Abstract
Persistent hiccups (lasting more than 48 hours) can cause physical and emotional distress. They can result in dehydration, exhaustion, malnutrition, insomnia, wound dehiscence, ventilatory desynchronization, and hemodynamic changes. Hiccups are thought to be due to a complex reflex arc involving peripheral nerves and central structures such as the brainstem, temporal lobe, basal ganglia, hypothalamus, and spinal cord levels C3-5. Medullary strokes, for instance, have been reported to cause hiccups. We report a patient with a thalamic bleed who developed persistent hiccups. A 56-year-old man was brought to the hospital in an unresponsive state. He was intubated for airway protection. CT brain showed a left thalamic hemorrhage with edema and mass effect on the 3rd ventricle, intraventricular extension of hemorrhage, and hydrocephalus. An external ventricular drain was placed successfully with adequate drainage. One week after admission, the patient developed persistent abdominal jerks. These jerks were occurring every 3–4 seconds and would last for hours with brief periods of remission. He was started on levetiracetam 1000 mg IV bid and then increased to 1500 mg IV BID without any improvement of symptoms. The patient was also placed on EEG which did not reveal any epileptiform abnormality but did show an EMG artifact. His electrolytes including sodium, and potassium, and corrected calcium levels were normal. He did not have any evidence of pneumonia or other infections. It was determined that these jerks were likely hiccups. Metoclopramide 10 mg IV was tried without any benefit. He was then started on Baclofen 10 mg PO TID which resulted in a significant improvement in hiccups. Our case suggests that thalamic lesions might also lead to persistent hiccups.
Keywords: Stroke, Thalamus, Hiccups
Highlights
-
•
Persistent hiccups can be very distressing.
-
•
Central components of the reflex arc include the hypothalamus, medulla, and C3-5 spinal cord levels.
-
•
Our patient had persistent hiccups due to a thalamic bleed.
-
•
Thalamic lesions can also possibly lead to persistent hiccups.
1. Introduction
Hiccups are a common occurrence that most people experience in their lifetimes. The medical term is singultus and is derived from the Latin term “singult” which means ‘to catch one's breath while sobbing’ [1]. Hiccups result from a sudden and involuntary contraction of the diaphragm and intercostal muscles. This is followed by an abrupt closure of the glottis which produces the characteristic “hic” sound [2]. Acute hiccups, lasting less than 48 hours, are uncomfortable and can be an annoyance but are brief by nature. Persistent hiccups, lasting more than 48 hours, can significantly impact the quality of life by interfering with eating, sleeping, and speaking and can result in other medical complications [3]. The mechanism of hiccups is unclear. The reflex arc is thought to be comprised of the vagus, phrenic and sympathetic nerves peripherally while the central components include the hypothalamus, medulla, and C3-5 spinal cord levels [4]. Here we describe a patient with a thalamic bleed who developed persistent hiccups which suggests that the thalamus might also play a role in the hiccup reflex arc.
1.1. Case presentation
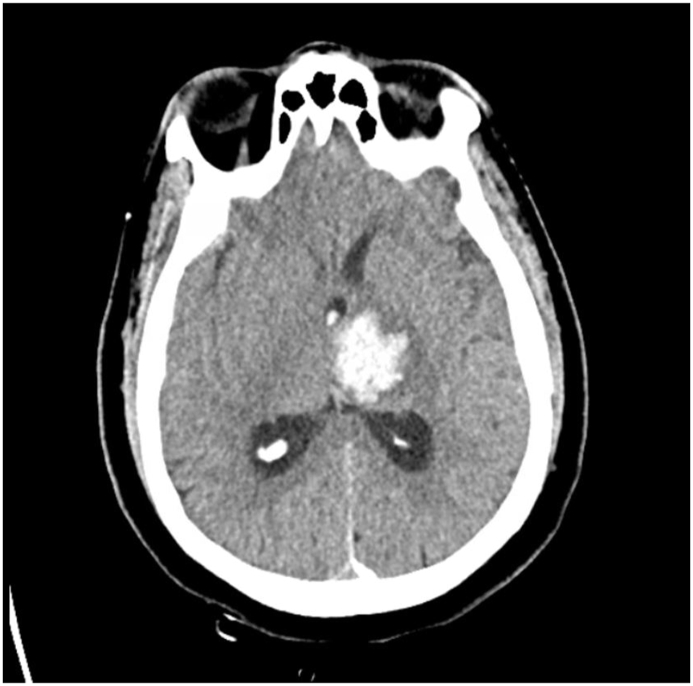
A 56-year-old man was brought to the hospital in an unresponsive state. His Glasgow Coma Scale on presentation was 6. He was afebrile with a pulse of 93/min and a BP of 182/108 mm Hg. On neurological examination, his pupils were reactive to light with positive corneal and gag reflex. He withdrew his left upper and lower extremity to pain but had a weak response on the right side. He was intubated for airway protection. Computed tomography (CT) brain showed a left thalamic hemorrhage (Fig. 1) with edema and mass effect on the 3rd ventricle, intraventricular extension of hemorrhage, and hydrocephalus. An external ventricular drain was placed successfully with adequate drainage. He was started on hypertonic saline with a serum sodium goal of 150–160 mmol/L. He was placed on video electroencephalography (vEEG) which did not reveal any epileptiform activity and was discontinued after two days. Magnetic resonance imaging (MRI) on day 2 showed improvement in hydrocephalus but there was a 1 cm midline shift of the septum pellucidum without any transtentorial herniation. He self-extubated himself on day 4 of his admission and underwent a tracheostomy due to a difficult re-intubation. On day 5, repeat CT brain showed improvement of midline shift to 3 mm. Therefore, the hypertonic saline was switched to normal saline. On day 7 of the admission, the patient developed persistent abdominal jerks. These jerks were occurring every 3–4 seconds and would last for hours with brief periods of remission. Repeat CT brain was unchanged. His sodium was 145 mmol/L, potassium was 4.3 mmol/L and calcium was 7.6 mg/dL. His albumin was 2.5 g/dL, therefore his corrected calcium level was 8.5 mg/dL. He did not have any evidence of pneumonia on a chest X-ray. CT of the abdomen did not reveal any acute process. He was started on levetiracetam 1000 mg IV bid for presumed myoclonus and it was then increased to 1500 mg IV BID without any improvement of symptoms. The patient was also placed on vEEG again which did not reveal any epileptiform abnormality but did show an electromyography (EMG) artifact (Video 1). It was determined that these jerks were likely hiccups. The levetiracetam was discontinued. Metoclopramide 10 mg IV was tried without any benefit. He was then started on baclofen 10 mg PO TID which resulted in a significant improvement in hiccups. Over the next week, the patient continued to gradually improve. He was then discharged home with outpatient rehabilitation. At the time of discharge, he did not have any focal weakness. His cranial nerve examination was normal. He had mildly diminished sensations to temperature and light touch in the right upper and lower extremities. His deep tendon reflexes were 2/4 in all extremities, and he did not exhibit any signs of cerebellar dysfunction.
Fig. 1.
Computed tomography of the brain showing a left thalamic hemorrhage.
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e16409
The following are the Supplementary data related to this article:
Video electroencephalography showing absence of epileptiform activity during the abdominal jerks and presence of EMG artifact.
2. Discussion
The hiccup reflex arc is comprised of an afferent limb, the central processing unit, and the efferent limb. The afferent limb is comprised of the phrenic nerve, vagus nerve, and sympathetic nerves which convey somatic and visceral sensory signals [2]. The central processing of hiccups is not well understood but has been thought to involve the medulla, reticular formation, chemoreceptors in the periaqueductal gray, the phrenic, glossopharyngeal, solitary and ambiguus nuclei, hypothalamus, temporal lobe and C3-5 spinal cord levels [4]. The central neurotransmitters involved include dopamine, gamma-aminobutyric acid (GABA), and serotonin which explains the efficacy of some medications that inhibit these neurotransmitters [5]. The efferent component of the arc is made up of motor fibers of the phrenic nerve supplying the diaphragm and the accessory nerves that supply the intercostal muscles. The thalamus has interconnections with the hypothalamus and the glossopharyngeal and solitary nuclei which might explain the causation of hiccups. Our workup did not reveal any thoracic, abdominal, or metabolic cause for the hiccups. His repeat CT brain scans showed a gradual improvement in the midline shift. There was no evidence of brainstem ischemia or hemorrhage on the CT scans. Therefore, we believe that his hiccups were likely due to the thalamic hemorrhage itself.
Acute hiccups typically last less than 8 hours. Persistent hiccups last more than 48 hours while intractable hiccups last more than a month. There are as many as 4000 admissions annually in the United States for hiccups [6]. Males and those with greater weight and height are more likely to experience persistent hiccups [7,8]. There have been many reported causes of hiccups and these are summarized in Table 1. Central nervous system (CNS) lesions such as stroke, posterior inferior cerebellar artery aneurysms, and tumors have been reported to cause hiccups [9]. Lateral medullary infarcts have often been reported as a central cause of hiccups [10,11]. Among the peripheral causes of hiccups, gastroesophageal reflux disease (GERD) has been well documented [12]. Those hiccups often respond to proton pump inhibitors. Helicobacter pylori infections can also lead to hiccups [13]. Surgeries in the thorax and abdomen can lead to hiccups due to post-instrumentation gastroparesis while anesthetic drugs like propofol can be causative too [14]. Hiccups in cancer patients can result from tumors such as esophageal tumors which might be impacting the reflex arc directly or as an effect of chemotherapy drugs such as Cisplatin [15].
Table 1.
Etiologies of hiccups.
| Lesion site/type | Disease/Disorder |
|---|---|
| Central Nervous System | |
| Vascular | Stroke, aneurysms |
| Tumor | Astrocytoma, cavernoma, brain stem tumors |
| Inflammation | Neuromyelitis optica, multiple sclerosis |
| Trauma | Brain injury |
| Miscellaneous | Parkinsonism, encephalitis, seizures |
| Peripheral pathway | |
| Thoracic | Mediastinal lesions, diaphragmatic tumors, |
| Heart | Ischemic heart disease, aneurysms |
| Gastrointestinal tract | Gastroesophageal reflux disease, esophageal tumors, Helicobacter pylori infection |
| Pulmonary | Pneumonia, bronchitis, tuberculosis |
| Miscellaneous | Ascites, pelvic tumors |
| Procedure | Thoracic and abdominal surgery, bronchoscopy, central venous catheterization, atrial pacing |
| Drug-induced | Anesthesia, anti-parkinsonian, opioids, benzodiazepines |
| Metabolic | Hyponatremia, hypocalcemia, hypokalemia |
| Psychogenic | Anxiety, excitation, hyperventilation, fear |
Acute hiccups are transient and do not require any further testing. However, persistent or intractable hiccups warrant further investigation. Evaluation should include a detailed history and documentation of all medications the patient might be already taking. A comprehensive exam including an evaluation of the thorax, abdomen, and nervous system should be performed. Routine blood workup should be done including complete blood count, electrolytes, blood urea nitrogen, creatinine, calcium, and liver function tests. A chest radiograph would help to identify pneumonia or adenopathy. A CT or MRI of the brain may demonstrate CNS lesions such as strokes, demyelination, vascular malformations, or tumors. A CT of the thorax or abdomen might also be indicated.
Acute hiccups generally resolve spontaneously. Physical maneuvers such as interrupting normal respiratory function (e.g., breath holding, Valsalva maneuver), stimulating the nasopharynx or uvula (e.g., sipping cold water, gargling with water, swallowing a teaspoon of dry sugar), increasing vagal stimulation (e.g., pressing on the eyeballs), and countering irritation of the diaphragm (e.g., pulling knees to chest, leaning forward to compress the chest) are some non-pharmacological treatments for hiccups [16]. Persistent hiccups might improve/resolve after the underlying etiology is treated. However, persistent hiccups often require pharmacological intervention. There are no formal treatment guidelines for hiccups. Combination therapy might be necessary in some cases [17].
Chlorpromazine is the only drug that has been approved by the U.S. Food and Drug Administration (FDA). However, it is no longer the clear first choice because of multiple potential adverse reactions including hypotension, urinary retention, delirium, and dystonic reactions [18]. Other antipsychotics such as haloperidol, risperidone, or olanzapine might be effective too but carry a risk of causing parkinsonism in addition to other side effects. Metoclopramide and domperidone are dopamine antagonists which are also effective. Metoclopramide has central anti-emetic properties as well as peripheral prokinetic effects. The recommended dose is 5–10 mg intravenously three to four times daily [19]. Domperidone is also dosed similarly but is devoid of neurological side effects because it does not cross the blood-brain barrier. Baclofen is a GABA-B receptor agonist, and it helps to reduce neuroexcitation and induce muscle relaxation. It is effective in persistent hiccups in stroke patients as well as idiopathic causes without gastroesophageal disease [20,21]. The recommended starting dose is 5–10 mg orally three times daily. Gabapentin has a relatively favorable side effect profile and decreases neuroexcitation by binding voltage-gated calcium channels and decreasing the release of excitatory neurotransmitters. The recommended dose is 300–400 mg three times daily and it is effective in cancer and brainstem stroke patients [22,23]. There have been anecdotal reports of the use of valproic acid, amantadine, carvedilol, nifedipine, and lidocaine. Refractory cases might benefit from more invasive therapies such as vagus nerve stimulation, stellate or phrenic nerve block, or acupuncture [[24], [25], [26]].
Acute hiccups can cause discomfort and emotional disturbances, but persistent hiccups can have more significant effects on quality of life. They can result in reduced intake, dehydration, malnutrition, weight loss, insomnia, wound dehiscence, and depression. It can persist during non-rapid eye movement (NREM) and REM sleep thus reducing sleep efficiency. Persistent hiccups in intubated patients can result in ventilatory desynchronization, respiratory alkalosis, and hemodynamic changes [27,28]. Forceful hiccups can also lead to bradycardia, carotid dissection, and barotrauma such as pneumothorax and pneumomediastinum.
3. Conclusion
Persistent hiccups can be very distressing and can also result in medical complications. Our case demonstrates that the thalamus might play a role in the hiccups reflex arc. Baclofen, metoclopramide, and gabapentin are effective in treating persistent hiccups.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Cole J.A., Plewa M.C. StatPearls; Treasure Island (FL): 2022. Singultus. [Google Scholar]
- 2.Becker D.E. Nausea, vomiting, and hiccups: a review of mechanisms and treatment. Anesth. Prog. 2010;57:150–156. doi: 10.2344/0003-3006-57.4.150. quiz 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samuels L. Hiccup; a ten year review of anatomy, etiology, and treatment. Can. Med. Assoc. J. 1952;67:315–322. [PMC free article] [PubMed] [Google Scholar]
- 4.Chang F.Y., Lu C.L. Hiccup: mystery, nature and treatment. J. Neurogastroenterol. Motil. 2012;18:123–130. doi: 10.5056/jnm.2012.18.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nausheen F., Mohsin H., Lakhan S.E. Neurotransmitters in hiccups. SpringerPlus. 2016;5:1357. doi: 10.1186/s40064-016-3034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobelle W.H. Use of breathing pacemakers to suppress intractable hiccups of up to thirteen years duration. Am. Soc. Artif. Intern. Organs J. 1999;45:524–525. doi: 10.1097/00002480-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Souadjian J.V., Cain J.C. Intractable hiccup. Etiologic factors in 220 cases. Postgrad. Med. 1968;43:72–77. doi: 10.1080/00325481.1968.11693139. [DOI] [PubMed] [Google Scholar]
- 8.Lee G.W., Kim R.B., Go S.I., Cho H.S., Lee S.J., Hui D., Bruera E., Kang J.H. Gender differences in hiccup patients: analysis of published case reports and case-control studies. J. Pain Symptom Manag. 2016;51:278–283. doi: 10.1016/j.jpainsymman.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Gambhir S., Singh A., Maindiratta B., Jaeger M., Darwish B., Sheridan M. Giant PICA aneurysm presenting as intractable hiccups. J. Clin. Neurosci. 2010;17:945–946. doi: 10.1016/j.jocn.2009.09.046. [DOI] [PubMed] [Google Scholar]
- 10.Sampath V., Gowda M.R., Vinay H.R., Preethi S. Persistent hiccups (singultus) as the presenting symptom of lateral medullary syndrome. Indian J. Psychol. Med. 2014;36:341–343. doi: 10.4103/0253-7176.135397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park M.H., Kim B.J., Koh S.B., Park M.K., Park K.W., Lee D.H. Lesional location of lateral medullary infarction presenting hiccups (singultus) J. Neurol. Neurosurg. Psychiatry. 2005;76:95–98. doi: 10.1136/jnnp.2004.039362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gluck M., Pope C.E., 2nd Chronic hiccups and gastroesophageal reflux disease: the acid perfusion test as a provocative maneuver. Ann. Intern. Med. 1986;105:219–220. doi: 10.7326/0003-4819-105-2-219. [DOI] [PubMed] [Google Scholar]
- 13.Orr C.F., Rowe D.B. Helicobacter pylori hiccup. Intern. Med. J. 2003;33:133–134. doi: 10.1046/j.1445-5994.2003.00351.x. [DOI] [PubMed] [Google Scholar]
- 14.Baraka A. Inhibition of hiccups by the laryngeal mask airway. Anaesthesia. 2004;59:926. doi: 10.1111/j.1365-2044.2004.03924.x. [DOI] [PubMed] [Google Scholar]
- 15.Takiguchi Y., Watanabe R., Nagao K., Kuriyama T. Hiccups as an adverse reaction to cancer chemotherapy. J. Natl. Cancer Inst. 2002;94:772. doi: 10.1093/jnci/94.10.772. [DOI] [PubMed] [Google Scholar]
- 16.Petroianu G.A. Treatment of hiccup by vagal maneuvers. J. Hist. Neurosci. 2015;24:123–136. doi: 10.1080/0964704X.2014.897133. [DOI] [PubMed] [Google Scholar]
- 17.Smith H.S., Busracamwongs A. Management of hiccups in the palliative care population. Am. J. Hosp. Palliat. Care. 2003;20:149–154. doi: 10.1177/104990910302000214. [DOI] [PubMed] [Google Scholar]
- 18.Friedgood C.E., Ripstein C.B. Chlorpromazine (thorazine) in the treatment of intractable hiccups. J. Am. Med. Assoc. 1955;157:309–310. doi: 10.1001/jama.1955.02950210005002. [DOI] [PubMed] [Google Scholar]
- 19.Wang T., Wang D. Metoclopramide for patients with intractable hiccups: a multicentre, randomised, controlled pilot study. Intern. Med. J. 2014;44:1205–1209. doi: 10.1111/imj.12542. [DOI] [PubMed] [Google Scholar]
- 20.Zhang C., Zhang R., Zhang S., Xu M., Zhang S. Baclofen for stroke patients with persistent hiccups: a randomized, double-blind, placebo-controlled trial. Trials. 2014;15:295. doi: 10.1186/1745-6215-15-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boz C., Velioglu S., Bulbul I., Ozmenoglu M. Baclofen is effective in intractable hiccups induced by brainstem lesions. Neurol. Sci. 2001;22:409. doi: 10.1007/s100720100075. [DOI] [PubMed] [Google Scholar]
- 22.Porzio G., Aielli F., Verna L., Aloisi P., Galletti B., Ficorella C. Gabapentin in the treatment of hiccups in patients with advanced cancer: a 5-year experience. Clin. Neuropharmacol. 2010;33:179–180. doi: 10.1097/WNF.0b013e3181de8943. [DOI] [PubMed] [Google Scholar]
- 23.Moretti R., Torre P., Antonello R.M., Ukmar M., Cazzato G., Bava A. Gabapentin as a drug therapy of intractable hiccup because of vascular lesion: a three-year follow up. Neurol. 2004;10:102–106. doi: 10.1097/01.nrl.0000117824.29975.e7. [DOI] [PubMed] [Google Scholar]
- 24.Grewal S.S., Adams A.C., Van Gompel J.J. Vagal nerve stimulation for intractable hiccups is not a panacea: a case report and review of the literature. Int. J. Neurosci. 2018;128:1114–1117. doi: 10.1080/00207454.2018.1486307. [DOI] [PubMed] [Google Scholar]
- 25.Lee A.R., Cho Y.W., Lee J.M., Shin Y.J., Han I.S., Lee H.K. Treatment of persistent postoperative hiccups with stellate ganglion block: three case reports. Medicine (Baltim.) 2018;97 doi: 10.1097/MD.0000000000013370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi T.Y., Lee M.S., Ernst E. Acupuncture for cancer patients suffering from hiccups: a systematic review and meta-analysis. Compl. Ther. Med. 2012;20:447–455. doi: 10.1016/j.ctim.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Rousseau P. Hiccups. South Med. J. 1995;88:175–181. doi: 10.1097/00007611-199502000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Byun S.H., Jeon Y.H. Treatment of idiopathic persistent hiccups with positive pressure ventilation -a case report. Korean J. Pain. 2012;25:105–107. doi: 10.3344/kjp.2012.25.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video electroencephalography showing absence of epileptiform activity during the abdominal jerks and presence of EMG artifact.
Data Availability Statement
Data included in article/supplementary material/referenced in article.