Abstract
Endometriosis is a chronic inflammatory condition affecting nearly 10–15% of women of reproductive age and most frequently occurs in the pelvis. Extrapelvic endometriosis leading to sacral neuropathy is rare. A 29-year old woman, para 1 (vaginal delivery 8 years previously), presented with worsening right hip and buttock pain radiating to the right leg, resulting in limping and other gait changes due to delayed diagnosis and treatment. A diagnosis of sciatic nerve endometriosis was made based on both clinical and imaging findings. The final diagnosis was confirmed on histopathological examination. Transgluteal excision of the sciatic nerve with concomitant laparoscopy for exploration of the pelvic part of the sciatic nerve and excision of the pelvic endometriosis were undertaken. The operating team included a gynaecologist, an orthopaedic surgeon and a neurosurgeon. Postoperative recovery was uneventful and physiotherapy was started. Pain and gait improved. Endometriosis of the sciatic nerve should be suspected if a patient complains of cyclical sciatica. Magnetic resonance remains the imaging modality of choice. This case report illustrates the benefit of a multidisciplinary approach.
Keywords: Endometriosis, Transgluteal, Laparoscopy, Pelvic pain, Sciatic nerve, Sciatica
Highlights
-
•
A high index of suspicion is required to diagnose sciatic nerve endometriosis.
-
•
Magnetic resonance is the best imaging modality to supplement the clinical diagnosis.
-
•
A multidisciplinary team should be involved in the care of women with sciatic nerve endometriosis.
-
•
Excellent knowledge of the retroperitoneal neuro-anatomy is essential.
-
•
The approach for such complex cases needs individualisation.
1. Introduction
Endometriosis is a chronic inflammatory condition characterised by the presence of functional endometrial-like glands and stroma outside the uterus. It affects nearly 10–15% of women of reproductive age and most frequently occurs in the pelvis [1]. Extra-pelvic endometriosis has been described infrequently, where there has been infiltration of major pelvic nerves, causing sciatic neuropathy or lumbosacral plexopathy. The typical presentation of endometriosis involving the sciatic nerve is “catamenial sciatica”, which describes the cyclical pattern and worsening of sciatica during menstruation. Being a rare entity, sciatic nerve endometriosis is often misdiagnosed, or diagnosed late, which can aggravate the emotional and physical distress of affected patients.
We report a case of endometriosis affecting both the intra-pelvic compartment in the form of deep infiltrating pelvic endometriosis (DIE) and extra-pelvic part of the right sciatic nerve near the right greater sciatic foramen. The patient was managed with a concomitant transgluteal and laparoscopic approach involving a gynaecologist, an orthopaedic surgeon and a neurosurgeon. The case highlights how, owing to its rare incidence, this condition was not diagnosed by multiple physicians of different specialities, leading to a delay in diagnosis. This in turn increased the severity of the symptoms and the morbidity for this young woman. The case is reported in accordance with CARE guidelines.
2. Case Presentation
A 29-year-old woman, parity 1 (one living child aged 8 years, delivered vaginally), presented with severe pain in the right sciatic nerve distribution, associated with limping and other gait changes. The pain worsened during menstruation. The patient first developed symptoms suggestive of endometriosis 3 years earlier (aged 26 years), when she had severe dysmenorrhoea and underwent laparoscopic endometriotic cystectomy at another institution. Following that surgery, she was on a cyclical oral contraceptive pill for six months.
She was symptomatically better for a year after her laparoscopy, but then one year after her first laparoscopy for endometriosis, she started developing mild to moderate dysmenorrhoea. She additionally started experiencing pain in her right buttock, which radiated to her right leg and foot. For this she consulted an orthopaedic surgeon and underwent magnetic resonance imaging (MRI) of the spine. She was diagnosed with lumbar disc prolapse (L5/ S1) and was prescribed gabapentin and physiotherapy. Because this afforded no relief, she consulted a neurosurgeon after six months. She had both an X-ray and an MRI scan of the spine, both of which were suggestive of Tarlov cyst. Surgery to treat this was proposed if a trial of more conservative management with physiotherapy and medical therapy proved unsuccessful.
The patient did report to the treating doctors the cyclical nature of the pan: she would develop pain around the 4th day of the menses, and it would last for 7 days. Nevertheless, sciatic nerve endometriosis was neither suspected nor detected. She began limping and had other gait changes during periods. She had another consultation, this time with a spine specialist, who suggested postural correction and physiotherapy. She also visited a gynaecologist and was prescribed dienogest for 2 months, but this did not provide pain relief. She also took homeopathy medications for one month but there was no improvement in pain symptoms. After consulting a pain specialist, she tried epidural analgesia but her symptoms kept worsening.
Thus, before the presentation reported here, the patient had consulted multiple specialists over a period of one and half years. At the current presentation, she was advised to have transvaginal ultrasound (TVS) and MRI of the pelvis. TVS was suggestive of DIE and MRI revealed a 4 cm endometriotic lesion involving the right sciatic nerve near the right greater sciatic foramen (Fig. 1). Extensive pre-operative multidisciplinary counselling was done, involving an endometriosis expert, orthopaedic surgeon and neurosurgeon, who were also later part of the operative team. A concomitant transgluteal and laparoscopic approach was planned.
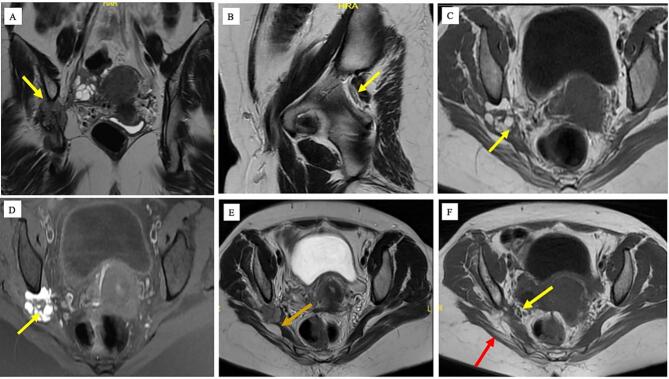
Fig. 1.
: (A) The right sciatic nerve in sacrosciatic notch is completely effaced and encased by the mass. The length of the nerve involvement was ∼5.2 cm. (B) Left sacrosciatic foramen. The left sciatic nerve was unremarkable. (C,D) There was a definite mass noted on the right, posterolateral to the right ovary, clearly separate from it, external to the iliac vessels, suggesting extraperitoneal location in the sacrosciatic foramen. The mass was 32 × 16 × 30 mm with multiple coalescent small cysts abutting and anterior to the right sciatic nerve clearly posterior and separate from the right ovary and posterior to the right sacral plexus nerves. The cyst showed signal pattern of blood (T2 shading and T1 hyperintensity) with adjacent T2 hypointense thickening, suggesting chronic inflammation and fibrosis. (E) The sacral plexus nerves (sacral gluteal and pudendal are localised between the ovary and the sciatic neural endometrioma and no evidence of encasement was noted. (F) Muscles around the right hip joint show features of atrophy involving the right pyriformis muscle (Yellow arrow), right gluteal muscles (maximus, medius and minimus) (red arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
The patient was initially placed in the prone position for the transgluteal approach to expose the right sciatic nerve. The transgluteal approach was tried first because the lesion was extra-pelvic and if it slips into the foramen when removal is attempted, it can be removed via laparoscopy later in the course of surgery. After incising fibres of the right gluteus maximus muscle and identification of the right sciatic nerve, nearly 4 cm of diffusely spread endometriotic tissue was noted near the right sciatic nerve (Fig. 2). This tissue was soft to firm in consistency, and contained chocolate-coloured fluid inside. Complete excision of this lesion was done along with the infiltrated tissue, which appeared scarred and fibrotic. Right sciatic nerve adhesions were released and nerve decompression was done. Intraoperative nerve stimulation showed physiologic continuity. The right sciatic nerve was found to be anatomically and physiologically intact.
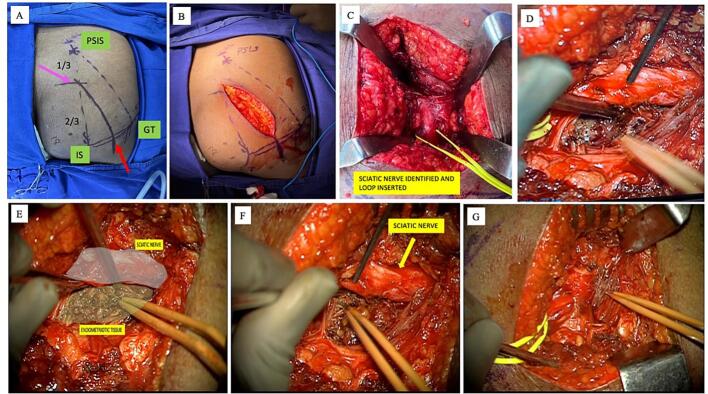
Fig. 2.
: (A,B) Patient in prone position and landmarks for incision are marked: posterior superior iliac spine (PSIS), ischial tuberosity (IT), and third greater trochanter (GT). Line joining PSIS and IT, a point at one-third and two-thirds (pink arrow), and a point midway on the line joining IS and GT (red arrow). These two points are joined and this is the surface marking for sciatic nerve. Incision is given along this line, splitting the gluteus maximus, and feeling for the sciatic nerve. (C,D) Once the sciatic nerve is identified, a vessel loop is put around the nerve and traced upwards to enter the sciatic notch and the proximal origin of sciatic nerve is identified. (E) The sciatic nerve and the endometriotic tissue and cyst in the sacrosciatic formen. (F,G) Endometriotic tissues excised with careful dissection and compression over the sciatic nerve is released. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Dorsal low lithotomy repositioning was then undertaken. On laparoscopic port placement deep infiltrating endometriosis was found. The pouch of Douglas was completely obliterated with the rectum pulled up and adherent to the lower part of the posterior surface of the uterus (Fig. 3). After the laparoscopic endometriosis excision was completed, the pelvic portion of the right sciatic nerve was explored by dissecting in the space between the right infundibulopelvic ligament, right round ligament and the external iliac vessels near the pelvic side wall. Dissection was carried out, identifying the obturator nerve and vessels, and the right sciatic foramen was reached (Fig. 4). This was to ensure complete excision of the endometriotic tissue compressing the sciatic nerve.
Fig. 3.
(A,B) Initial laparoscopic view of the pelvis with adhesions in the posterior compartment. (C) Ventrosuspension of the uterus was done, followed by bowel adhesiolysis and uterosacral nodule excision. (D) Left parametrial nodule excision done. (E, F) Final view after complete excision of bilateral uterosacral nodules, parametrial nodule excision and adhesiolysis.
Fig. 4.
(A,B,C,D) A peritoneal incision parallel to the lateral aspect of external iliac artery (blue arrow) was made, and the underlying vessels were carefully retracted. Dissection was carried out caudally to identify the proximal segment of the obturator nerve (green arrow) typically surrounded by adipose tissue at the level of pelvic brim in an oblique orientation toward the obturator foramen. The lumbosacral trunk and sciatic nerve (pink arrow) was then identified lying caudally to the proximal obturator nerve (green arrow), traveling toward the greater sciatic foramen, also surrounded by adipose tissue. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
The patient had an uneventful recovery. Physiotherapy started in the post-operative period and she was discharged 5 days after the operation. Sciatic nerve endometriosis was confirmed histopathologically. Four months post-operatively, the patient had recovered well, with no cyclical sciatica-like pain. Her gait had improved and she no longer had a limp.
3. Discussion
The sciatic nerve is the largest somatic nerve in the human body. Head et al. in 1962 first reported a case of cyclical sciatica [2]. Its precise pathogenesis is still unknown. The migration of endometrial cells from pelvic endometriotic deposits is suggested [3]. Alternative hypotheses such as hematogenous spread, coelomic metaplasia and embryonic cell rests have also been suggested, and Possover et al. proposed a “neurologic hypothesis” [4,5]. Endometriosis over the sciatic nerve can also be present in isolation, that is, without any apparent endometriosis in the pelvis [6].
The most common location of endometriotic involvement of the sciatic nerve is over the lateral aspect proximal to the greater sciatic foramen [7]. The right sciatic nerve is more commonly involved than the left. Cyclical haemorrhage into the surrounding tissues causes an inflammatory reaction, leading to fibrosis and scarring, which in turn cause further compression of the nerve.
Suspicion of sciatic nerve endometriosis is based on both clinical and imaging findings, although the final diagnosis is confirmed on histopathological examination. Clinical features suggestive of sciatic nerve endometriosis include the cyclical nature of the sciatica related to menstruation. The pain-free interval becomes progressively shorter and at later stages the pain becomes constant, but still with significant menstrual exacerbation. The pain radiates down from the gluteal region to the posterior or lateral aspect of the limb to the foot. It may be associated with sensory loss, muscle weakness and altered reflexes. Neurological findings depend on the extent of the neurological injury. Lasegue's sign can be commonly elicited, which is described as pain on raising a straight leg [8].
MRI remains the imaging modality of choice for sciatic endometriosis, as it has a sensitivity of 90% and specificity of 98% [9]. Endometriotic lesions depending on the stage of the haemorrhage exhibit high signal intensity on T1-weighted images, and high and low signal intensity on T2-weighted images [10,11]. It is important to mention that the absence of pelvic endometriosis does not exclude the diagnosis of sciatic nerve endometriosis.
The majority of these cases require surgical intervention as they are non-responsive to medical therapy [12]. Timely surgical intervention in the form of complete endometriosis excision and decompression of the sciatic nerve can prevent significant neurological damage due to the associated adhesions, fibrosis and the compression caused by endometriotic tissue over the sciatic nerve. Patients with >30% sciatic nerve damage associated with gait disturbances additionally require intensive physiotherapy for a minimum of 3 years [7]. Total recovery of the motor function is rare in advanced cases, even after complete surgical removal of the lesion. Recovery of the nerve function in the post-operative period depends on the time interval between the onset of symptoms, diagnosis and prompt intervention. This highlights the need for timely diagnosis of this condition, but this is difficult if there is lack of knowledge regarding this condition.
If the pelvic part of the sciatic nerve alone is involved, a laparoscopic or robotic approach can be carried out by a skilled gynaecologist [13]. However, when the disease affects the extra-pelvic part of the nerve solely or in addition to the intra-pelvic part, a trans-gluteal approach is required, which necessitates the involvement of a neurosurgical and orthopaedic team [14].
4. Conclusion
To conclude, sciatic nerve endometriosis should be suspected when a patient presents with symptoms of sciatica with a cyclical pattern. MRI is the best imaging modality to supplement the clinical diagnosis. A multidisciplinary team should be involved in the care of these women. The correct approach to the surgery, whether laparoscopic or transgluteal, is important and should be planned pre-operatively. Excellent knowledge of the retroperitoneal neuroanatomy is essential. Early diagnosis and prompt intervention followed by extensive physiotherapy in the post-operative period can help these patients in recovery more quickly.
Acknowledgments
Contributors
Vimee Bindra contributed to patient management and care, conception of the case report, and the literature review, drafted the manuscript, and revised the article critically for important intellectual content.
Madhavi Nori contributed to pre-operative diagnosis and editing of the manuscript.
Rajesh Reddy contributed to patient management and editing of the manuscript.
Rajeev Reddy contributed to patient management and editing of the manuscript.
Gayatri Satpathy contributed to the literature review, and drafting and editing of the manuscript.
C Archana Reddy contributed to patient management and editing of the manuscript.
All authors approved the final manuscript submitted.
Funding
This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Patient consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Provenance and peer review
This article was not commissioned and was peer reviewed.
Acknowledgments
Acknowledgements
We acknowledge the contribution of our whole team, operation theatre staff and hospital staff who helped us successfully manage this case.
Conflict of interest statement
The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Smolarz B., Szyłło K., Romanowicz H. Endometriosis: epidemiology, classification, pathogenesis, treatment and genetics (review of literature) Int. J. Mol. Sci. 2021 Sep 29;22(19):10554. doi: 10.3390/ijms221910554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Head W.B., Welch J.S., Mussey E., Espinosa R.E. Cyclic sciatica: report of a case with introduction of a new surgical sign. JAMA. 1962;180:521–524. doi: 10.1001/jama.1962.03050200005002. [DOI] [PubMed] [Google Scholar]
- 3.Dhote R., Tudoret L., Bachmeyer C., Lagmann P., Christoforov B. Cyclic sciatica: a manifestation of compression of the sciatic nerve by endometriosis: a case report. Spine. 1996;21:2277–2279. doi: 10.1097/00007632-199610010-00021. [DOI] [PubMed] [Google Scholar]
- 4.Vercellini P., Chapron C., Fedele L., Frontino G., Zaina B., Crosignani P.G. Evidence for asymmetric distribution of sciatic nerve endometriosis. Obstet. Gynecol. 2003 Aug;102(2):383–387. doi: 10.1016/s0029-7844(03)00532-5. (PMID: 12907116) [DOI] [PubMed] [Google Scholar]
- 5.Possover M., Rhiem K., Chiantera V. The “neurologic hypothesis”: a new concept in the pathogenesis of the endometriosis? Gynecol. Surg. 2005;2:107. [Google Scholar]
- 6.Possover M., Chiantera V. Isolated infiltrative endometriosis of the sciatic nerve: a report of three patients. Fertil. Steril. 2007;87(417):e17–e19. doi: 10.1016/j.fertnstert.2006.05.084. [DOI] [PubMed] [Google Scholar]
- 7.Possover M. Five-year follow-up after laparoscopic large nerve resection for deep infiltrating sciatic nerve endometriosis. J. Minim. Invasive Gynecol. 2017;24:822–826. doi: 10.1016/j.jmig.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 8.Mannan K., Altaf F., Maniar S., Tirabosco R., Sinisi M., Carlstedt T. Cyclical sciatica: endometriosis of the sciatic nerve. J. Bone Joint Surg. (Br.) 2008 Jan;90(1):98–101. doi: 10.1302/0301-620X.90B1.19832. (PMID: 18160509) [DOI] [PubMed] [Google Scholar]
- 9.Gaeta M., Minutoli F., Mileto A., et al. Nuck canal endometriosis: MR imaging findings and clinical features. Abdom. Imaging. 2010;35:737–741. doi: 10.1007/s00261-010-9607-7. [DOI] [PubMed] [Google Scholar]
- 10.Saar T.D., Pacquée S., Conrad D.H., Sarofim M., De Rosnay P., Rosen D., Cario G., Chou D. Endometriosis involving the sciatic nerve: a case report of isolated endometriosis of the sciatic nerve and review of the literature. Gynecol. Minim. Invas. Ther. 2018 Apr;7(2):81. doi: 10.4103/GMIT.GMIT_24_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pham M., Sommer C., Wessig C., Monoranu C.M., Pérez J., Stoll G., Bendszus M. Magnetic resonance neurography for the diagnosis of extrapelvic sciatic endometriosis. Fertil. Steril. 2010 Jun;94(1) doi: 10.1016/j.fertnstert.2009.12.046. 351.e11-4. Epub 2010 Feb 10. PMID: 20149357. [DOI] [PubMed] [Google Scholar]
- 12.Arányi Z., Polyák I., Tóth N., Vermes G., Göcsei Z. Ultrasonography of sciatic nerve endometriosis. Muscle Nerve. 2016;54:500–505. doi: 10.1002/mus.25152. [DOI] [PubMed] [Google Scholar]
- 13.Roman H., Seyer-Hansen M., Dennis T., Merlot B. Excision of deep endometriosis nodules of the sciatic nerve in 10 steps. J. Minim. Invasive Gynecol. 2021 Oct;28(10):1685–1686. doi: 10.1016/j.jmig.2021.05.019. Epub 2021 Jun 4. PMID: 34091045. [DOI] [PubMed] [Google Scholar]
- 14.Yanchun L., Yunhe Z., Meng X., Shuqin C., Qingtang Z., Shuzhong Y. Removal of an endometrioma passing through the left greater sciatic foramen using a concomitant laparoscopic and transgluteal approach: case report. BMC Womens Health. 2019 Jul 12;19(1):95. doi: 10.1186/s12905-019-0796-0. PMID: 31299947; PMCID: PMC6624926. [DOI] [PMC free article] [PubMed] [Google Scholar]