Abstract
The COVID-19 pandemic has profoundly impacted population well-being in the United States, exacerbating existing racial and socioeconomic inequalities in health and mortality. Importantly, as the pandemic disrupted the provision of vital preventive health screenings for cardiometabolic diseases and cancers, more research is needed to understand whether this disruption had an unequal impact across racialized and socioeconomic lines. We draw on the 2019 and 2021 National Health Interview Survey to explore whether the COVID-19 pandemic contributed to racialized and schooling inequalities in the reception of preventive screenings for cardiometabolic diseases and cancers. We find striking evidence that Asian Americans, and to a lesser extent Hispanic and Black Americans, reported decreased reception of many types of cardiometabolic and cancer screenings in 2021 relative to 2019. Moreover, we find that across schooling groups, those with a bachelor's degree or higher experienced the greatest decline in screening reception for most cardiometabolic diseases and cancers, and those with less than a high school degree experienced the greatest decline in screening reception for diabetes. Findings have important implications for health inequalities and U.S. population health in the coming decades. Research and health policy attention should be directed toward ensuring that preventive health care is a key priority for public health, particularly among socially marginalized groups who may be at increased risk of delayed diagnosis for screenable diseases.
Keywords: Population health, Social determinants of health, COVID-19, Preventive screenings, Cardiometabolic diseases, Cancers
1. Introduction
Despite substantial interest in the direct impacts of COVID-19 on U.S. health and mortality (Luck et al., 2022), less is known about the indirect ways in which the pandemic may impact population health and mortality in the long term. Preventive health screenings, such as those used to detect early stages of cancers and cardiometabolic diseases, are critical for preventing diseases and for detecting them at early stages when treatments are often most effective (Quintal and Antunes, 2022). Yet during the first quarter of 2020, U.S. healthcare facilities canceled non-urgent services to reduce the spread of COVID-19 and to preserve health care resources and personnel. These closures were recommended nationally when the Centers for Disease Control and Prevention and the Centers for Medicare and Medicaid Services published a statement in April 2020 recommending that “non-urgent procedures” be postponed (Song et al., 2021).
Thus, questions remain around whether inequalities in the uptake of health screenings occurred once health care facilities reopened for preventive care in late 2020. Specifically, it is yet unknown whether disruption in preventive screening reception caused by COVID-19 will have lasting consequences for inequalities in screening adherence along racialized and socioeconomic lines. Prior research indicates that individuals of low socioeconomic status and those racialized as non-white generally report lower preventive health care utilization rates. This may contribute to later diagnosis and poorer prognosis for a range of medical conditions that have been observed to disproportionately affect these groups (Chawla et al., 2015, Tejeda et al., 2009). Whether, and to what extent, the pandemic exacerbated these inequalities in preventive screening reception remains unknown.
To address this question, we use data from the National Health Interview Survey to investigate racialized and schooling inequalities in the reception of health screenings for several types of cardiometabolic diseases and cancers between 2019 and 2021 (which we refer to as the “peri-pandemic” period). We address the following research questions:
-
1.
How did trends in the reception of preventive health screenings for cardiometabolic diseases and cancers change between 2019 and 2021?
-
2.
Are inequalities in the reception of preventive health screenings between 2019 and 2021 observed across racialized and schooling groups?
We identify a general decline in the reception of health screenings for both cardiometabolic diseases and cancers in 2021 relative to 2019. A particularly stark decline is observed in the reception of health screenings for cardiometabolic diseases and cancers among Asian Americans, and to a lesser degree, Hispanic and Black Americans, during the peri-pandemic period. Despite significant research that finds a positive association between higher levels of schooling and reception of health screenings, we find that individuals with a bachelor's degree or higher experienced a substantial decline in the reception of screenings for some cardiometabolic diseases and cancers in 2021 compared to 2019; however, those with lower levels of education (i.e., those with less than a high school degree and those with a high school degree or GED) experienced the greatest decline in diabetes screening during the period. Our findings present some of the first nationally representative estimates to show how patterns in the reception of preventive health screenings changed during the early years of the COVID-19 pandemic, and how inequalities in the reception of a range of health screenings emerged across racialized and schooling groups. We argue that increased attention to preventive health screening trends is critical for understanding trends in population health and mortality in the coming years (Centers for Disease Control and Prevention, 2019).
2. Background
2.1. Inequalities in U.S. health and mortality
In 2019, 43% of all U.S. deaths were attributable to heart diseases and malignant neoplasms (cancers), making them the leading causes of death (National Center for Health Statistics and Heron, 2021, Mehta et al., 2020, Mokdad et al., 2003). Yet the burden of cardiometabolic diseases and cancers is unequal across race and socioeconomic status. Such inequalities are driven by sources of systemic disadvantage that profoundly shape access to resources, power, and privilege (Williams et al., 2019). Namely, systemic racism generates differential access to healthy food, safe housing, and health care among Black and Latinx individuals, resulting in their disproportionate risk for developing cardiometabolic diseases (Daviglus et al., 2012, Viruell-Fuentes et al., 2012). Direct exposure to interpersonal discrimination has also been found to contribute to poorer cardiometabolic health among Black, Latinx, and Asian Americans (Viruell-Fuentes et al., 2012, Williams et al., 2019, Yoo et al., 2009).Williams et al., 2019
Cancer morbidity and mortality also vary significantly across racialized groups. Breast cancer is the leading cause of cancer among women in the United States (Islami et al., 2018), but Black women are more likely than white women to be diagnosed with later stages of the disease and to die from it (Jatoi et al., 2022, Roberts, 2011). Although Asian American women demonstrate a lower incidence of breast cancer than white, Black, and Latinx women, it is the leading cause of death among Asian American women (Gomez et al., 2010). Cervical cancer also remains a significant cause of unequal morbidity and mortality among U.S. women (Yoo et al., 2017), with incidence and mortality among Latinx women being twice that of white women (O'Brien et al., 2010). Despite the lower incidence of cervical cancer among Asian women compared to Latinx and Black women, they are more likely to be diagnosed with later stages of the disease (Wang et al., 2008).
Similar inequalities are observed among cancers affecting men. Black, Latinx, and Asian men are more likely to be diagnosed with late-stage prostate cancer, resulting in poorer disease prognosis (Siegel et al., 2021). Additionally, among men and women, colorectal cancer is the third most diagnosed cancer, with Black Americans having the highest incidence and mortality rates compared to non-Latinx white, Latinx, and some subgroups of Asian Americans (Zavala et al., 2021).
Socioeconomic status is also strongly associated with morbidity and mortality from cardiometabolic diseases and cancers. Schooling level, an important indicator of socioeconomic status, may impact health by providing individuals of higher schooling with greater access to resources and knowledge that improves health and well-being (Di Cesare et al., 2013, Elo et al., 2006). Those with higher levels of schooling often have access to better housing, food, and health insurance, and are more likely to have well-informed social networks that encourage positive health behaviors. Those with lower levels of schooling may be more likely to engage in negative health behaviors, including smoking, substance abuse, and consumption of unhealthy foods, which are important mediators of the relationship between schooling and cardiometabolic diseases and some cancers (Mouw et al., 2008, Shiovitz-Ezra and Litwin, 2012).
2.2. Inequalities in preventive health care utilization
Despite the significant burden of cardiometabolic diseases and cancers in the United States, many of these diseases are preventable (or can be detected in earlier stages of their progression) through routine preventive health screenings. Still, access to and utilization of these services varies across race and socioeconomic status. Research finds that Black, Asian, and Latinx Americans are less likely than white Americans to have access to and receive regular health screenings (Dubay and Lebrun, 2012). Similarly, individuals of lower socioeconomic status are generally less likely to receive regular hypertension and cholesterol screenings compared to their high socioeconomic status counterparts (Shahu et al., 2021).
Moreover, according to the Centers for Disease Control, Latinx and Asian women are least likely among racialized groups to receive cancer screenings, such as those for cervical cancer, compared to Black and white Americans (Peralta et al., 2015). Furthermore, Asian women are less likely to receive breast cancer screenings compared to other racialized groups of women (Chawla et al., 2015). Black men are disproportionately less likely to obtain screening for prostate cancer, and are more likely to experience delayed diagnoses and poorer prognoses for the disease (Zavala et al., 2021). Further, research shows that not only are Black Americans less likely to receive colorectal cancer screenings than white Americans, but that this inequality is a key driver of the higher colorectal cancer mortality rates observed among Black Americans (Rutter et al., 2021).
Those with higher levels of schooling may have better access to and greater utilization of preventive health care (Elo et al., 2006). Formal schooling can potentially enhance the use of preventive health services as it increases awareness of the vital importance of screening for preventable health conditions. Studies show that the likelihood of obtaining breast, cervical, colorectal, and prostate cancer screenings increases with schooling and income (Gornick et al., 1996, Sabates and Feinstein, 2006). Because of this, cancer survival rates are higher for those of higher socioeconomic status who are diagnosed and treated early in the progression of their disease (Fiva et al., 2014).
3. Data and methods
3.1. Data
Our analyses draw on data from the 2019 and 2021 survey rounds of the National Health Interview Survey (NHIS), the oldest ongoing health survey in the United States. The NHIS conducts around 30,000 interviews annually, producing a nationally representative sample of the non-institutionalized civilian population. It collects vital information on health care and health outcomes, making it the ideal data source to explore preventive health care trends.
We investigate how preventive health screenings for cardiometabolic diseases and cancers changed in the peri-pandemic period. We explore trends in screenings for: 1) hypertension (measured via an automated or manual blood pressure test), 2) high cholesterol (via a blood draw), 3) diabetes (via a blood draw hemoglobin A1C test), 4) breast cancer (via a radiological test known as mammography), 5) cervical cancer (via a Papanicolaou (PAP smear) test or an HPV test), 6) prostate cancer (measured via a blood draw measuring prostate-specific antigen known as a PSA test), and 7) colorectal cancer (measured via procedural tests such as colonoscopy, sigmoidoscopy, or CT colonography).
We restrict our sample to 35,945 NHIS respondents aged 40 to 75. The following factors informed this definition of the analytical sample age range. For cardiometabolic screenings, ages 40–75 fall within the recommended screening age range put forth by the United States Preventive Screening Taskforce (USPSTF). For mammogram screenings, although the USPSTF recommends mammography screening begin at age 50 (Ren and Feagin, 2021), women often begin breast cancer screening at age 40 in accordance with guidelines from the American Cancer Society. For prostate cancer, the USPSTF recommends that men aged 55 to 69 discuss the decision to undergo periodic screenings with their health care provider and that the decision to undergo such screenings should occur on an individual, case-by-case basis. Despite the lack of population-level screening recommendations for prostate cancer, we include individuals between 40 and 75 in our analyses as the NHIS asks respondents about prostate cancer screening beginning at age 40. For colorectal cancer, the USPSTF recommends that all adults above age 45 be screened every 5–10 years (Ponce et al., 2022). Similar to our prostate cancer screening analyses and based on the NHIS questionnaire, we include individuals between 40 and 75 in our colorectal cancer screening analyses as this reflects the age range for which the NHIS asks respondents to report colorectal cancer screening reception.
Of these 35,945 respondents, we excluded those who were pregnant (n = 16), as pregnant people are often ineligible for cancer screening exams. We also excluded respondents who were missing information on education or sex (n = 1,240) and those who identified their race-ethnicity as American Indian/Alaskan Native, other, or multiracial (n = 778) due to small sample sizes for respondents who reported these identities. Finally, we excluded 1,226 respondents who were missing information on whether they received cardiometabolic screenings. The resulting analytical sample is 32,685 respondents, consisting of 17,557 women and 15,128 men.
For our analyses of cancer screening uptake in 2019 and 2021, we excluded respondents who were missing information on whether they obtained cancer screening exams (n = 1,224). Moreover, we excluded individuals who received diagnostic exams, given the focus of this article on COVID-19's impact on routine preventive care (n = 1,672).
Finally, we excluded respondents from the cervical cancer subsample who reported having had a hysterectomy (n = 746). Our final sample sizes for cancer-specific analyses are as follows: 16,806 women for mammograms; 16,197 women for cervical cancer screenings; 13,832 men for prostate cancer screenings; and 16,794 women and 14,613 men for colorectal cancer screenings.
3.2. Variables
Key outcomes measure variation in the reception of several preventive health screenings for cardiometabolic diseases and cancers. These exams fall across a “complexity continuum,” meaning that whereas some screenings (including hypertension screenings) are relatively simple to conduct and are often completed routinely during outpatient visits, other, more complex screenings (including mammography and colorectal cancer screenings) require advanced scheduling and more time and preparation from patients to complete. As more complex exams require more time and planning to undergo, they are more susceptible to scheduling backlogs, which may have prevented prompt uptake of these screenings when health care facilities were once again open to patients in late 2020 (Fedewa et al., 2022).
Our first set of outcomes explores trends in the reception of screening exams for three cardiometabolic risk factors and diseases - hypertension, high cholesterol, and diabetes - within a one-year period. Our second set of outcomes investigates trends in the reception of cancer screenings - breast, cervical, prostate, and colorectal - within a one-year period. Our key independent variables include a categorical measure of respondent-reported race (white; Black; Hispanic; Asian) and a categorical measure of respondents' highest degree of schooling (less than high school; high school degree/GED; associate's degree; bachelor's degree or higher).
Racial categories are taken directly from the NHIS survey question asking respondents to identify their race and Hispanic ethnicity. For our schooling variable, we combined the original NHIS schooling categories, “never attended school; grades 1–11; 12th grade, no diploma” into the category “less than high school”; “high school or equivalent, and some college but no degree” into “high school degree or GED”; “technical or vocational associate's degree and academic associate degree” into “associate's degree”; and finally, “bachelor's, master's, and professional/doctoral degree” into “bachelor's degree or higher.”
We include several relevant controls in our regression analyses to adjust for factors that may impact trends in preventive health screenings among racialized and schooling groups of individuals. The first control is a categorical measure of age. We include this control to account for the fact that the likelihood of individuals obtaining preventive screenings may vary by age; specifically, research shows that older adults are less likely to obtain many types of preventive health screenings relative to young and mid-age adults (Kim et al., 2014). Second, we include a categorical measure of U.S. census region of residence (Northeast; Midwest; South; West) to account for potential geographic heterogeneity in preventive health screening availability and reception between 2019 and 2021. This control is also important to include because of the substantial variation in COVID-19 burden across U.S. regions during the study period.
Third, we include a binary measure of whether respondents reported having any health insurance coverage, an important determinant of financial access to care that may drive the likelihood of an individual accessing health services such as preventive health screenings. Finally, we include a binary measure of whether respondents had ever been diagnosed with any of the conditions or diseases for which we explore trends in screening reception (hypertension; high cholesterol; diabetes; breast cancer; cervical cancer; prostate cancer; or colorectal cancer). We include this control in our models because individuals with a history of these diseases may be more likely to obtain preventive health screenings. On the other hand, individuals who were ever diagnosed with a cardiometabolic or cancer comorbidity may have reduced their use of health care services during the pandemic, as screening for these conditions required interaction with the health care system, potentially putting them at greater risk for contracting COVID-19.
3.3. Methods
We first present weighted sex-stratified summary statistics for the entire study sample. We then estimate sex-stratified logistic regression models by maximum likelihood estimation, separately for women and men and for each screening outcome. The models estimate the probability of receiving preventive health screenings in 2019 and 2021 for different racialized and schooling groups. The basic form of the model equation is shown below:
| logit(p) = log(p/1-p) = β0 + β1 Yeari + β2 Xi + β3 Yeari * Xi + β4 Zi |
where p is the probability of y being equal to 1 (p = P(Y =1)), and Y is a binary outcome variable, where 1 indicates that an individual received a screening and 0 indicates that they did not receive a screening for a particular disease or condition. Yeari refers to the survey year (2019 or 2021, where 2019 is the pre-pandemic indicator). Xi represents racialized or schooling categories of respondents. Zi refers to the vector of control variables. We also include an interaction term between Yeari and Xi since the effects associated with screening can vary by racialized or schooling categories of respondents. We present the average marginal effects of the peri-pandemic period (2019 and 2021) on the probability of receiving a screening for each racialized or schooling category of respondents.
4. Results
4.1. Summary statistics
Table 1 presents weighted sex-stratified summary statistics for the analytical sample (n = 32,685 respondents aged 40–75). On average, women were 57 years old, and men were 56 years old at the time of survey response. The racial distribution of men and women was similar; both men and women largely identified as white (69% for men, 67% for women), followed by Black (10% versus 12%), Hispanic (15% for each), and Asian (6% for each). The majority of men and women had either a high school/GED degree (42% versus 41%, respectively) or a bachelor's degree or higher (35% for each) at the time of survey response. Finally, 62% of men and 58% of women reported having ever been diagnosed with a comorbidity for which screening behaviors were explored in this article (i.e., hypertension, high cholesterol, diabetes, breast cancer, cervical cancer, prostate cancer, or colorectal cancer).
Table 1.
Summary statistics for men and women aged 40 to 75 years
| Men | Women | |
|---|---|---|
| Age (mean) | 56 | 57 |
| Racial categories(%) | ||
| White | 69 | 67 |
| Black | 10 | 12 |
| Hispanic | 15 | 15 |
| Asian | 6 | 6 |
| Highest degree of schooling obtained (%) | ||
| Less than high school | 11 | 10 |
| High school or GED | 42 | 41 |
| Associate's Degree | 12 | 14 |
| Bachelor's degree or higher | 35 | 35 |
| Census region(%) | ||
| Northeast | 18 | 18 |
| Midwest | 21 | 21 |
| South | 38 | 39 |
| West | 23 | 22 |
| Has health insurance (%) | 91 | 93 |
| Ever diagnosed with cardiometabolic or cancer comorbidity (%) | 62 | 58 |
Notes: Weighted estimates using 2019 and 2021 National Health Interview Survey. The sample consists of 17,557 women and 15,128 men. “Ever diagnosed with a comorbidity” refers to whether a respondent was ever diagnosed with any of the following conditions: high cholesterol, diabetes, hypertension, or cervical, breast, prostate, or colorectal cancer.
4.2. Changes in the reception of preventive health screenings during the peri-pandemic period
Appendix A, Table A1, presents average marginal effects (AME) calculated from models estimating changes in screening reception among men and women in 2021 relative to 2019. Estimates show that generally, reception of all types of cardiometabolic and cancer screenings decreased between 2019 and 2021. On average, declines in the reception of cancer screenings were more minimal than those in the reception cardiometabolic screenings for both men and women. In particular, the greatest decline in screening reception is observed for diabetes screenings; both men and women experienced an 18 percentage point (“p.p.”) (CI = -0.19.0, -0.16 for women; CI = -0.20, -0.16 for men) decrease in screening reception in 2021 relative to 2019.
4.3. Racialized inequalities in the reception of preventive health screenings
4.3.1. Cardiometabolic screenings
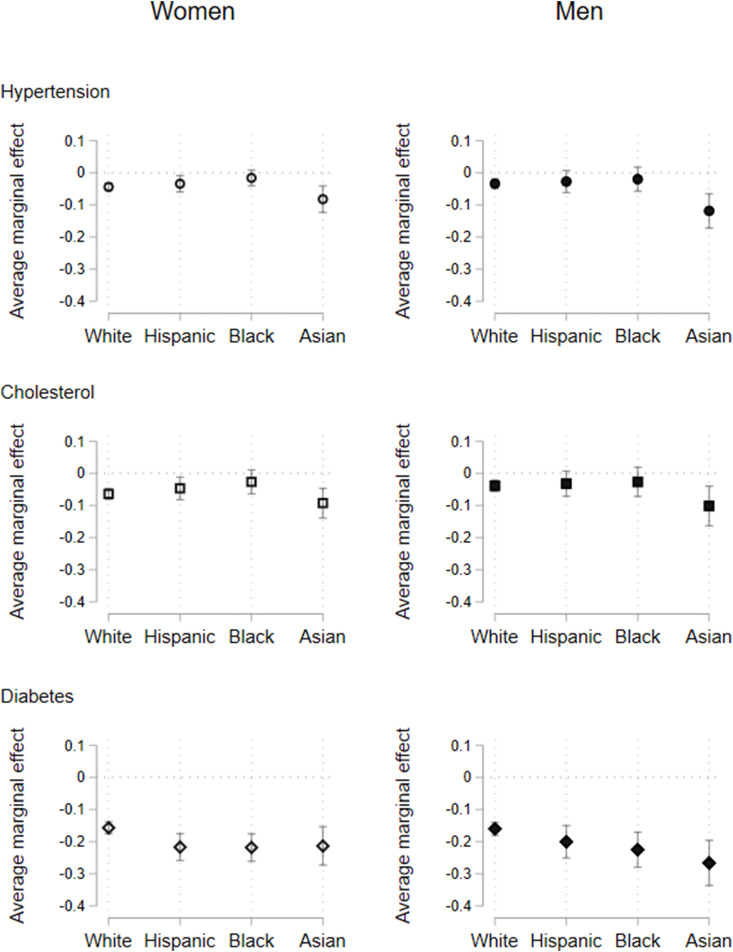
Fig. 1 presents AME calculated from models that were estimated using the model equation for each type of cardiometabolic health screening, and for women and men separately. The results describe the association between the survey year (i.e., 2019 or 2021) and the probability of receiving hypertension, cholesterol, or diabetes screenings for each racialized group. The left panel of graphs in Fig. 1 illustrates findings estimated for the sample of women, and the right panel presents findings for the sample of men. We present average marginal effects in the main body of this article, as we estimate a non-linear model with interaction terms (Ai and Norton, 2003). Model coefficients are provided in Appendix B, Table B1 and Table B2. All figures include 95% confidence intervals.
Fig. 1.
Changes in the reception of cardiometabolic screenings between 2019 and 2021, for women and men by race
Note: Sample consists of women and men aged 40 to 75. All models include sample weights and controls for age, health insurance, census region, and ever diagnosed with a cardiometabolic or cancer comorbidity. Figures plot average marginal effects with 95% C.I. calculated from logistic regression models.
The results for women show that compared to the pre-pandemic period (2019), white women were 4 p.p. (CI = -0.06, -0.03), Asian women were 8 p.p. (CI = -0.12, -0.04), Hispanic women were 3 p.p. (CI = -0.06, -0.01), and Black women were 2 p.p. (CI = -0.04, 0.01) less likely to receive a hypertension screening in 2021. We observe a similar pattern for cholesterol screenings, with decreases of 6 p.p. (CI = -0.08, -0.05) for white women, 9 p.p. (CI = -0.14, -0.05) for Asian women, 5 p.p. (CI = -0.08, -0.01) for Hispanic women, and 3 p.p. (CI = -0.06, 0.01) for Black women. However, for diabetes screenings, we see larger decreases at 16 p.p. (CI = -0.18, -0.14) among white women, 21 p.p. (CI = -0.27, -0.15) among Asian women, 22 p.p. (CI = -0.26, -0.18) among Hispanic women, and 22 p.p. (CI = -0.26, -0.18) among Black women in 2021 compared to 2019.
The right panel of Fig. 1 presents results for men. The results show small declines in the reception of hypertension and cholesterol screenings, and only among white and Asian men. However, there are large declines in the reception of diabetes screenings: 16 p.p. (CI = -0.18, -0.14) for white men, 27 p.p. (CI = -0.34, -0.20) for Asian men, 20 p.p. (CI = -0.25, -0.15) for Hispanic men, and 22 p.p. (CI = -0.28, -0.17) for Black men.
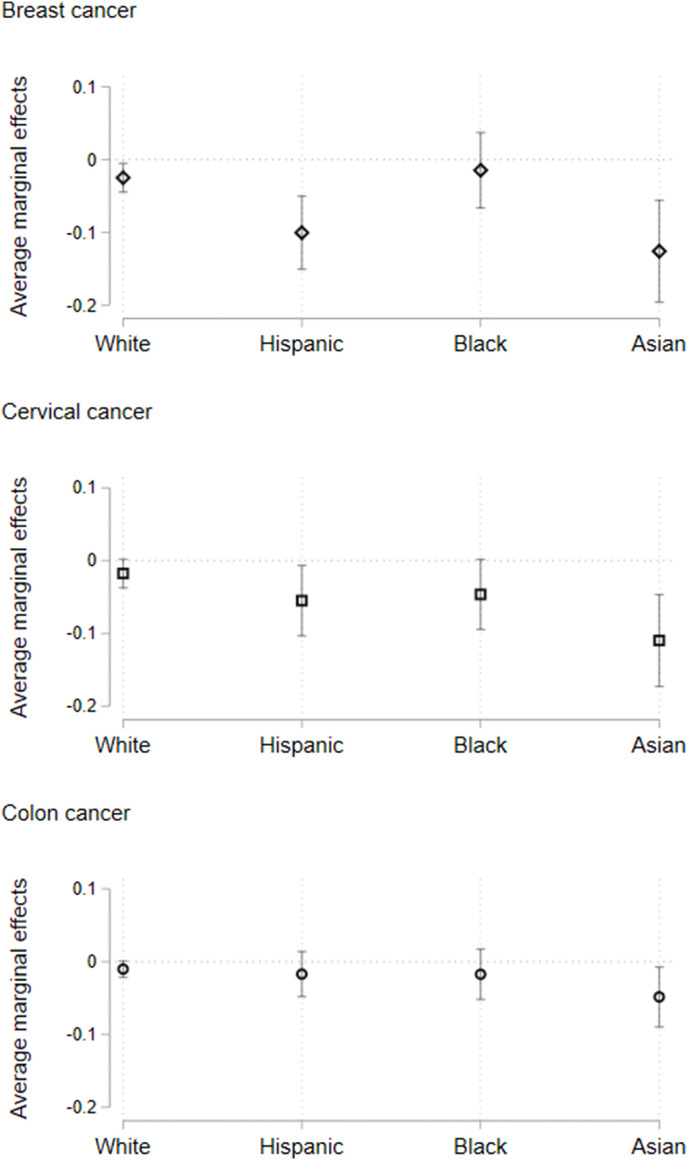
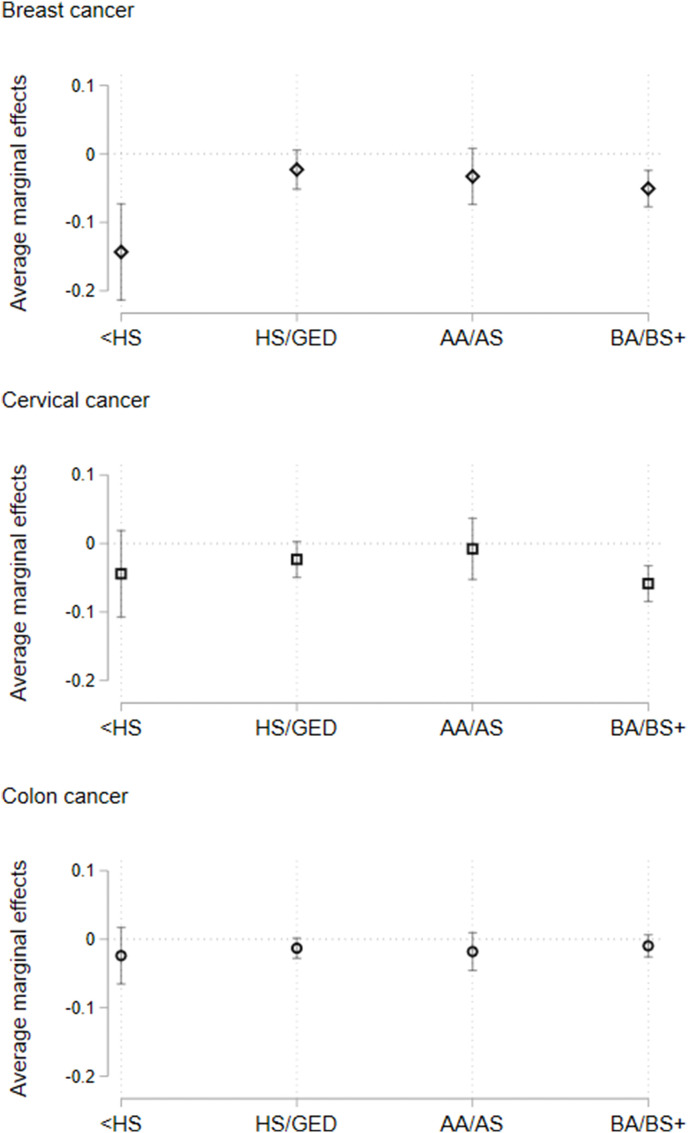
4.3.2. Cancer screenings
Fig. 2 presents the average marginal effects for models estimating changes in the reception of cancer screenings among women during the study period. The results describe the association between the peri-pandemic period and the probability of receiving mammograms, cervical cancer screenings, and colorectal cancer screenings for each racialized group of women. Model coefficients are presented in Appendix B, Table B3. For mammogram screenings, a large decline in reception is observed among Asian women (13 p.p., CI = -0.20, -0.06) and Hispanic women (10 p.p., CI = -0.15, -0.05) in 2021 compared to 2019. White women, however, experienced only a small decline in the reception of mammogram screenings. For cervical cancer screenings, Asian women (11 p.p., CI = -0.17, -0.05) again experienced a large decline in reception in 2021 relative to 2019, and Hispanic women experienced a smaller decline (5 p.p., CI = -0.10, -0.01). Finally, for colorectal cancer screenings, a modest decline in reception is observed for Asian women (5 p.p., CI = -0.09, -0.01).
Fig. 2.
Changes in the reception of cancer screenings between 2019 and 2021, for women by race.
Note: Sample consists of women and men aged 40–75. All models include sample weights and controls for age, health insurance, census region, and ever diagnosed with a cardiometabolic or cancer comorbidity. Figures plot average marginal effects with 95% C.I. calculated from logistic regression models.
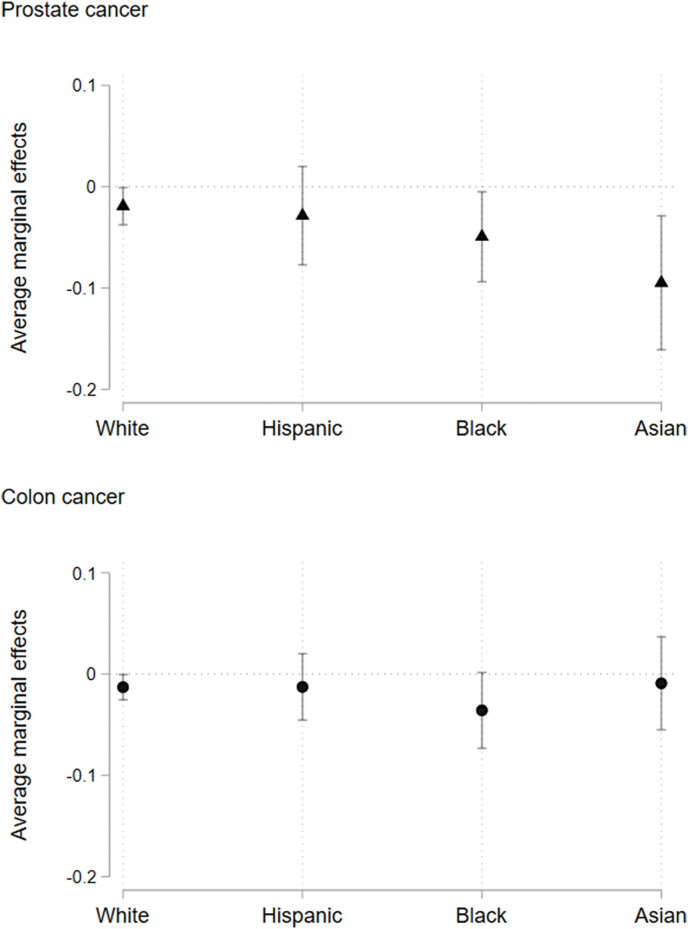
Fig. 3 presents average marginal effects describing the association between the peri-pandemic period and the probability of receiving prostate and colorectal cancer screenings for racialized groups of men (coefficients shown in Appendix B, Table B4). Compared to the pre-pandemic period, Asian men (9 p.p., CI = -0.16, -0.03) are observed to experience a large decline in prostate cancer screening reception in 2021. For Black men (5 p.p., CI = -0.09, -0.00), we observe a small decline in the reception of prostate cancer screening during the study period. We do not see clear patterns of change in the reception of colorectal cancer screenings among men between 2019 and 2021.
Fig. 3.
Changes in the reception of cancer screenings between 2019 and 2021, for men by race
Note: Sample consists of women and men aged 40–75. All models include sample weights and controls for age, health insurance, census region, and ever diagnosed with a cardiometabolic or cancer comorbidity. Figures plot average marginal effects with 95% C.I. calculated from logisitc regression models.
4.4. Schooling inequalities in the reception of preventive health screenings
4.4.1. Cardiometabolic screenings
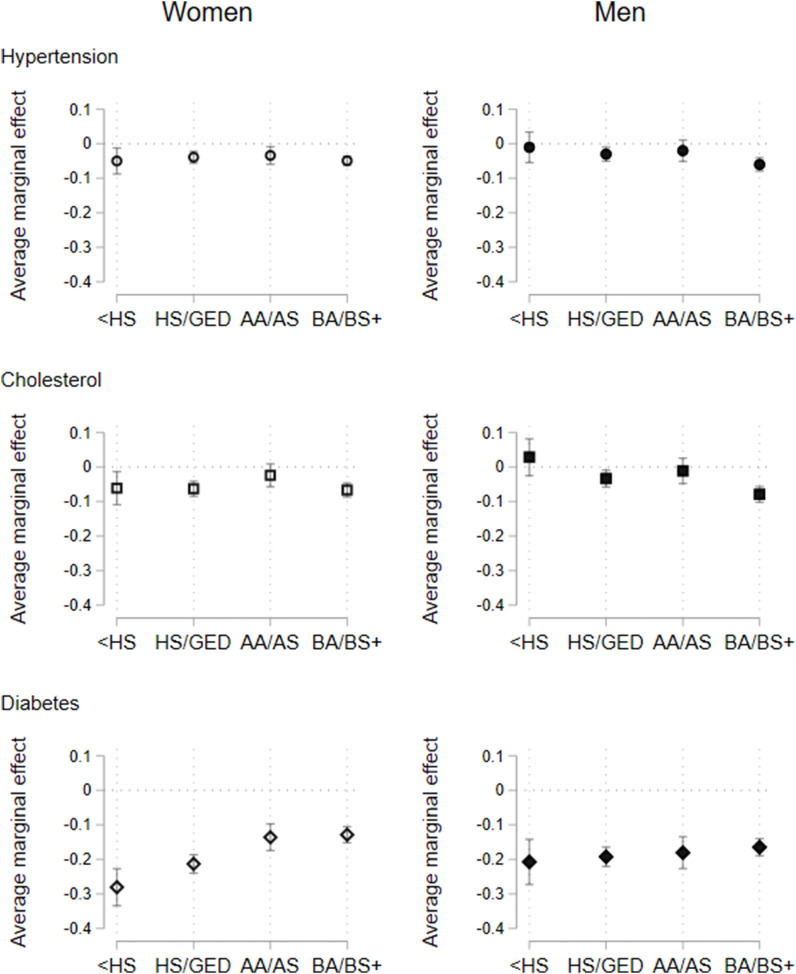
Fig. 4 presents the change in the reception of hypertension, cholesterol, and diabetes screenings in 2021 compared to 2019 for different schooling groups of respondents. As in the previous section, the left panel of graphs presents findings for women, and the right panel presents findings for men. Model coefficients are shown in Appendix B, Table B5, and Table B6.
Fig. 4.
Changes in the reception of cardiometabolic screenings between 2019 and 2021, for women and men by schooling group
Note: Sample consists of women and men aged 40–75. All models include sample weights and controls for age, health insurance, census region, and ever diagnosed with a cardiometabolic or cancer comorbidity. Figures plot average marginal effects with 95% C.I. calculated from logistic regression models. <HS - Less than high school; HS - High school degree/GED; AA/AS - Associate of Arts (AA) or Science (AS); BA/BS+ - Bachelor's degree or higher.
Reception of hypertension screenings decreased in 2021 compared to 2019 for men (6 p.p., CI = -0.08, -0.04) and women (5 p.p., CI = -0.06, -0.04) with a bachelor's degree; for men (3 p.p., CI = -0.05, -0.01) and women (4 p.p., CI = -0.06, -0.02) with a high school degree or GED; and for women (5 p.p., CI = -0.09, -0.01) with less than a high school degree. Similar patterns of decline are observed in the reception of cholesterol screenings. For diabetes screenings, a large decline is observed across each schooling category of men and women. Reductions in diabetes screening ranged from 28 p.p. (CI = -0.33, -0.23) for women with less than a high school degree to 13 p.p. (CI = -0.15, -0.11) for women with a bachelor's degree or higher. For men, the range of decline varied from 21 p.p. (CI = -0.27, -0.14) for those with less than a high school degree, to 16 p.p. (CI = -0.19, -0.14) for men with a bachelor's degree or higher.
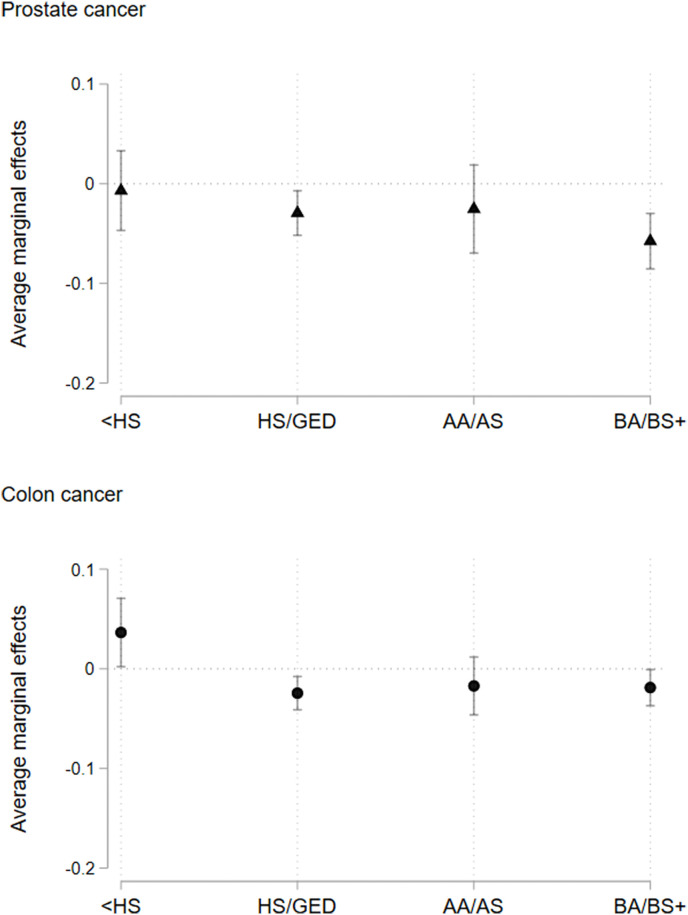
4.4.2. Cancer screenings
Fig. 5 (and corresponding models in Appendix B, Table B7) shows that compared to the pre-pandemic period, decreased reception of mammogram screenings is observed for women with a bachelor's degree or higher (5 p.p., CI = -0.08, -0.02) in 2021. We also observe a particularly large decline in mammogram screening reception for women with less than a high school degree (14 p.p., CI = -0.21, -0.07). In terms of cervical cancer screenings, only women with a bachelor's degree or higher are observed to experience a decline in screening reception during the peri-pandemic period (6 p.p., CI = -0.08, -0.03). Finally, for colorectal cancer screenings, we do not observe clear changes in screening reception across schooling categories of women.
Fig. 5.
Changes in the reception of cancer screenings between 2019 and 2021, for women by schooling group
Note: Sample consists of women and men aged 40–75. All models include sample weights and controls for age, health insurance, census region, and ever diagnosed with a cardiometabolic or cancer comorbidity. Figures plot average marginal effects with 95% C.I. calculated from logistic regression models. <HS - Less than high school; HS - High school degree/GED; AA/AS - Associate of Arts (AA) or Science (AS); BA/BS+ - Bachelor's degree or higher.
Fig. 6 (and corresponding models in Appendix B, Table B8) presents findings for men of different schooling groups. For prostate cancer screening, men with a bachelor's degree or higher are observed to experience a decline in screening reception in 2021 compared to 2019 (6 p.p., CI = -0.09, -0.03). For colorectal cancer screenings, we observe a marginal increase in screening reception among men with less than a high school degree (4 p.p., CI = 0.00, 0.07), and a marginal decline in screening reception among men with a high school degree or GED (2 p.p., CI = -0.04, -0.01).
Fig. 6.
Changes in the reception of cancer screenings between 2019 and 2021, for men by schooling group
Note: Sample consists of women and men aged 40–75. All models include sample weights and controls for age, health insurance, census region, and ever diagnosed with a cardiometabolic or cancer comorbidity. Figures plot average marginal effects with 95% C.I. calculated from logistic regression models. <HS - Less than high school; HS - High school degree/GED; AA/AS - Associate of Arts (AA) or Science (AS); BA/BS+ - Bachelor's degree or higher.
5. Discussion
Our analyses identify salient changes in the association between the reception of preventive health screenings and key indicators of social stratification (race and schooling) during the peri-pandemic period. Despite many health care facilities re-opening for outpatient screenings after the first quarter of the pandemic, our analyses reveal that both men and women were generally less likely to report obtaining screenings for both cardiometabolic diseases and cancers in 2021 compared to 2019. In exploring racialized inequalities in the reception of cardiometabolic screenings, our results indicate that hypertension, cholesterol, and diabetes screenings declined in 2021 relative to 2019 among Asian men and women, and to a lesser degree, among Black and Hispanic men and women. For cancer screenings, Hispanic and Asian women were less likely to obtain mammograms and cervical cancer screenings in 2021 than in 2019. However, only Asian women were less likely to obtain colorectal cancer screenings. Asian men, and to a lesser degree, Black men, experienced decreased screening for prostate cancer in 2021 relative to 2019.
Results around schooling inequalities in screening reception indicate that men and women with a high school degree or GED, and those with a bachelor's degree or higher, experienced the greatest changes in hypertension and cholesterol screening reception in 2021 compared to 2019. Moreover, for diabetes screenings, men and women across all schooling groups experienced decreased screening uptake. Still, those with the lowest levels of education (i.e., those with less than a high school degree and those with a high school degree or GED) experienced the greatest magnitude of decline in diabetes screening reception in 2021. Schooling inequalities in cancer screenings show that among women and men, those with a bachelor's degree or higher were generally more likely to report decreased reception of screenings in 2021 compared to 2019 (i.e., for prostate, breast, and cervical cancer screenings). Additionally, men with a high school degree or GED were less likely to obtain a prostate cancer or colorectal cancer screening, and women with less than a high school degree were less likely to obtain a mammogram, in 2021 than in 2019.
Our findings indicate that, in particular, the screening uptake of Asian Americans appears to have been significantly impacted during the pandemic. We hypothesize that several factors may explain this finding. Notably, literature identifies that prior to the pandemic, preventive health screening adherence was already a significant issue among Asian Americans for numerous cancers, including cervical, breast, and prostate (Nghiem et al., 2016, Peralta et al., 2015, Tejeda et al., 2009, Trinh et al., 2016). Our findings that Asian Americans reported significantly decreased reception of cervical, breast, and prostate cancer screenings during the pandemic might reflect a continuation of these pre-pandemic trends. Such estimates are concerning, as breast and cervical cancers are leading causes of mortality among Asian American women, and prostate cancer remains the most diagnosed cancer among Asian men (Trinh et al., 2016).
Findings that identify declines in the reception of diabetes screening among most racialized groups of individuals between 2019 and 2021 are particularly concerning from a population health standpoint. Whereas diabetes has remained a substantial health concern among Black and Hispanic Americans over the past several decades (Katz et al., 2021), the prevalence of the disease is also increasing among Asian Americans (Echeverria et al., 2017). Our findings that these groups reported particularly decreased diabetes screening uptake in 2021 have important implications for widening inequalities in diabetes morbidity. Again, these findings may be contextualized as a continuation of pre-pandemic screening trends, as research demonstrates that Asian Americans, and in particular, those who have already been diagnosed with diabetes, have lower adherence to preventive exams, including daily blood glucose checks and routine eye and feet exams for the disease (Kim et al., 2012).
Another potential explanation for our findings that Asian Americans exhibited lower rates of screening reception for numerous cardiometabolic conditions and cancers is rooted in the racial and sociopolitical climate in the United States during the pandemic. Research finds that during the pandemic, Asian Americans reported increased stress and heightened awareness and experiences of racism and xenophobia that were associated with delayed health care utilization and avoidance of health care services altogether (Ponce et al., 2022, Ren and Feagin, 2021, Yoo et al., 2009Yoo et al., 2009). Thus, it is also possible that low screening levels among Asian Americans pre-pandemic may have been exacerbated by widespread fear that seeking health care during the pandemic would put them at greater risk of experiencing discrimination or violence.
Finally, another important barrier to the re-uptake of preventive health screenings during the pandemic was the likelihood that individuals faced difficulties in obtaining appointments for these screenings. As virtually all appointments for routine screening exams were canceled in the first quarter of the pandemic, once facilities re-opened for appointments, many patients likely faced immense backlogs that prevented them from rescheduling exams in a timely manner. Notably, scheduling and appointment backlogs may have disproportionately affected urban and rural health clinics, community hospitals, and less well-resourced health care facilities that are more likely to serve individuals of color, immigrants, and low-income individuals (Fisher-Borne et al., 2021). This may explain why our results show lower rates of preventive screening reception among Hispanic and Asian Americans and may also explain why we find that women with less than a high school degree were less likely to obtain mammogram screenings in 2021. Current interventions, such as the American Cancer Society's “Back on Track with Screening" quality improvement program, are working to reduce backlogs and promote outreach to patients about returning to routine screenings (Fisher-Borne et al., 2021). Still, it has yet to be identified whether, and for whom, such interventions will be effective.
Our findings around the effect of schooling level on the reception of screening exams between 2019 and 2021 reveal intriguing trends in preventive health care utilization among both men and women. During the pandemic period, we find that those with a bachelor's degree or higher were most likely to report decreased reception of a host of screening exams. These findings are perhaps puzzling, as research suggests that individuals with higher levels of schooling are more likely to obtain routine health screenings compared to those with lower levels of schooling (Di Cesare et al., 2013, Documet et al., 2015), perhaps due to greater awareness of the health benefits of receiving routine screenings (Lange, 2011). During the pandemic, however, individuals with higher levels of schooling may have decided that the risk of contracting COVID-19 outweighed the benefits of obtaining timely screenings. Moreover, given research that finds those with higher levels of schooling are generally observed to have a health advantage over those with lower levels of schooling (Elo et al., 2006, Kavanagh et al., 2010), our findings may reflect that those with a higher degree of schooling were more likely to delay screening if they were generally of better health and thus perceived a lower need for preventive health screenings during the pandemic period. However, given that our study period extends only until 2021, we are unable to determine whether the observed declines represent a temporary delay in screening reception, or altogether forgone screening, for this group.
Moreover, of particular concern is that overall, individuals with less than a high school degree and those with a high school degree or GED experienced the greatest declines in reception of diabetes screenings between 2019 and 2021. This finding has concerning implications for population health, as research suggests that those with lower levels of schooling (and those of low socioeconomic status) have the highest prevalence of, and are at greater risk for, developing diabetes and diabetes-related complications (Di Cesare et al., 2013).
5.1. Limitations
Strengths of the current analyses include the nationally-representative nature of the data analyzed, as well as the robust set of screening examinations that span various types of both cardiometabolic diseases and cancers. Our analyses, therefore, make an important contribution to the current literature on disrupted preventive health screen-ings during the COVID-19 pandemic, which have tended to draw on data from clinical samples specific to individual health systems, and which have often focused on exploring changes in one, specific type of preventive health screening. Despite these strengths, however, several data limitations warrant attention in future research. First, due to changes in the structure of the NHIS survey between 2018 and 2019, NHIS data from 2019 to 2021 cannot be compared to earlier years of data collection, meaning that we cannot explore longer-term trends in preventive health screenings (Centers for Disease Control and Prevention, 2019).
Second, we cannot explore trends in preventive screening reception across specific subgroups of Asian and Hispanic Americans due to how the NHIS reports information about respondent race-ethnicity. As such, we cannot parse out whether certain ancestry groups (e.g., Chinese Americans, South Asian Americans, Mexican Americans, etc.) are reporting the greatest decline in the uptake of screenings in the era post-pandemic. Similarly, due to a lack of information regarding the number of years an individual has lived in the United States, we cannot disentangle further the effect of generational status on the uptake of screening exams.
Third, although we hypothesize that lower screening rates among Asian Americans in 2021 may reflect increased fear of experiencing anti-Asian violence or discrimination, we cannot directly test this potential mechanism, as the NHIS does not ask respondents about experiences of discrimination. Finally, our analyses are descriptive in nature, and further research is needed to measure whether there was a causal impact of COVID-19 on trends in health screening uptake.
6. Conclusion
The COVID-19 pandemic will undoubtedly have a lasting impact on the health and well-being of the U.S. population. Our study provides nationally representative estimates to demonstrate how inequalities in preventive health screenings unfolded for a series of cardiometabolic diseases and cancers during the early pandemic years. Future research using data collected during the tail-end of the COVID-19 pandemic (from 2022 onward) is needed to continue investigating whether decreased screening uptake during the pandemic persisted into the future, and for whom. More attention must also be directed toward further disentangling health and health care inequalities among Asian and Hispanic populations at the national level, as these racialized groups are growing in demographic importance in the United States (Frey, 2018).
Findings from our analyses have important implications for health policy and clinical practice. Critically, policymakers, health care administrators, and health care providers must emphasize and prioritize safe ways to resume screening exams in the post-pandemic era. Delayed or forgone preventive health care during the pandemic may result in increased demand for screening (and reduced capacity to screen) patients, particularly in regions of the United States that are still recovering from high rates of COVID-19 infection, and whose health care providers and systems were particularly taxed by the pandemic. Re-assessing the daily operations of health care systems to enhance and streamline patient care will be vital in the coming years (Song et al., 2021).
Moreover, health care providers and health systems should continue to emphasize the importance of adherence to preventive health screening recommendations for their patient populations. This may be achieved through increased hiring of certain roles of providers and staff (e.g., community health workers and social workers) to contact patients who may be delayed in obtaining screening exams. Additionally, whereas the screening exams explored in this article cannot be administered remotely via telehealth, telehealth may play an important role in ensuring patients have access to a health care provider with whom to discuss the benefits of obtaining timely screenings. Specifically, telehealth may help health care providers engage with vulnerable patient populations who face transportation, cost, and/or logistical barriers to accessing care.
Furthermore, agencies that fund health research should also prioritize funding projects that aim to intervene in and improve uptake of preventive health screenings. Prioritized projects should aim to ensure that groups who were most disadvantaged by the pandemic (e.g., those who are racially and socioeconomically minoritized) are able to safely and easily resume screenings. For example, the “Back on Track with Screening" quality improvement program (funded by the American Cancer Society) is just one of many important efforts being implemented toward ensuring patients obtain preventive screening exams in a timely manner.
Finally, substantially less attention has been given to investigating Asian-white and Hispanic-white health and health care inequalities compared to Black-white health and health care inequalities, which should be remedied in research, policy, and practice as the demographic composition of the United States continues to diversify. Greater policy attention must be directed toward the health of Asian and Hispanic Americans, as reduced utilization of health screenings during the pandemic may render them more susceptible to delayed diagnoses for screenable diseases in the post-pandemic era. Over time, and as new waves of NHIS data are collected and linked to mortality records, research must directly assess how health care-seeking behaviors and health care utilization patterns observed during the pandemic are associated with future morbidity and mortality from cardiometabolic diseases and cancers.
Funding statement
This research was supported by the NIH National Institute on Aging (NIA) under grant award T32AG000243 (PI: David Meltzer, MD, PhD). Its contents are solely the responsibility of the author(s) and do not necessarily represent the official views of the NIA.
Acknowledgments
We thank the editors and anonymous reviewers for their helpful comments and feedback. We are additionally grateful to Allison Dunatchik and Eugenio Paglino for their helpful suggestions to improve our manuscript.
Handling Editor: Social Epidemiology Editorial Office
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2023.116003.
Appendix A and Appendix B. Supplementary data
The following is the Supplementary data to this article:
Data availability
Code used for these analyses will be made available through GitHub.
References
- Ai C., Norton E.C. Interaction terms in logit and probit models. Econ. Lett. 2003;80(1):123–129. doi: 10.1016/S0165-1765(03)00032-6. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention . Technical report, CDC; 2019. Preliminary Evaluation of the Impact of the 2019 National Health Interview Survey Questionnaire Redesign and Weighting Adjustments on Early Release Program Estimates. [Google Scholar]
- Chawla N., Breen N., Liu B., Lee R., Kagawa-Singer M. Asian American women in California: a pooled analysis of predictors for breast and cervical can- cer screening. Am. J. Publ. Health. 2015;105(2):e98–e109. doi: 10.2105/AJPH.2014.302250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus M.L., Talavera G.A., Avilés-Santa M.L., et al. Prevalence of major cardiovas- cular risk factors and cardiovascular diseases among hispanic/latino individu- als of diverse backgrounds in the United States. JAMA. 2012;308(17):1775. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Cesare M., Khang Y.H., Asaria P., et al. Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381(9866):585–597. doi: 10.1016/S0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- Documet P., Bear T.M., Flatt J.D., Macia L., Trauth J., Ricci E.M. The association of social support and education with breast and cervical cancer screening. Health Educ. Behav. 2015;42(1):55–64. doi: 10.1177/1090198114557124. Publisher: SAGE Publications Incdoi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubay L.C., Lebrun L.A. Health, behavior, and health care disparities: disentan- gling the effects of income and race in the United States. Int. J. Health Serv. 2012;42(4):607–625. doi: 10.2190/HS.42.4.c. [DOI] [PubMed] [Google Scholar]
- Echeverria S.E., Mustafa M., Pentakota S.R., et al. Social and clinically-relevant car- diovascular risk factors in Asian Americans adults: NHANES 2011–2014. Prev. Med. 2017;99:222–227. doi: 10.1016/j.ypmed.2017.02.016. [DOI] [PubMed] [Google Scholar]
- Elo I.T., Martikainen P., Smith K.P. Socioeconomic differentials in mortality in Fin- land and the United States: the role of education and income. Eur. J. Popul./Revue européenne de Démographie. 2006;22(2):179–203. doi: 10.1007/s10680-006-0003-5. [DOI] [Google Scholar]
- Fedewa S.A., Star J., Bandi P., et al. Changes in cancer screening in the US dur- ing the COVID-19 pandemic. JAMA Netw. Open. 2022;5(6) doi: 10.1001/jamanetworkopen.2022.15490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher-Borne M., Isher-Witt J., Comstock S., Perkins R.B. Understanding COVID-19 impact on cervical, breast, and colorectal cancer screening among feder- ally qualified healthcare centers participating in “Back on track with screening” quality improvement projects. Prev. Med. 2021;151 doi: 10.1016/j.ypmed.2021.106681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiva J.H., Hægeland T., Rønning M., Syse A. Access to treatment and educational inequalities in cancer survival. J. Health Econ. 2014;36:98–111. doi: 10.1016/j.jhealeco.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Frey W.H. Brookings Institution Press; 2018. Diversity Explosion: How New Racial Demographics Are Remaking Amer- Ica. (Google-Books-ID: JHUzDwAAQBAJ) [Google Scholar]
- Gomez S.L., Clarke C.A., Shema S.J., Chang E.T., Keegan T.H.M., Glaser S.L. Disparities in breast cancer survival among asian women by ethnicity and immigrant status: a population-based study. Am. J. Publ. Health. 2010;100(5):861–869. doi: 10.2105/AJPH.2009.176651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gornick M.E., Eggers P.W., Reilly T.W., et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N. Engl. J. Med. 1996;335(11):791–799. doi: 10.1056/NEJM199609123351106. Publisher: Massachusetts Medical Society _eprint: [DOI] [PubMed] [Google Scholar]
- Islami F., Miller K.D., Jemal A. Cancer burden in the United States—a review. Annals of Cancer Epidemiology. 2018;1:1. doi: 10.21037/ace.2018.08.02. [DOI] [Google Scholar]
- Jatoi I., Sung H., Jemal A. The emergence of the racial disparity in U.S. Breast-cancer mortality. N. Engl. J. Med. 2022;386(25):2349–2352. doi: 10.1056/NEJMp2200244. Publisher: Massachusetts Medical Society _eprint: [DOI] [PubMed] [Google Scholar]
- Katz S.F., Rodriguez F., Knowles J.W. Health disparities in cardiometabolic risk among Black and Hispanic youth in the United States. American Journal of Pre- ventive Cardiology. 2021;6 doi: 10.1016/j.ajpc.2021.100175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh A., Bentley R.J., Turrell G., Shaw J., Dunstan D., Subramanian S.V. So- cioeconomic position, gender, health behaviours and biomarkers of cardiovascu- lar disease and diabetes. Soc. Sci. Med. 2010;71(6):1150–1160. doi: 10.1016/j.socscimed.2010.05.038. [DOI] [PubMed] [Google Scholar]
- Kim G., Ford K.L., Chiriboga D.A., Sorkin D.H. Racial and ethnic disparities in healthcare use, delayed care, and management of diabetes mellitus in older adults in California. J. Am. Geriatr. Soc. 2012;60(12):2319–2325. doi: 10.1111/jgs.12003. https://onlinelibrary.wiley.com/doi/pdf/10.1111/jgs.12003doi: 10.1111/jgs.12003 _eprint: [DOI] [PubMed] [Google Scholar]
- Kim E.S., Moored K.D., Giasson H.L., Smith J. Satisfaction with aging and use of preventive health services. Prev. Med. 2014;69:176–180. doi: 10.1016/j.ypmed.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange F. The role of education in complex health decisions: evidence from cancer screening. J. Health Econ. 2011;30(1):43–54. doi: 10.1016/j.jhealeco.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Luck A.N., Preston S.H., Elo I.T., Stokes A.C. The unequal burden of the Covid-19 pandemic: capturing racial/ethnic disparities in US cause-specific mortality. SSM - Population Health. 2022;17 doi: 10.1016/j.ssmph.2021.101012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta N.K., Abrams L.R., Myrskylä M. US life expectancy stalls due to cardiovas- cular disease, not drug deaths. Proc. Natl. Acad. Sci. USA. 2020;117(13):6998–7000. doi: 10.1073/pnas.1920391117. Publisher: Proceedings of the National Academy of Sciencesdoi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A.H., Ford E.S., Bowman B.A., et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- Mouw T., Koster A., Wright M.E., et al. Education and risk of cancer in a large cohort of men and women in the United States. PLoS One. 2008;3(11) doi: 10.1371/journal.pone.0003639. Publisher: Public Library of Sciencedoi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Heron M. National Center for Health Statistics; 2021. Deaths: Leading Causes for 2018. Tech. Rep. [PubMed] [Google Scholar]
- Nghiem V.T., Davies K.R., Chan W., Mulla Z.D., Cantor S.B. Disparities in cervical cancer survival among Asian American women. Ann. Epidemiol. 2016;26(1):28–35. doi: 10.1016/j.annepidem.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien M.J., Halbert C.H., Bixby R., Pimentel S., Shea J.A. Community health worker intervention to decrease cervical cancer disparities in hispanic women. J. Gen. Intern. Med. 2010;25(11):1186–1192. doi: 10.1007/s11606-010-1434-6. 10.1007/s11606-010-1434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peralta M. dA., Holaday B., McDonell J.R. Factors affecting hispanic women's par- ticipation in screening for cervical cancer. J. Immigr. Minority Health. 2015;17(3):684–695. doi: 10.1007/s10903-014-9997-7. [DOI] [PubMed] [Google Scholar]
- Ponce N.A., Adia A.C., Banawa R.A., Tan S., Sabado-Liwag M.D. Measuring Asian hate: discordant reporting of race-based hate incidents and unfair treatment and association with measures of wellbeing. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.958857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintal C., Antunes M. Mirror, mirror on the wall, when are inequalities higher, after all? Analysis of breast and cervical cancer screening in 30 European countries. Soc. Sci. Med. 2022;312 doi: 10.1016/j.socscimed.2022.115371. [DOI] [PubMed] [Google Scholar]
- Ren J., Feagin J. Face mask symbolism in anti-Asian hate crimes. Ethn. Racial Stud. 2021;44(5):746–758. doi: 10.1080/01419870.2020.1826553. [DOI] [Google Scholar]
- Roberts D. New Press/ORIM; 2011. Fatal Invention: How Science, Politics, and Big Business Re-create Race in the Twenty-First Century. Google-Books-ID: yb7xxeSczFYC. [Google Scholar]
- Rutter C.M., Knudsen A.B., Lin J.S., Bouskill K.E. Black and white differences in colorectal cancer screening and screening outcomes: a narrative review. Cancer Epidemiol. Biomarkers Prev. 2021;30(1):3–12. doi: 10.1158/1055-9965.EPI-19-1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabates R., Feinstein L. The role of education in the uptake of preventative health care: the case of cervical screening in Britain. Soc. Sci. Med. 2006;62(12):2998–3010. doi: 10.1016/j.socscimed.2005.11.032. [DOI] [PubMed] [Google Scholar]
- Shahu A., Okunrintemi V., Tibuakuu M., et al. Income disparity and utilization of cardiovascular preventive care services among U.S. adults. American Journal of Preventive Cardiology. 2021;8 doi: 10.1016/j.ajpc.2021.100286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiovitz-Ezra S., Litwin H. Social network type and health-related behaviors: ev- idence from an American national survey. Soc. Sci. Med. 2012;75(5):901–904. doi: 10.1016/j.socscimed.2012.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer statistics, 2021. CA. A Cancer Journal for Clinicians. 2021;71(1):7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- Song H., Bergman A., Chen A.T., et al. Disruptions in preventive care: mammograms during the COVID-19 pandemic. Health Serv. Res. 2021;56(1):95–101. doi: 10.1111/1475-6773.13596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tejeda S., Thompson B., Coronado G.D., Martin D.P. Barriers and facilitators related to mammography use among lower educated Mexican women in the USA. Soc. Sci. Med. 2009;68(5):832–839. doi: 10.1016/j.socscimed.2008.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinh Q.D., Li H., Meyer C.P., et al. Determinants of cancer screening in Asian- Americans. Cancer Causes Control. 2016;27(8):989–998. doi: 10.1007/s10552-016-0776-8. [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes E.A., Miranda P.Y., Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc. Sci. Med. 2012;75(12):2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- Wang J.H., Sheppard V.B., Schwartz M.D., Liang W., Mandelblatt J.S. Disparities in cervical cancer screening between asian American and non-hispanic white women. Cancer Epidemiol. Biomarkers Prev. 2008;17(8):1968–1973. doi: 10.1158/1055-9965.EPI-08-0078. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: evidence and needed research. Annu. Rev. Publ. Health. 2019;40(1):105–125. doi: 10.1146/annurev-publhealth-040218-043750. _eprint: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo H.C., Gee G.C., Takeuchi D. Discrimination and health among Asian American immigrants: disentangling racial from language discrimination. Soc. Sci. Med. 2009;68(4):726–732. doi: 10.1016/j.socscimed.2008.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo W., Kim S., Huh W.K., et al. Recent trends in racial and regional disparities in cervical cancer incidence and mortality in United States. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0172548. Publisher: Public Library of Sciencedoi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zavala V.A., Bracci P.M., Carethers J.M., et al. Cancer health disparities in racial/ethnic minorities in the United States. Br. J. Cancer. 2021;124(2):315–332. doi: 10.1038/s41416-020-01038-6. Number: 2 Publisher: Nature Publishing Groupdoi: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Code used for these analyses will be made available through GitHub.