ABSTRACT
BACKGROUND:
Laparoscopic appendectomy is the gold standard surgical procedure currently performed for acute appendicitis. The conversion rate is one of the main factors used to measure laparoscopic competence, being important to avoid wasting time in a laparoscopic procedure and proceed directly to open surgery.
AIMS:
To identify the main preoperative parameters associated with a higher risk of conversion in order to determine the surgical method indicated for each patient.
METHODS:
Retrospective study of patients admitted with acute appendicitis who underwent laparoscopic appendectomy. A total of 725 patients were included, of which 121 (16.7%) were converted to laparotomy.
RESULTS:
The significant factors that predicted conversion, identified by univariate and multivariate analysis, were: the presence of comorbidities (OR 3.1; 95%CI; p<0.029), appendicular perforation (OR 5.1; 95%CI; p<0.003), retrocecal appendix (OR 5.0; 95%CI; p<0.004), gangrenous appendix, presence of appendicular abscess (OR 3.6; 95%CI; p<0.023) and the presence of difficult dissection (OR 9.2; 95%CI; p<0.008).
CONCLUSIONS:
Laparoscopic appendectomy is a safe procedure to treat acute appendicitis. It is a minimally invasive surgery and has many advantages. Preoperatively, it is possible to identify predictive factors for conversion to laparotomy, and the ability to identify these reasons can aid surgeons in selecting patients who would benefit from a primary open appendectomy.
HEADINGS: Appendectomy, Laparoscopy, Conversion to open surgery, Laparotomy
RESUMO
RACIONAL:
A apendicectomia laparoscópica é o procedimento cirúrgico padrão-ouro realizado atualmente para apendicite aguda. A taxa de conversão é um dos principais fatores utilizados para medir a competência laparoscópica, e importante para evitar perda de tempo em um procedimento laparoscópico e proceder diretamente à cirurgia aberta.
OBJETIVO:
Identificar os principais parâmetros pré-operatórios associados ao maior risco de conversão para determinar o método cirúrgico indicado para cada paciente.
MÉTODOS:
Estudo retrospectivo de pacientes admitidos com apendicite aguda, submetidos a apendicectomia laparoscópica. Foram incluídos 725 pacientes, sendo que destes, 121 (16,7%) foram convertidos para laparotomia.
RESULTADOS:
Os fatores significativos que predizem a conversão, identificados por análise univariada e multivariada, foram: presença de comorbidades (OR 3,1; IC95%; p<0,029), perfuração apendicular (OR 5,1; IC95%; p<0,003), apêndice retrocecal (OR 5,0; IC95%; p<0,004), apêndice gangrenoso, presença de abscesso apendicular (OR 3,6; IC95%; p<0,023) e a presença de dissecção difícil (OR 9,2; IC95%; p<0,008).
CONCLUSÕES:
A apendicectomia laparoscópica é um procedimento seguro para tratar apendicite aguda. É uma cirurgia minimamente invasiva e tem muitas vantagens. No pré-operatório, é possível identificar os fatores preditores de conversão para laparotomia, e a capacidade de identificar essas razões pode ajudar os cirurgiões na seleção de pacientes que se beneficiariam de uma apendicectomia aberta primária.
DESCRITORES: Apendicectomia, Laparoscopia, Conversão para cirurgia aberta, Laparotomia
INTRODUCTION
Open appendectomy (OA) was considered the standard approach for acute appendicitis for a long time 7,10 . Laparoscopic appendectomy (LA) was reported for the first time in 1983, and since then it has been adopted as the gold standard for the treatment of acute appendicitis 4,9,15 . For quite some time, its advantages have been evaluated by some authors in systematic reviews or meta-analysis 15,16 . Many studies confirmed that the laparoscopic approach is a mainstream technique in acute appendicitis 3,7 . However, complicated appendicitis is considered a dilemma in their management regarding the greater demand for a high-quality experience and the fear of postoperative septic complications 15,16 . But the LA approach is moreover used in complicated patterns and rates of conversion to OA varies from 1 to 10% 6 . Therefore, conversion to OA may be the best solution in these cases 15 . A decision on which approach should be performed must be subject to preoperative criteria 1,10 .
We aimed to evaluate the predictors of conversion from LA to OA through a retrospective study highlighting whether patients’ characteristics and surgeons’ prior experience could impact the conversion.
METHODS
From January 2010 to December 2020, appendectomy for acute appendicitis was performed on 853 patients in the Surgical Department at Habib Thameur Hospital in Tunis, Tunisia. Of these, 725 (84.9%) underwent LA. The clinical, demographic, surgical, and pathological data of these patients were included in a prospective database and were retrieved from our hospital. To record, only LA were considered in the analysis.
The following factors were analyzed to determine which ones were related to the conversion from LA to OA: age, sex, body mass index (BMI), previous abdominal surgery, comorbidities, clinical and laboratory parameters including Alvarado score 1 , preoperative C-reactive protein (CRP), intraoperative findings such as anatomy and degree of inflammation.
During the study period, LA were performed by different surgeons both resident and attending surgeons. The decision to convert to an open procedure was made personally by the surgeon.
Inclusion criteria
The inclusion criteria were: all adult patients older than 14 years of age, admitted with acute appendicitis and who underwent LA.
Exclusion criteria
The exclusion criteria were: patients with missing data, incomplete records, those who underwent two simultaneous procedures, and direct OA cases.
Statistical analysis
All data were assessed with the Statistical Package for Social Sciences (SPSS) software (version 25.0). Multivariate analysis was performed with logistic regression. Two-sided p-values <0.05 were considered statistically significant. The qualitative variables were expressed by their percentages, the quantitative variables by the mean, and by standard deviation (±SD) when the distribution was Gaussian, otherwise, by the median, interquartile, and extremes. Once the data analyzed were from the hospital database, prior approval of the Institution’s Ethics Committee was waived.
The technique of laparoscopic appendectomy
LA was performed using a 3-trocar approach (umbilical, 10 mm port; suprapubic, 5 mm port; and lower-left quadrant, 10 mm port), in the Trendelenburg position.
The appendix was extracted through the lower-left quadrant trocar in a plastic bag or through the trocar when removed, depending on the operator preference.
The technique of OA was performed via Mc-Burney’s incision or midline incision.
RESULTS
The study enrolled 725 patients who underwent LA. Demographic, clinical, and pathological data of the patients included in the analysis are summarized in Tables 1 and 2.
Table 1. Patients’ demographics.
| n (%) | ||
|---|---|---|
| Sex | ||
| Male | 201 (27.7) | |
| Female | 524 (72.3) | |
| Age (mean±SD) | 35.2±16 | |
| Comorbidities | ||
| One or more | 40 (5.5) | |
| None | 685 (94.5) | |
| Type of comorbidities | ||
| Arterial hypertension | 7 (0.97) | |
| Cardiovascular morbidities | 6 (0.83) | |
| Chronic obstructive pulmonary disease | 3 (0.42) | |
| Diabetes | 24 (3.31) | |
| BMI (kg/m2) mean±SD | 24.6±17.8 | |
| Previous abdominal surgery | 36 (4.97) | |
| Tenderness of iliac fossa | 596 (82.2) | |
| Defense of iliac fossa | 76 (10.5) | |
| Diffuse tenderness | 20 (2.76) | |
| Nausea and/or vomiting | 324 (44.7) | |
| Fever | 336 (46.34) | |
| WBC count (>10.000/mm3) | 572 (78.9) | |
| Alvarado score (mean±SD) | 5.4±1.7 | |
| CRP (mg/dL) (mean±SD) | 44±162.59 | |
BMI: body mass index; WBC: white blood cell; SD: standard deviation; CRP: C-reactive protein.
Table 2. Surgical and anatomical characteristics.
| n (%) | ||
|---|---|---|
| Surgeon | ||
| Attending surgeon | 225 (31) | |
| Resident | 500 (69) | |
| Retrocecal appendix | 112 (15.45) | |
| Edematous inflammation | 193 (26.62) | |
| Phlegmonous inflammation | 168 (23.17) | |
| Gangrenous inflammation | 132 (18.2) | |
| Perforated appendicitis | 59 (8.14) | |
| Appendicular abscess | 320 (44.14) | |
| Diffuse peritonitis | 24 (3.31) | |
| Conversion | 121 (16.7) | |
| Cause of conversion: | ||
| Difficult dissection | 351 (48.4) | |
| Surgery time (minutes, mean±SD) | 69.5±25.1 | |
SD: standard deviation.
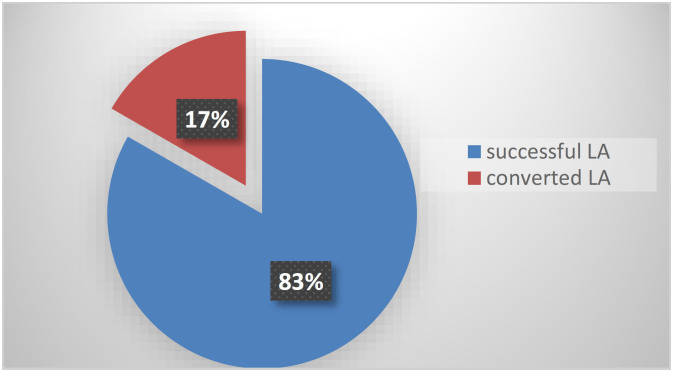
A total of 604 (83.3%) procedures were successfully performed using the laparoscopic approach while 121 (16.7%) were converted to the open approach (Figure 1). The mean age was 35.2±16 years with a range from 15–80 years. LA patients were significantly younger than the OA (34±14 vs 48±16), which is statistically significant (p<0.01).
Figure 1. Overall laparoscopic appendectomy conversion rate and successful completed laparoscopic rate.
LA: laparoscopic appendectomy.
LA was completed without conversion in 147 male patients and 457 female patients. The ratio of females to males is almost 2.6.
Previous abdominal surgery in LA group was performed in 32/604 (5.3%) patients, and in OA, it was performed in 4/121 (3.3%).
On comparing the clinical presentation of appendicitis, fever was the most common symptom, followed by vomiting and diarrhea in both groups. Symptoms of diffuse tenderness, rebound tenderness, localized guarding, and diffuse guarding were found to be significantly associated with conversion appendicectomy.
The preoperative CRP was higher in the OA group (162.59±100.4) with p<0.001, which is statistically significant. The present study highlights that significantly elevated CRP is also an independent risk factor for conversion from LA to OA.
The computed tomography (CT) scan findings showed that the presence of significant fat stranding, free fluid or free air, abscess formation, and CT grade of 4–5 significantly increased the possibility of conversion; in our study, we found that 68 patients were converted due to the presence of an abscess.
Intraoperatively, difficult dissection associated with a severe acute inflammatory process has been the most common reason to convert (84/121; 69.4%), followed by perforated appendix (44/121; 36.36%), and retrocecal appendix (44/121; 36.36%).
Other reasons justified the conversion, such as difficulty to identify the appendix, uncontrolled bleeding, impossibility to maintain an adequate pneumoperitoneum, and hypotension due to the Trendelenburg’s position.
The univariate analysis of factors related to conversion is shown in Tables 3 and 4, concluding that diffuse tenderness is a significant predictive factor for the conversion.
Table 3. Univariate analysis on demographics and clinical factors related to conversion.
| LA group n=604 n (%) |
OA group n=121 n (%) |
p-value | ||
|---|---|---|---|---|
| Sex | 0.003 | |||
| Male | 145 (24) | 54 (44.6) | ||
| Female | 457 (76) | 67 (55.4) | ||
| Age (mean±SD) | 34±14 | 48±16 | 0.001 | |
| Comorbidities | 0.760 | |||
| One or more | 32 (5.3) | 8 (6.6) | ||
| None | 572 (94.7) | 113 (93.4) | ||
| Type of comorbidities | ||||
| Arterial hypertension | 3 (0.5) | 4 (3.3) | 0.017 | |
| Cardiovascular morbidities | 2 (0.33) | 4 (3.3) | 0.008 | |
| Chronic obstructive pulmonary disease |
1 (0.16) | 2 (1.65) | 0.074 | |
| Diabetes | 20 (3.31) | 4 (3.3) | 0.740 | |
| BMI (kg/m2, mean±SD) | 23.5±4.3 | 25.8 ± 4.9 | 0.716 | |
| Previous abdominal surgery | 32 (5.3) | 4 (3.3) | 0.469 | |
| Tenderness of iliac fossa | 524 (86.75) | 72 (59.5) | 0.455 | |
| Defense of iliac fossa | 44 (7.28) | 32 (26.45) | 0.612 | |
| Diffuse tenderness | 8 (1.32) | 12 (9.92) | 0.009 | |
| Nausea and/or vomiting | 184 (30.46) | 140 (1.16) | 0.703 | |
| Fever | 276 (45.7) | 60 (49.6) | 0.670 | |
| WBC count (>10.000/mm3) | 530 (87.7) | 42 (34.7) | 0.568 | |
| Alvarado score (mean±SD) | 5.3±1.6 | 5.5±1.9 | 0.0025 | |
| CRP (mg/dL) (mean±SD) | 44±51.04 | 100.4±162.59 | <0.001 | |
CRP: C reactive protein; SD: standard deviation; WBC: white blood cell; BMI: body mass index; LA: laparoscopic appendectomy; OA: open appendectomy.
Table 4. Univariate analysis on surgical and pathological factors related to conversion.
| LA n (%) |
OA n (%) |
p-value | ||
|---|---|---|---|---|
| Surgeon | 1 | |||
| Attending surgeon | 117 (19.4) | 108 (89.26) | ||
| Resident | 487 (80.6) | 13 (10.74) | ||
| Retrocecal appendix | 68 (11.26) | 44 (36.36) | <0.001 | |
| Phlegmonous inflammation | 148 (24.5) | 20 (16.53) | 1 | |
| Perforated appendicitis | 15 (12.4) | 44 (36.36) | <0.001 | |
| Appendicular abscess | 289 (47.8) | 31 (25.6) | 0.001 | |
| CRP (mg/dL) | 44±51.04 | 100.4±162.59 | <0.001 | |
| Difficult dissection | 267 (44.2) | 84 (69.4) | <0.001 | |
LA: Laparoscopic appendectomy; OA: open appendectomy; CRP: C-reactive protein.
A multivariate analysis (Table 5) was then conducted to assess which of the factors were independently related to the decision to convert the intervention. The factors statistically predictive of conversion were: presence of comorbidities (odds ratio [OR] 3.1; 95% confidence interval [CI] 1.1–8.8; p<0.029), a finding of an appendiceal perforation (OR 5.2; 95%CI 1.8–15.0; p<0.003), retrocecal appendix (OR 5.0; 95%CI 1.7–14.8; p<0.004), gangrenous appendix, the presence of appendicular abscess (OR 3.6; 95%CI 1.2–11.1; p<0.023) and the presence of difficult dissection (OR 9.2; 95%CI 1.8–47.8; p<0.008).
Table 5. Multivariate analysis of factors related to conversion.
| Factors | OR (95%CI) | p-value |
|---|---|---|
| Comorbidities | 1.27 (0.57–2.83) | 0.029 |
| Male/Female | 2.54 (1.7–3.81) | 0.295 |
| Appendiceal perforation | 5.2 (1.8–15) | 0.003 |
| Retrocecal appendix | 4.5 (2.87–13.8) | 0.004 |
| Appendicular abscess | 3.3 (1.2–11) | 0.023 |
| Alvarado score 1 (mean±SD) | 1.329 (1.024–1.724) | 0.033 |
| Difficult dissection | 2.87 (2.56–3.2) | 0.045 |
| CRP | 2.69 (0.989–1.16) | 0.002 |
SD: standard deviation; OR: odds ratio; CI: confidence interval; CRP: C-reactive protein.
DISCUSSION
Since its initial description by Kurt Karl Stephan Semm, many other studies had encouraged LA over OA, due to its advantages 12,15 . LA leads to lower postoperative pain, shorter postoperative hospital stay, conducting to a reduced recovery time 7,11,14,15 .
Conversion rate is one of the main factors used to measure laparoscopic competence 5 . The rate of conversion evaluated by many studies was related to various factors and was more associated with higher hospital costs 10 . The main goal of this study was to develop a clinical tool that enables surgeons to estimate the risk of conversion from AL to OA based on objective and easily available preoperative patient parameters.
Almost all studies on the conversion rate from LA to OA affirmed a rate of 9–12% 8,13 .
The conversion rate of 16.7% in this current work is almost identical to the literature’s results. We concluded that multiple factors related to patients’ characteristics may influence LA conversion to OA 12 such as advanced age (≥65) 10,12 ; patients older than 65 years were associated with higher conversion rate (33.3%) compared to <65 years-old patients (8.9%), (p-value 0.002) 10 . In our study, advanced age was associated with a higher rate of conversion (p-value 0.001) as well.
Other studies demonstrated that males and old age were significant independent factors predicting conversion to OA 4 . Male patients consulting for right lower abdominal pain were more associated with perforated appendicitis, thereby they had the highest-level conversion 2,11,12 .
The majority of patients (96.7%) who underwent laparoscopic conversion recorded in this study, had no previous abdominal surgery. However, the most common reason of conversion was a severe inflammation causing difficult and unsafe dissection. Delayed presentation of appendicitis is also associated with a higher risk of conversion to OA 4 .
On physical examination, diffuse tenderness carried a high risk of conversion to OA (9.92%; p<0.009) 11 , whereas in CT scan, severe inflammation was considered to be an independent predictor of conversion 4 .
Peedikathara et al. 11 found that ultrasonography findings like an abscess (OR -8.000; 95%CI -1.006–63.962; p=0.049) and probe tenderness without visualizing appendix (OR -0.133; 95%CI -0.020–0.880; p=0.036) were significantly predicting factors of conversion to OA.
The CT scan grade of 4–5 is an important predictor factor of conversion 10 . In our study, the Alvarado score 1 is significantly associated with a higher rate of conversion (p<0.0025).
The CRP is a good marker of severe inflammation which could be a significant risk factor for conversion to OA. A higher value of CRP is associated with severe located inflammatory reaction with increased risk of bleeding, adhesion with the surrounding tissue, and complicated appendicitis 4 .
According to the receiver operating characteristic (ROC) analysis of Aydın et al. 2 , a CRP value of 108.5 mg/L was a risk factor for the conversion to OA. Shimoda et al. 13 concluded that preoperative CRP of >100 and >150 mg/L were a statistically significant predictor for conversion.
Increased value of white blood cell (WBC) count >15000 cells/cumm was seen to be more associated with conversion to OA, but it is not a statistical independent factor related to conversion 2 . Aydın et al. indicated that a neutrophil ratio of 81.5% was a significant predictive factor of a higher rate conversion because it concludes to bacterial translocation leading to diffuse peritonitis and intraabdominal abscess development 2 .
The preoperative findings such as severe inflammation, gangrenous and perforated appendicitis are the major factors impacting the operative difficulties and associated with conversion to OA 6,8,13 .
Wei et al. 14 concluded to higher conversion rate due to less surgeon experience. Inexperienced surgeons couldn’t handle the intraoperative difficulties leading usually to conversion to OA 12 . Liu et al. 10 have confirmed this relationship between the higher rate of conversion (31.3%) and the inexperienced surgeons (≤10 LA performed). However, in the present study, there was no difference in the overall conversion rate between experienced surgeons and resident surgeons, which can be explained by their good initial learning curve.
The higher surgical level of experience in LA leads to a shorter operating time, especially in complicated appendicitis which can need hand touching 6 . Intra-operative complications like Iatrogenic bowel injury and bleeding could not be managed laparoscopically, and mostly lead to open conversion 16 .
This study had concluded to independent factors of conversion: advanced age, Alvarado score 11 , high CRP value, and intraoperatively findings such as retrocecal appendix, perforated appendicitis, and appendicular abscess.
CONCLUSIONS
Laparoscopic appendectomy is a minimally invasive procedure that has become recommended as a standard technique for routine appendicitis, resulting in a better cosmetic outcome, and a shorter recovery time. Conversion from LA to OA procedure is done for more than one reason. Preoperatively, it is possible to identify predictive factors for conversion to laparotomy, and the ability to identify these reasons of conversion can aid surgeons in selecting patients who would benefit from a primary open appendectomy.
Footnotes
Financial source: None
Editorial Support: National Council for Scientific and Technological Development (CNPq).
Central Message
Many studies have confirmed that the laparoscopic approach is a mainstream technique in acute appendicitis. However, complicated appendicitis is considered a dilemma in their management regarding the greater demand for a high-quality experience and the fear of postoperative septic complications. A decision on which approach should be performed must be subject to preoperative criteria.
Perspectives
Laparoscopic appendectomy is a safe procedure to treat acute appendicitis. It is a minimally invasive surgery and has many advantages. Preoperatively, it is possible to identify predictive factors for conversion to laparotomy, and the ability to identify these reasons can aid surgeons in selecting patients who would benefit from a primary open appendectomy.
REFERENCES
- 1.Antonacci N, Ricci C, Taffurelli G, Monari F, Del Governatore M, Caira A, et al. Laparoscopic appendectomy: which factors are predictors of conversion? A high-volume prospective cohort study. Int J Surg. 2015;21:103–107. doi: 10.1007/s10120-014-0443-2. [DOI] [PubMed] [Google Scholar]
- 2.Aydın HO, Avcı T, Tezcaner T, Kırnap M, Yıldırım S, Moray G. Role of preoperative C-reactive protein value and neutrophil ratio in the determination of conversion from laparoscopic appendectomy to open appendectomy. Ulus Travma Acil Cerrahi Derg. 2018;24(5):429–433. doi: 10.5505/tjtes.2018.68705. [DOI] [PubMed] [Google Scholar]
- 3.Belotto M, Coutinho L, Pacheco AM, Jr, Mitre AI, Fonseca EAD. Influence of minimally invasive laparoscopic experience skills on robotic surgery dexterity. Arq Bras Cir Dig. 2022;34(3):e1604. doi: 10.1590/0102-672020210003e1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi KW, Park BK, Suh SW, Lee ES, Lee SE, Park JM, et al. Risk factors for additional port insertion in single-port laparoscopic appendectomy. Wideochir inne tech maloinwazyjne. 2019;14(2):223–228. doi: 10.5114/wiitm.2018.77714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deboni VS, Rosa MI, Lima AC, Graciano AJ, Garcia CE. The appendicitis inflammatory response score for acute appendicitis: is it important for early diagnosis? Arq Bras Cir Dig. 2022;35:e1686. doi: 10.1590/0102-672020220002e1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finnerty BM, Wu X, Giambrone GP, Gaber-Baylis LK, Zabih R, Bhat A, et al. Conversion-to-open in laparoscopic appendectomy: a cohort analysis of risk factors and outcomes. Int J Surg. 2017;40:169–175. doi: 10.1016/j.ijsu.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 7.Hansen JB, Smithers BM, Schache D, Wall DR, Miller BJ, Menzies BL. Laparoscopic versus open appendectomy: prospective randomized trial. World J Surg. 1996;20(1):17–20. doi: 10.1007/s002689900003. [DOI] [PubMed] [Google Scholar]
- 8.Hiramatsu K, Toda S, Tate T, Fukui Y, Tomizawa K, Hanaoka Y, et al. Can laparoscopic appendectomy be safely performed by surgical residents without prior experience of open appendectomy? Asian J Surg. 2018;41(3):270–273. doi: 10.1016/j.asjsur.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Korndorffer Jr, JR, Fellinger E, Reed W. SAGES guideline for laparoscopic appendectomy. Surg Endosc. 2010;24(4):757–761. doi: 10.1007/s00464-009-0632-y. [DOI] [PubMed] [Google Scholar]
- 10.Liu SI, Siewert B, Raptopoulos V, Hodin RA. Factors associated with conversion to laparotomy in patients undergoing laparoscopic appendectomy. J Am Coll Surg. 2002;194(3):298–305. doi: 10.1016/s1072-7515(01)01164-4. [DOI] [PubMed] [Google Scholar]
- 11.Peedikathara LM, Mandumpala JM, Vallon SM, Kavalakat AJ. Predictors for conversion to open appendicectomy in patients undergoing laparoscopic appendicectomy: a prospective study. Int Surg J. 2018;5(7):2588–2588. doi: 10.18203/2349-2902.isj20182779. [DOI] [Google Scholar]
- 12.Sakpal SV, Bindra SS, Chamberlain RS. Laparoscopic appendectomy conversion rates two decades later: an analysis of surgeon and patient-specific factors resulting in open conversion. J Surg Res. 2012;176(1):42–49. doi: 10.1016/j.jss.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Shimoda M, Maruyama T, Nishida K, Suzuki K, Tago T, Shimazaki J, et al. Preoperative high C-reactive protein level is associated with an increased likelihood for conversion from laparoscopic to open appendectomy in patients with acute appendicitis. Clin Exp Gastroenterol. 2019;12:141–147. doi: 10.2147/CEG.S196471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei HB, Huang JL, Zheng ZH, Wei B, Zheng F, Qiu WS, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc. 2010;24(2):266–269. doi: 10.1007/s00464-009-0563-7. [DOI] [PubMed] [Google Scholar]
- 15.Yau KK, Siu WT, Tang CN, Yang GP, Li MK. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007;205(1):60–65. doi: 10.1016/j.jamcollsurg.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Yu MC, Feng YJ, Wang W, Fan W, Cheng HT, Xu J. Is laparoscopic appendectomy feasible for complicated appendicitis? A systematic review and meta-analysis. Int J Surg. 2017;40:187–197. doi: 10.1016/j.ijsu.2017.03.022. [DOI] [PubMed] [Google Scholar]