Abstract
Taurine has been proven in many trials to alleviate the symptoms of metabolic associated fatty liver disease. Here its protective effect for hepatic steatosis and modulation of AMP-activated protein kinase and insulin signaling pathway were investigated. Steatotic HepG2 cell established with oleic acid (0.05 mmol/L), treated with taurine (5 mmol/L), dorsomorphin (10 μmol/L) for 24 h. Sprague Dawley rats were divided into regular and high-fat diet (HFD) groups, and their corresponding taurine (70 or 350 mg/kg BW/d) groups, fed for 8 weeks. In steatotic cell, taurine reduced the TG concentration and SREBP-1c, PPARγ, FAS, ACC, SCD1 protein levels, decreased phosphorylation of mTOR, IRS1 (Ser302), increased phosphorylation of AMPKα, LKB1, PI3K, Akt, ACC. While dorsomorphin eliminated taurine's TG-lowering effect. In HFD-fed rats, taurine reduced liver TG, serum TG, ALT, AST, IL-1β, IL-4, TNF-α. The effects of taurine on the main factors of fatty acid synthesis were mostly consistent with cell experiments, and the reduction of microRNAs (451, 33, 291b) was aligned with the improvement in LKB1 and AMPK expression in HFD rats. Taurine alleviated steatosis-induced inhibition of IRS1-PI3K-Akt pathway, but suppressed its positively regulated downstream factor mTOR. In parallel, taurine reduced steatosis by activating LKB1-AMPKα pathway via phosphorylation and no-phosphorylation manner, then inhibiting SREBP-1c directly or by suppressing mTOR phosphorylation.
Keywords: Taurine, AMP-activated protein kinase (AMPK), Triacylglycerol, Hepatic steatosis
Graphical abstract
Taurine played the TG lowering effect by activating LKB1-AMPKα pathway via phosphorylation and no-phosphorylation manner (via inhibiting miR451, 33, 291b), subsequently inhibited mTOR, SREBP-1c, PPARγ and their downstream FA synthesis-related enzymes, or directly increased ACC phosphorylation to reduce ACC activity, alleviated the inhibition of IRS1-PI3K-Akt pathway caused by steatosis, and improve inflammatory and injury status by inhibiting pro-inflammatory factors (IL-4, IL-β, TNF-α).
Highlights
-
•
Taurine attenuated hepatic steatosis in oleic acid-treated HepG2 cells and high-fat diet-fed SD rats.
-
•
Taurine reduced TG levels by activating AMPK pathway was proved in cell and animal experiments, validated by AMPK inhibitor.
-
•
Taurine activated the AMPK pathway by promoting phosphorylation and inhibiting the associated microRNAs (miR-451,33,291b).
1. Introduction
Metabolic associated fatty liver disease (MAFLD), also named non-alcoholic fatty liver disease, is defined as a chronic liver disease with hepatic steatosis (triacylglycerol (TG) accumulation) in combination with one of the following 3 criteria: overweight/obesity, type 2 diabetes mellitus and metabolic dysfunction [1,2]. Its global prevalence is increasing yearly and has increased to 37.3% in 2019 [3]. If left untreated, hepatic steatosis can lead to end-stage liver disease (hepatocellular carcinoma) and cardiovascular co-morbidity [4,5], which can greatly deteriorate the quality of human life and put enormous pressure on society. However, there are no pharmaceuticals approved for the treatment of hepatic steatosis and MAFLD [6], so it is significant to explore effective treatment or active ingredients in the food that can interfere with fat synthesis.
Taurine (2-aminoethanesulfonic), a small sulfur-containing amino acid, is a food ingredient and rich in marine products, also widely exists in human tissues and organs, especially in the heart, retina, liver, brain, etc. [7,8]. A variety of biological functions are performed by taurine in the body, including anti-oxidation, anti-inflammatory, regulation of osmolality, calcium homeostasis regulation, central nervous system regulation, etc. [8]. The TG-lowering effect of taurine has been studied in different models, such as diet induced hyperlipidemia mice and hamster, high-fat alcohol liquid diet induced FLD rats and epidemiological surveys etc. [[9], [10], [11], [12], [13]]. One of the ways for taurine to reduce TG level and maintain the homeostasis of fat metabolism is to inhibit TG synthesis by repressing sterol regulatory element binding proteins-1c (SREBP-1c) and its downstream lipase [14,15]. SREBP-1c is the dominant subtype of the SREBP family in the liver and is involved in hepatic fatty acid (FA) synthesis by encoding the rate-limiting and key enzymes such as fatty acid synthase (FAS), acetyl-CoA carboxylase (ACC) and stearoyl-CoA desaturase1 (SCD1) [16].
SREBP-1c expression is mainly regulated by AMP-activated protein kinase (AMPK) and insulin signaling pathway [17,18]. AMPK, a promising therapeutic target for the treatment of MAFLD, can be activated when the Thr172 site of core subunit α is phosphorylated by the upstream kinases liver kinase B1 (LKB1) or calcium/calmodulin-dependent protein kinase kinase 2 (CaMKK2) [19]. Activated AMPK enhances deacetylase activity, thereby removing the acetyl groups on lysines 289 and 309 of SREBP-1c and directly inhibiting it [20]. The insulin signaling pathway initiates with tyrosine phosphorylation of insulin receptor substrate-1/2 (IRS-1/2), which further activates phosphatidylinositol 3-kinase (PI3K) and protein kinase B (Akt) via phosphorylation [21]. Mammalian target of rapamycin (mTOR), as a hub for regulating SREBP-1c, can increase the transcriptional level of SREBP-1c, while its phosphorylation level can be inhibited and promoted by AMPK and insulin signaling pathways, respectively [22,23]. MicroRNAs (miRNAs) control the expression of mRNA by binding to 3′-UTRs, and their effects on metabolism, especially on lipogenesis in MAFLD, have received much attention in recent years. Among them AMPK-SREBP-1c is the main pathway regulated by miRNAs [24,25].
The present research is to study the regulative effect of taurine on AMPK and IRS1/2-PI3K-AKT pathway by oleic acid-stimulated steatotic HepG2 cells and high fat/cholesterol diet-induced MAFLD rats.
2. Materials and methods
2.1. Experimental equipment
WD-9405B Shaking table, WD-9413 Gel imaging instrument (Beijing Liuyi Instrument Plant, China), Gel imaging system (Beijing Thmorgan, China), DG-3D Large horizontal electrophoresis tank, DG-III Bistable Digital Electrophoresis Apparatus (Beijing Donglinchangsheng, China), ZWY-211B Horizontal constant temperature culture oscillator (Shanghai Zhicheng, China), HWS24 Electric-heated thermostatic water bath (Shanghai Yiheng, China), Q-5000 UV–Visible Spectrophotometer (Unicosh, China), ME204E Electronic balance (Mettler Toledo, China), SG-603A Biological safety cabin (Baker, USA), N-EVAP112 Nitrogen blowing instrument (Organomation, USA), Vibra-Cell Ultrasonic disruptor (SONICS, USA), Mini-PROTEAN Tetra Electrophoresis System, Mini Trans-Blot (Bio-Rad, USA), ABI PRISM 7500 Fluorescence quota PCR meter, 9600 PCR instrument (ABI, USA), MCO-15AC CO2 incubator (Sanyo, Japan), IX71 Inverted trinocular microscope (Olympus, Japan).
2.2. Reagents, antibodies and preparation of main solutions
Taurine was purchased from Sigma-Aldrich Co. (MO, USA) for cell experiments and YONGAN Pharmaceutical (Hubei, China) for animal experiments. Oleic acid, Triton X-100 were purchased from Sigma-Aldrich Co. (MO, USA). Dulbecco's modified eagle medium (DMEM), 100 units/mL anti-biotic mixture of penicillin, streptomycin and gentamicin, 2.5% trypsin, bovine serum albumin (BSA) were purchased from Gen-view Scientific Inc. (DE, USA). Fetal bovine serum (FBS) and dimethyl sulfoxide were purchased from Absin Inc. (Shanghai, China). Dorsomorphin was purchased from Cell Signaling Technology (CST) (MA, USA). The antibodies used in the Western blot are listed in Table 1. Radio immunoprecipitation assay (RIPA) lysis buffer, 100 × phenylmethanesulfonyl fluoride (PMSF), 50 × Phosphatase inhibitor, 5 × Sodium dodecyl sulfate (SDS) protein loading buffer, skimmed milk powder and all other reagents were purchased from Dingguochangsheng Biotechnology Inc. (Beijing, China).
Table 1.
Antibodies and their manufacturers.
| Antibody | Manufacturer |
|---|---|
| Primary antibodies against AMPKα (CAT#5831), Phospho-AMPKα (Thr172) (CAT#2535), LKB1 (CAT#3047), Phospho-LKB1 (Ser428) (CAT#3482), CaMKK2 (CAT#16810), mTOR (CAT#2983), Phospho- mTOR (Ser2448) (CAT#5536), IRS1 (CAT#2390), Phospho-IRS1 (Ser302) (CAT#2384), Phospho-IRS1 (Ser307) (CAT#2381), PI3K (CAT#4249), Akt (CAT#4685), Phospho-Akt (Thr308) (CAT#13038), Phospho-Akt (Ser473) (CAT#4060), PPARγ (CAT#2435), FAS (CAT#3180), ACC (CAT#3676), Phospho-ACC (Ser79) (CAT#11818), GAPDH (CAT#2118); Secondary antibody: anti-rabbit IgG, HRP-linked antibody (CAT#7074) | CST, USA |
| Primary antibody against SREBP-1c (CAT#AF4728) | Affinity, USA |
| Primary antibodies against Phospho-PI3K (p85) (Tyr607) (CAT# ab182651), SCD1 (CAT#ab236868) | Abcam, UK |
Preparation of the solutions required in further experiments: 1. Cell lipid extracting solution: A mixture of 50 mL n-hexane and 25 mL isopropanol. 2. Liver lipid extracting solution: A mixture of 50 mL chloroform and 25 mL methanol. 3. Lipid lysis solution (Isopropanol containing 10% Triton-X100): A mixture of 18 mL isopropanol and 2 mL Triton-X100. 4. Protein extraction lysate for Western Blot: The protein extraction lysate was obtained by mixing 100× PMSF and 50× phosphorylation protease inhibitor with RIPA lysis buffer.
2.3. Cell culture and treatment
The human HepG2 hepatocytes were cultured in DMEM medium supplemented with 10% FBS and an anti-biotic mixture at 37 °C in a humidified atmosphere of 5% CO2, which were obtained from the Cell Culture Center of the Institute of Basic Medicine of Peking Union Medical University (Beijing, China). The cells were treated as indicated [26,27]. HepG2 cells were incubated with 0.05mmol/L oleic acid (OA) for 24 h in the model group (M group) to establish the steatotic cell model, corresponding to the control group (C group) without treatment. For the exploration of the effect of taurine, the CT and MT groups were treated with 5 mmol/L taurine at the basis of C and M groups. The role of AMPK on TG levels was verified in MD and MTD groups by treatment with Dorsomorphin (10 μmol/L) for 24 h.
2.4. Animal feeding and experimental design
SPF Male Sprague Dawley (SD) rats (120 ± 5 g) were purchased from HFK bioscience Co., Ltd (Beijing, China) on arrival, production license number SCXK (2014-0004), housed separately in a controlled environment (22 ± 2°C with a humidity of 55 ± 5%) under a 12 h light-dark cycle with free access to food and water. After 1 week of acclimatization, the rats were randomly divided into six groups (9 rats in each group), as follows: control group (C) and corresponding low/high dose taurine group (CT1, CT2), model group (M) and corresponding low/high dose taurine group (MT1, MT2). The C/ CT1/ CT2 and M/ MT1/ MT2 groups were respectively given a regular diet and a high-fat diet (HFK Bioscience Co., Ltd., China), the taurine groups were given taurine every day by intragastrical administration with the low and high dose of 70 mg/kg BW and 350 mg/kg BW respectively. Bodyweight and food intake were measured twice a week. After eight weeks, all rats fasted from 9 p.m. for 12 h and anesthetized. Blood was collected from the femoral artery. The left lobe of liver was fixed with 10% formalin solution and the right lobe was collected and snap frozen in liquid nitrogen for subsequent analyses. The research protocol was approved by Experimental Animal Ethics Committee of Functional Test Center for Health Food of Beijing Union University.
2.5. Serum biochemical assays
After blood was set at room temperature for 30 min, serum was separated by centrifuging at 3500 rpm for 20 min at 4 °C. Serum TG and TC contents were measured by triacylglycerol assay kit, total cholesterol assay kit (NANJINGJIANCHENG Bio, China), transaminase levels were detected using alanine aminotransferase assay kit and aspartate aminotransferase assay kit (NANJINGJIANCHENG Bio, China), and inflammatory factors levels were measured using Rat IL-1β ELISA kit (CUSABIO, China), Rat IL-4 ELISA kit and Rat TNF-α ELISA kit (ExCELL Bio, China).
2.6. Extraction and quantification of TG and TC in hepatic cell and tissue
Lipids in cells were extracted using 1.5 mL/well cell lipid extracting solution on the ice for 1 h. The solution was dried using nitrogen and then dissolved in 80 μL of lipid lysis solution for TG quantification by triacylglycerol assay kit (NANJINGJIANCHENG Bio, China). Subsequently, the cellular protein was extracted with 0.2 mL/well of RIPA lysis buffer on ice for 20 min and measured by BCA protein assay kit (Dingguochangsheng, China). Liver tissue was homogenized with liver lipid extraction (mass (g): volume (mL) = 1:9) and the supernatant was obtained by centrifugation at 3000 rpm for 10 min at 4 °C. The supernatant was dried by nitrogen and then residue was dissolved in 3 mL lipid lysis solution for lipid quantification with triacylglycerol assay kit and total cholesterol assay kit (NANJINGJIANCHENG Bio, China). The result is expressed as micromoles of lipid in per gram of cellular protein or per gram of liver weight.
2.7. Histopathological assessment
Part of liver tissues from the left liver lobe were embedded in paraffin wax and cut into 5 μm slices and stained with hematoxylin and eosin (H&E). Another part was frozen at −80 °C, cut into 10 μm slices and stained with oil red O according to standard procedures.
2.8. Measurement of miRNA levels in the liver
Total RNA was isolated from the liver by using the Trizol® reagent kit (Invitrogen, Carlsbad, CA) according to the manufacturer's instructions. Using total RNA as a template, cDNA was synthesized by reverse transcription kit (Invitrogen, Carlsbad, CA). qPCR was performed using Fast SYBR® Green Master Mix Bulk Pack (Invitrogen, Carlsbad, CA) on ABI Prism® 7500 Sequence Detection System to quantify the level of miRNA with the 2-ΔΔCT method. All miRNAs were normalized by using rat U6 as internal standard. Primer sequences are shown in Table 2.
Table 2.
Primers for PCR.
| gene | Primers | Sequence (5′ to 3′) | Length of PCR products |
|---|---|---|---|
| U6 rat | F | CCTGCTTCGGCAGCACAT | 102bp |
| R | AAATATGGAACGCTTCACG | ||
| miR-451 | F | GCGAAACCGTTACCATTACT | 65bp |
| R | GTCGTATCCAGTGCGTGTCGTGGAGTCGGCAATTGCACTGGATACGACAACTCAG | ||
| miR-33 | F | GCGTGCATTGTAGTTGCA | 63bp |
| R | GTCGTATCCAGTGCGTGTCGTGGAGTCGGCAATTGCACTGGATACGACTGCAATG | ||
| miR291b | F | GGCGAAAGTGCATCCATTTTG | 66bp |
| R | GTCGTATCCAGTGCGTGTCGTGGAGTCGGCAATTGCACTGGATACGACACTAACA |
2.9. Western blot assay
HepG2 cells and liver tissues were lysed by using protein extraction lysate, then crushed by ultrasonic crusher and homogenized by tissue grinder, respectively. After centrifugation, the supernatant was collected and the protein concentrations were determined using BCA protein assay kit (Dingguochangsheng, China), which were subsequently adjusted to 4 μg/μL and the protein samples were denatured by boiling with the addition of 5 × SDS protein loading buffer. Equal amounts of protein were separated using sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE). The proteins were transferred to the 0.45 μm polyvinylidene difluoride (PVDF) membranes (Cytiva, USA) by the wet transmembrane method. The target proteins were cut and blocked with 5% skimmed milk powder or 5% BSA for 1 h at 25 °C, and incubated with the primary antibody overnight at 4 °C and then with the secondary antibody at 25 °C for 2 h. Finally, the target protein bands were exposed, photographed and analyzed in greyscale using the efficient chemiluminescence kit (Genview, USA). All proteins were normalized by glyceraldehyde-3-phosphate dehydrogenase (GAPDH).
2.10. Statistical analyses
All data are resented as mean ± Standard Deviation (mean ± SD). The results were plotted using GraphPad Prism 8 (Graphpad Software, La Jolla, CA, USA) and analyzed with the Student's t-test. The differences were considered to be statistically significant at p < 0.05.
3. Results
3.1. Effect of taurine on TG levels, SREBP-1c, PPARγ and their downstream FA synthesis-related enzymes protein levels in HepG2 cells
In cell experiments, 0.05 mmol/L oleic acid treatment was used to establish the steatotic cell model, after 24 h a significant more than two-fold increment in TG levels could be observed from Fig. 1a in M group compared to C group. It also shows that there was no difference in TG levels between CT and C groups, and cellular TG levels in the MT group were significantly lower than those in the M group. These results indicate that taurine can reduce TG levels in the steatotic cell model while not affecting cellular TG in the normal state.
Fig. 1.
Effect of taurine on the TG level and FA synthesis-related enzymes and factors protein level in HepG2 cells. (a) TG levels; (b, d) protein band diagram; (c, e) Relative protein level. C: control group; CT: control supplemented with taurine; M: steatotic cell model; MT: steatotic model supplemented with taurine. *p < 0.05 vs. C group; #p < 0.05 vs. M group.
As shown in Fig. 1b-e, protein level of SREBP-1c, PPARγ and their downstream FA synthesis-related enzymes (FAS, SCD1) were all significantly increased in M group, but not altered by 5 mmol/L taurine supplementation in CT group. Compared to M group, taurine decreased the level of SREBP-1c, PPARγ, FAS, SCD1 and ACC, suggesting that taurine may inhibit FA synthesis by regulating SREBP-1c and PPARγ in steatotic cells. Notably, in CT and MT groups taurine not only decreased the ACC level but also increase p-ACC-Ser79 level compared to C and M groups respectively.
3.2. Effect of taurine on AMPK pathway and insulin signaling pathway in HepG2 cells
AMPK pathway and insulin signaling pathway, the main upstream of SREBP-1c and PPARγ, were been detected through protein level in the present study. As shown in Fig. 2a and b, oleic acid did not change the level of AMPKα pathway factors, compared to M group taurine increased the p-AMPKα-Thr172 and p-LKB1-Ser428 level in MT group, indicating that taurine can activate AMPK by increasing the phosphorylation level of LKB1 in the steatotic cell model.
Fig. 2.
Effect of taurine on the protein level of the AMPK pathway, insulin signaling pathway and mTOR in HepG2 cells. (a) Protein band diagram; (b,c,d) Relative protein level; (e) TG levels. C: control; CT: control supplemented with taurine; M: steatotic cell model; MT: steatotic model supplemented with taurine. *p < 0.05 vs. C group; #p < 0.05 vs. M group.
In terms of insulin signaling pathway, there was no significant difference between 4 groups in the protein level of IRS-1, PI3K and Akt. Compared to C group, oleic acid increased p-IRS1-Ser307 and decreased p-PI3K-Tyr607, p-Akt-Ser473 and p-Akt-Thr308 levels in M group, while in MT group taurine reversed the oleic acid-induced changes of phosphorylation of the above factors (Fig. 2a, c). The results suggest that oleic acid promoted IRS1 serine phosphorylation and thus inhibited its tyrosine phosphorylation then interfered with the insulin signaling pathway, whereas taurine countered the oleic acid-induced increase in phosphorylation of the serine site of IRS1, thereby reducing the disruption of the PI3K-Akt signaling pathway.
mTOR is the pivotal protein in the role of AMPK pathway and insulin signaling pathway to regulate level of SREBP-1c and PPARγ. As shown in Fig. 2a, d, the level of p-mTOR-Ser2448 increased in M group compared to C group, and decreased in MT group compared to M group. Taurine reduced the increase of mTOR phosphorylation induced by oleic acid and this alteration was in line with the regulation of its inhibition by the AMPK pathway.
In order to further confirm that AMPK pathway is the key for taurine to reduce TG, we treated steatotic cell with 10 μmol/L dorsomorphin, which is an inhibitor of AMPK, the TG level in MD group was further increased compared to M group, but taurine did not change the TG level between MD and MDT groups (Fig. 2e). Dorsomorphin eliminated the effect of taurine in reducing TG levels in steatotic cells. These results confirm that taurine inhibits mTOR by activating AMPK pathway, thereby interfering with FA synthesis.
3.3. Effect of taurine on body weight, organ weight, serum and liver lipid levels, serum transaminase and inflammatory factors in rats
To further investigate the effect of taurine on FA synthesis, animal experiments with SD rats were conducted. After 8 weeks feed, there were no significant differences in food intake, cardiac or kidney weight among C, CT1 and CT2 group, as well among M, MT1 and MT2 group. Fig. 3a and b shows that high-fat diet increased the body weight and epididymal fat weight of rats, whereas high dose of taurine alleviated this increasement.
Fig. 3.
Effect of taurine on body weight, organ weight, serum lipid, transaminase and inflammatory factors level, liver lipid level and tissue slices of rats. (a) Body weight; (b) Organ weight; (c) Serum lipid; (d) Liver lipid; (e) HE staining of hepatic tissue (arrow: lipid droplets); (f) Oil red O staining (arrow) of hepatic tissue; (g) Serum transaminase; (h) Serum inflammatory factors. C: control group; CT1: control supplemented with low dose of taurine; CT2: control supplemented with high dose of taurine; M: high-fat diet group; MT1: high-fat diet group supplemented with low dose of taurine; MT2: high-fat diet supplemented with high dose of taurine. *p < 0.05 vs. C group; #p < 0.05 vs. M group. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
In terms of TG level, serum TG level was significantly lower in CT2 group with a high dose of taurine and liver TG level was significantly higher in M group fed a high-fat diet compared to the regular diet group; compared to M group, liver TG level of MT2 group with a high dose of taurine and serum TG level of MT1 and MT2 groups with both doses of taurine were significantly decreased. TC level in serum and liver was significantly higher in M group compared with C group; serum and liver TC levels were significantly lower in MT2 group than in M group (Fig. 3c and d). These data suggest that taurine ameliorated the increase in serum and liver lipids induced by a high-fat diet in rats.
The effect of taurine on tissue morphology and fat deposition was represented in liver tissue sections. HE staining (Fig. 3e) showed that in the visual field cells were arranged orderly with no abnormalities and no obvious fat vacuoles in groups C, CT1 and CT2. In M group the normal hepatocytes were less and cell volume was larger, the nucleus was narrowed and irregular, and large fat vacuoles were observed. Compared with M group, the morphology and boundary of hepatocytes in MT1 and MT2 groups became clearer, the nucleus became larger and round, and the fat vacuoles were decreased significantly. The results of the Oil red O staining showed that the accumulation of lipid droplets decreased in CT1 and CT2 groups, and increased in M group compared to C group (Fig. 3f). Compared with M group, lipid droplets accumulation was alleviated in MT1 and MT2 groups. It can be suggested that taurine protected against hepatocyte morphology and attenuated hepatic lipid accumulation in rats fed with high-fat diet.
As shown in Fig. 3g and h, compared with C group, the serum IL-1β level decreased in group CT1, CT2, and serum ALT, AST, IL-1β, IL-4, TNF-α levels increased significantly in M group; compared with M group, serum ALT, AST, IL-1β, IL-4, TNF-α levels decreased in MT2 group. The data were consistent with the HE staining results. Taurine reduced the serum transaminase levels, inhibited the elevation of pro-inflammatory factors induced by high-fat diet, and improved liver damage and inflammation levels in rats.
3.4. Effect of taurine on the protein level of FA synthesis-related factors in rat liver
In Fig. 4, the protein level of PPARγ in rat liver was not significantly different between the 6 groups, the SREBP-1c, FAS, SCD1, ACC levels were significantly increased in M group compared to C group, and decreased in MT2 group with high-dose of taurine supplementation compared to M group. Notably, the level of p-ACC-Ser79 and the ratio of p-ACC to ACC in M group decreased compared to C group, and p-ACC/ACC was significantly higher in MT2 group than in M group. This suggests that in rat liver, taurine reduces fatty acid and TG levels, both by inhibiting the level of SREBP-1c and FA synthesis-related enzymes (FAS, SCD1, ACC) and also by increasing phosphorylation of ACC to inhibit its activity.
Fig. 4.
Effect of taurine on the protein level of FA synthesis-related enzymes and factors in rat liver: (a, c) Protein band diagram. (b, d) Relative protein level. C: control group; CT1: control supplemented with low dose of taurine; CT2: control supplemented with high dose of taurine; M: high-fat diet group; MT1: high-fat diet group supplemented with low dose of taurine; MT2: high-fat diet supplemented with high dose of taurine. *p < 0.05 vs. C group; #p < 0.05 vs. M group.
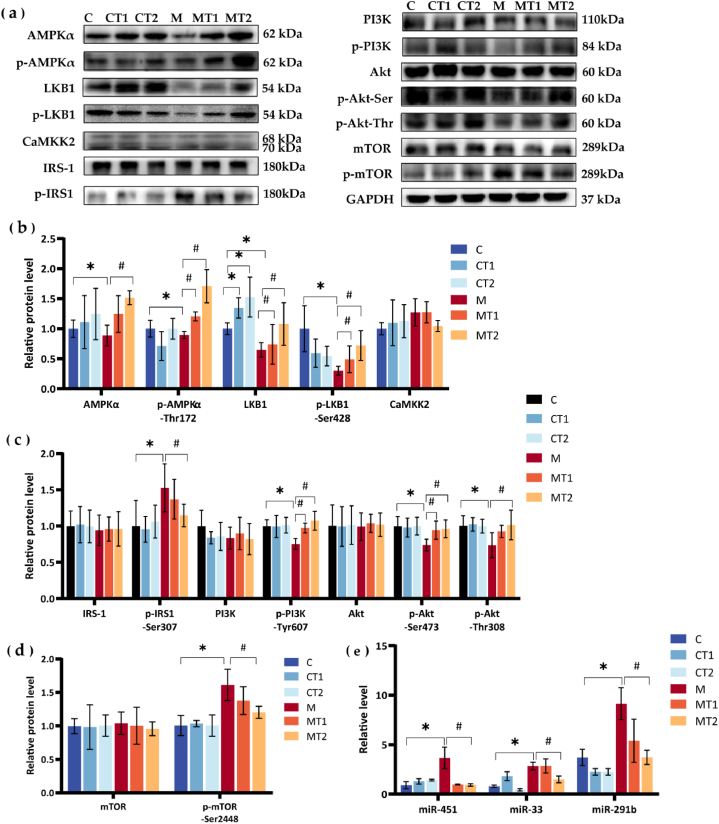
3.5. Effect of taurine on the AMPK and insulin signaling pathway in rat liver
We next examined the protein level of AMPK pathway and insulin signaling pathway-related factors in rat liver, which were shown to correlate with reduced FA synthesis by taurine in cell experiments.
Regarding the AMPK pathway, Fig. 5a and b shows that there was no significant difference in CaMKK2 level among 6 groups. Compared with C group, LKB1 expression was significantly increased in CT1, CT2 groups, AMPKα, p-AMPKα-Thr172, LKB1 and p-LKB1-Ser428 levels were significantly decreased in M group; compared with M group, the level of p-AMPKα-Thr172, LKB1 and p-LKB1-Ser428 were significantly increased both of MT1 and MT2 groups, the protein level of AMPKα was also significantly increased in MT2 group.
Fig. 5.
Effect of taurine on the protein level of the AMPK pathway, insulin signaling pathway, mTOR and the miRNAs expression level related to FA synthesis in rats liver. (a) Protein band diagram; (b, c, d) Relative protein levels; (e) Relative level of miRNA. C: control group; CT1: control supplemented with low dose of taurine; CT2: control supplemented with high dose of taurine; M: high-fat diet group; MT1: high-fat diet group supplemented with low dose of taurine; MT2: high-fat diet supplemented with high dose of taurine. *p < 0.05 vs. C group; #p < 0.05 vs. M group.
In relation to insulin signaling pathway, it can be observed from Fig. 5a, c that the level of IRS-1, PI3K and Akt did not differ in the liver of the six groups. Compared with C group, the p-IRS1-Ser302 level was significantly increased and the level of p-PI3K-Tyr607, p-Akt-Ser473 and p-Akt-Thr308 were significantly decreased in M group; compared with M group, in MT2 group p-IRS1-Ser302 level was decreased and p-Akt-Thr308 level was significantly increased, besides the level of p-PI3K-Tyr607 and p-Akt-Ser473 were increased both in MT1 and MT2 groups. The results showed that taurine improved the increase in serine phosphorylation level of IRS1 in the liver of high-fat diet rats and the decrease in the phosphorylation levels of PI3K and Akt.
In Fig. 5d, high-fat diet and taurine did not affect the level of mTOR. p-mTOR-Ser2448 level in M group significantly increased compared with C group, and high dose of taurine decreased it, which was consist with the results in HepG2 cells. The level of mTOR was in line with AMPK pathway rather than insulin signaling pathway.
In summary, it can be concluded that taurine improves the interference of high-fat diet on IRS1/PI3K/Akt signaling pathway, and also increases the phosphorylation level of LKB1 and AMPKα to decrease the phosphorylation level of mTOR and thereby decreasing the level of SREBP-1c and its downstream lipid synthesis-related enzymes.
3.6. Effect of taurine on miRNAs which regulate AMPK protein level
To investigate whether taurine regulates the AMPK pathway to reduce the synthesis of TG in a manner other than phosphorylation modifications, we measured the expression levels of microRNAs 33 and 291b, which regulate AMPK [28,29], and microRNA 451, which regulates the upstream kinase LKB1 [30], in rat liver. As shown in Fig. 5e, the levels of miR-451, miR-33 and miR-291b were significantly higher in M group fed a high-fat diet than in C group, whereas they were significantly lower in MT2 group after supplementation with high doses of taurine compared with M group. The results showed that taurine inhibited the expression of miR-291b, miR-33 and miR-451 in the liver of rats induced by high fat diet.
4. Discussion
MAFLD is a disease continuum normally associated with obesity, that begins with an anomalous accumulation of TG in the liver, parallels cellular injury as well as exacerbating inflammation, fibrosis and carcinogenesis [31,32]. Here, high dose of taurine (350 mg/kg bw/d) reduced the weight gain and epididymal fat induced by a high-fat diet in rats (Fig. 3a and b), exerted a suppressive effect in the early stages of obesity, while the low dose was ineffective. Several lines of evidence indicate that taurine has the TG-lowering effect in rats, mice, hamsters, and HepG2 cells MAFLD models [[9], [10], [11],26], and 0.5%–5% taurine in diet or drinking water can show the effect to decrease the hepatic TG level. In the currently reported experiments, taurine is added to drinking water or feed and fed to animals, but animals can take feed and water ad libitum. Therefore, the intake of taurine is not accurate and individual differences are large. In this animal experiments, the intragastrical administration method was chosen and precise dose of taurine was supplemented to rat, high dose of taurine reduced the serum TG and TC levels in rats on a high-fat diet but also decreased serum TG levels on regular diet fed rats (Fig. 3c). In steatotic HepG2 cells, 5 mM taurine significantly reduced TG levels, but had not impact on normal state (Fig. 1a). Although no upper limit has been set for the safe dose of taurine in many countries, but current studies shows that the dose of taurine used as a single ingredient is 1–6 g [33], so 350 mg/kg bw/d taurine may be somewhat high for rats in normal state. As for hepatic lipid level, taurine had no effect on regular diet rats, both doses of taurine significantly inhibited the elevated liver TG levels induced by high-fat diet, and high doses of taurine also reduced liver TC levels (Fig. 3d). The results of HE staining and oil red O staining of liver sections were consistent with the above, taurine clarified hepatocyte borders, reduced fat vacuoles and droplets (Fig. 3e and f).
When hepatocytes are damaged, serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) activity increases and then diffuse from cytoplasm and mitochondria of hepatocytes into the blood [34]. Serum ALS and ALT are usually used to access and monitor patients with liver diseases in clinic. Abd Elwahab AH et al. [35] found that 500 mg/kg BW/day of taurine oral solution for 12 weeks significantly reduced ALT and AST levels in rats with diet-induced steatohepatitis, however, in our experiments, 350 mg/kg BW/d taurine orally for 8 weeks also reduced the elevated rat serum ALT and AST induced by a high-fat diet (Fig. 3g). Studies shown that the release of proinflammatory cytokines such as TNFα, IL-4, and IL-1β will be stimulated in steatosis [36]. We found that taurine reversed the elevated levels of serum IL-4, IL-1β and TNF-α in high-fat diet fed rats (Fig. 3h), suggesting the certain anti-inflammatory effect of taurine in MAFLD.
De novo lipogenesis is a dominant abnormality in steatosis [37], in this process, acetyl-CoA synthetase 1 catalyzes the conversion of acetic acid and coenzyme A to acetyl-CoA, and then carboxylated to methylmalonyl- CoA by ACC [38]. Subsequently under the catalysis of FAS, acetyl-CoA and methylmalonyl- CoA undergo a 4-step cycle reaction. Both ACC and FAS play the role of rate limit in de novo lipogenesis [39,40]. SCD1 restricts the synthesis of monounsaturated fatty acid through catalyzing the formation of N-9 series monounsaturated fatty acids from the 9th carbon chain of saturated fatty acids [41]. SREBP-1c is one of the major transcriptional factors for de novo lipogenesis, translocates its N terminus to the nucleus and upregulates all genes in the fatty acid biosynthetic pathway, including FAS, ACC and SCD1 [42]. PPARγ appears to regulate the expressions of genes involved in lipogenesis, and the knockdown of PPARγ gene in high-fat diet-induced fatty liver mice resulted in decreased expression of lipid synthesis-related factors (such as SREBP-1c, SCD1, ACC) and improved hepatic steatosis [43]. In the present study, it was concluded for the first time that taurine inhibited the protein level of PPARγ in steatotic HepG2 cells (Fig. 1b and c). Both 5 mM taurine in oleic acid-induced steatotic HepG2 cells and 350mg/kg bw/d of taurine in the liver of SD rats fed with high-fat diet reduced the protein level of SREBP-1c, FAS, ACC and SCD1 (Fig. 1b-e, 4a-d), which is basically consistent with the studies of Tang et al. [14] in the model of alcoholic liver disease and Miyata et al. [15] in the genetic model of fatty liver disease. The above suggests that taurine inhibits the SREBP-1c, PPARγ and their downstream enzymes to reduce the accumulation of TG. In addition, our experiment observed that taurine also increased the phosphorylation of ACC both in steatotic cell and high-fat diet-fed rat liver (Fig. 1d-e, 4c-d). ACC activity is reversibly regulated by phosphorylation and AMPK can phosphorylate the Ser79 site of ACC and inactivate it [44], and providing further negative feedback on TG accumulation.
AMPK pathway is involved in the regulation of SREBP-1c and PPARγ, and mTOR plays a pivotal role in this process. mTOR, a point of divergence of glucose and lipid metabolism in the liver, is positively regulated by the insulin signaling pathway and also depressed by the AMPK pathway [45]. In this study, taurine inhibited the increase of mTOR phosphorylation induced by oleic acid and high-fat diet (Fig. 2, Fig. 5d), which echoed its regulation of AMPK pathway.
AMPK is known as an energy receptor and plays an important role in energy homeostasis [46]. In eukaryotes, such as mammals, AMPK acts as a key master switch and phosphorylation on a conserved key threonine-172 residue in the N-terminal region of its alpha subunit is the predominant way in which it is stimulated [47]. Two pieces of evidence in this study suggest that the TG-lowering effect of taurine may be related to the AMPK pathway, one is that taurine elevated the phosphorylation level of the Ser37 site of ACC as mentioned above, and the second is that taurine decreased the phosphorylation level of mTOR in both steatotic HepG2 cells and high-fat dietary rat livers. Morsy et al. [48] showed that 500 mg/kg bw/d of taurine reversed the reduction in hepatic AMPKα phosphorylation induced by a high-fat diet in rats. In the present study, taurine was consistently shown to increase AMPK phosphorylation levels both in cell and animal experiments. Taurine elevates phosphorylation of the Thr172 site of AMPK in steatotic HepG2 cells (Fig. 2a and b). Both doses (70/350 mg/kg bw/d) of taurine significantly increased p-AMPKα-Thr172 levels in rats on a high-fat diet in a dose-dependent manner, and even high doses of taurine significantly increased AMPKα protein level (Fig. 5a and b).
AMPK is regulated by upstream kinases (LKB1, CaMKK2). CaMKK2 is activated when intracellular Ca2+ levels increase and LKB1 is phosphorylated when intracellular AMP levels increase, both of which subsequently activate AMPKα by phosphorylating the Thr172 site [49,50]. Taurine at a certain concentration can stimulate the cells and rapidly increase the intracellular Ca2+ concentration [51], suggesting that taurine may activate AMPK through CaMKK2. In this paper, however, taurine did not affect CaMKK2 expression either in rat liver or HepG2 cells (Fig. 2, Fig. 5b). LKB1 is the most important kinase upstream of AMPKα, but there are few studies on the regulatory effects of taurine on AMPK and LKB1. Consistent results were obtained in our studies both with steatotic cell and high-fat diet-fed rat livers. Taurine significantly increased the levels of p-LKB1-Ser428 and taurine even increased the expression of LKB1 protein in the livers of high-fat diet-fed rats (Fig. 2, Fig. 5b). All of the above results reflect the important role of the AMPK pathway in the TG-lowering effect of taurine, and dorsomorphin treatment further clarified it. Dorsomorphin is a reversible, ATP-competitive AMPK inhibitor [52]. And in this study, dorsomorphin eliminated the TG-lowering effect of taurine in steatotic cells (Fig. 2e), which confirmed that taurine does lower TG levels via the AMPK pathway.
Insulin resistance is the common underlying pathophysiology of metabolic dysfunction in MAFLD [45]. High fat or fructose diet, the common metabolic stress, could induce insulin resistance through suppressing IRS1 phosphorylation at Tyr608 and then inhibiting its downstream PI3K and AKT phosphorylation [53]. 2% taurine drinking water improved the insulin sensitivity in skeletal muscle of rats fed with high sugar and high-fat diet by increasing the mRNA and protein expression of IRS1 [54]. In this study, oleic acid increased the serine phosphorylation of IRS-1 and decreased the expression of p-PI3K (p85)-Tyr607, p-Akt-Thr308, p-Akt-Ser473 in HepG2 cells and induced insulin resistance, taurine reduced the serine phosphorylation level of IRS-1 and improved the interference of oleic acid with IRS1-PI3K-Akt pathway (Fig. 2a, c). In agreement with the results of steatotic cells, taurine reduced the serine phosphorylation level of IRS-1 in the liver of rats fed with high-fat diet and improved the inhibition of the IRS1-PI3K-Akt pathway by high-fat diet (Fig. 5a, c). Considering the opposite regulation of mTOR by AMPK and insulin signaling pathways, it seems unlikely that taurine can improve both pathways. But taurine did, and it alleviated the inhibition of insulin signaling pathway and activated AMPK pathway. From the perspective of mTOR, the common downstream target of the two pathways, taurine is ultimately shown to inhibit its phosphorylation. This suggests the important role of AMPK pathway in the intervention of taurine in fat synthesis. Meanwhile, this also suggests taurine is a fantabulous metabolic regulator because of showing a positive ameliorative effect on both of insulin resistance and steatosis of MAFLD.
Based on the results of animal experiments results, in terms of the dosage of taurine, both dose of taurine decreased the liver TG in rats fed a high fat diet, and showed certain improvement effects on AMPK and insulin signaling pathways. And the effect of high-dose taurine is more obvious, because only high-dose taurine inhibited the protein level of SREBP-1c and its downstream enzymes in the liver of rats fed a high-fat diet, even decreased the serum TG level in regular diet fed rat. That indicated that the high dose is somewhat high, while the optimal dose for taurine TG-lowering action may be in the range of high and low doses (70–350mg/kg bw/day), which requires further investigation in the subsequent experiments.
In addition to post-translational modifications (phosphorylation of LKB1-AMPK), miRNAs, small endogenous RNAs, are also capable of regulating the AMPK pathway, and they play important role in post-transcriptional gene regulation and regulate their targets by translational inhibition [55]. miR-451 has been proved to be able to directly target the scaffold protein (Calcium-binding protein 39) of LKB1 and increase the expression of SREBP-1c by inhibiting the LKB1-AMPK pathway in mice cardiac myocytes, thereby promoting the synthesis of fatty acids [30]. In macrophages, miR-33 encoded by SREBP gene intron can directly target inhibits the expression of AMPKα in order to indirect regulation SREBP and lipid metabolism [56,57]. Activation of AMPK can inhibit lipid accumulation and decrease the expression of miR-291b-3p in NCTC1469 hepatic cells [29]. In the present study, taurine suppressed the increase in miR-451, 33 and 291b expression in rat liver induced by a high-fat diet (Fig. 5e), which was consistent with the increased expression of LKB1 and AMPK proteins, suggesting that taurine also activates the LKB1-AMPKα pathway at the post-transcriptional level via miRNAs.
5. Conclusion
Taurine is effective in alleviating MAFLD in steatotic HepG2 cells and high-fat dietary SD rats. The mechanisms of hepatoprotection by taurine include: 1) against TG synthesis through activation of LKB1-AMPKα by phosphorylation or by no-phosphorylation manner (via inhibiting miR451, 33, 291b), subsequently inhibiting mTOR, SREBP-1c, PPARγ and their downstream FA synthesis-related enzymes, or directly increasing ACC phosphorylation to reduce ACC activity; 2) inhibit serine phosphorylation of IRS-1 to improve IRS-1-PI3K-AKT pathway; 3) improve inflammatory and injury status. The results promise that administration of taurine is ameliorative for the initial MAFLD and provide reference for the dosage of taurine.
Author contribution statement
Qi Song: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Jun xia Guo, Yu xun Ma: Performed the experiments; Analyzed and interpreted the data.
Tong Ou, Jing Zhang, Hui zi Li, Yan zhen Zhang: Performed the experiments.
Sheng quan Mi: Analyzed and interpreted the data.
Hiroaki Oda, Wen Chen: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data.
Funding statement
We gratefully acknowledge the support of Academic Research Projects of Beijing Union University (XP202005) and Qi Song thanks China CSC Scholarship for financial support (202208050007).
Data availability statement
The data that has been used is confidential.
Ethics statement
This research protocol was approved by the Experimental Animal Ethics Committee of the Functional Test Center for Health Food, College of Arts and Sciences, Beijing Union University. Animal welfare and experimental procedures were performed strictly in accordance with the Guidelines for the Care and Use of Laboratory Animals.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that might influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e16401.
Contributor Information
Hiroaki Oda, Email: hirooda@agr.nagoya-u.ac.jp.
Wen Chen, Email: wlchenwen@buu.edu.cn.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
figs1.
figs2.
figs3.
figs4.
figs5.
figs6.
figs7.
figs8.
figs9.
figs10.
figs11.
figs12.
figs13.
figs14.
figs15.
figs16.
figs17.
figs18.
figs19.
figs20.
figs21.
figs22.
figs23.
figs24.
figs25.
figs26.
figs27.
figs28.
figs29.
figs30.
figs31.
figs32.
figs33.
figs34.
figs35.
figs36.
figs37.
figs38.
figs39.
figs40.
figs41.
figs42.
figs43.
figs44.
figs45.
References
- 1.Eslam M., Newsome P.N., Sarin S.K., Anstee Q.M., Targher G., Romero-Gomez M., Zelber-Sagi S., Wong V.W.-S., Dufour J.-F., Schattenberg J.M., Kawaguchi T., Arrese M., Valenti L., Shiha G., Tiribelli C., Yki-Järvinen H., Fan J.-G., Grønbæk H., Yilmaz Y., Cortez-Pinto H., Oliveira C.P., Bedossa P., Adams L.A., Zheng M.-H., Fouad Y., Chan W.-K., Mendez-Sanchez N., Ahn S.H., Castera L., Bugianesi E., Ratziu V., George J. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J. Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 2.Puri P., Baillie R.A., Wiest M.M., Mirshahi F., Choudhury J., Cheung O., Sargeant C., Contos M.J., Sanyal A.J. A lipidomic analysis of nonalcoholic fatty liver disease. Hepatology. 2007;46:1081–1090. doi: 10.1002/hep.21763. [DOI] [PubMed] [Google Scholar]
- 3.Le M.H., Yeo Y.H., Li X., Li J., Zou B., Wu Y., Ye Q., Huang D.Q., Zhao C., Zhang J., Liu C., Chang N., Xing F., Yan S., Wan Z.H., Tang N.S.Y., Mayumi M., Liu X., Liu C., Rui F., Yang H., Yang Y., Jin R., Le R.H.X., Xu Y., Le D.M., Barnett S., Stave C.D., Cheung R., Zhu Q., Nguyen M.H. Clinical Gastroenterology and Hepatology; 2019. Global NAFLD Prevalence: A Systematic Review and Meta-Analysis. (2021) S1542356521012805. [DOI] [PubMed] [Google Scholar]
- 4.Huang D.Q., El-Serag H.B., Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2021;18:223–238. doi: 10.1038/s41575-020-00381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guerreiro G.T.S., Longo L., Fonseca M.A., de Souza V.E.G., Álvares-da-Silva M.R. Does the risk of cardiovascular events differ between biopsy-proven NAFLD and MAFLD? Hepatol. Int. 2021;15:380–391. doi: 10.1007/s12072-021-10157-y. [DOI] [PubMed] [Google Scholar]
- 6.EASL-EASD-EASO clinical practice Guidelines for the management of non-alcoholic fatty liver disease. Obes. Facts. 2016;9:65–90. doi: 10.1159/000443344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wen C., Li F., Zhang L., Duan Y., Guo Q., Wang W., He S., Li J., Yin Y. Taurine is involved in energy metabolism in muscles, adipose tissue, and the liver. Mol. Nutr. Food Res. 2019;63 doi: 10.1002/mnfr.201800536. [DOI] [PubMed] [Google Scholar]
- 8.Lambert I.H., Kristensen D.M., Holm J.B., Mortensen O.H. Physiological role of taurine – from organism to organelle. Acta Physiol. 2015;213:191–212. doi: 10.1111/apha.12365. [DOI] [PubMed] [Google Scholar]
- 9.Murakami S., Ono A., Kawasaki A., Takenaga T., Ito T. Taurine attenuates the development of hepatic steatosis through the inhibition of oxidative stress in a model of nonalcoholic fatty liver disease in vivo and in vitro. Amino Acids. 2018;50:1279–1288. doi: 10.1007/s00726-018-2605-8. [DOI] [PubMed] [Google Scholar]
- 10.Chang Y.-Y., Chou C.-H., Chiu C.-H., Yang K.-T., Lin Y.-L., Weng W.-L., Chen Y.-C. Preventive effects of taurine on development of hepatic steatosis induced by a high-fat/cholesterol dietary habit. J. Agric. Food Chem. 2011;59:450–457. doi: 10.1021/jf103167u. [DOI] [PubMed] [Google Scholar]
- 11.Chen X., Sebastian B.M., Tang H., McMullen M.M., Axhemi A., Jacobsen D.W., Nagy L.E. Taurine supplementation prevents ethanol-induced decrease in serum adiponectin and reduces hepatic steatosis in rats. Hepatology. 2009;49:1554–1562. doi: 10.1002/hep.22811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang M., Bi L.F., Fang J.H., Su X.L., Da G.L., Kuwamori T., Kagamimori S. Beneficial effects of taurine on serum lipids in overweight or obese non-diabetic subjects. Amino Acids. 2004;26 doi: 10.1007/s00726-003-0059-z. [DOI] [PubMed] [Google Scholar]
- 13.Yamori Y., Taguchi T., Mori H., Mori M. Low cardiovascular risks in the middle aged males and females excreting greater 24-hour urinary taurine and magnesium in 41 WHO-CARDIAC study populations in the world. J. Biomed. Sci. 2010;17:S21. doi: 10.1186/1423-0127-17-S1-S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang R., Yang Q., Lin S., Feng Y., Yang J., Lv Q., Wu G., Hu J. In: Preventive or Curative Administration of Taurine Regulates Lipid Metabolism in the Liver of Rats with Alcoholic Liver Disease. Hu J., Piao F., Schaffer S.W., El Idrissi A., Wu J.-Y., editors. Springer Singapore; Singapore: 2019. pp. 119–131. (Taurine 11). [DOI] [PubMed] [Google Scholar]
- 15.Miyata M., Funaki A., Fukuhara C., Sumiya Y., Sugiura Y. Taurine attenuates hepatic steatosis in a genetic model of fatty liver disease. J. Toxicol. Sci. 2020;45:87–94. doi: 10.2131/jts.45.87. [DOI] [PubMed] [Google Scholar]
- 16.Fang D., Wan Y., Shen W., Cao J., Sun Z., Yu H., Zhang Q., Cheng W., Chen J., Ning B. Endoplasmic reticulum stress leads to lipid accumulation through upregulation of SREBP-1c in normal hepatic and hepatoma cells. Mol. Cell. Biochem. 2013;381:127–137. doi: 10.1007/s11010-013-1694-7. [DOI] [PubMed] [Google Scholar]
- 17.Xu X., So J.-S., Park J.-G., Lee A.-H. Transcriptional control of hepatic lipid metabolism by SREBP and ChREBP, Seminars in Liver Disease. Thieme Medical Publishers; 2013. pp. 301–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y., Xu S., Mihaylova M.M., Zheng B., Hou X., Jiang B., Park O., Luo Z., Lefai E., Shyy J.Y.-J., Gao B., Wierzbicki M., Verbeuren T.J., Shaw R.J., Cohen R.A., Zang M. AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice. Cell Metabol. 2011;13:376–388. doi: 10.1016/j.cmet.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Day E.A., Ford R.J., Steinberg G.R. AMPK as a therapeutic target for treating metabolic diseases. Trends Endocrinol. Metabol. 2017;28:545–560. doi: 10.1016/j.tem.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Ponugoti B., Kim D.-H., Xiao Z., Smith Z., Miao J., Zang M., Wu S.-Y., Chiang C.-M., Veenstra T.D., Kemper J.K. SIRT1 deacetylates and inhibits SREBP-1C activity in regulation of hepatic lipid metabolism. J. Biol. Chem. 2010;285:33959–33970. doi: 10.1074/jbc.M110.122978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akhtar A., Sah S.P. Insulin signaling pathway and related molecules: role in neurodegeneration and Alzheimer's disease. Neurochem. Int. 2020;135 doi: 10.1016/j.neuint.2020.104707. [DOI] [PubMed] [Google Scholar]
- 22.Gwinn D.M., Shackelford D.B., Egan D.F., Mihaylova M.M., Mery A., Vasquez D.S., Turk B.E., Shaw R.J. AMPK phosphorylation of raptor mediates a metabolic checkpoint. Mol. Cell. 2008;30:214–226. doi: 10.1016/j.molcel.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yecies J.L., Zhang H.H., Menon S., Liu S., Yecies D., Lipovsky A.I., Gorgun C., Kwiatkowski D.J., Hotamisligil G.S., Lee C.-H., Manning B.D. Akt stimulates hepatic SREBP1c and lipogenesis through parallel mTORC1-dependent and independent pathways. Cell Metabol. 2011;14:21–32. doi: 10.1016/j.cmet.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agbu P., Carthew R.W. MicroRNA-mediated regulation of glucose and lipid metabolism. Nat. Rev. Mol. Cell Biol. 2021;22:425–438. doi: 10.1038/s41580-021-00354-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eren F. The relationship between polyphenols and miRNAs: a novel therapeutic strategy for metabolic associated fatty liver disease. Hepatol. Forum. 2021:128–136. doi: 10.14744/hf.2021.2021.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu-xun M., Qi S., Jing Z., Jun-xia G., Tian-ze X., Wen C. Effect of taurine on triglyceride synthesis in HepG2 cells. Nat. Product Res. Dev. 2020;32:867–873. [Google Scholar]
- 27.Quan H.Y., Kim D.Y., Chung S.H. Caffeine attenuates lipid accumulation via activation of AMP-activated protein kinase signaling pathway in HepG2 cells. BMB Rep. 2013;46:207–212. doi: 10.5483/BMBRep.2013.46.4.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karunakaran D., Richards L., Geoffrion M., Barrette D., Gotfrit R.J., Harper M.-E., Rayner K.J. Therapeutic inhibition of miR-33 promotes fatty acid oxidation but does not ameliorate metabolic dysfunction in diet-induced obesity. ATVB. 2015;35:2536–2543. doi: 10.1161/ATVBAHA.115.306404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meng X., Guo J., Fang W., Dou L., Li M., Huang X., Zhou S., Man Y., Tang W., Yu L., Li J. Liver MicroRNA-291b-3p promotes hepatic lipogenesis through negative regulation of adenosine 5′-monophosphate (AMP)-activated protein kinase α1. J. Biol. Chem. 2016;291:10625–10634. doi: 10.1074/jbc.M116.713768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuwabara Y., Horie T., Baba O., Watanabe S., Nishiga M., Usami S., Izuhara M., Nakao T., Nishino T., Otsu K., Kita T., Kimura T., Ono K. MicroRNA-451 exacerbates lipotoxicity in cardiac myocytes and high-fat diet-induced cardiac hypertrophy in mice through suppression of the LKB1/AMPK pathway. Circ. Res. 2015;116:279–288. doi: 10.1161/CIRCRESAHA.116.304707. [DOI] [PubMed] [Google Scholar]
- 31.Cohen J.C., Horton J.D., Hobbs H.H. Human fatty liver disease: old questions and new insights. Science. 2011;332:1519–1523. doi: 10.1126/science.1204265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Torre P., Motta B.M., Sciorio R., Masarone M., Persico M. Inflammation and fibrogenesis in MAFLD: role of the hepatic immune system. Front. Med. 2021;8 doi: 10.3389/fmed.2021.781567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurtz J.A., VanDusseldorp T.A., Doyle J.A., Otis J.S. Taurine in sports and exercise. Sports Nutr. Rev. J. 2021;18:39. doi: 10.1186/s12970-021-00438-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo Y., Zhao Q., Cao L., Zhao B. Hepatoprotective effect of Gan Kang Yuan against chronic liver injury induced by alcohol. J. Ethnopharmacol. 2017;208:1–7. doi: 10.1016/j.jep.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 35.Abd Elwahab A.H., Ramadan B.K., Schaalan M.F., Tolba A.M. A novel role of SIRT1/FGF-21 in taurine protection against cafeteria diet-induced steatohepatitis in rats. Cell. Physiol. Biochem. 2017;43:644–659. doi: 10.1159/000480649. [DOI] [PubMed] [Google Scholar]
- 36.Saberi-Karimian M., Keshvari M., Ghayour-Mobarhan M., Salehizadeh L., Rahmani S., Behnam B., Jamialahmadi T., Asgary S., Sahebkar A. Effects of curcuminoids on inflammatory status in patients with non-alcoholic fatty liver disease: a randomized controlled trial. Compl. Ther. Med. 2020;49 doi: 10.1016/j.ctim.2020.102322. [DOI] [PubMed] [Google Scholar]
- 37.Softic S., Cohen D.E., Kahn C.R. Role of dietary fructose and hepatic de novo lipogenesis in fatty liver disease. Dig. Dis. Sci. 2016;61:1282–1293. doi: 10.1007/s10620-016-4054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Luong A., Hannah V.C., Brown M.S., Goldstein J.L. Molecular characterization of human acetyl-CoA synthetase, an enzyme regulated by sterol regulatory element-binding proteins. J. Biol. Chem. 2000;275:26458–26466. doi: 10.1074/jbc.M004160200. [DOI] [PubMed] [Google Scholar]
- 39.Tong L. Acetyl-coenzyme A carboxylase: crucial metabolic enzyme and attractive target for drug discovery. Cell. Mol. Life Sci. CMLS. 2005;62:1784–1803. doi: 10.1007/s00018-005-5121-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jensen-Urstad A.P.L., Semenkovich C.F. Fatty acid synthase and liver triglyceride metabolism: housekeeper or messenger? Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2012;1821:747–753. doi: 10.1016/j.bbalip.2011.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dumas S.N., Guo C., Kim J.K., Friedline R.H., Ntambi J.M. Interleukin-6 derived from cutaneous deficiency of stearoyl-CoA desaturase- 1 may mediate metabolic organ crosstalk among skin, adipose tissue and liver. Biochem. Biophys. Res. Commun. 2019;508:87–91. doi: 10.1016/j.bbrc.2018.11.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horton J.D., Goldstein J.L., Brown M.S. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J. Clin. Invest. 2002;109:1125–1131. doi: 10.1172/JCI0215593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morán-Salvador E., López-Parra M., García-Alonso V., Titos E., Martínez-Clemente M., González-Périz A., López-Vicario C., Barak Y., Arroyo V., Clària J. Role for PPARγ in obesity-induced hepatic steatosis as determined by hepatocyte- and macrophage-specific conditional knockouts. Faseb. J. 2011;25:2538–2550. doi: 10.1096/fj.10-173716. [DOI] [PubMed] [Google Scholar]
- 44.Ha J., Daniel S., Broyles S.S., Kim K.H. Critical phosphorylation sites for acetyl-CoA carboxylase activity. J. Biol. Chem. 1994;269:22162–22168. doi: 10.1016/S0021-9258(17)31770-2. [DOI] [PubMed] [Google Scholar]
- 45.Sakurai Y., Kubota N., Yamauchi T., Kadowaki T. Role of insulin resistance in MAFLD. IJMS. 2021;22:4156. doi: 10.3390/ijms22084156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yan Y., Zhou X., Xu H., Melcher K. Structure and physiological regulation of AMPK. IJMS. 2018;19:3534. doi: 10.3390/ijms19113534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang Q., Liu S., Zhai A., Zhang B., Tian G. AMPK-mediated regulation of lipid metabolism by phosphorylation. Biol. Pharm. Bull. 2018;41:985–993. doi: 10.1248/bpb.b17-00724. [DOI] [PubMed] [Google Scholar]
- 48.Morsy M.D., Aboonq M.S., Alsleem M.A., Abusham A.A. Taurine prevents high‐fat diet‐induced‐hepatic steatosis in rats by direct inhibition of hepatic sterol regulatory element‐binding proteins and activation of AMPK. Clin. Exp. Pharmacol. Physiol. 2021;48:72–85. doi: 10.1111/1440-1681.13387. [DOI] [PubMed] [Google Scholar]
- 49.Hardie D.G., Ross F.A., Hawley S.A. AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat. Rev. Mol. Cell Biol. 2012;13:251–262. doi: 10.1038/nrm3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Woods A., Dickerson K., Heath R., Hong S.-P., Momcilovic M., Johnstone S.R., Carlson M., Carling D. Ca2+/calmodulin-dependent protein kinase kinase-β acts upstream of AMP-activated protein kinase in mammalian cells. Cell Metabol. 2005;2:21–33. doi: 10.1016/j.cmet.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 51.Bkaily G., Jaalouk D., Sader S., Shbaklo H., Pothier P., Jacques D., D'Orléans-Juste P., Cragoe E.J., Bose R. Taurine indirectly increases [Ca]i by inducing Ca2+ influx through the Na(+)-Ca2+ exchanger. Mol. Cell. Biochem. 1998;188:187–197. [PubMed] [Google Scholar]
- 52.Liu X., Chhipa R.R., Nakano I., Dasgupta B. The AMPK inhibitor compound C is a potent AMPK-independent antiglioma agent. Mol. Cancer Therapeut. 2014;13:596–605. doi: 10.1158/1535-7163.MCT-13-0579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li L., Fang B., Zhang Y., Yan L., He Y., Hu L., Xu Q., Li Q., Dai X., Kuang Q., Xu M., Tan J., Ge C. Carminic acid mitigates fructose-triggered hepatic steatosis by inhibition of oxidative stress and inflammatory reaction. Biomed. Pharmacother. 2022;145 doi: 10.1016/j.biopha.2021.112404. [DOI] [PubMed] [Google Scholar]
- 54.Zhao D., Lv Q., Yang J., Wu G., Liu M., Yang Q., Han J., Feng Y., Lin S., Hu J. In: Taurine Improves Lipid Metabolism and Skeletal Muscle Sensitivity to Insulin in Rats Fed with High Sugar and High Fat Diet. Hu J., Piao F., Schaffer S.W., El Idrissi A., Wu J.-Y., editors. Springer Singapore; Singapore: 2019. pp. 133–146. (Taurine 11). [DOI] [PubMed] [Google Scholar]
- 55.Bushati N., Cohen S.M. microRNA Functions. Annu. Rev. Cell Dev. Biol. 2007;23:175–205. doi: 10.1146/annurev.cellbio.23.090506.123406. [DOI] [PubMed] [Google Scholar]
- 56.Rayner K.J., Esau C.C., Hussain F.N., McDaniel A.L., Marshall S.M., van Gils J.M., Ray T.D., Sheedy F.J., Goedeke L., Liu X., Khatsenko O.G., Kaimal V., Lees C.J., Fernandez-Hernando C., Fisher E.A., Temel R.E., Moore K.J. Inhibition of miR-33a/b in non-human primates raises plasma HDL and lowers VLDL triglycerides. Nature. 2011;478:404–407. doi: 10.1038/nature10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu D., Tan Q., Zhu J., Zhang Y., Xue Y., Song Y., Liu Y., Wang Q., Lai L. MicroRNA-33/33* inhibit the activation of MAVS through AMPK in antiviral innate immunity. Cell. Mol. Immunol. 2021;18:1450–1462. doi: 10.1038/s41423-019-0326-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.