Abstract
Spine fractures are most commonly observed among older people due to weak bones and irregular postures. These fractures of 10 lead to coccygodynia. Women are 5 times more prone to developing coccygodynia as compared to men. Initially, different painkillers, physiotherapy, and other non-surgical treatments are recommended to reduce the pain. However, in case of the failure of these treatments, a surgical procedure (named coccygectomy) is considered to remove the tailbone to achieve effective outcomes. The main aim of this study is to determine the effectiveness of coccygectomy in treating coccygodynia (after the failure of different non-surgical treatments) in the context of patients who were treated at Konya City Hospital neurosurgery department, Turkey. In this study, a total of 14 cases of coccygodynia treated with coccygectomy at Konya City Hospital were selected from the period of August 2020 and January 2022. These patients were given different treatments for 6 to 7 months before the operation. Therefore, due to the lack of positive outcomes, a coccygectomy was performed by a senior surgeon. Visual analogue scale was used to assess the pain of the patients after the surgery. Statistical Package for the Social Sciences was used for statistical analysis. The level of significance was set at P < .05. The results of this study showed that more women suffered from coccygodynia as compared to men. Most of the patients had Type I (35.7%) and Type IV (35.7%) coccyx. The visual analogue scale was reduced after the surgery (P < .0011), showing positive outcomes. Ten (71.4%) cases showed excellent outcomes, whereas only one (7.1%) case showed poor outcomes after the surgery, and wound infections were observed in two (14.2%) cases post-operatively. The results obtained from this study concluded that in case of failure of conservative non-surgical treatments for coccygodynia, coccygectomy has emerged as an effective surgical method which is recommended by various surgeons to reduce the pain by removing the tailbone. Additionally, only a few complications such as infection as a relevant concern after this type of surgery were observed, and most of the patients were satisfied with the outcomes and also recommended it to others.
Keywords: coccygectomy, coccygodynia, coccyx, single center, Turkey, VAS
1. Introduction
Coccygodynia is the pain in the coccyx region, commonly referred to as tailbone pain in layman’s terms.[1] It is characterized by tenderness and pain around the coccyx region, and most of the time and the condition remains undiagnosed for years due to misdiagnosis.[2,3] Fractures, hypermobility, repetitive microtrauma, or trauma are among the etiological factors associated with coccygodynia.[1,4,5] Individuals who have a history of trauma around the coccyx region develop chronic inflammation around the joint due to repetitive trauma causing coccygeal instability.[6–8] The rare syndrome is found to be relatively more common in overweight individuals, and women are likelier to get affected[9–12] and old age is also considered a risk factor.[13] The anatomy and physiology of the coccyx, which consists of 4 or 5 cranial bones attached to the sacrum, are important in understanding the pain resulting from trauma.[11,12,14] Furthermore, hyperactivity of nerve cells in the ganglion impar, which shapes at the end of lumbosacral sympathetic chains, can cause pain in the coccyx, pelvic and rectal region.[5,13] It has a varying size and location. Patients with coccygodynia typically complain about discomfort and soreness around the coccyx.[1,15]
Several factors can cause pain in the coccyx, such as spasms in pelvic floor muscles and prolonged sitting on hard surfaces for a long period. Individuals who have existing health issues such as obesity and degenerative disc or undergo surgical processes for weight loss can suffer from coccygodynia.[1,9] Furthermore, the pain is exacerbated when patients stand up or by sitting.[15] Pain can arise during defecation or intercourse[16]; however, these are quite infrequent and uncommon symptoms. The treatment of coccygodynia can be difficult and complex due to the variability of anatomy, along with the complexity of the visceral, autonomic, and neuropathic parts.[17] Radiography can be used in diagnosis[18]; however, an effective diagnostic tool to detect pain in the coccyx is the increase in palpation which is used.[1,3] Initially, conservative management is carried out by prescribing analgesic and anti-inflammatory drugs, and in severe cases, steroid injections are utilized or surgical treatment if issues persist.[19,20]
An effective and straightforward surgical procedure commonly used is coccygectomy.[15,20,21] The surgical procedure involves the removal of the coccyx, either partially or completely, and it is only recommended for patients with anatomic defects, failed conservative therapy, or significant disability.[3,15,20] Current literature has reported the success of coccygectomy in several cases of persistent coccygodynia.[3,11,22] Wound infection is stated to be one of the most common complications.[23,24] Radiographs are generally used in the diagnosis. Hypermobility and subluxation are commonly seen in radiographs.[25] For accurate diagnosis and appropriate treatment, it is necessary to evaluate the patient through physical examination and have access to satisfactory radiographs.
Coccygodynia is a rare condition that requires appropriate treatment and effective management to provide high-quality care to the patients suffering from it. Therefore, it is critical to evaluate the outcomes of surgical treatment, which can aid healthcare staff and patients in adopting suitable strategies. The outcome of surgical treatment of coccygodynia has not been extensively studied in Turkey; therefore, the purpose of the study is to determine the effectiveness of coccygectomy in a single-setting study among patients with coccydynia.
1.1. Literature review
The end segment of the spine is the coccyx, named after its similar appearance to the shape of a beak of a cuckoo.[25] This triangular bone comprises 3 to 5 segments, the levator ani muscle and sacrococcygeal ligament are to its anterior. Pathological mobility is observed in the sacrococcygeal joint as well as inter-coccygeal joints due to the existence of intact discs.[1] Internal or external trauma is regarded as the most common cause of coccygodynia, whereas internal trauma such as childbirth can cause coccygodynia,[26,27] and falling is categorized as external trauma.[28,29] A possible cause of the pain can be linked to the presence of an intervertebral disc between Co1 and Co2.[19] Along with the ischial tuberosities, individuals are supported while sitting by the coccyx. Nevertheless, the vulnerability of the coccyx to injury by external trauma increases due to this particular location.
Studies have shown that patients suffering from coccydynia have a previous history of direct trauma.[30] Furthermore, the injury depends on the severity of the trauma. The injury can be due to a muscle spasm of the pelvis or slight deformation over a fissure, or a serious fracture of the sacrococcygeal complex.[31,32] The description of the disease was given back in the 1960s by Thiele, and it is still considered accurate and true. Patients describe the pain as sharp, stabbing or aching pain in the coccygeal segments[8,33] Pain can be mild but severe cases are reported with agonizing pain that affects the daily functioning of individuals.[34] Previous studies have shown that pain is experienced particularly when sitting on hard surfaces.[1] Activities that cause strain on the levator ani muscle are found to be associated with aggravation of symptoms.[16] Imaging studies are widely used to diagnose hypermobility or hypomobility.[15,19]
In addition, adjustment to physical lifestyle is required, such as changing the sitting position and posture, using specific pillows, and physical therapy.[35] Despite the limited evidence, the use of non-steroidal anti-inflammatory drugs is the first choice of treatment adopted by physicians for conservative therapy. Furthermore, manual manipulation and massage are widely adopted,[36] and such treatment by chiropractors and physical therapists are found to be effective in relieving pain.[37,38] It is imperative to evaluate each patient individually, as no single treatment has been rendered as the most effective. Previous studies have established that conservative management is deemed successful and appropriate in 90% of patients.[37,39]
However, when conservative management and injections are ineffective, a surgical procedure is recommended, and a coccygectomy is carried out, which has resulted in good outcomes.[3,34,37,40] However, this surgical treatment is associated with challenges such as a high probability of infection and complex follow-up care.[21] As per research, coccygectomy has a complication rate ranging from 0 to 50%.[41] Wound-related complications are common, which causes a delay in healing. A study revealed that the infection rate could be reduced by following appropriate techniques, which consist of using skin adhesive along with the administration of prophylactic antibiotics and nonabsorbable skin sutures.[42]
A prospective study evaluated the outcome of coccygectomy among 98 patients and found that surgical procedures significantly improved the quality of life of patients.[43] Patients’ outcomes were analyzed 2 years after the operation.[43] The failure of a coccygectomy is linked with pre-operative conditions. Psychiatric illness, opiate use, and comorbidities are associated with the failure of coccygectomy.[43] Furthermore, research has shown that the success of surgical treatment is found to be highest among patients with painful and postpartum coccygodynia. The complication rate was found to be approximately 10.9% as per a review of 671 coccygectomies.[44] Wound infections and complications arise due to the excessive tension on the incision site during sitting and the difficult position of the coccyx.[15]
2. Materials and methods
For this study, 14 consecutive patients (including 5 males and 9 females) who underwent coccygectomy between January 2018 and January 2022 were included. All these patients were treated at Konya City Hospital neurosurgery department. The coccyx excision was applied to patients who did not benefit from conservative treatment applied for at least 1 year. All of the patients who were taken into surgery were treated conservatively with non-steroidal anti-inflammatory drugs (at least 1 year intermittently) and sitting in hot water (at least 3 months). Moreover all of them used a sitting pillow regularly for the last 3 months. Intradiscal injection (Citanest 1 ml-Diprospan 1 ml) was applied twice to 9 patients and once to 5 patients. Patients who did not benefit from these treatments were taken to surgery. All of these patients suffered from coccygodynia and underwent different treatments for 6 to 7 months before undergoing the surgical procedure. These non-surgical treatments included steroid injections, physical therapy, and non-steroidal anti-inflammatory drugs (NSAIDs). Before the operation, notes were made focusing on patients’ perceptions regarding misdiagnosis. However, no patient had any diagnosed psychiatric disorder. During clinical examination (before surgery), “marked tenderness on palpation” was observed over the coccyx in all patients. A rectal examination was also done digitally to determine any rectal-based pathology. All patients went through radiographic imaging and magnetic resonance imaging of the sacrum, as shown in Figures 1 and 2.
Figure 1.
Case I: (A) Coccygeal spicule presented in a sagittal view CT scan. (B) An evident spicule presented by a 3D CT scan. (C) Coccygeal spicule presented in a lateral view of the x-ray. (D) Incision line (intra = operative). (E) Coccyx sub-periosteal resection (intra-operative). CT = computerized tomography.
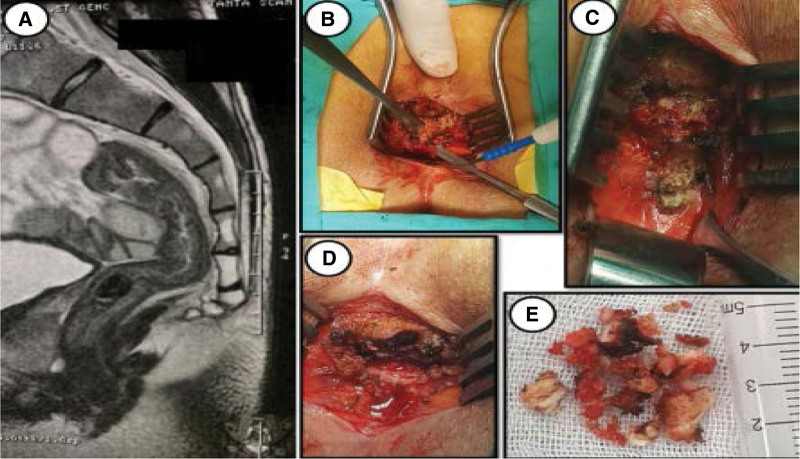
Figure 2.
Case II: (A) Coccygeal spicule (MRI sagittal). (B) Bony coccyx partial exposure (intra-operative). (C) Resected bony spicule (intra-operative). (D) Distal disc (intra-operative). (E) Meal fragments of the resected bony spicule. MRI = magnetic resonance imaging.
2.1. Surgical method
A rectal enema was conducted the night before the operation. General anesthesia was given to the patient, and an incision of about 4 to 6 cm long was made in the midline of the sacrococcygeal region. Electro-cauterization was used for exposing the coccyx and distal sacrum. In order to avoid any bowel injury, the separation of the intervertebral joint of the affected region was done, followed by the resection of the sub-periosteal coccyx. Hemostasis was obtained, and the subcutaneous and fascia tissues were closed by utilizing “interrupted number 1 and 2/0 Vicryl sutures.” The wound was covered by using a waterproof adhesive, and all patients were given 1g of cefazolin for 5 days (Every 8 hours) after the surgery performed by a senior surgeon (Figs. 1 and 2).
2.2. Post-operative management and follow-up
All patients were asked to avoid any physical activities for at least 3 weeks after the operation. They were prohibited from lifting heavy weights. They were also asked to avoid sitting until the stitches were healed to avoid any sort of discomfort.
The follow-up of the patients was performed during at least 5 years and they were observed at every 3 months. For this study, a standardized questionnaire was developed to determine the post-operative recovery of the patients. A “visual analogue scale” (VAS) was used to quantify the pain experienced by the patients’ pre and post-surgery. The patients were also asked whether their quality improved or not after the surgery. The success of the operation was determined based on the collected data. The results were considered according to VAS classes as excellent (≤2), good (≤3), satisfactory (≤6), and poor (> 6). Different notes were also made regarding the post-operative complications faced by the patients and their stay at the hospital.
2.3. Morphological categorization
Concerning the patients who underwent “lateral radiographs of the coccyx” before the operation, the morphology was categorized into 4 types, as presented by Postacchini and Massobrio.[45] These types are discussed in Table 1.
Table 1.
Morphology categorization of the coccyx.
| Type I | It is slightly curved at the forward, and the apex is usually pointing downwards |
| Type II | It points straight in the forward direction |
| Type III | It is angulated in the forward direction between the 2nd and 3rd segments or the 1st and 2nd segments |
| Type IV | It is subluxated at the anterior position levelling the SC joint |
However, for the patients who did not have these radiographs, computerized tomography scans or magnetic resonance imagines were considered to observe the coccyx. Radiology reports were found to be effective for this study. Therefore, any dislocated coccyx presented in the reports was categorized as Type IV.
2.4. Statistical analysis
The statistical analysis was performed by Statistical Package for the Social Sciences with version 20.0 (IBM Inc, Chicago, IL). The descriptive statistics were presented as frequencies (percentages) for representing categorical variables, and mean ± standard deviation for representing continuous variables. The comparison between the pre and post VAS scores was performed by Paired Sample t test. The significant level for this study was set at P < .05.
2.5. Ethical considerations
Ethical considerations were also taken into account for this study. The study was initiated with the approval of the KTO Karatay University Medical Faculty Clinical Researches Ethics Committee (2023-52839). No patient was forced to participate in the study. The consent of the patients and healthcare professionals was taken before collecting the data. The confidentiality of the patients was ensured. Moreover, while collecting the data, a professional nurse accompanied the researcher.
3. Results
3.1. Patients’ characteristics
Table 2 shows the characteristics of the patients who willingly participated in the present study. It has been observed from the table that the total number of patients who participated in this study was 14. The mean age of these patients was 38.3 years. Nine (64.2%) of these patients were female, while only 5 of them (35.7%) were male. This shows that this coccygodynia was most commonly observed in women than in men. The most common coccygodynia cases were found to be indirect or direct trauma which was observed in 10 (71.4%) patients. At the same time, only 4 (28.5%) cases were idiopathic. However, the “lateral sacrococcygeal radiographs” helped in determining the types of the coccyx in every case. Table 2 shows that Type I coccyx was found in five (35.7%) cases, whereas Type II coccyx was found in only one (7.1%) case. Type III coccyx was observed in three (21.4%) cases, while Type IV was observed in five (35.7%) cases.
Table 2.
Characteristics of the patients.
| Characteristics | N | % |
|---|---|---|
| Mean age (yr), mean ± SD | 38.3 ± 8.7 | |
| Gender | ||
| Female | 9 | 64.2 |
| Male | 5 | 35.7 |
| Total | 14 | 100 |
| Coccygodynia cases | ||
| Indirect or direct trauma | 10 | 71.4 |
| Idiopathic | 4 | 28.5 |
| Total | 14 | 100 |
| Morphological classification of the coccyx | ||
| Type I | 5 | 35.7 |
| Type II | 1 | 7.1 |
| Type III | 3 | 21.4 |
| Type IV | 5 | 35.7 |
| Total | 14 | 100 |
3.2. VAS results
Table 3 shows that the mean value of VAS was recorded to be 9.63 before the operation, whereas, after the surgery, it was recorded to be 2.26 (P < .001). Thus it has been concluded from this result that pain decreased after the operation. However, the median time (in which the symptoms were reported by the patients) was stated to be 29.3 months. At the same time, only 28% of the patients claimed to be misdiagnosed. They were of the view that they suffered from some other pathological condition. Additionally, 85% of the patients were determined to undergo the surgical procedure again in case of the same condition. Moreover, 91% of the patients said that they would have the surgical procedure earlier if they were given the option, and 85% of the patients recommended this surgical procedure to other patients.
Table 3.
Visual analogue scale of patients.
| Pre-operative | Post-operative | |
|---|---|---|
| Mean ± SD | 9.63 ± 4.28 | 2.26 ± 1.37 |
| P value | <.001 |
3.3. Detailed overview of the included cases
A detailed overview of the included cases is observed in Table 4. It has been observed that most of the cases showed excellent outcomes after the surgery. About 10 (71.4%) of the 14 cases showed excellent outcomes after the surgery (VAS < 2/10). Out of these 10 cases, 8 (80%) were traumatic cases, while 2 (20%) were idiopathic. The pre-operative treatments provided to these patients included physical therapy, local injection, steroid injection, and NSAIDs.
Table 4.
Cases overview.
| Case no. | Age (yr) | Gender | Coccygodynia cases | Management | Management duration (mo) | Coccyx type (radiological finding) | Comp. | VAS (pre-op) | VAS (post-op) | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 38 | F | Trau. | 4, 3 | 11 | IV | N | 9 | 1 | Exc |
| 2 | 39 | M | Trau. | 4, 3, 2, 1 | 8 | I | N | 8 | 1 | Exc |
| 3 | 44 | F | Trau. | 4, 3, 2 | 10 | I | N | 10 | 1 | Exc |
| 4 | 56 | F | Idio. | 4, 3, 1 | 21 | IV | N | 9 | 2 | Exc |
| 5 | 36 | F | Trau. | 4, 3, 2 | 31 | III | WI | 9 | 2 | Good |
| 6 | 28 | M | Idio. | 4, 2 | 30 | I | N | 10 | 1 | Exc |
| 7 | 29 | F | Trau. | 2, 3, 2, 1 | 21 | I | N | 9 | 1 | Exc |
| 8 | 33 | F | Trau. | 4, 3, 2 | 10 | III | N | 8 | 4 | Fair |
| 9 | 45 | M | Trau. | 4, 3, 2 | 21 | I | N | 10 | 2 | Exc |
| 10 | 49 | F | Idio. | 4, 2 | 11 | III | WI | 9 | 4 | Good |
| 11 | 31 | M | Trau. | 4, 2 | 17 | IV | N | 10 | 1 | Exc |
| 12 | 34 | F | Idio. | 4, 3, 2 | 22 | IV | N | 8 | 6 | Poor |
| 13 | 35 | F | Trau. | 4, 3, 2, 1 | 25 | II | N | 10 | 1 | Exc |
| 14 | 46 | M | Trau. | 4, 3, 2 | 28 | IV | N | 9 | 1 | Exc |
1 = “pericoccygeal steroid injection,” 2 = local injection, 3 = physical therapy, 4 = oral medicines for pain, Comp = complications, exc = excellent, F = female, idio = idiopathic, M = male, N = none, post-op = postoperative, pre-op = preoperative, Trau = traumatic, VAS = visual analogue scale, WI = wound infection.
Moreover, wound infection was only observed in two (14.2%) cases after surgery. The outcomes of these cases were found to be good. Therefore, only one (7.1%) case with a Type III coccyx showed fair results, and one (7.1%) case with a Type IV coccyx showed poor outcomes after the surgery.
4. Discussion
The rare but painful condition of coccygodynia makes up approximately 1% of all cases of back pain.[40] Coccygectomy is opted for treating coccygodynia when conservation methods and therapies fail to bring relief and treat the condition.[20,37,46] However, due to the rarity of the condition and complications associated with the surgical treatment, operations are usually delayed. Hence, the aim of the study was to analyze the outcome of coccygectomy among patients with coccygodynia.
In terms of gender, the findings of the study showed that women had a greater likelihood of developing coccygodynia (64.2%) compared to men (35.7%). Similarly, previous studies have reported that a greater number of women were found to suffer from coccygodynia as compared to men.[3,20,21] Furthermore, direct or indirect trauma was found to be the common etiology of coccydynia in cohorts, which is in line with previous studies.[5,21] However, a few studies have reported a slightly higher percentage of idiopathy.[43]
It was found that VAS significantly improved from 9.63 before the operation to 2.26 after the surgery. The reduction in VAS was observed in previous studies as well.[37] VAS was reduced from 9.62 before the coccygectomy to 2.25 after the operation.[3] Similarly, Hanley et al reported that surgical treatment significantly improved VAS. The majority of the patients were satisfied with the surgical outcome, as found in previous studies.[47] A study conducted on Turkish patients found that patients were satisfied with noninvasive and surgical treatments for coccygodynia.[48] However, when patients’ weight was taken into account, a study found that overweight individuals were less satisfied with the coccygectomy.[49–51]
Infection in the wound was found in 2 cases after the surgical procedure (14.2%). The low infection rate is associated with the adoption of appropriate pre-operative and post-operative measures. Pre-operative measures consisted of using physical therapy, local and steroid injections, and NSAIDS in the cohorts. The debate regarding coccygectomy centers around the infection rate; hence, pre-operative and post-operative care can significantly reduce the infection rate. The infection rate after surgical treatment has been reported as the most common complication with ranging from 6% to 27%. In the coccyx excision, the existing incision area is considered as clean-contaminated tissue. Prophylactic antibiotic therapy is recommended to prevent surgical wound infection. Compared to a few past research, the infection rate observed in the study is significantly lower, which can be due to the pre-operative and post-operative measures,[52] which included waterproof adhesive and antibiotic administration. Antibiotics are found to significantly reduce the infection rate and have been widely adopted as an effective post-operative practice.[23,24,53,54] Wound complications are regarded as the most frequent complication; however, it was shown in a study of 10 cases of coccygectomy that using “Z” plasty closure resulted in no wound infection among all the cases.[37] A review of treatments for coccygodynia, such as physical therapy, local injections, and surgical procedure, was conducted. Similar to our findings, it was found that coccygectomy is effective in treating patients with coccygodynia compared to conservative therapies.[55]
According to the results, most of the cases showed excellent outcomes after the surgery. Among the cases with excellent outcomes, the majority were traumatic cases. A case of Type III coccyx reported a fair outcome, whereas only 1 case of Type IV showed a poor outcome. Similarly, it was found that 36 out of 38 of the patients reported excellent results after coccygectomy.[20] Furthermore, a satisfactory outcome was observed in 79% of the patients who underwent coccygectomy.[56] A review of 24 studies showed that out of 702 patients, excellent or good outcomes were observed in 83% of the patients.[45] A review of 64 studies analyzed 1980 patients with coccygodynia, and different treatments were investigated. The findings of the study showed that non-surgical treatment was found to relieve pain for many patients. noninvasive procedures are given first priority, and coccygectomy is only considered after the ineffectiveness of non-operative measures. Furthermore, the study revealed that coccygectomy is considered the most effective treatment for refractory cases, and it is the most examined surgical treatment option.[11]
5. Conclusion
The results obtained from this study concluded that in case of failure of conservative non-surgical treatments for coccygodynia, coccygectomy has emerged as an effective surgical method which is recommended by various surgeons to reduce the pain by removing the tailbone. Additionally, only a few complications such as infection as a relevant concern after this type of surgery were observed, and most of the patients were satisfied with the outcomes and also recommended it to others.
5.1. Limitations and future research recommendations
Further studies are required to evaluate the effectiveness of coccygectomy for the generalizability of the results, as the cohorts consisted of Turkish patients only. The sample size in the study is small due to the rarity of the condition along with the greater use of non-operative methods, as most patients are treated with conservative management. Additionally, randomized control studies are required to assess the outcomes of coccygectomy by examining the length of pain relief and surgical complications. Therefore, further studies can utilize a larger sample size and evaluate the outcomes for a longer period of time.
Author contributions
Conceptualization: Emir Kaan İzci.
Formal analysis: Fatih Keskin.
Investigation: Emir Kaan İzci.
Methodology: Emir Kaan İzci.
Software: Fatih Keskin.
Validation: Fatih Keskin.
Visualization: Emir Kaan İzci.
Writing – original draft: Emir Kaan İzci.
Writing – review & editing: Emir Kaan İzci, Fatih Keskin.
Abbreviations:
- NSAIDS
- non-steroidal anti-inflammatory drugs
- VAS
- visual analogue scale
PRISMA
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Izci EK, Keskin F. Coccygectomy for coccygodynia: A single-center experience. Medicine 2023;102:22(e33606).
References
- [1].Garg B, Ahuja K. Coccydynia-A comprehensive review on etiology, radiological features and management options. J Clin Orthop Trauma. 2021;12:123–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ali L, Malik SH, Ahmed K, et al. Chronic pelvic pain; a tragic miss. Anaesth Pain Intensive Care. 2022;26:828–30. [Google Scholar]
- [3].Sarmast A, Kirmani A, Bhat A. Coccygectomy for coccygodynia: a single center experience over 5 years. Asian J Neurosurg. 2018;13:277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gufeld L, Vossen JA, Urquia D. Coccydynia: diagnostic and management guidance. J Nurse Pract. 2020;16:735–43. [Google Scholar]
- [5].Lirette LS, Chaiban G, Tolba R, et al. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J. 2014;14:84–7. [PMC free article] [PubMed] [Google Scholar]
- [6].Foye PM. Coccydynia: tailbone pain. Phys Med Rehabil Clin. 2017;28:539–49. [DOI] [PubMed] [Google Scholar]
- [7].Foye PM, Shah JM, Sinha D. Coccyx fracture and dislocation. Musculoskelet Sports Spine Disord. 2017:461–3. [Google Scholar]
- [8].Rana A-J, Shah KB. Coccydynia. In: Interventional Management of Chronic Visceral Pain Syndromes. Elsevier; 2021:47–52. [Google Scholar]
- [9].Akar E, Öğrenci A, Dalbayrak S. Coccydynia: a narrative review of pathophysiology, etiology and treatment. MNJ. 2023;9:33–9. [Google Scholar]
- [10].Haghighat S, Asl MM. Effects of extracorporeal shock wave therapy on pain in patients with chronic refractory coccydynia: a quasi-experimental study. Anesth Pain Med. 2016;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Andersen GØ, Milosevic S, Jensen MM, et al. Coccydynia – the efficacy of available treatment options: a systematic review. Global Spine J. 2022;12:1611–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Yarikov A, Perlmutter O, Sosnin A, et al. Coccygodynia: etiology, diagnosis, and treatment. Vrach. 2021;32:18–22. [Google Scholar]
- [13].Dampc B, Słowiński K. Coccygodynia – pathogenesis, diagnostics and therapy. Review of the writing. Pol J Surg. 2017;89:33–40. [DOI] [PubMed] [Google Scholar]
- [14].Won H, Moon S-Y, Park JH, et al. Epidemiology and risk factors of coccyx fracture: a study using national claim database in South Korea. Injury. 2020;51:2278–82. [DOI] [PubMed] [Google Scholar]
- [15].Almetaher HA, Mansour MA, Shehata MA. Coccygectomy for chronic refractory coccygodynia in pediatric and adolescent patients. J Indian Assoc Pediatr Surg. 2021;26:102–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lee J, Purnomo G, Hutabarat AF. Management of coccydynia: literature review, clinical decision making, and case studies. Crit Rev Phys Rehabil Med. 2020;32. [Google Scholar]
- [17].Usmani H, Dureja GP, Andleeb R, et al. Conventional radiofrequency thermocoagulation vs pulsed radiofrequency neuromodulation of ganglion impar in chronic perineal pain of nononcological origin. Pain Med. 2018;19:2348–56. [DOI] [PubMed] [Google Scholar]
- [18].Özkal B, Avnioğlu S, Candan B. Morphometric evaluation of coccyx in patients with coccydynia and classification. Acta Med Alanya. 2020;4:61–7. [Google Scholar]
- [19].Dayawansa S, Garrett D, Wong M, et al. Management of coccydynia in the absence of X-ray evidence: case report. Int J Surg Case Rep. 2019;54:63–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hochgatterer R, Gahleitner M, Allerstorfer J, et al. Coccygectomy for coccygodynia: a cohort study with a long-term follow-up of up to 29 years. Eur Spine J. 2021;30:1072–6. [DOI] [PubMed] [Google Scholar]
- [21].Mulpuri N, Reddy N, Larsen K, et al. Clinical outcomes of coccygectomy for coccydynia: a single institution series with mean 5-year follow-up. Int J Spine Surg. 2022;16:11–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Alkhamisy A, Morjan M, Abbas W. Posttraumatic coccydynia in a 7-year-old girl treated with coccygectomy. J Pediatr Surg Case Rep. 2021;71:101910. [Google Scholar]
- [23].Kalstad AM, Knobloch RG, Finsen V. Coccygectomy in the treatment of chronic coccydynia. Spine. 2022;47:E442–7. [DOI] [PubMed] [Google Scholar]
- [24].Sagoo NS, Haider AS, Palmisciano P, et al. Coccygectomy for refractory coccygodynia: a systematic review and meta-analysis. Eur Spine J. 2021:1–14. [DOI] [PubMed] [Google Scholar]
- [25].Skalski MR, Matcuk GR, Patel DB, et al. Imaging coccygeal trauma and coccydynia. Radiographics. 2020;40:1090–106. [DOI] [PubMed] [Google Scholar]
- [26].Márquez-Carrasco ÁM, García-García E, Aragúndez-Marcos MP. Coccyx pain in women after childbirth. Enferm Clín (English Edition). 2019;29:245–7. [DOI] [PubMed] [Google Scholar]
- [27].Vishnupriya S, Jagatheesan A, Dasarapu I. Coccydynia and disability on postpartum vaginal delivery women. INTI J. 2022:1–5. [Google Scholar]
- [28].Meer MJ, Atif MM, Afzal F, et al. Causes and risk factors of coccydynia in postpartum women in Dhq sargodha.
- [29].Protopapas M, Alhooie K. Coccydynia. Clin Guide Musculoskelet Med. 2022:179–84. [Google Scholar]
- [30].Malhotra N, Goyal S, Kumar A, et al. Comparative evaluation of transsacrococcygeal and transcoccygeal approach of ganglion impar block for management of coccygodynia. J Anaesthesiol Clin Pharmacol. 2021;37:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Jachak S, Samal S. Advanced physical rehabilitation in hairline coccyx fracture: a case report. J Pharm Res Int. 2021;221:227. [Google Scholar]
- [32].Cakir O, Sade R, Pirimoglu B, et al. Posterior dislocation of coccyx: a rare cause of Coccydynia. Am J Phys Med Rehabil. 2021;100:e109. [DOI] [PubMed] [Google Scholar]
- [33].Roa JA, White S, Barthélemy EJ, et al. Minimally invasive endoscopic approach to perform complete coccygectomy in patients with chronic refractory coccydynia: illustrative case. J Neurosurg Case Lessons. 2022;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Abdel-Aal NM, Elgohary HM, Soliman ES, et al. Effects of kinesiotaping and exercise program on patients with obesity-induced coccydynia: a randomized, double-blinded, sham-controlled clinical trial. Clin Rehabil. 2020;34:471–9. [DOI] [PubMed] [Google Scholar]
- [35].Gunduz OH, Sencan S, Kenis-Coskun O. Pain relief due to transsacrococcygeal ganglion impar block in chronic coccygodynia: a pilot study. Pain Med. 2015;16:1278–81. [DOI] [PubMed] [Google Scholar]
- [36].Mokhchani Y, Rachdi A, Rabbah A, et al. Coccygectomy: is it necessary for coccydynia? about a case and review of the literature. 2022.
- [37].Kulkarni AG, Tapashetti S, Tambwekar VS. Outcomes of coccygectomy using the “Z” plasty technique of wound closure. Global Spine J. 2019;9:802–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Seker A, Sarikaya IA, Korkmaz O, et al. Management of persistent coccydynia with transrectal manipulation: results of a combined procedure. Eur Spine J. 2018;27:1166–71. [DOI] [PubMed] [Google Scholar]
- [39].Trollegaard A, Aarby N, Hellberg S. Coccygectomy: an effective treatment option for chronic coccydynia: retrospective results in 41 consecutive patients. J Bone Joint Surg Br. 2010;92:242–5. [DOI] [PubMed] [Google Scholar]
- [40].Kleimeyer JP, Wood KB, Lønne G, et al. Surgery for refractory coccygodynia. Spine. 2017;42:1214–9. [DOI] [PubMed] [Google Scholar]
- [41].Dai Kwon H, Schrot RJ, Kerr EE, et al. Coccygodynia and coccygectomy. Korean J Spine. 2012;9:326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Nagappa S, Alshameeri Z, Elmajee M, et al. Clinical outcome of coccygectomy using a paramedian curvilinear skin incision in adults and children with meta-analysis of the literature focusing on post-operative wound infection. Global Spine J. 2021:21925682211058155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Hanley EN, Ode G, Jackson Iii BJ, et al. Coccygectomy for patients with chronic coccydynia: a prospective, observational study of 98 patients. Bone Joint J. 2016;98-b:526–33. [DOI] [PubMed] [Google Scholar]
- [44].Postacchini F, Massobrio M. Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx. JBJS. 1983;65:1116–24. [PubMed] [Google Scholar]
- [45].Aarby NS, Trollegaard AM, Hellberg S. Coccygectomy can be a treatment option in chronic coccygodynia. Ugeskr Laeger. 2011;173:495–500. [PubMed] [Google Scholar]
- [46].Soliman AY, Abou El-Nagaa BF. Coccygectomy for refractory coccydynia: a single-center experience. Interdiscip Neurosurg. 2020;21:100735. [Google Scholar]
- [47].Ogur HU, Seyfettinoğlu F, Tuhanioğlu Ü, et al. An evaluation of two different methods of coccygectomy in patients with traumatic coccydynia. J Pain Res. 2017:881–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Shalaby MM. The surgical role in the management of persistent coccygodynia in adolescent and pediatric patients: a retrospective case series. HSS J. 2022;18:110–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Kodumuri P, Raghuvanshi S, Bommireddy R, et al. Coccydynia – could age, trauma and body mass index be independent prognostic factors for outcomes of intervention? Ann R Coll Surg Engl. 2017;100:12–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Akşan O. Management of persistent coccygodynia and health behavior: a survey study on patients with coccygodynia of age 41 to 69 years. Am J Health Behav. 2022;46:821–33. [DOI] [PubMed] [Google Scholar]
- [51].Karadimas EJ, Trypsiannis G, Giannoudis PV. Surgical treatment of coccygodynia: an analytic review of the literature. Eur Spine J. 2011;20:698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Milosevic S, Andersen GØ, Jensen MM, et al. The efficacy of coccygectomy in patients with persistent coccydynia: a retrospective cohort study of 134 consecutive patients with a minimum follow-up of one year. Bone Joint J. 2021;103:542–6. [DOI] [PubMed] [Google Scholar]
- [53].Hodges SD, Eck JC, Humphreys SC. A treatment and outcomes analysis of patients with coccydynia. Spine J. 2004; 4:138–40. [DOI] [PubMed] [Google Scholar]
- [54].Maigne JY, Lagauche D, Doursounian L. Instability of the coccyx in coccydynia. J Bone Joint Surg Br. 2000;82:1038–41. [DOI] [PubMed] [Google Scholar]
- [55].Elkhashab Y, Ng A. A review of current treatment options for coccygodynia. Curr Pain Headache Rep. 2018;22:1–8. [DOI] [PubMed] [Google Scholar]
- [56].Doursounian L, Maigne J-Y, Jacquot F. Coccygectomy for coccygeal spicule: a study of 33 cases. Eur Spine J. 2015;24:1102–8. [DOI] [PubMed] [Google Scholar]