Abstract
Renal artery stenosis (RAS) is associated with hypertension and high mortality rates. With its prevalence and associated risk of death, it is important to screen for patients displaying symptoms of RAS. RAS has a wide spectrum of clinical manifestations and is usually resistant to medical therapy. Of these clinical manifestations is Pickering syndrome which is characterized by bilateral renal arterial occlusion inflow lesions, flash pulmonary edema, acute kidney injury, and hypertensive emergencies in the setting of a preserved left ventricle function. Stenting techniques have been used extensively to treat symptomatic renal artery stenosis with excellent primary patency rate, however have failed to demonstrate a long-term benefit over the optimal medical management alone in randomized trials. However, accumulating evidence suggests that stenting is justified in specific patient subgroups that have severe occlusive renal artery stenoses with significant clinical sequelae, including flash pulmonary edema, acute ischemic kidney injury, and uncontrolled hypertension. In this report we discuss the case of a 32-year-old male who presented to our center with recurrent flash pulmonary edema and hypertensive emergency and was found to have RAS, which responded well to renal artery stenting. In conclusion, correcting the renal arterial inflow stenosis is beneficial and warranted in selective clinical scenarios.
Keywords: Pickering syndrome, Renal artery, Stenting, Stenosis
Introduction
The primary symptom of renal artery stenosis (RAS) is hypertension that is usually resistant to medical therapy [1], [2], [3]. RAS is associated with a high mortality rate. The prevalence of significant RAS using ultrasound screening in 824 free-living Medicare patients with an average age of 77 years was 6.8% [4]. It is important to note that RAS can occur bilaterally and as a result, tests which rely on difference in renal perfusion between the kidneys are not preferred [4]. When patients with RAS present with flash pulmonary edema in the setting of preserved left ventricle function and hypertension, this constellation of findings is called Pickering syndrome [1]. While the recommended therapy of RAS is medical in nature, there is a role for angioplasty and stenting in a group of patients [4]. Here, we report on a 32-year-old male with a single kidney who presented with recurrent flash pulmonary edema and hypertensive emergency and was found to have severe RAS, which responded well to renal artery stenting [[5], [6], [7]].
Case report
A 32-year-old African-American male presented with dyspnea, flash pulmonary edema, hypertensive emergency, and worsening renal function. His past medical history was remarkable for hypertension, chronic kidney disease (baseline creatinine 2.1 mg/dL), and antiphospholipid antibody syndrome, which caused left hemiplegia and right atrophic kidney. Notably, the patient had multiple admissions with similar presentation of flash pulmonary edema accompanied with hypertensive emergencies and recurrent acute kidney injury requiring dialysis. During this admission, he was treated with intravenous antihypertensive medications and diuretics with poor response. Laboratory data were significant for serum creatinine 6.2 mg/dL, metabolic acidosis, and normal left renal artery Doppler. Preserved left ventricle function was noted on echocardiogram. Magnetic resonance imaging of the abdomen without contrast revealed total occlusion of both right renal artery and infra-renal abdominal aorta as well as severe stenosis of left renal artery. Renal artery angiogram confirmed high-grade stenosis of the left renal artery (Fig. 1A and B). Subsequently, he underwent renal artery angioplasty and stenting (Fig. 2) with marked improvement of the renal function (serum creatinine improved from 6.2 to 2.3 mg/dL). The patient did not require further dialysis and the blood pressure was better controlled.
Fig. 1.
Selective cannulation and angiogram showed severe osteal stenosis of the left renal artery (A, arrow) with poor perfusion of the renal cortex (B).
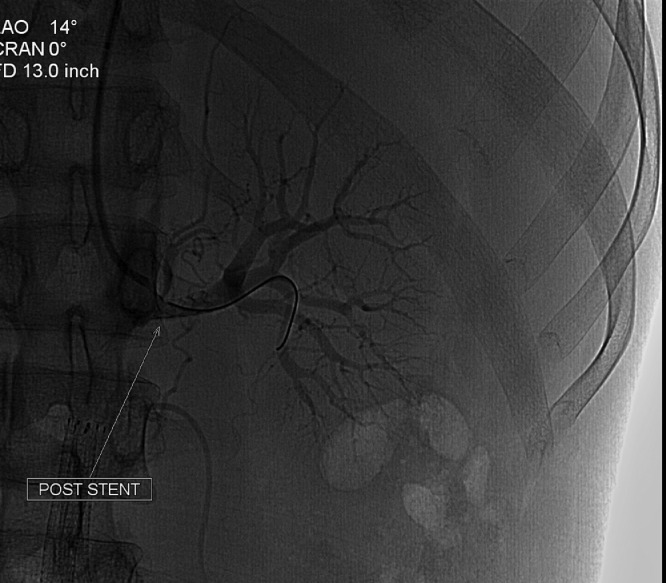
Fig 2.
Postangioplasty and stenting of the left renal artery showing marked improvement of the renal perfusion.
Discussion
Renal artery atherosclerotic stenosis has a wide spectrum of clinical manifestations based on the laterality of the affected vessel. Essentially, in cases with unilateral involvement, renovascular hypertension appears to be the main clinical presentation. However, bilateral renal artery stenosis could lead to progressive and/or acute ischemic kidney disease with flash pulmonary edema [8]. Within this context, Pickering syndrome is encountered when both renal arteries have occlusive inflow lesions. Accordingly, this syndrome is considered in patients who present with recurrent flash pulmonary edema, acute kidney injury, and hypertensive emergencies in the setting of a preserved left ventricle function [1,2].
With the advancements achieved in the catheter-based intervention field, percutaneous angioplasty and stenting techniques were used extensively to treat symptomatic renal artery stenosis with excellent primary patency rate. However, the use of these interventions has been tempered by the fact that most of the randomized trials of renal artery angioplasty/stenting have failed to demonstrate a long-term benefit (blood pressure control, preserve kidney function, and overall survival) over the optimal medical management alone [[7], [8], [9]]. Despite this conflicting data, accumulating evidence suggests that those interventions are justified in specific patient subgroups that have severe occlusive renal artery stenosis with significant clinical sequelae, including flash pulmonary edema, acute ischemic kidney injury, and uncontrolled hypertension. Therefore, we believe that careful patient selection is crucial in order to maximize the potential clinical benefit of catheter-based interventions [[7], [8], [9]].
In summary, the case presented underscores the fact that correcting the renal arterial inflow stenosis is beneficial and warranted in selective clinical scenarios. Additionally, it invites interventionalists and medical practitioners for careful examination of the available literature so that “the baby is not thrown out with the bath water” [7].
Patient consent
Written informed consent was obtained from the patient for all procedures and publication of this case and accompanying images.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Messerli FH, Bangalore S, Makani H, Rimoldi SF, Allemann Y, White CJ, et al. Flash pulmonary oedema and bilateral renal artery stenosis: the Pickering syndrome. Eur Heart J. 2011;32(18):2231–2235. doi: 10.1093/eurheartj/ehr056. [DOI] [PubMed] [Google Scholar]
- 2.Rimoldi SF, Yuzefpolskaya M, Allemann Y, Messerli F. Flash pulmonary edema. Prog Cardiovasc Dis. 2009;52(3):249–259. doi: 10.1016/j.pcad.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Planken II, Rietveld AP. Rapid onset pulmonary edema (flash edema) in renal artery stenosis. Neth J Med. 1998;52(3):116–119. doi: 10.1016/s0300-2977(97)00094-6. [DOI] [PubMed] [Google Scholar]
- 4.White CJ. Catheter-based therapy for atherosclerotic renal artery stenosis. Prog Cardiovasc Dis. 2007;50(2):136-50. [DOI] [PubMed]
- 5.Eirin A, Lerman LO. Darkness at the end of the tunnel: poststenotic kidney injury. Physiology (Bethesda) 2013;28(4):245–253. doi: 10.1152/physiol.00010.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prince M, Tafur JD, White CJ. When and how should we revascularize patients with atherosclerotic renal artery stenosis? JACC Cardiovasc Interv. 2019;12(6):505–517. doi: 10.1016/j.jcin.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 7.Mousa AY, Bates MC, Broce M, Bozzay J, Morcos R, AbuRahma AF. Issues related to renal artery angioplasty and stenting. Vascular. 2017;25(6):618–628. doi: 10.1177/1708538116677654. [DOI] [PubMed] [Google Scholar]
- 8.Lenz T. Treatment of renal artery stenosis in the year 2021. Internist (Berl) 2021;62(3):252–262. doi: 10.1007/s00108-020-00935-5. [DOI] [PubMed] [Google Scholar]
- 9.Manaktala R, Tafur-Soto JD, White CJ. Renal artery stenosis in the patient with hypertension: prevalence, impact and management. Integr Blood Press Control. 2020;13:71–82. doi: 10.2147/IBPC.S248579. [DOI] [PMC free article] [PubMed] [Google Scholar]