Abstract
Background
The postnatal period is a critical in the lives of mothers and babies due to the risk of maternal and perinatal morbidity and mortality. According to the Nigeria Demographic Health Survey 2018, only 38 % of women and 42;% of newborns received a postnatal check in the first 2 days after birth. The World Health Organisation (WHO) recommends that postpartum women should have contact with healthcare providers within 24 h, at day 3, days 10–14 and 6 weeks post-delivery. Multiple postnatal clinic (PNC) visits will allow assessment and prompt treatment of complications arising from delivery. This study assessed the attitude of postpartum women towards multiple PNC schedule.
Methods
This descriptive cross-sectional study assessed the attitude of postpartum women towards multiple PNC schedules. A total of 167 respondents participated in the study and data was collected using a semi-structured interviewer administered questionnaire. Information on awareness, knowledge and purpose of postnatal care, preference for multiple schedules and the timing of postnatal care visits were obtained. Data was analysed using IBM SPSS version 23; and the level of significance was set at p < 0.05.
Results
Of the respondents, 71.9 % had poor or incorrect knowledge. About 87.4 % perceived PNC as beneficial; and that mothers and newborns should be seen at least three times (47.9 %) in the postnatal period. A high proportion of women were willing to come for PNC on day 3 (74.3 %), days 10–14 (86.2 %) and six weeks postpartum (91.6 %). Also, 69.5 % were willing to come for multiple PNC visits. Parity was significantly associated with willingness to attend multiple PNC visits.
Conclusion
Despite suboptimal knowledge of the components of postnatal care services, postpartum women have a good attitude to postnatal care and are willing to attend scheduled and multiple PNC schedules. However, fewer women wanted the multiple PNC schedules. Health education and quality postnatal care will enhance postpartum surveillance with prompt detection and treatment of maternal and neonatal complications to forestall life-threatening complications or mortality.
Keywords: Postnatal care, Postpartum care, Postnatal clinic, Multiple postnatal clinic visit, Postnatal clinic schedule
1. Introduction
Postnatal care is care given to the mother and newborn baby after the delivery up to six weeks post-partum [1]. The postnatal period is critical in the lives of women and newborns as a wide range of maternal and infant morbidity and mortality occur at this time [2]. Despite this, the postnatal period often receives less attention from the obstetricians and postpartum women compared to pregnancy, labour and delivery [3]. In the postpartum period, the woman is saddled with recovery from childbirth, concerns about newborn care, nutrition, breastfeeding, immunisation, family planning and so on. Postnatal care will enable the healthcare professionals identify post-delivery problems, potential risks and complications, and provide prompt treatments including follow-up [4].
According to the Nigeria Demographic and Health Survey (NDHS) 2018, only 38 % of women and 42 % of newborns received a postnatal check within the first two days after birth [5]. Perinatal mortality rates decreased by 8 % during this period - from 40 deaths per 1000 live births to 37 deaths per 1000 live births [6]. Despite the health benefits of PNC, the NDHS 2013 reported that 58 % of Nigerian women had no postnatal check-up [6]. The proportion of women receiving a postnatal check-up within 2 days of delivery is higher in urban than rural areas (61 % and 30 %, respectively) and increases with increasing education and wealth [5], [7].
Most maternal and infant deaths occur in the first month after birth; almost half of the postnatal maternal deaths occur within the first 24 h, and 66 % occur during the first week. The maternal mortality ratio in Nigeria is 512 deaths/100,000 live births according to the NDHS 2018 [5].
In 2013, the World Health Organisation (WHO) recommended that postpartum women should have contact with a maternal healthcare provider within 24 h of delivery, at day 3, between days 10–14 and at 6 weeks postpartum. This will allow prompt detection and treatment of complications, as well as counsel women on care of mother and newborn [2], [8]. The WHO guidelines for postnatal care emphasised the need for more contacts with mothers and babies after delivery, especially in low-income and resource poor countries. While addressing the timing, number, place of contact, and content of postnatal care for mothers and babies during the six weeks after birth; it focused on assessment of mothers and newborns to detect complications [2].
Various factors such as maternal age, region, employment status, desire for the pregnancy, health insurance coverage, maternal autonomy and decision-making affect PNC attendance by women [9]. In Northern Nigeria, the predictors of postnatal care utilisation among women in the rural areas are different from urban settings. The predictors of utilisation of PNC services among women in the urban areas were large-sized babies, wealth status, age and transportation problems, while in the rural setting, paternal and maternal education, hospital waiting-time of ≤ 30 min; family sociocultural and financial issues were factors identified [10]. Antenatal clinic (ANC) attendance can positively predict PNC utilisation among women in the rural and urban areas [9], [10]. Using NDHS (2013), Agho et al. found that poverty, rural dwelling, poor maternal education, and limited access to the mass media were associated with lack of PNC patronage [11]. It is estimated that if routine PNC and curative care in the postnatal period reached 90 % of babies and mothers; 10–27 % of newborn deaths could be averted thus saving up to 310,000 newborn lives a year in Africa [12]. The impact of PNC on maternal survival and well-being would also be significant. The previous schedule of a single PNC visit at six weeks may allow complications in the early postpartum period to worsen before presentation. The reported incidence of re-admission during the puerperium varies between 0.7 % and 3 % [13], [14]. In Lagos Nigeria, the incidence of re-admission was 0.5 % (118 out of 6081). Of 34 subjects delivered in the facility, 20(58.8 %) were re-admitted within the second- and third-week postpartum [15]. .
There is a consensus on the content of PNC, but questions about the best timing, place for PNC visits and who can deliver this package have been addressed by the new WHO PNC recommendations. Among the crucial health indicators of using postnatal care are mother/newborn receiving PNC within three days, subsequent follow-up visits, place where care is provided and type of care provider [12]. After an uncomplicated vaginal birth in a health facility, healthy mother and newborn should receive care/postnatal care for at least 24 h after birth. If birth was at home, the first postnatal contact should be as early as possible within 24 h of birth. At least three additional postnatal contacts are recommended for all mothers and newborns, on day 3, between days 7–14, and six weeks post-delivery. Home visit in the first week after birth is recommended for care of the mother and newborn [2].
In Nigeria and some countries, this is yet to be domesticated. Considering the low prevalence of uptake of single PNC visit at 6weeks among postpartum women in Nigeria, there is a need to determine the acceptability of multiple PNC schedule and willingness of the women to attend. This study assessed the attitude of postpartum women towards multiple PNC schedule.
2. Materials and methods
2.1. Study design
This study was a cross-sectional prospective study among postpartum women over a three-month period.
2.2. Study location/setting
The study was conducted at the Obstetric unit of the University College Hospital (UCH), Ibadan, Southwest Nigeria – a government owned tertiary healthcare facility.
2.3. Study population
This included postpartum women who recently delivered at the obstetric unit of UCH, Ibadan. Postpartum women were counselled on the purpose of the study, consenting women were enroled and interviewed. Women on admission for more than a week post-delivery before discharge were excluded. A sample size of 167 was calculated using a prevalence of postnatal care uptake of 42 %.
2.4. Postpartum care protocol
At the study site, pregnant women receive antenatal, labour and delivery care by skilled birth attendants. In the postpartum period, women receive postpartum care; counselling on postnatal care, family planning, immunisation, exclusive breastfeeding and Papanicolaou test. Women are discharged between the second and fifth- postpartum day for follow-up care at the PNC in 6 weeks. High risk postpartum women are seen earlier in the PNC.
2.5. Data collection
Ethical approval was obtained from the ethical review committee of University of Ibadan /University College Hospital, Ibadan, Nigeria. Ethical approval number- UI/EC/20/0493. Data was collected using a pretested semi-structured interviewer-administered questionnaire. The information obtained included socio-demographic and obstetric characteristics, maternal and foetal outcomes, respondents’ knowledge and attitude to multiple of PNC schedule, and preferred timing of the visit. The knowledge was categorised into poor, fair and good based on the number of key components of postnatal care services the respondent was able to mention. The eight components of knowledge assessed included the knowledge and ability to identify maternal postpartum and neonatal complications, monitoring of mother and baby for at least 24 h postpartum in the hospital; counselling on exclusive breastfeeding, family planning, infant immunisation, nutrition, personal hygiene and Papanicolaou smear. The categories were Poor knowledge for 0–2 components, Fair Knowledge – 3–4 components, and good knowledge – 5–8 components.
2.6. Data analysis
Data was entered and analysed using the IBM SPSS version 23. Descriptive statistics and bivariate analysis was conducted.
3. Results
This study assessed the postpartum women’s knowledge of postnatal care and attitude to multiple PNC schedules. One hundred and sixty-seven respondents were interviewed and analysed.
Table 1 shows the socio-demographic characteristics of respondents. Majority (75 %) were in the age bracket 26–35 years. Participants were married (98.2 %), Christian (68.3 %), Yoruba (76.6 %) and had a tertiary level of education (88.0 %). They were mostly in unskilled employment (34.1 %) or professionals (30.5 %). The obstetrics characteristics, maternal and foetal outcomes are shown in Table 2. The respondents were mostly booked (74.9 %), multiparous (64.1 %) women. About 62.2 % had no post-delivery complications, 92.2 % were satisfied with their health status at delivery, 65.3 % had a haematocrit of > 30 %, while 34.7 % had mild anaemia. A normal birth weight (2.5–3.9 kg) was seen in 74.2 %; low birth weight in 22.8 %; and 78.4 % had no neonatal complications.
Table 1.
Socio-demographic characteristics of the respondents.
| Variables | Frequency (N = 167) | Percentage |
|---|---|---|
| Age (Years) | ||
| < 25 | 16 | 9.6 |
| 26–30 | 57 | 34.1 |
| 31–35 | 70 | 41.9 |
| > 35 | 24 | 14.4 |
| Marital Status | ||
| Married | 164 | 98.2 |
| Single | 3 | 1.8 |
| Religion | ||
| Christianity | 114 | 68.3 |
| Islamic | 51 | 30.5 |
| Others | 2 | 1.2 |
| Occupation | ||
| Unemployed | 19 | 11.4 |
| Unskilled | 57 | 34.1 |
| Skilled | 40 | 24.0 |
| Professional | 51 | 30.5 |
| Tribe | ||
| Yoruba | 128 | 76.6 |
| Igbo | 19 | 11.4 |
| Other tribes | 20 | 12.0 |
| Level of Education | ||
| None/Primary | 7 | 4.2 |
| Secondary | 13 | 7.8 |
| Tertiary | 147 | 88.0 |
| Family Income (Naira) | ||
| None | 21 | 12.6 |
| < 50,000 ($100) | 62 | 37.1 |
| 50,000–100,000($100–200) | 43 | 25.7 |
| 100,000–150,000($100–300) | 19 | 11.4 |
| > 150,000 ($300) | 22 | 13.2 |
Table 2.
Obstetrics characteristics, maternal and foetal outcomes of the respondents.
| Variables | Frequency (N = 167) | Percentage |
|---|---|---|
| Parity | ||
| Primiparous | 60 | 35.9 |
| Multiparous | 107 | 64.1 |
| Antenatal care Booking Status | ||
| Booked | 125 | 74.9 |
| Unbooked | 42 | 25.1 |
| Gestational age at booking | ||
| 1st Trimester | 26 | 15.6 |
| 2nd Trimester | 81 | 48.5 |
| 3rd Trimester | 18 | 10.8 |
| Not sure | 42 | 25.1 |
| Mode of Delivery | ||
| Vaginal delivery | 85 | 50.9 |
| Caesarean section | 82 | 49.1 |
| Medical co-morbidity in pregnancya | ||
| Yes | 50 | 29.9 |
| No | 117 | 70.1 |
| Foetal Status | ||
| Alive | 161 | 96.6 |
| Perinatal death | 6 | 3.6 |
| Birth Weight | ||
| Low birth weight (< 2.5 kg) | 38 | 22.8 |
| Normal (2.5–3.9 kg) | 124 | 74.2 |
| Macrosomia (4.0 and above) | 5 | 3.0 |
| Neonatal Complication** | ||
| Yes | 36 | 21.6 |
| No | 131 | 78.4 |
| SCBU admission | ||
| Yes | 11 | 6.6 |
| No | 156 | 93.4 |
| Anaemia at discharge (PCV < 30 %) | ||
| Yes | 58 | 34.7 |
| No | 109 | 65.3 |
| Postpartum health satisfaction | ||
| Satisfied | 154 | 92.2 |
| Indifferent | 7 | 4.2 |
| Dissatisfied | 6 | 3.6 |
| Immediate postpartum complications | ||
| Postpartum haemorrhage | 10 | 6.0 |
| Delayed lactation | 25 | 15.0 |
| Others | 28 | 16.8 |
| None | 104 | 62.2 |
**Neonatal Complications: Neonatal jaundice, neonatal sepsis, perinatal asphyxia.
Medical Co-morbidities: Hypertensive disorders of pregnancy, asthma, sickle cell disease, malaria, Human Immunodeficiency Virus Infection.
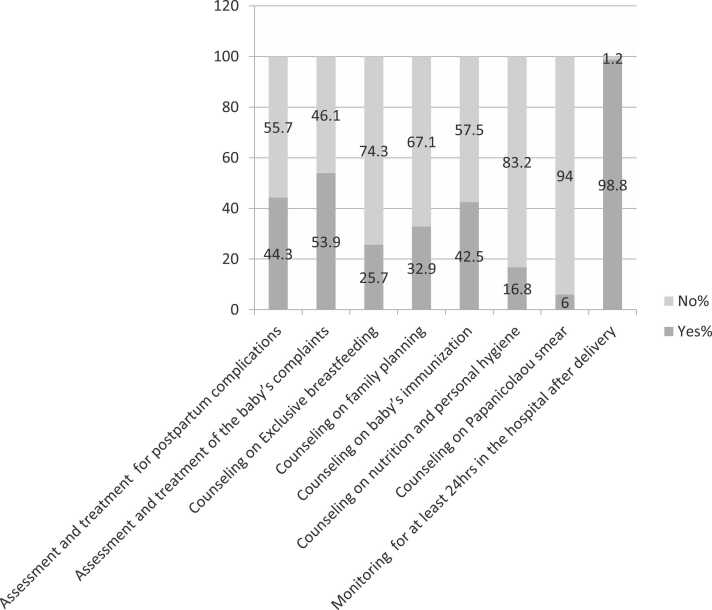
Poor knowledge of PNC was high (71.9 %), and only 4.1 % had good knowledge. (Table 3). Fig. 1 shows the knowledge of PNC components among respondents. Women’s willingness to attend PNC, preference for the timing and multiple PNC schedule are shown in Table 4. A high proportion of women were willing to attend PNC. However, fewer women (69.5 %) were willing to return for multiple PNC visits. Preference and willingness to attend multiple PNC schedules were associated with parity as shown in (Table 5).
Table 3.
Knowledge and perception of postnatal care.
| Variables | Frequency (n = 167) | Percentage |
|---|---|---|
| PNC within 24 h beneficial | ||
| Yes | 146 | 87.4 |
| No | 2 | 1.2 |
| Not sure | 19 | 11.4 |
| Knowledge of PNC services | ||
| Poor knowledge | 120 | 71.9 |
| Fair knowledge | 40 | 24.0 |
| Good knowledge | 7 | 4.1 |
| PNC is mandatory | ||
| Yes | 144 | 86.2 |
| No | 20 | 12.0 |
| Not sure | 3 | 1.8 |
| Number of PNC visit | ||
| 0 | 5 | 3.0 |
| 1 | 30 | 18.0 |
| 2 | 52 | 31.1 |
| 3 and above | 80 | 47.9 |
*PNC – Postnatal care.
Fig. 1.
Distribution of knowledge of post-natal care services components.
Table 4.
Willingness and preference for timing of postnatal clinic visit in the postpartum period.
| Variables | Frequency (N = 167) | Percentage |
|---|---|---|
| Willingness to attend PNC on Day 3 | ||
| Willing | 124 | 74.3 |
| Unwilling | 43 | 25.7 |
| Willingness to attend PNC on Days 10–14 | ||
| Willing | 144 | 86.2 |
| Unwilling | 23 | 13.8 |
| Willingness to attend PNC at 6 weeks | ||
| Willing | 153 | 91.6 |
| Unwilling | 14 | 8.4 |
| Willingness to attend multiple* PNC | ||
| Willing | 116 | 69.5 |
| Unwilling | 51 | 30.5 |
* PNC – Postnatal care.
*Multiple PNC – On day 3, days 10–14 and 6 weeks.
Table 5.
Association between socio-demographic characteristics and preference for multiple postnatal visits.
| Variable | χ2/chi-square | P-value |
|---|---|---|
| Age | 13.259 | 0.582 |
| Occupation | 11.143 | 0.517 |
| Level of education | 3.319 | 0.950 |
| Family income | 11.945 | 0.850 |
| Means of transportation | 2.31 | 0.884 |
| Parity | 18.165 | 0.033* |
| Gestational age at booking | 4.695 | 0.583 |
| PNC knowledge | 5.418 | 0.796 |
| Neonatal complications | 0.888 | 0.825 |
*Significant.
4. Discussion
This study evaluated the knowledge and attitude of postpartum women to multiple PNC visits. The main finding is that the correct knowledge of PNC and its components was low. About 7 in 10 respondents had poor knowledge of postnatal care components. Only a few participants had in-depth knowledge of PNC. Majority of the women were willing to return for PNC on either day 3, day 10–14 or 6weeks postpartum. However, only about two-thirds were willing to attend multiple PNC schedule (Table 5).
The majority were aged 26–35years, mostly married, Christians and Yoruba. The study evaluated women in the reproductive age-group, hence the age-range. This is similar to the findings of Ilesanmi et al. evaluating the quality of postnatal care and mothers’ satisfaction at UCH, Ibadan [7]. This is higher than the age-range found by Igboanusi et al. evaluating the factors affecting the utilisation of PNC in Primary Health Care facilities in urban and rural settlements in Kaduna, North-western Nigeria [10]. The early ages at marriage in the Northern Nigeria explains the difference. The participants had tertiary level of education, this is higher than the level reported by Nankwanga et al. and Igboanusi et al. [10], [16].
Poor knowledge of PNC components was high, and less than a third demonstrated fair to good knowledge. The awareness and ability to identify specific components of PNC services was low, as less than 50 % of the respondents knew of counselling on family planning, immunisation, exclusive breastfeeding, and management of maternal postpartum complications as components. A few women knew about counselling on cervical cancer screening - Papanicolaou smear and nutrition/personal hygiene as part of PNC. This is similar to the reports of Ugboaja et al. in South-East, Ayinde et al. in South-west and Oche et al. in North-West, Nigeria [17], [18], [19]. Despite this finding, about 9 in 10 women agreed that hospital-based postpartum assessment within 24 h of delivery is beneficial and that postpartum women should attend PNC. This suggests a good perception of utilisation of postnatal care. Appropriate counselling and health education will improve the awareness, knowledge, perception and utilisation of PNC services among postpartum women. In this study, participants delivered in the healthcare facility and received postnatal care in the immediate postpartum and up to 24–48 h post-delivery, thus providing an opportunity for quality postnatal care, counselling, health education, and follow-up care for mother and newborn. This is similar to other report; women who delivered in the healthcare facility are more likely to receive early postnatal care [20].
Concerning the timing of PNC appointments, respondents were willing to attend PNC on either the third day (7 of 10), second week (8 of 10) and sixth week (9 of 10) respectively. Women were willing to come for PNC on the scheduled appointment day, more women preferred to come at 6 weeks. Despite this, it is interesting that only about two-thirds of the postpartum women were willing to come for the three appointments as multiple PNC visit schedule. In contrast, Abubakar et al. showed that there was high knowledge of PNC services, however, this did not translate positively to willingness to attend PNC among women of child-bearing age [21]. Multiple PNC schedule may be acceptable among postpartum women in some settings; acceptability and uptake of PNC may vary from region to region.
The high willingness in this study may be explained by good health-seeking behaviour, ANC attendance, high level of education and satisfaction with their health status at the time of discharge. Parity was associated with willingness to attend multiple PNC visits and may be due to having had a previous experience of PNC attendance. Women who were adequately counselled and educated on the importance PNC are more willing to utilise it after delivery. This shows the feasibility of practising the WHO recommendation in terms of frequency and timing of postnatal contacts. At least, three additional contacts are recommended for all mothers and newborns, on day 3, 2 and 6 weeks after birth [2], [8].
The uptake and quality of postnatal care are affected by place of delivery, provider of first postnatal checkup, provider of postnatal care, level of education, parity, women in urban areas, location of delivery, wealth and socioeconomic status, patient’s perception of quality care and availability of manpower [20], [22], [23]. Postpartum women with higher wealth quintile and education are more likely to receive postnatal care from skilled healthcare provider. Younger women, with no education, higher parity women, women in the rural areas are less likely to receive antenatal care [6], [20].
The coverage of postnatal care in Nigeria is suboptimal with only 42 % of postpartum women receiving a postnatal care which is beneficial to both the mother and the baby. Thus, the postpartum women may be reluctant to come for multiple PNC visits. Although many women were willing to attend postnatal care at scheduled times during the period, a fewer proportion of women were willing to return for multiple visits. The multiple PNC schedule may be affected by lower compliance, uptake by postpartum women, patient load as well as inadequate manpower. Multiple PNC schedule will be challenging in a setting of high client-provider ratio [22]. It is important to consider various factors in the implementation of multiple PNC schedule. The recommendation should be domesticated and modified to fit the peculiarities of various healthcare settings and regions at implementation [2], [8]. Health education, counselling and reinforcement of counselling during the antenatal and postnatal periods, and impactful postnatal care will enhance quality care desired for the mother and newborn. Strategies to improve postnatal uptake and compliance should be explored. These may include community healthcare provider home visit, virtual consultation where the facility is available and staggered clinic appointment to reduce waiting time [24], [25]. During the COVID-19 pandemic lockdown, PNC uptake was affected in many regions and interventions such as telemedicine was found to be a useful and effective tool for patient management when clinic attendance reached its nadir [25], [26].
The limitation is that this study did not compare timing and number of ANC visits attended with respondents’ preference, acceptability and willingness to return for multiple PNC schedule.
In conclusion, despite poor knowledge of postnatal care, women had good attitude, perception and showed willingness to attend multiple PNC schedules. The antenatal care period, particularly the first ANC contact should be used as an opportunity and primer for health education and counselling on contents, benefits and compliance with antenatal and postnatal care. The components of postnatal care and importance of frequent visits should be explained and emphasised to women during antenatal and at discharge to improve attitude towards multiple PNC schedules. These will reduce maternal and infant morbidities and mortalities from treatable complications when identified and managed early before deterioration in clinical condition.
CRediT authorship contribution statement
Sanusi TA: Design, planning, conduct, interpretation of results, and manuscript writing. Abdus-salam RA (RA): Design, planning, conduct, data analysis, interpretation of results, and manuscript writing. Oladokun A: Design, planning, conduct, data analysis, interpretation of results, and manuscript writing.
Ethical approval
This study was approved by the institutional ethics Review Committee of University College Hospital and the College of Medicine, University of Ibadan (UI/UCH Ethics committee – UI/EC/20/0493). Voluntary and informed consent of the participants was obtained.
Funding Statement
Self-sponsored.
Declaration of Competing Interest
This is a declaration that the authors of this research work and manuscript have no conflicts of interest.
Acknowledgement
None.
Submission Declaration
This work has not been published previously in any journal or in any other form.
Statement of Informed Consent
All participants in this study gave voluntary informed consent.
References
- 1.W.H.O . Technical consultation on postpartum and postnatal care: department of making pregnancy safer. World Health Organisation; Switzerland: 2010. p. 12. [PubMed] [Google Scholar]
- 2.WHO. Recommendations on postnatal care of the mother and newborn. World Health Organization; 2013. [PubMed]
- 3.Onoh R.C., Umeora O.U.J., Ezeonu P.O., et al. Prevalence, pattern and consequences of intimate partner violence during pregnancy at Abakaliki, Southeast Nigeria. Ann Med Health Sci Res. 2013;3:484–490. doi: 10.4103/2141-9248.122048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Umar N.J., Sanusi A.A., Rejuaro F.M., et al. Knowledge and utilization of post natal care services among women in Edu Local Government Area, Kwara State, Nigeria. J Res Nurs Midwifery (JRNM) 2017;61:1–6. [Google Scholar]
- 5.National Population Commission (NPC) [Nigeria], ICF. Nigeria demographic and health survey 2018. Abuja, Nigeria: NPC; Rockville, Maryland, USA: ICF; 2019.
- 6.National Population Commission (NPC) [Nigeria], ICF International. Nigeria demographic and health survey 2013. Abuja, Nigeria: NPC; Rockville, Maryland, USA: ICF International; 2014.
- 7.Ilesanmi R.E., Akinmeye J.A. Evaluation of the quality of postnatal care and mothers’ satisfaction at the university college hospital Ibadan. Niger Int J Nurs Midwifery. 2018;10(9):99–108. [Google Scholar]
- 8.Postnatal care guidelines: highlights from WHO recommendations. World Health Organization; 2015.
- 9.Tukur D.I., Oche M.O. Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr Med J. 2015;21:321. doi: 10.11604/pamj.2015.21.321.6527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Igboanusi C.J., Sabitu K., Gobir A.A. Factors affecting the utilization of postnatal care services in primary health care facilities in urban and rural settlements in Kaduna State. North-West Niger Am J Public Health Res. 2019;7(3):111–117. [Google Scholar]
- 11.Agho K.E., Ezeh O.K., Issaka A.I., et al. Population attributable risk estimates for factors associated with nonuse of postnatal care services among women in Nigeria. BMJ. 2016;6 doi: 10.1136/bmjopen-2015-010493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Warren C, Daly P, Toure L. Postnatal care. Opportunities for Africa’s Newborns; Chapter 4, p. 79–90.
- 13.Lydon-Rochelle M., Holt V., Martin D.P., Easterling T.R. Association between method of delivery and maternal re-hospitalization. JAMA. 2000;283:2411–2416. doi: 10.1001/jama.283.18.2411. [DOI] [PubMed] [Google Scholar]
- 14.Glazener C.M., Abdalla M., Stroud P., Naji S., Templeton A., Russell I.T. Postnatal maternal morbidity: extent, causes, prevention and treatment. Br J Obstet Gynaecol. 1995;102(4):282–287. doi: 10.1111/j.1471-0528.1995.tb09132.x. [DOI] [PubMed] [Google Scholar]
- 15.Oshodi Y.A., Gbadegesin A., Akinlusi F.M., et al. Pattern of postpartum re-admission in Lagos, Nigeria. Int J Recent Sci Res. 2019;10(10):35554–35558. [Google Scholar]
- 16.Nankwanga A. Factors influencing utilisation of postnatal services in Mulago and Mengo Hospitals Kampala, Uganda. University of the Western Cape Library Portal; 2004. 〈http://hdl.handle.net/11394/237〉 [Google Scholar]
- 17.Ugboaja J.O., Berthrand N.O., Igwegbe A.O., Ob-Nwosu A.L. Barriers to postnatal care and exclusive breastfeeding among urban women in Southeast Nigeria. Niger Med J. 2013;54(1):45–50. doi: 10.4103/0300-1652.108895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ayinde O.A., Omigbodun A.O., Ilesanmi A.O. Awareness of cervical cancer, Papanicolaou’s smear and its utilization among female undergraduates in Ibadan. Afr J Reprod Health. 2004;8(3):68–80. [PubMed] [Google Scholar]
- 19.Oche M.O., Umar A.S., Ahmed H. Knowledge and practice of exclusive breastfeeding in Kware, Nigeria. Afr Health Sci. 2011;11(3):518–523. [PMC free article] [PubMed] [Google Scholar]
- 20.National Population Commission (NPC) [Nigeria], ICF. Nigeria demographic and health survey 2018, Abuja, Nigeria: NPC; Rockville, Maryland, USA: ICF; 2019.
- 21.Abubakar K., Akanbi L., Saliohu R. Willingness of women to utilize postnatal care services in Edu LGA of Kwara state, Nigeria. Afr J Nurs Midwifery. 2017;5(1):689–694. [Google Scholar]
- 22.Okonofua F., Ntoimo L., Ogu R., Galandaci H., Abdus-Salam R., Gana M., et al. Association of the client-provider ration with the risk of maternal mortality in referral hospitals: a multi-site study in Nigeria. Reprod Health. 2018;15(1):32. doi: 10.1186/s12978-018-0464-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nwaeze I.L. Perception and satisfaction with quality of antenatal care services among pregnant women at the University College Hospital, Ibadan. Ann Ib Postgrad Med. 2013;11(1):22–28. [PMC free article] [PubMed] [Google Scholar]
- 24.Abdus-Salam RA, Adeniyi AA, Bello FA. Antenatal clinic waiting time. Patient satisfaction and preference for staggered appointment–a cross-sectional study. J Pat Exp. Vol. 8, 23743735211060802. [DOI] [PMC free article] [PubMed]
- 25.James O., Akinboboye B.O., Okunade K.S., Adekunle A.A., Adeyemo W.L. Evaluation of the use and effectiveness of telemedicine among health professionals during the COVID-19 lockdown period: a cross sectional study. J Clin Sci. 2021;18:117–122. [Google Scholar]
- 26.Abdus-Salam R.A., Idowu O.C., Sanusi A.T. Utilization of postnatal care during COVID-19 pandemic: perception and intents of postpartum women at Tertiary Health Facility in Southwest, Nigeria. J Pat Exp. 2022;9 doi: 10.1177/23743735221106595. [DOI] [PMC free article] [PubMed] [Google Scholar]