sampled in each dwelling. Excluded from the survey were residents of institutions; of collective, unmailable, inactive or vacant dwellings; and of First Nations reserves; together, these groups represented less than 2% of the population of interest.
Respondents completed the SCMH voluntarily through an electronic questionnaire or a computer-assisted telephone interview. The response rate was 53.3% (14 689 responses) for the 2020 cycle and 49.3% (8032 responses) for the 2021 cycle. A total of 18 936 respondents (83.3%) agreed to share their information with PHAC. Of these respondents, 3265 were aged 18 to 34 years. After excluding 10respondents who did not answer the question about suicidal ideation, we analyzed data from the remaining 3255 respondents.
Measures
Suicidal ideation was determined with the question, “Have you seriously contemplated suicide since the COVID-19 pandemic began?” Sociodemographic factors examined were gender, age group, racialized group member, immigrant status, income tertile, area of residence, education, living alone, and social and material deprivation. The social and material deprivation index developed by the Institut national de sant publique du Qubec is a measure of social and material inequalities at the neighbourhood level, based on census dissemination areas.16,17 The material deprivation component includes measures of area-level income, education and employment; the social deprivation component refers to social ties, that is, marital status, living alone and lone-parent family status.16,17 Our analysis used the deprivation index based on the 2016 Census.
The variables for COVID-19 stressors were pandemic-related experiences; alcohol and cannabis use; concerns about violence in people’s own homes; symptoms of mental illness; ever experienced stressful events in lifetime; and work status. These variables, and the surveys, have been described in detail elsewhere.18
Analysis
We estimated the prevalence of suicidal ideation in the 2020 and 2021 SCMH separately, by gender and by age group. We then estimated the prevalence of suicidal ideation using combined data from the two cycles, by sociodemographic characteristics and pandemic-related stressors, and used logistic regressions to examine disparities of reporting suicidal ideation. We computed crude odds ratio (OR) and adjusted odds ratios (aOR) for gender, age group and survey year. All estimates were adjusted with sampling weights provided by Statistics Canada; 95% modified Clopper–Pearson confidence intervals (CI)19 were estimated using the bootstrap technique. We conducted the analyses using SAS Enterprise Guide version 7.1 (SAS Institute, Cary, NC, USA).
Results
Table 1 shows the prevalence of suicidal ideation, by gender and age group, in 2020 and 2021. For both cycles, this prevalence tended to be higher in younger age groups. In 2021, the prevalence of suicidal ideation among those aged 18 to 34 was 8.0%, with the highest prevalence (10.7%) among those aged 18 to 24. The prevalence of suicidal ideation was similar for women and men (7.8% versus 7.6%) in 2021. The seemingly higher prevalence among women in 2020 (5.2% versus 2.9% among men) was not statistically significant.
Table 1. Prevalence of suicidal ideation during the COVID-19 pandemic,a by gender and age group, population aged 18–34 years, Canada.
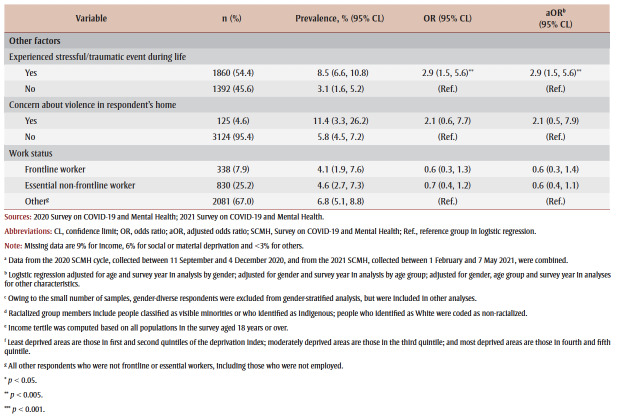
Table 2 shows the prevalence of and odds ratios for suicidal ideation among people aged 18 to 34 years, by sociodemographic characteristics and pandemic-related stressors, based on combined data from the 2020 and 2021 SCMH. The odds of suicidal ideation were significantly higher among people aged 18 to 24 years, those with low and middle income, those with lower educational attainment or those living in materially deprived areas. In contrast, the odds were significantly lower among racialized adults and immigrants to Canada. Young adults in the most materially deprived areas had almost double the odds of suicidal ideation compared with those in the least deprived areas. No significant differences were observed across levels of social deprivation.
Table 2. Prevalence and odds ratios of suicidal ideation during the COVID-19 pandemic,a by sociodemographic characteristics and pandemic-related stressors, population aged 18–34 years, Canada.
Most of the pandemic-related experiences examined were associated with higher odds of suicidal ideation, and particularly feelings of loneliness (aOR = 11.1; 95% CI: 6.1–20.2) and emotional distress (aOR= 7.7; 95% CI: 3.7–16.2). A dose–response relationship was evident; the odds of young adults with 5 or more pandemic-related experiences reporting suicidal ideation were 14 times that of the odds reported by those with 0 or 1 of these experiences.
Discussion
Using data from the 2020 and 2021 SCMH, we analyzed suicidal ideation among young adults aged 18 to 34 years in Canada. The prevalence of suicidal ideation tended to be higher in younger age groups and some sociodemographic subgroups. Pandemic-related stressors were associated with a higher prevalence of suicidal ideation.
In 2021 in Canada, the prevalence of suicidal ideation was 10.7% for young adults 18 to 24 years old; this was more than double the prevalence of suicidal ideation for adults overall, 4.2%.5 Our findings on disparities in suicidal ideation between sociodemographic groups and associations with pandemic-related stressors experienced by young adults aged 18 to 34 are consistent with those of a recent study of adults 18 years and older.18 The results also align with the findings of a United States study that reported the prevalence of seriously considering suicide in the past 30 days in June 2020 as higher among respondents aged 18 to 24 years than among older age groups, with prevalence decreasing with age.9
During the pandemic, young adults were more likely than older adults to develop anxiety and depressive symptoms6,20-22 and experience loneliness;7,23 they also had the largest increase in psychological distress over time.8 School and university closures may have played a role by restricting opportunities to form and maintain social relationships.24 Surveys conducted in Germany found a high prevalence of suicidal ideation among university students compared with before or during the early months of the pandemic.25,26 A national survey of students aged 18 to 35 years in Norway found a negative correlation between time spent in person on campus and suicidal ideation.27 Job loss could also be a factor; 15- to 24-year-olds experienced unemployment more than other age groups during the pandemic.28,29 Those living in the most deprived areas had high prevalence of suicidal ideation, which supports previous findings that the rise in suicidal ideation is most likely to occur among young people living in poverty.30
Our analysis used data derived from survey cycles with modest sample sizes, which limits the statistical power needed to detect significant differences between subgroups. In addition, the cross-sectional design does not allow for examination of causal relationships. Nevertheless, the results of this study indicate that young adults in Canada had a higher risk of suicidal ideation than older adults, and that modifiable factors, including loneliness, emotional distress and symptoms of mental illness, played important roles in increasing this risk. These findings suggest that age-specific clinical and population interventions that target key risk factors may help decrease suicidal thinking among young adults during the COVID-19 pandemic.
Acknowledgements
The editorial assistance provided by Mary Sue Devereaux is gratefully acknowledged.
Conflicts of interest
The authors have no conflicts of interest.
Authors’ contributions and statement
All authors conceived the project. LL and GC drafted the article, and all authors contributed to its revisions. LL conducted the statistical analyses and all authors interpreted the results. All authors critically reviewed every draft of the article and approved the final submission.
The content and views expressed herein are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020:468–71. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J, Gunnell D, Shin S, et al, et al. Suicide numbers during the first 9-15 months of the COVID-19 pandemic compared with pre-existing trends: an interrupted time series analysis in 33 countries. EClinicalMedicine. 2022:101573–71. doi: 10.1016/j.eclinm.2022.101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MM, Sherry SB, Hewitt PL, Stewart SH, et al. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021:113998–71. doi: 10.1016/j.psychres.2021.113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Capaldi CA, Dopko RL, et al. Suicide ideation in Canada during the COVID- 19 pandemic. Health Promot Chronic Dis Prev Can. 2021;41((11)):378–91. doi: 10.24095/hpcdp.41.11.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Pollock NJ, Contreras G, Tonmyr L, Thompson W, et al. Prevalence of suicidal ideation among adults in Canada: results of the second Survey on COVID-19 and mental health. Health Rep. 2022;33((5)):13–21. doi: 10.25318/82-003-x202200500002-eng. [DOI] [PubMed] [Google Scholar]
- Nwachukwu I, Nkire N, Shalaby R, et al, et al. COVID-19 pandemic: age-related differences in measures of stress, anxiety and depression in Canada. Int J Environ Res Public Health. 2020:6366–21. doi: 10.3390/ijerph17176366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickens CM, McDonald AJ, Marshall T, et al, et al. Loneliness in the COVID-19 pandemic: associations with age, gender and their interaction. J Psychiatr Res. 2021:103–8. doi: 10.1016/j.jpsychires.2021.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte F, et al. A longitudinal nationwide study of psychological distress during the COVID-19 pandemic in Chile. Front Psychiatry. 2022:744204–8. doi: 10.3389/fpsyt.2022.744204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler ME, Lane RI, Petrosky E, et al, et al. Mental health, substance use, and suicidal ideation during the COVID- 19 pandemic – United States, June 24-30, 2020. Czeisler ME, Lane RI, Petrosky E, et al. 2020;69((32)):1049–57. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq S, Tunmore J, Ali M, Ayub M, et al. Suicide, self-harm and suicidal ideation during COVID-19: a systematic review. Psychiatry Res. 2021:a systematic review–57. doi: 10.1016/j.psychres.2021.114228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- bano J, Cabrera MM, et al. Suicidal ideation and suicidal thoughts in university students during the COVID-19 pandemic: a systematic review. Rev Argentina de Clin Psicol. 2021;30((2)):390–405. [Google Scholar]
- Shobhana SS, Raviraj KG, et al. Global trends of suicidal thought, suicidal ideation, and self-harm during COVID- 19 pandemic: a systematic review. Egypt J Forensic Sci. 2022;12((1)):28–405. doi: 10.1186/s41935-022-00286-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira K, Lisboa JL, Dias BM, Ferreira RC, Zarzar PM, Sampaio AA, et al. Suicidal ideation among university students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Res Soc Dev. 2022:e2211426426–405. [Google Scholar]
- Statistics Canada. Ottawa(ON): Survey on COVID- 19 and Mental Health (SCMH): detailed information for September to December 2020 [Internet] Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=1283036. [Google Scholar]
- Statistics Canada. Ottawa(ON): Survey on COVID- 19 and Mental Health (SCMH): detailed information for February to May 2021 [Internet] Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=1295371. [Google Scholar]
- Gamache P, Hamel D, Blaser C, et al. Institut national de sant publique du Qubec. Quebec(QC): Material and social deprivation index: a summary [Internet] Available from: http://www.inspq.qc.ca/en/publications/2639. [Google Scholar]
- Pampalon R, Hamel D, Gamache P, Simpson A, Philibert MD, et al. Validation of a deprivation index for public health: a complex exercise illustrated by the Quebec index. Chronic Dis Inj Can. 2014;34((1)):12–22. [PubMed] [Google Scholar]
- Liu L, Pollock NJ, Contreras G, Tonmyr L, Thompson W, et al. Pandemic-related impacts and suicidal ideation among adults in Canada: a population-based cross-sectional study. Health Promot Chronic Dis Prev Can. 2022:1–14. doi: 10.24095/hpcdp.43.3.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clopper CJ, Pearson ES, et al. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26((4)):404–13. [Google Scholar]
- era D, lek T, et al. Impacts of COVID-19 pandemic on the mental health of working adults in the Czech Republic: analysis of self-report psychological data in a one year perspective. Eur J Investig Health Psychol Educ. 2021;11((3)):1061–72. doi: 10.3390/ejihpe11030079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzwiedz CL, Green MJ, Benzeval M, et al, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health. 2021:224–31. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia R, Ayling K, Chalder T, et al, et al. The prevalence, incidence, prognosis and risk factors for symptoms of depression and anxiety in a UK cohort during the COVID-19 pandemic. BJPsych Open. 2022;8((2)):e64–31. doi: 10.1192/bjo.2022.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades ME, Chatburn E, Sweeney N, et al, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. jaac. 2020;59((11)):1218–39. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner RM, Russell SJ, Croker H, et al, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4((5)):a rapid systematic review–39. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brailovskaia J, Teismann T, Friedrich S, Schneider S, Margrafa J, et al. Suicide ideation during the COVID-19 outbreak in German university students: comparison with pre-COVID 19 rates. J Affect Disord Rep. 2021 doi: 10.1016/j.jadr.2021.100228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogan-Sander E, Kohls E, Baldofski S, et al. More depressive symptoms, alcohol and drug consumption: increase in mental health symptoms among university students after one year of the COVID- 19 pandemic. Front Psychiatry. 2021:790974–39. doi: 10.3389/fpsyt.2021.790974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen B, Knapstad M, Petrie K, O’Connor R, nning KJ, Hysing M, et al. Changes in mental health problems and suicidal behaviour in students and their associations with COVID- 19-related restrictions in Norway: a national repeated cross-sectional analysis. BMJ Open. 2022:e057492–39. doi: 10.1136/bmjopen-2021-057492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development. Paris(FR): Unemployment Rates, OECD - Updated: May 2020. Available from: http://www.oecd.org/employment/unemployment-rates-oecd-update-may-2020.htm. [Google Scholar]
- Statistics Canada. Ottawa(ON): Labour force characteristics by age group, monthly, seasonally adjusted. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410028701. [Google Scholar]
- Barzilay S, Apter A, et al. Recent research advances in identification and prevention of youth suicide risk. Curr Opin Psychiatry. 2022;35((6)):395–400. doi: 10.1097/YCO.0000000000000816. [DOI] [PubMed] [Google Scholar]