Abstract
Social support is an influential component of postpartum recovery, adjustment, and bonding, which was disrupted by social distancing recommendations related to the COVID-19 pandemic. This study reports on changes in the availability of social support for postpartum women during the pandemic, investigates how those changes may have contributed to postpartum mental health, and probes how specific types of social support buffered against poor postpartum mental health and maternal-infant bonding impairment. Participants were 833 pregnant patients receiving prenatal care in an urban USA setting and using an electronic patient portal to access self-report surveys at two time points, during pregnancy (April–July 2020) and at ~12 weeks postpartum (August 2020–March 2021). Measures included an assessment of COVID-19 pandemic–related change in social support, sources of social support, ratings of emotional and practical support, and postpartum outcomes including depression, anxiety, and maternal-infant bonding. Overall self-reported social support decreased during the pandemic. Decreased social support was associated with an increased risk of postpartum depression, postpartum anxiety, and impaired parent-infant bonding. Among women reporting low practical support, emotional support appeared to protect against clinically significant depressive symptoms and impaired bonding with the infant. Decreases in social support are associated with a risk for poor postpartum mental health outcomes and impaired maternal-infant bonding. Evaluation and promotion of social support are recommended for healthy adjustment and functioning of postpartum women and families.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00737-023-01330-3.
Keywords: Postpartum mental health, Postpartum depression, Maternal mental health, Social support, Maternal-infant bonding
Introduction
Pregnancy and the postpartum period are associated with increased vulnerability to mental health disorders, including postpartum depression and anxiety. Research over the last 30 years has highlighted that social support plays a key role in maintaining mental well-being during and after pregnancy (Gjerdingen et al. 1991; Maharlouei 2016; Orr 2004). Specifically, social support is a major buffer against postpartum depression (Gjerdingen & Chaloner 2004; Howell et al. 2005; Mckee et al. 2001) and promotes general postpartum well-being (Ginja et al. 2018; Siedlecki et al. 2014). Qualitative research found that birthing individuals expect instrumental or practical support (i.e., help with functional tasks) from partners and family members, believing that this type of support is critical to their postpartum physical and emotional recovery (Negron et al. 2013). Despite this fact, many birthing individuals report that they receive neither the practical nor the emotional support that they want and need (Slomian et al. 2017). The change in social milieu caused by the COVID-19 pandemic, henceforth referred to as the pandemic, may have further limited the availability of social support across the postpartum period.
Increasingly, reports have documented the negative effects of the pandemic on social relationships (Dib et al. 2020; Liu et al. 2021; Zhou et al. 2021). During the pandemic, typical avenues of perinatal support and care were unavailable due to social distancing recommendations (Saleh et al. 2022). For example, family and friends were less likely to spontaneously “drop in” to provide help with household tasks including cooking or childcare (Saleh et al. 2022). This lack of support may have increased vulnerability to poor postpartum mental health outcomes among birthing individuals during the pandemic. In fact, among a sample of pregnant and postpartum women, pandemic-related changes in perceived support were associated with depression symptoms (Zhou et al. 2021). Similarly, we (Kornfield et al. 2021) and others (Liu et al. 2021) found that postpartum depression in the context of the pandemic was related to disruptions to maternal-infant bonding. Reports of how social support contributes to mother-infant bonding are equivocal (Liu et al. 2021; Ohara et al. 2017); thus, more research is needed to fully understand how the pandemic may have affected the social milieu of postpartum individuals and how social support is linked to risk for postpartum depression, anxiety, and maternal-infant bonding.
This study leveraged data from a diverse longitudinal cohort of pregnant women in the Philadelphia area during the early phase of the pandemic and again after they had given birth. We aimed to (1) examine perceived changes in social support for postpartum women during the pandemic and describe the frequency of virtual social support, (2) understand how changes in social support contribute to postpartum mental health and mother-infant bonding. and (3) probe how specific types of social support (i.e., emotional vs. practical support) may differentially buffer against poor postpartum outcomes. We hypothesized that during the pandemic, postpartum women would report a decrease in their social support, and that this change in support would be negatively associated with mental health (i.e., depression and anxiety) and impaired mother-infant bonding. Examining specific types of social support, we hypothesized that increased practical support would be more strongly related to bonding impairment, whereas emotional support would be differentially related to postpartum mental health status.
Methods
Participants
The study included 833 perinatal patients from a longitudinal cohort followed from pregnancy through postpartum (Gur et al. 2020; Kornfield et al. 2021); see Table 1 for sample demographics and the consort flow diagram for more information about the recruitment of the cohort (Fig. S1). Participants were identified through Penn Medicine medical records during prenatal care in the University of Pennsylvania Hospital System. Participants were emailed study details and invited to complete an online survey (Gur et al. 2020) at two time periods: April 17–July 8, 2020, during a statewide stay-at-home order and a period of high community spread of the COVID-19 virus (T1; M=25.27 weeks’ gestation, SD=8.20) and August 11, 2020–March 2, 2021 (T2; M=11.83 weeks postpartum, SD=4.26). Childbirth information and participant race (Black/African American, White, Asian, Latina not otherwise specified, Native Hawaiian/Pacific Islander, Declined, Other, and Unknown) and ethnicity (Hispanic/Latina, Non-Hispanic/Non-Latina, Declined, Unknown) were collected from electronic medical records (EMR). As individuals in the study had uteruses and gave birth in the manner of biological females, we refer to participants as “women,” but note that data on gender identity and precise genetic makeup was not collected at this assessment. The University of Pennsylvania Institutional Review Board approved the study.
Table 1.
Sample characteristics and descriptive statistics for social support variables and postpartum outcomes
| Percent | ||
|---|---|---|
| Race | ||
| White | 71.9% | |
| Black | 18.1% | |
| Other | 10.0% | |
| Ethnicity | ||
| Latinx | 4.9% | |
| Non-Latinx | 94.5% | |
| Education | ||
| No college | 19.0% | |
| College or graduate education | 81.0% | |
| Relationship status | ||
| Partnered | 81.5% | |
| Single, divorced, or widowed | 18.5% | |
| Parity | ||
| First pregnancy | 56.9% | |
| Prior pregnancies | 43.1% | |
| Range | Mean (SD) | |
| SES | −2.60–2.08 | −.35 (.93) |
| Maternal age (years) | 18.00–46.29 | 32.96 (4.49) |
| Pre-pandemic perceived social support | 1-4 | 3.07 (.89) |
| Current pandemic perceived social support | 6–42 | 35.94 (7.75) |
| Emotional social support | 0–9 | 6.50 (2.51) |
| Practical social support | 1–4 | 3.07 (.89) |
| Virtual interactions | 1–4 | 3.04 (.84) |
| Postpartum depression (EPDS) | 0–6 | .59 |
| Postpartum anxiety (GAD-7) | 0–21 | 4.08 |
| Impaired bonding (BIQ) | 0–36 | 5.67 |
SES, socioeconnomoc status; EPDS, Edinburgh Depression Scale; GAD-7, Generalized Anxiety Scale-7; BIQ, Bonding Impairment Questionnaire. SES was a census-based neighborhood composite variable based on participant zip codes. The score was created from census-based geocoding of zip code–based variables (i.e., % residence in poverty, % married, median family income). The clinical cutoff for depression and anxiety scores was ≥10, and ≥12 was used for impaired bonding status. A total of 195 met screening criteria for postpartum depression; 78 met criteria for postpartum anxiety; 94 met criteria for impaired bonding
Timeline context
T1: April 17–July 8, 2020
During the time that T1 assessments were administered, Philadelphia and the surrounding region were under an emergency “Stay at Home Order,” which restricted any public or private gatherings of any individuals outside of a single household. Residents were urged to stay home or at their place of residence unless engaged in essential personal activities, such as seeking food or medical attention, including prenatal care. Schools, daycares, and preschools remained closed. Essential employees in the sectors of healthcare, food service, and delivering essential goods were permitted to leave home to work. For the most part, women were told not to bring supportive others to medical appointments, including during labor and delivery.
T2: August 11, 2020–March 2, 2021
During the T2 assessment timeframe, Philadelphia entered the Yellow Phase of its Safer at Home guidelines. This meant easing some of the initial restrictions but still mandated social distancing, mask-wearing in public places, and limitations placed on public and private gatherings, including for religious observance (no more than 25 people). Many Philadelphia public schools remained closed during the beginning of this phase. Individuals were permitted to bring one supportive other to medical appointments.
Procedures
Social support measures
Pandemic-related perceived change in social support
At T2, participants were asked two items that measured overall perceived social support prior to and during the pandemic: “Prior to the pandemic, how well supported did you feel by your social network?” and “Currently (i.e., since the pandemic and your delivery), how well supported do you feel by your social network?” Response options were a 4-point Likert scale ranging from “Not at all” to “Strongly.” These items were adapted from the COPE study (Zhou et al. 2021). To assess change in support, a difference score was created based on the perceived social support from before the pandemic to that during pandemic, regressing out the pre-social support score. Skewness and kurtosis were <1.
Sources of social support and frequency of virtual social connections
Participants were asked to report from whom they were receiving social support (i.e., friends, family, therapist/counselor). They were also asked about how frequently they tried to connect with their social supports (i.e., family and friends): “Since the pandemic, how much have you tried to connect with friends and family through virtual interactions (e.g., phone calls, emails, text, video calls, Facebook, Instagram)?”. Participants answered these items using the following scale: not at all, a few times a month, a few times a week, or every day.
Emotional social support
Participants completed the short (6-item) Multidimensional Scale of Perceived Social Support (MSPSS; Porter et al. 2019) to assess levels of emotional and social support from family, friends, and significant others. Response options were a 7-point Likert scale ranging from “very strongly disagree” to “very strongly agree,” with higher scores reflecting greater perceived support (α=.93).
Practical social support
Participants completed the instrumental support section of the Maternal Social Support Index (MSSI) at T2 (Pascoe et al. 1988), which includes 9 items assessing whether the parent had help with household chores or parenting tasks, such as grocery shopping and putting the child to bed. The response options were either “I take sole responsibility” or “Someone else does this task or helps me complete this task.” The nine items were summed with higher scores reflecting greater practical support (one item “takes care of car problems” was removed for this study) (α =.82).
Postpartum outcomes
Postpartum depression was assessed using the Edinburgh Postnatal Depression Scale (EPDS; Cox et al. 1987). The last item of the scale about self-harm was not assessed as surveys were administered online without clinical oversight. A cutoff ≥10 was used to indicate a positive depression screen. Anxiety was assessed via the seven-item Generalized Anxiety Scale (GAD-7; Spitzer et al. 2006). A cutoff ≥10 was used to indicate a positive anxiety screen. Mother-infant bonding was assessed by the 12-item “General Impairment” scale from the Postpartum Bonding Questionnaire (PBQ; Brockington et al. 2006). A cutoff ≥12 was used to indicate a positive screen for bonding impairment (range, α =.80–.90).
Data analysis
The first analysis was descriptive, identifying the overall sources of support to participants during the postpartum period. This support encompassed friends, family members, healthcare providers, and mental health professionals. However, all subsequent analyses are specific to support provided by friends and family and did not include references to healthcare providers or mental health professionals.
The next set of analyses examined the social milieu of postpartum women during the pandemic. Specifically, we examined perceived changes in social support and the frequency of virtual social interactions reported (Aim 1). First, we tested the hypothesis that participants would report a decrease in social support from before to after the pandemic using a chi-square test to examine differences in the distribution of support ratings from before and after the pandemic. We also examined the difference in overall mean ratings using a two-tailed t-test. Second, we examined factors (i.e., participant characteristics and reported pandemic experiences) that may have influenced changes in postpartum social support using a multivariable linear regression. In this model, change in perceived social support was the dependent variable with the following independent variables: EMR race (dummy coded for white, black, and other), Hispanic or Latinx ethnicity (yes, no), Education (no college vs college or graduate education), SES (continuous score based on neighborhood census data; Moore et al. 2016), maternal age, relationship status (partnered vs single, divorced, or widowed), and parity (first pregnancy or not). Next, we examined the frequency of participants’ virtual social connections. Finally, we examined if the frequency of virtual social interactions during the pandemic was related to the reported change in social support using a t-test.
The third set of analyses was aimed at understanding how a perceived change in social support during the postpartum period contributed to postpartum mental health outcomes (Aim 2). Three multivariable logistic regressions were conducted using the binary (above clinical screening threshold vs below threshold) dependent variables of postpartum depression (PPD), anxiety (PPA), or impaired bonding. As before, we first entered sample characteristics (i.e., EMR race, ethnicity, education, SES, maternal age, relationship status, and parity) and then added change in perceived social support as the independent variable. When impaired bonding was specified as the dependent variable, we also included PPD as a covariate to test the specificity of effects.
The last set of analyses probed how specific types of social support (i.e., emotional vs. practical) may have differentially buffered against postpartum mental health outcomes (Aim 3). We conducted three multivariable logistic regression models to estimate associations between the different types of social support and the binary outcomes of PPD, PPA, and impaired bonding. As before, we first entered sample characteristics as covariates and then added practical and emotional support as independent variables, before adding an interaction term between practical and emotional support. As before, when impaired bonding was specified as the dependent variable, we also included PPD as a covariate to test the specificity of effects. To probe significant interactions, regressions were conducted to examine associations between emotional support and postpartum mental health outcomes at high and low levels (median split) of practical support. To reduce multicollinearity, practical support was regressed out of emotional support and vice versa. Supplemental analyses were performed to predict continuous postpartum outcomes using multivariable linear regressions. Statistical analyses were conducted in SPSS version 27.
Results
Sample characteristics are reported in Table 1.
Overall reporting on sources of social support
During the pandemic, the majority of postpartum women reported receiving support from family (95%, n=794) and friends (81%, n=678). In addition, 14% (n=115) of the sample reported getting support from a mental health professional and 9% (n=76) reported support from a healthcare provider.
Pandemic-related perceived change in social support and virtual social interactions (Aim 1)
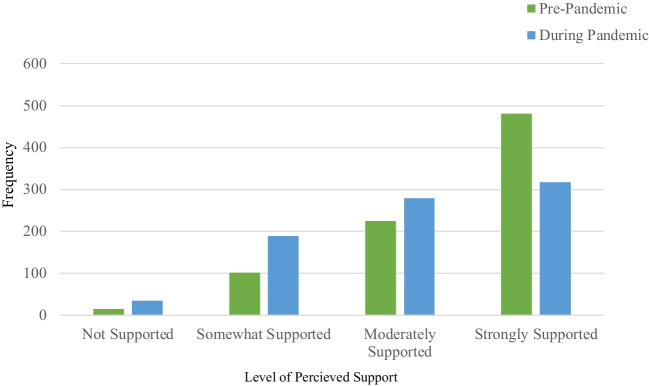
There was a significant difference in the distributions of ratings of perceived social support from before versus during the pandemic ((9)= 412.60, p<.001, see Fig. 1). Participants reported a perceived decline in their social support from before (M=3.43, SD=.78) to during the pandemic (M=3.07, SD=.89), t(819)=13.51, p<.001. This perceived decline in support was reported by 36% (n=300) of participants (difference score <0), while 55% (n=461) reported no perceived change in support (difference score =0) and 7% (n=59) reported increased social support during the pandemic (difference score >0). No sample characteristics were associated with a perceived change in social support (Table S.1).
Fig. 1.
Ratings of perceived social support before and during the pandemic. Notes. The figure illustrates level of support that participants felt they received from their social network (friends and family) before and during their pandemic postpartum experience
For the frequency of social interactions, the majority of participants reported having virtual social connections with friends and family either several times a week (n=310, 37%) or everyday (n=287, 35%), while 25% (n=208) of the sample reported a few times a month and 3% (n=21) reported they had no virtual social connections. Those reporting more frequent virtual connections (i.e., several times a week to everyday) reported less of a decline (M=.14; SD=.92) in social support from before to during the pandemic compared to those with less frequent virtual connections (i.e., no interactions or a few times a month; M=−.36; SD=1.11), t(818)=-5.97, p<.001).
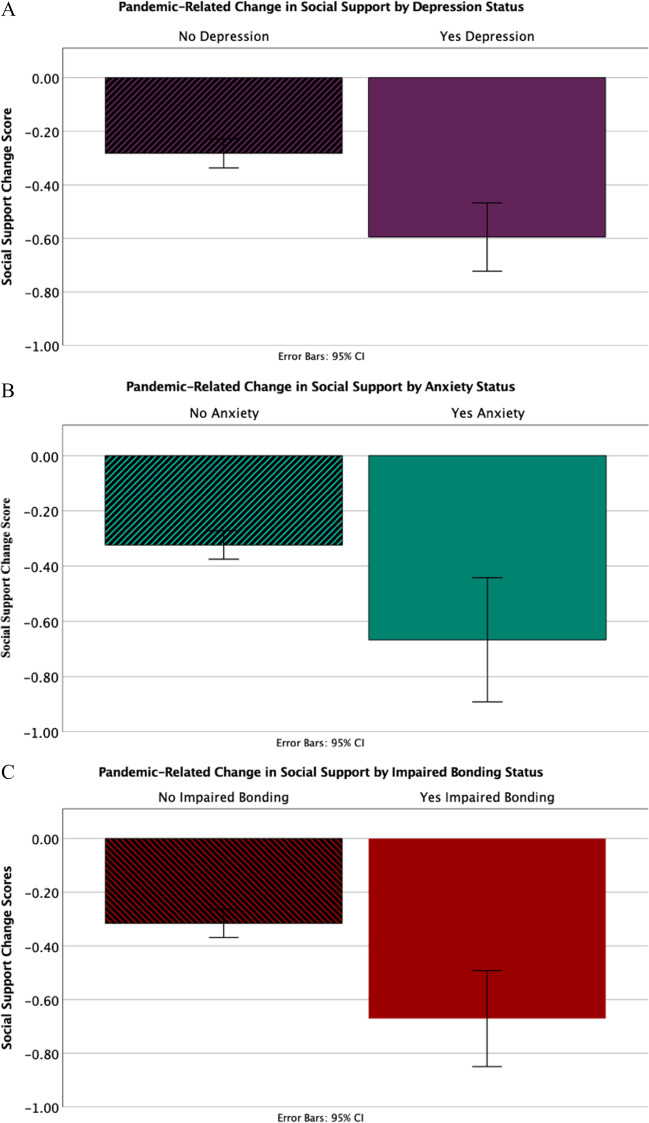
Perceived pandemic-related perceived change in social support and poor postpartum outcomes (Aim 2)
Results for Aim 2 are presented in Table 2 and Fig. 2. A decrease in pandemic-related perceived social support (more negative difference score) was associated with an increased likelihood of a positive PPD screen (OR=.56, 95%CI=.48–.67) and PPA screen (OR=.53, 95%CI=.41–.67). A decrease in perceived social support was also related to impaired parent-infant bonding (OR=.67, 95%CI=.53–.83). Similar findings emerged using continuous measures (Table S1).
Table 2.
Pandemic-related change in perceived social support predicting postpartum outcomes
| Postpartum outcomes | ||||||
|---|---|---|---|---|---|---|
| Postpartum depression | Postpartum anxiety | Impaired bonding | ||||
| Block 1 | χ2(8)=7.49, p=.49, R2=.01 | χ2(8)=12.19, p=.14, R2=.03 | χ2(9)=64.99, p<.001, R2=.15 | |||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Race (dummy v1; Black=1) | .57 | .33–1.00 | .51 | .24–1.08 | 1.71 | .60–4.14 |
| Race (dummy v2; White=1) | .92 | .52–1.62 | .98 | .42–2.28 | .86 | .42–1.78 |
| Ethnicity | .96 | .44–2.11 | .29 | .13–.67 | 2.72 | .60–12.30 |
| Education | 1.14 | .64–2.02 | .86 | .48–2.42 | 2.13 | .82–5.53 |
| SES | 1.08 | .88–1.33 | .96 | .70–1.31 | 1.23 | .93–1.61 |
| Maternal age | .99 | .95–1.03 | .98 | .92–1.04 | 1.03 | .97–1.09 |
| Marital status | .60 | .32–1.11 | .91 | .40–2.08 | 1.47 | .57–3.78 |
| Parity | .90 | .63–1.28 | 1.13 | .67–1.92 | 1.52 | .93–2.50 |
| Postpartum depression | - | - | - | - | .19 | .12–.30 |
| Block 2 | χ2(1)=46.56, p<.001, R2=.10 | χ2(1)=28.86, p<.001, R2=.11 | χ2(1)=13.36, p<.001, R2=.18 | |||
| Pandemic effects on perceived change in social support | .56 | .48–.67 | .53 | .41–.67 | .67 | .53–.83 |
SES, socioeconnomoc status. SES was a census-based neighborhood composite variable based on participant zip codes. The score was created from census-based geocoding of zip code–based variables (i.e., % residence in poverty, % married, median family income). Values in bold indicate significance
Fig. 2.
Pandemic change in social support by postpartum outcomes. Notes. Error bars represent 95% CI. The figure illustrates differences in social support change scores by postpartum depression, postpartum anxiety, and impaired bonding screening status
Types of social support and poor postpartum outcomes: emotional support as a buffer against the depression risk of low practical support (Aim 3)
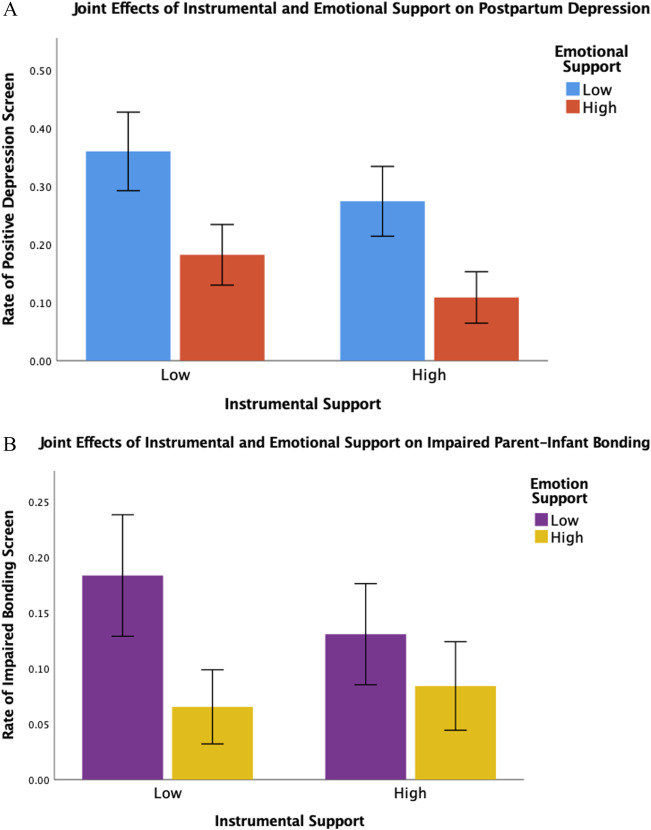
Results for Aim 3 are presented in see Table 3. Practical support and emotional support were moderately correlated (r=.29, p<001). First, logistic regressions showed that higher levels of emotional support (OR=.61, 95%CI=.51–.72) and practical support (OR=.67, 95%CI=.54–.82) were both uniquely to reduced likelihood of positive PPD screen. A significant interaction between the two types of support emerged (b=.18, p=.013), such that emotional support was only associated with decreased PPD risk among those reporting low practical support (b=–.74, OR=.48, 95%CI=.36–.63) and not those reporting high practical support (b=–.20, OR=.82, 95%CI=.65–1.02; see Fig. 3A). Second, higher levels of both emotional support (OR=.61, 95%CI=.49–.75) and practical support (OR=.64, 95%CI=.48–.85) were also uniquely related to a decreased likelihood of a positive PPA screen. However, there was no significant interaction between the two (p=.23). Finally, both increased emotional support (OR=.66, 95%CI=.53–.82) and increased practical support (OR=.70, 95%CI=.53–.93) were associated with lower odds of impaired bonding, after controlling for PPD. A significant interaction between the two support types emerged (b=.20, p=.046), such that higher emotional support was only associated with lower impaired bonding among those with low practical support (b=–.71, OR=.49, 95%CI=.34–.71) but not among those reporting high practical support (b= –.07, OR=.93, 95%CI=.67–1.30; see Fig. 3B). Similar findings emerged using continuous measures for postpartum outcomes, (Table S2), with the exception that the interaction term predicting PPA was now significant and followed a similar pattern as PPD and impaired bonding.
Table 3.
Joint effects of emotional and practical support predicting postpartum outcomes
| Postpartum outcomes | ||||||
|---|---|---|---|---|---|---|
| Postpartum depression | Postpartum anxiety | Impaired bonding | ||||
| Block 1 | χ2(8)=7.40, p=.49, R2=.01 | χ2(8)=12.16, p=.14, R2=.03 | χ2(9)=64.99 p<.001, R2=.15 | |||
| Exp(B) | 95%CI | Exp(B) | 95%CI | Exp(B) | 95%CI | |
| Race (dummy v1; Black=1) | .57 | .33–1.00 | .51 | .24–1.08 | 1.71 | .70–4.14 |
| Race (dummy v2; White=1) | .92 | .52–1.62 | .98 | .42–2.28 | .86 | .42–1.78 |
| Ethnicity | .96 | .44–2.11 | .29 | .13–.67 | 2.72 | .60–12.30 |
| Education | 1.14 | .64–2.02 | 1.07 | .48–2.42 | 2.13 | .82–5.53 |
| SES | 1.08 | 88–1.33 | .96 | .70–1.31 | 1.23 | .93–1.62 |
| Maternal age | .99 | .95–1.03 | .98 | .92–1.04 | 1.03 | .97–1.09 |
| Marital status | .60 | .32–1.11 | .91 | .40–2.08 | 1.47 | .57–3.78 |
| Parity | .90 | .63–1.28 | 1.14 | .67–1.93 | 1.52 | .93–2.50 |
| Postpartum depression | – | – | – | – | .19 | .12–.30 |
| Block 2 | χ2(2)=37.56, p<.001, R2=.08 | χ2(2)=22.84, p<.001, R2=.09 | χ2(2)=25.09, p<.001, R2=.09 | |||
| Emotional support | .61 | .51–.72 | .61 | .49–.75 | .66 | .53–.82 |
| Practical support | .67 | .54–.82 | .64 | .48–.85 | .70 | .53–.93 |
| Block 3 | χ2(1)=6.88, p=.01, R2=.09 | χ2(1)=1.52, p=.22, R2=.10 | χ2(1)=4.55, p=.03, R2=.19 | |||
| b | p | b | p | b | p | |
| Emotional*practical support | .18 | .01 | .10 | .23 | .20 | .05 |
SES, socioeconnomoc status. SES was a census-based neighborhood composite variable based on participant zip codes. The score was created from census-based geocoding of zip code–based variables (i.e., % residence in poverty, % married, median family income). Values in bold indicate significance
Fig. 3.
Joint effects of emotional support and practical support predicting postpartum depression and parent-infant bonding. Notes. Error bars represent 95% CI. The figure illustrates the interaction between emotional and practical support on postpartum depression status. For illustrative purposes, both variables were split into high and low (median split) groups. Emotional support only predicted depression and impaired bonding status for women reporting low practical support
Discussion
Social support is universally important to mental health and well-being, and its significance is only further amplified during the perinatal period (Hirsch & Hirsch 1980; Hutchens & Kearney, 2020; Rich-Edwards 2006; Siedlecki et al. 2014; Turner & Turner 2013). Our findings highlight the importance of different types of social support and expand on the known effects of perceived social support during the perinatal period, especially in the context of an extreme global stressor. National stay-at-home orders during the spring of 2020 and beyond encouraged people to reduce exposure to others, both to limit the potential risk of becoming infected or infecting vulnerable others. Pregnant individuals and very young infants were among those at high risk of poor outcomes from COVID-19 infection and thus advised to follow social distancing recommendations closely (CDC 2022). It is not surprising that social support was reduced in this sample of 833 racially diverse women who were in the early postpartum stage during the COVID-19 pandemic. Consistent with our findings, others have also found that compared to their social support ratings before the onset of the pandemic, pregnant and postpartum women self-reported lower support after social distancing regulations were in effect (Zhou et al. 2021). The fact that participant characteristics did not relate to perceived loss or change of social support emphasizes the universality of the pandemic’s effect on new parents during this global stressor.
The findings add to recent evidence showing elevated levels of poor mental health symptoms for pregnant and newly postpartum women during the pandemic (Basu et al. 2021; Gildner et al. 2021; Gur et al. 2020; Ostacoli et al. 2020; Puertas-Gonzalez et al. 2021; Racine et al. 2021; Zhou et al. 2021). We find that a significant source of the detriment to maternal mental health was the resultant loss of social support during the postpartum pandemic period. Women who reported greater losses of social support during the postnatal period were significantly more likely to screen positive for probable postpartum depression and anxiety and were even at higher risk for impaired bonding with their infant. Although we did not have a pre-pandemic control group or information on women’s social support or mental health before the pandemic, other work has directly compared a cohort of women who delivered before the onset of COVID-19 to those who delivered after the onset, showing higher rates of psychopathology for women who gave birth during the pandemic (Puertas-Gonzalez et al. 2021). Moreover, loss of support does not seem to be specific to the postpartum period or the pandemic as significant associations between negative changes in perceived social support and mental distress across prenatal and postpartum periods have been noted (Spry et al. 2021; Zhou et al. 2021).
Social support is delivered in distinct forms (e.g., practical, emotional, etc.). Our study uniquely adds to the literature by demonstrating both independent and interactive relationships between emotional and practical dimensions of social support and postpartum depression, anxiety, and maternal bonding. Exploring the role of different types of support amid the pandemic is important, especially given the established links between loss of support and increased depression and anxiety symptoms (Gildner et al. 2021; Hutchens & Kearney 2020; Lin et al. 2022; Schwab-Reese et al. 2017; Terada et al. 2021; Zhou et al. 2021). The experiences of individuals in this study reinforce the protective properties of practical support against depressive symptoms for people in the early postpartum. To some degree, evidence from this sample echoes what is known: that mothers with young children who reported continuous childcare, assistance with housework, and newborn care support scored significantly lower on EPDS when compared to women who reported disruptions to practical support because of the pandemic (Gildner et al., 2021). For mothers caring for other children in addition to the index infant, qualitative reports suggest the likelihood of women feeling “burdened by childcare, homeschooling and working during the pandemic” contributes to low postpartum moods (Racine et al. 2021).
Still, in a setting of reduced practical support, our results suggested that emotional support protected against clinically significant depressive symptoms and impaired bonding with the infant. The current results show that the perception of adequate emotional support helped prevent negative postpartum outcomes in the context of major stress (i.e., a global health crisis), even in cases where perceived practical support was low. This substantiates qualitative evidence indicating pregnant and early postpartum women found emotional support to be the most beneficial source of support amid high stress and feelings of anxiety during the pandemic (Farewell et al. 2020). In contrast, a pre-pandemic study (Hetherington et al., 2018) affirms the association between types of emotional support and protection against risk for mental health symptoms for women in the early postpartum but identifies no one dimension of social support as having a superior effect on decreasing risk for clinically relevant mental health symptoms for women in the early postpartum.
Given that social distancing regulations in effect during the COVID-19 pandemic likely limited in-person exchanges of support (i.e., practical support from friends and family outside the home), it is probable that emotional support was provided through virtual methods among this sample. Supporting this notion, we found that women who reported more frequent virtual connections reported less of a decline in perceived social support. Our findings are consistent with those of other studies showing strong virtual means of support during the pandemic appear to buffer against mental health problems during the pandemic (Myers & Emmott 2021). Interestingly, virtual support has been shown to buffer against postpartum depression even before the pandemic (Dennis et al. 2009), suggesting that encouraging prevention measures involving virtual support to perinatal women may be helpful.
This study has limitations. Participants were asked to retrospectively estimate their pre-pandemic social support, during the pandemic which may increase the likelihood of recall bias. The estimation of pre-pandemic support was also based on only two questions that had not been previously validated (though were adapted from published questionnaires from the COPE study (Zhou et al. 2021)). Similarly, participants were asked to rate perceptions of support and we did not directly assess actual support from partners or close others. Finally, the current study captures social support during a constrained time of the COVID-19 pandemic in the USA, which may not generalize to other portions of the pandemic or outside the USA.
Conclusions
The current study underscores the importance of postpartum social support during a universal global stressor which limited the provision of typical avenues of support. The change in perceived support was directly related to increased risk for postpartum depression, anxiety, and impaired maternal-infant bonding. While emotional and practical support both uniquely protected against negative outcomes, emotional support specifically protected against the risk of PPD and impaired bonding in the setting of low practical support. Even in the post-pandemic world, obstetrics, pediatric, and psychiatric providers who have contact with perinatal women should assess for the presence of social support, particularly emotional support, and encourage mothers to reach out to friends and family for this type of resilience-promoting support. In settings where partners or family members accompany perinatal patients to doctor’s visits, they should be directly encouraged to provide both emotional and practical support as it is a major benefit to both maternal and infant well-being and mental health. While we focused on the period of the pandemic, changes in social support or stable low or poor social support can occur at any time during the perinatal period, increasing the risk for poor postpartum mental health outcomes. Evaluation of social support is universally pertinent and can contribute to our ability to improve maternal and family health and functioning.
Supplementary information
(DOCX 47 kb)
Author contribution
All authors contributed to the study’s conception and design. MH prepared and maintained the database. The study questions were conceptualized by SK and LW, and LW performed the data analysis. SK and LW contributed equally to the writing of the first draft of the manuscript. MF contributed significantly to the revisions. All other authors commented on previous drafts of the manuscripts and read and approved the final version.
Funding
The study was supported by the Lifespan Brain Institute of Penn Medicine and Children’s Hospital of Philadelphia and the following grants: National Institute of Mental Health (NIMH) R01 MH125904 (PI: Waller), NIMH R01 MH128593 (PI: Njoroge), and NIMH K08 MH129657 (PI: Chaiyachati).
Data Availability
The data are available upon request.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lauren K. White and Sara L. Kornfield contributed equally to this manuscript.
References
- Basu A, Kim HH, Basaldua R, Choi KW, Charron L, Kelsall N, Hernandez-Diaz S, Wyszynski DF, Koenen KC. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PloS One. 2021;16(4):e0249780. doi: 10.1371/journal.pone.0249780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockington IF, Fraser C, Wilson D. The postpartum bonding questionnaire: a validation. Arch Womens Ment Health. 2006;9(5):233–242. doi: 10.1007/s00737-006-0132-1. [DOI] [PubMed] [Google Scholar]
- CDC (2022) Pregnant and recently pregnant people, Centers for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html. Accessed 10 Jun 2022
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dennis C-L, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE, Kiss A. Effect of peer support on prevention of postnatal depression among high risk women: Multisite randomised controlled trial. BMJ. 2009;338:a3064–a3064. doi: 10.1136/bmj.a3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dib S, Rougeaux E, Vázquez-Vázquez A, Wells JCK, Fewtrell M. Maternal mental health and coping during the COVID-19 lockdown in the UK: data from the COVID-19 New Mum Study. In. Int J Gynecol Obstet. 2020;151(3):407–414. doi: 10.1002/ijgo.13397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farewell CV, Jewell J, Walls J, Leiferman JA. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. J Prim Care Community Health. 2020;11:215013272094407. doi: 10.1177/2150132720944074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gildner TE, Uwizeye G, Milner RL, Alston GC, Thayer ZM. Associations between postpartum depression and assistance with household tasks and childcare during the COVID-19 pandemic: evidence from American mothers. BMC Pregnancy Childbirth. 2021;21(1):828. doi: 10.1186/s12884-021-04300-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginja S, Coad J, Bailey E, Kendall S, Goodenough T, Nightingale S, Smiddy J, Day C, Deave T, Lingam R. Associations between social support, mental wellbeing, self-efficacy and technology use in first-time antenatal women: data from the BaBBLeS cohort study. BMC Pregnancy Childbirth. 2018;18(1):1–11. doi: 10.1186/s12884-018-2049-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjerdingen DK, Chaloner KM. The relationship of women’s postpartum mental health to employment, childbirth, and social support. J Fam Pract. 2004;38(5):465–472. [PubMed] [Google Scholar]
- Gjerdingen DK, Froberg DG, Fontaine P. The effects of social support on women’s health during pregnancy, labor and delivery, and the postpartum period. Fam Med. 1991;23(5):370–375. [PubMed] [Google Scholar]
- Gur RE, White LK, Waller R, Barzilay R, Moore TM, Kornfield S, Njoroge WFM, Duncan AF, Chaiyachati BH, Parish-Morris J, Maayan L, Himes MM, Laney N, Simonette K, Riis V, Elovitz MA. The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Res. 2020;293:113475. doi: 10.1016/j.psychres.2020.113475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetherington E, McDonald S, Williamson T, Patten SB, Tough SC. Social support and maternal mental health at 4 months and 1 year postpartum: analysis from the All Our Families cohort. J Epidemiol Community Health. 2018;72(10):933–939. doi: 10.1136/jech-2017-210274. [DOI] [PubMed] [Google Scholar]
- Hirsch BJ, Hirsch BJ. Natural support systems and coping with major life changes. Am J Community Psychol. 1980;8(2):159–172. doi: 10.1007/BF00912658. [DOI] [Google Scholar]
- Howell EA, Mora PA, Horowitz CR, Leventhal H, Howell EA, Mora PA, Horowitz CR, Leventhall H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005;105(6):1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchens BF, Kearney J. Risk factors for postpartum depression: an umbrella review. J Midwifery Womens Health. 2020;65(1):96–108. doi: 10.1111/jmwh.13067. [DOI] [PubMed] [Google Scholar]
- Kornfield SL, White LK, Waller R, Njoroge W, Barzilay R, Chaiyachati BH, Himes MM, Rodriguez Y, Riis V, Simonette K, Elovitz MA, Gur RE. Risk and resilience factors influencing postpartum depression and mother-infant bonding during COVID-19. Health Aff. 2021;40(10):1566–1574. doi: 10.1377/hlthaff.2021.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H-C, Zehnah PL, Koire A, Mittal L, Erdei C, Liu CH. Maternal self-efficacy buffers the effects of COVID-19–related experiences on postpartum parenting stress. J Obstet Gynecol Neonatal Nurs. 2022;51(2):177–194. doi: 10.1016/j.jogn.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CH, Hyun S, Mittal L, Erdei C (2021) Psychological risks to mother–infant bonding during the COVID-19 pandemic. Pediatr Res. 10.1038/s41390-021-01751-9 [DOI] [PMC free article] [PubMed]
- Maharlouei N (2016) The importance of social support during pregnancy. Women’s. Health Bull 3(1). 10.17795/whb-34991
- Mckee M, Cunningham M, Jankowski KR, Zayas L. Health-related functional status in pregnancy: relationship to depression and social support in a multi-ethnic population. Obstet Gynecol. 2001;97(6):988–993. doi: 10.1016/S0029-7844(01)01377-1. [DOI] [PubMed] [Google Scholar]
- Moore TM, Martin IK, Gur OM, Jackson CT, Scott JC, Calkins ME, Ruparel K, Port AM, Nivar I, Krinsky HD, Gur RE, Gur RC. Characterizing social environment’s association with neurocognition using census and crime data linked to the Philadelphia Neurodevelopmental Cohort. Psychol Med. 2016;46(3):599–610. doi: 10.1017/S0033291715002111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers S, Emmott EH. Communication across maternal social networks during England’s first national lockdown and its association with postnatal depressive symptoms. Front Psychol. 2021;12:648002. doi: 10.3389/fpsyg.2021.648002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negron R, Martin A, Almog M, Balbierz A, Howell EA. Social support during the postpartum period: mothers' views on needs, expectations, and mobilization of support. Maternal and child health journal. 2013;17(4):616–623. doi: 10.1007/s10995-012-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohara M, Okada T, Aleksic B, Morikawa M, Kubota C, Nakamura Y, Shiino T, Yamauchi A, Uno Y, Murase S, Goto S, Kanai A, Masuda T, Nakatochi M, Ando M, Ozaki N. Social support helps protect against perinatal bonding failure and depression among mothers: a prospective cohort study. Sci Rep. 2017;7(1):9546. doi: 10.1038/s41598-017-08768-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr ST. Social support and pregnancy outcome: a review of the literature. Clin Obstet Gynecol. 2004;47(4):842–855. doi: 10.1097/01.grf.0000141451.68933.9f. [DOI] [PubMed] [Google Scholar]
- Ostacoli L, Cosma S, Bevilacqua F, Berchialla P, Bovetti M, Carosso AR, Malandrone F, Carletto S, Benedetto C. Psychosocial factors associated with postpartum psychological distress during the Covid-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703. doi: 10.1186/s12884-020-03399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe JM, Ialongo NS, Horn WF, Reinhart MA, Perradatto D. The reliability and validity of the maternal social support index. Fam Med. 1988;20(4):271–276. [PubMed] [Google Scholar]
- Porter B, Kolaja CA, Powell TM, Pflieger JC, Stander VA, Armenta RF (2019) Reducing the length of the multidimensional scale of perceived social support. European Journal of Psychological Assessment. 10.1027/1015-5759/a000553
- Puertas-Gonzalez JA, Mariño-Narvaez C, Romero-Gonzalez B, Peralta-Ramirez MI. Giving birth during a pandemic: from elation to psychopathology. Int J Gynecol Obstet. 2021;155(3):466–474. doi: 10.1002/ijgo.13803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N, Hetherington E, McArthur BA, McDonald S, Edwards S, Tough S, Madigan S. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry. 2021;8(5):405–415. doi: 10.1016/S2215-0366(21)00074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards JW. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60(3):221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh L, Canclini S, Greer K, Mathison C, Combs SM, Dickerson B, Collins K. Mothers’ experiences of pregnancy, labor and birth, and postpartum during COVID-19 in the United States. J Perinat Neonatal Nurs. 2022;36(1):55–67. doi: 10.1097/JPN.0000000000000624. [DOI] [PubMed] [Google Scholar]
- Schwab-Reese LM, Schafer EJ, Ashida S. Associations of social support and stress with postpartum maternal mental health symptoms: main effects, moderation, and mediation. Women Health. 2017;57(6):723–740. doi: 10.1080/03630242.2016.1181140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedlecki KL, Salthouse TA, Oishi S, Jeswani S. The relationship between social support and subjective well-being across age. Soc Indic Res. 2014;117(2):561–576. doi: 10.1007/s11205-013-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slomian J, Emonts P, Vigneron L, Acconcia A, Glowacz F, Reginster JY, Oumourgh M, Bruyère O. Identifying maternal needs following childbirth: a qualitative study among mothers, fathers and professionals. BMC Pregnancy Childbirth. 2017;17(1):213. doi: 10.1186/s12884-017-1398-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006;166(10):1092. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Spry EA, Moreno-Betancur M, Middleton M, Howard LM, Brown SJ, Molyneaux E, Greenwood CJ, Letcher P, Macdonald JA, Thomson KC, Biden EJ, Olsson CA, Patton GC. Preventing postnatal depression: a causal mediation analysis of a 20-year preconception cohort. Philos Trans R Soc Lond B Biol Sci. 2021;376(1827):20200028. doi: 10.1098/rstb.2020.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terada S, Kinjo K, Fukuda Y. The relationship between postpartum depression and social support during the COVID -19 pandemic: a cross-sectional study. J Obstet Gynaecol Res. 2021;47(10):3524–3531. doi: 10.1111/jog.14929. [DOI] [PubMed] [Google Scholar]
- Turner JB, Turner RJ. Social relations, social integration, and social support. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the Sociology of Mental Health. Netherlands: Springer; 2013. pp. 341–356. [Google Scholar]
- Zhou J, Havens KL, Starnes CP, Pickering TA, Brito NH, Hendrix CL, Thomason ME, Vatalaro TC, Smith BA. Changes in social support of pregnant and postnatal mothers during the COVID-19 pandemic. Midwifery. 2021;103:103162. doi: 10.1016/j.midw.2021.103162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 47 kb)
Data Availability Statement
The data are available upon request.